- 1Department of Psychiatry, University of Michigan, Ann Arbor, MI, USA
- 2Center for Research on Ethnicity, Culture and Health, School of Public Health, University of Michigan, Ann Arbor, MI, USA
- 3Medicine and Health Promotion Institute, Tehran, Iran
Background: The Black–White health paradox can be defined as lower frequency of depression despite higher prevalence of economic and social adversities as well as chronic medical conditions (CMC) among American Blacks compared to American Whites. Based on this paradox, the CMC – depressive symptoms link is expected to be weaker among Blacks than Whites. We conducted a 10-year longitudinal study to compare Blacks and Whites for bidirectional associations between number of CMC and negative affect over time.
Methods: We used data from the MIDUS (Midlife in the United States), a nationally representative longitudinal study of American adults. A total number of 7,108 individuals with an age range of 25–75 years (N = 7,108) were followed for 10 years from 1995 to 2004. Age, gender, and socioeconomic status (education and income) were measured at baseline. Negative affect and CMC were measured at baseline (1995) and end of follow up (2004). Race was the moderator. Linear regression was used to test the moderating effect of race on the reciprocal associations between CMC and negative affect, net of covariates.
Results: In the pooled sample, while baseline CMC was predictive of an increase in negative affect over time, baseline negative affect was also predictive of an increase in CMC. We found interactions between race and baseline CMC on change in depressive symptoms, as well as race with negative affect on CMC change, suggesting that the associations between CMC and negative affect are stronger for Whites in comparison to Blacks.
Conclusion: Blacks and Whites differ in reciprocal links between CMC and negative affect over time. This finding replicates recent studies on differential links between psychosocial factors and physical health based on race. Findings may help us better understand how Black-White health paradox develops across mid and later life.
Introduction
Chronic medical conditions (CMC) are more prevalent among Blacks than Whites (1, 2). Emotional problems such as depression are, however, less common among Blacks (3–5). As a result, a larger discrepancy exists between CMC and depression among Blacks (6, 7). Disproportionately lower prevalence of depression despite higher levels of social and economic adversities as well as CMC among Blacks, compared to Whites, is also known as the Black–White health paradox (5, 6). Studies that have found weaker associations between CMC and depression among Blacks (8–11) have lent empirical support to the Black–White health paradox. Not all studies, however, have found such group differences (11–14).
As most prior studies in this area have used a cross-sectional design (9–14), there is still a need for additional longitudinal research (7). In 2015, Assari and colleagues applied multi-group structural equation modeling to data from the Americans’ Changing Lives (ACL) study and showed that among White but not Black respondents, higher CMC at baseline predicted an increase in depressive symptoms over a 25-year follow up period. Among Whites but not Blacks, depressive symptoms at baseline were predictive of incident CMC over time, as well (7). In another attempt, Assari and colleagues used multi-group cross-lagged modeling and documented race by gender group differences in the lagged effects of depressive symptoms and restless sleep on change in CMC over time. While White men, White women, and Black women were similar in the residual effect of restless sleep over depressive symptoms on CMC, such effect was missing among Black men (15).
These studies all suggest that contextual factors such as race and ethnicity should be conceptualized as moderators that may alter the reciprocal associations between CMC and depression (16–18). Also called as the differential effect hypothesis, this approach focuses on the contextual (moderating) effects of race and ethnicity, rather than their main (direct) effects. In this view, populations differ for associations that ultimately influence health and illness (16–18).
Despite our knowledge of the bidirectional nature of the relationship between depression and CMC, existing information is still limited on potential population differences in the reciprocal relationships between CMC and negative affect over time. Built on the existing literature (7, 11, 12, 19–22), we compared Blacks and Whites for the reciprocal associations between CMC and negative affect over a 10-year period.
Materials and Methods
Design and Setting
Data came from the MIDUS, 1995–2004. The MIDUS is a nationally representative longitudinal cohort study of 7,000 + adult Americans aged 25–74. The study is carried out by the MacArthur Midlife Research Network. The main purpose of the study was to investigate the role of psychosocial factors in understanding age variation in physical and mental health (23–26).
Ethics
The study was approved by the Institutional Review Board at University of Wisconsin-Madison, UCLA, and Georgetown University. Informed written consent was obtained for all participants. The study was funded by the National Institute on Aging. Monetary incentives were offered at both wave 1 and 2 to compensate for potential respondent burden (US$20 for completion of MIDUS 1 surveys and up to US$60 for completion of MIDUS 2 surveys).
Process
The survey was multimodal, composed of phone interviews and self-report questionnaires. First, the study employed an initial 30-min phone or face-to-face interview followed by a set (two) of self-administered questionnaires (SAQs). Questionnaires were mailed to individuals after completing the phone interview.
Data collection of the wave 1 was conducted in 1995 and 1996. Data collection of the wave 2 of the MIDUS was conducted in 2004 and 2005. The time-2 data collection used the original protocol (wave 1). All participants received letters as a reminder that an interviewer would contact them for a telephone survey in few weeks. Following completion of a phone interview that lasted 30-mins on average, participants received two SAQs via mail.
Participants and Sampling
The study used random digit dialing (RDD) to enroll participants. RDD is a widely accepted method for recruiting people to telephone statistical surveys. RDD generates telephone numbers at random, thus MIDUS enrolled a random sample of adults. The study used telephone numbers within the continental United States as the sampling frame for the national RDD survey. The study also used an oversampling in five cities. This stage resulted in 4,244 individuals enrolled via RDD sampling. By randomly selecting 529 cases from the RDD sample who had at least one sibling, a sibling sample was generated. Siblings were limited to those within a family that had the same biological mother and father. Using this strategy, the study enrolled 950 siblings. The study also used a two-part sampling design to enroll the twin sample [957 twin pairs (n = 1,914)].
Follow-up Data
From the total 7,108 participants who started the study (completing the phone survey at MIDUS 1), data were collected at wave 2 for 4,963 (70%) at MIDUS 2, which was 9–10 years later. Thus the MIDUS overall retention rate is 75% (adjusted for mortality). The retention rate was higher for siblings (81%) and twins (81%) compared to the RDD sample (69%). Major causes for non-participation at MIDUS 2 included refusal (12%), could not be contacted (10%), and too ill to be interviewed (8%) or deceased (verified by the National Death Index).
Measures
We collected data on core demographic variables and socioeconomic factors at baseline. Depressive symptoms and CMC were measured at waves 1 and 2.
Socioeconomic Factors
Demographic variables were collected at baseline in 1995 and included age (continuous), gender (0 = male, 1 = female), and race (0 = Whites, 1 = Blacks). Socioeconomic variables included educational attainment (treated as a continuous measure; 1 = less than high school, 2 = high school graduate or equivalent, 3 = some college, 4 = college graduate or more) and personal income (continuous measure).
Chronic Medical Conditions
Data were collected at wave 1 and 2 on history of 20 CMC. Examples of conditions are cancer, heart disease, diabetes (high blood sugar), asthma, bronchitis or emphysema, ulcer, migraine, and thyroid disease (27, 28).
Negative Affect
State negative affect (SNA) was assessed using a 6-item questionnaire that asked participants how much of the time over the past 30 days did they feel: “so sad,” “nervous,” “restless or fidgety,” “hopeless,” “worthless,” and “everything was an effort.” Participants rated their response on a 5-point scale from 1 (none of the time) to 5 (all of the time). We calculated a mean score, which could range from 1 to 5, with higher score indicating more negative affect. In this measure, SNA is conceptualized as symptoms of depression and anxiety, two emotions commonly used to define negative affect (29–31). The scale was similar to K-6 developed by Kessler and colleagues, which has yielded a single factor structure representing current, general psycho-logical distress (32). Cronbach’s alpha ranged from 0.75 to 0.85 across the eight administrations of this scale (33). Internal consistency (reliability) was excellent (α = 0.86 for Whites and 0.87 for Blacks).
Statistical Note
Data analysis was conducted in SPSS 20.0 for Windows (IBM Inc. Armonk, NY, USA). We ran multiple linear regressions in the pooled sample as well as based on race, with and without interaction. In the first step, CMC was the independent variable, and negative affect was the dependent variables. Then in the second step, negative affect was the independent variable, and CMC was the dependent variable. Race was the focal moderator. Age, gender, education, and income were covariates. Regression coefficients (b), SE with 95% Confidence Intervals (CI) were reported.
Results
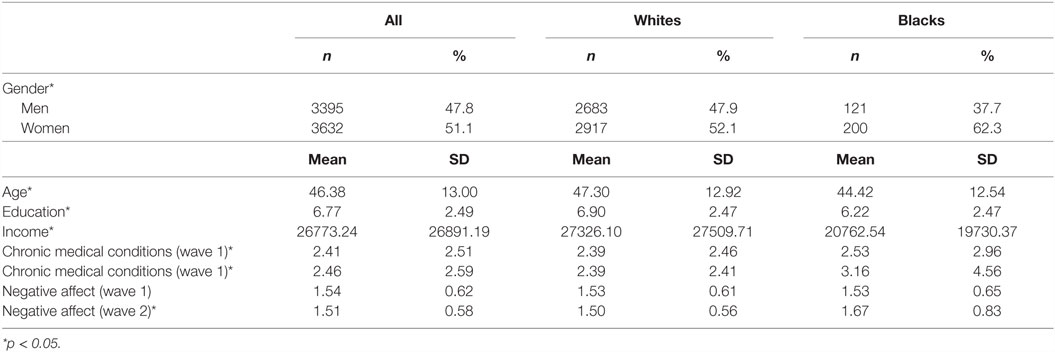
Table 1 presents the results of descriptive analysis in the pooled sample and based on race. Compared to Whites, Blacks were younger, were more frequently women, and had lower education and income. Blacks had higher CMC at wave 1 and 2 compared to Whites. Blacks also had higher negative affect at wave 2.
Table 2 summarizes two regression models in the pooled sample with CMC as the predictor and depressive symptoms as the outcome. According to Model 1, which did not include the interaction term, baseline CMC predicted change in negative affect, net of socioeconomic factors. Model 2 also included an interaction between race and CMC showed a significant and negative interaction between Black race and baseline CMC on change in negative affect, suggesting that the association between baseline CMC and subsequent change in negative affect is stronger for Whites in comparison to Blacks.
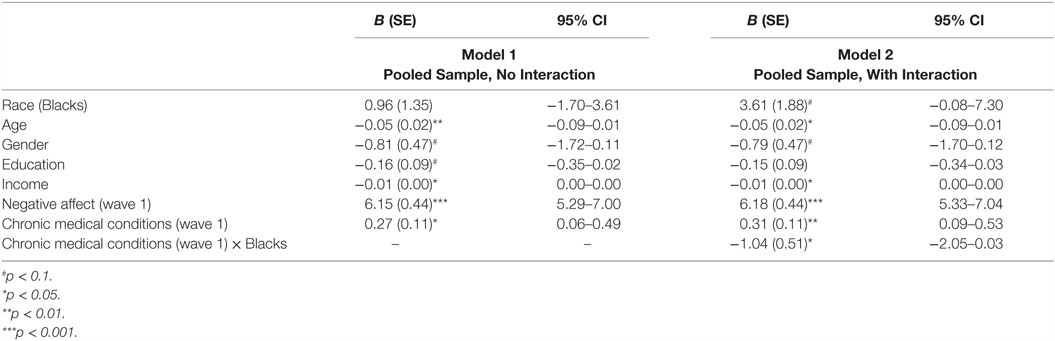
Table 2. Predictive role of baseline chronic medical conditions on wave 2 negative affect in the pooled sample.
Table 3 provides a summary of two regression models in the pooled sample with negative affect at wave 1 as the predictor and CMC at wave 2 as the outcome. According to our Model 1 which did not include the interaction term, baseline negative affect was predictive of change in CMC, net of socioeconomic factors. Based on Model 2, there was a significant interaction between race and baseline negative affect on CMC at wave 2, suggesting that race alters the effect of baseline negative affect and change in CMC.
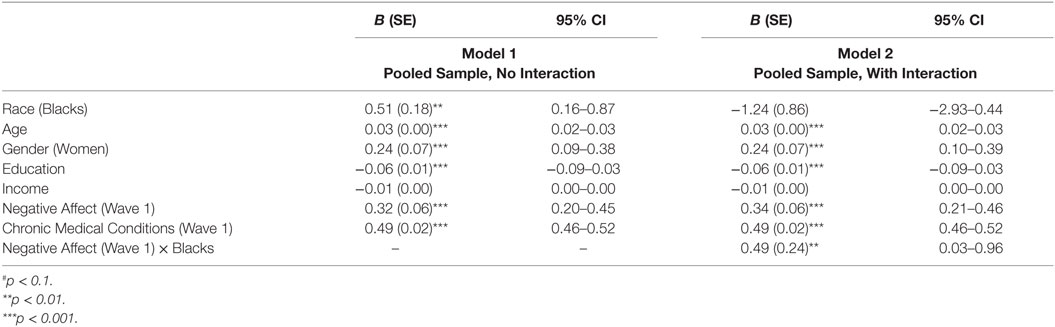
Table 3. Predictive role of baseline negative affect on wave 2 chronic medical conditions in the pooled sample.
Table 4 presents the results of regression models with CMC at wave 1 as the independent variable and negative affect at wave 2 as the outcome across race groups. Only among Whites (Model 1) but not Blacks (Model 2), baseline CMC predicted a change in negative affect over time, net of socioeconomic factors.
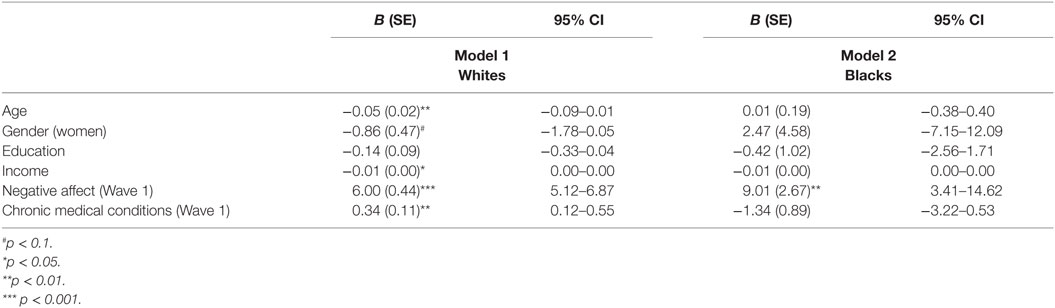
Table 4. Predictive role of baseline chronic medical conditions (1995) on subsequent negative affect (2004) among Whites and Blacks.
Table 5 summarizes the results of race-specific regression models with negative affect at wave 1 as the predictor and CMC at wave 2 as the outcome. Among Whites (Model 1), baseline negative affect predicted CMC change over time, net of demographic and socioeconomic factors. The same association could not be found for Blacks (Model 2).
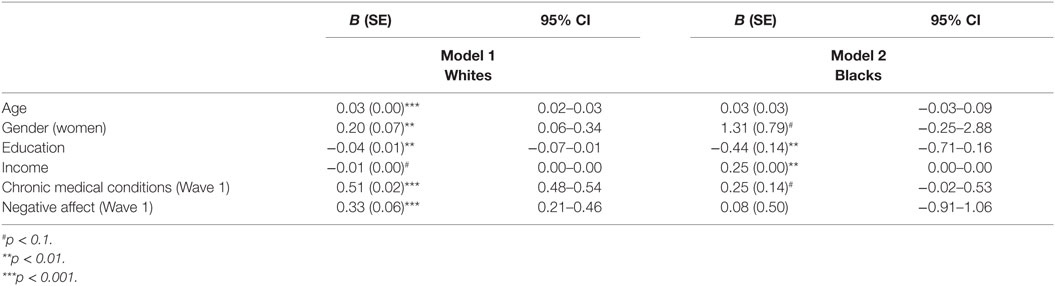
Table 5. Predictive role of baseline negative affect (1995) on subsequent chronic medical conditions (2004) among Whites and Blacks.
Discussion
According to our findings, Whites and Blacks differ in reciprocal and longitudinal associations between CMC and negative affect over a 10-year period. Thus, race alters the inter-relation between baseline and change of CMC and negative affect in the United States.
In our study, baseline CMC predicted change in negative affect among Whites but not Blacks. Similarly, baseline negative affect predicted change in CMC among Whites but not Blacks. These findings replicate a previous report by Assari et al., using 25-year follow-up data (7). This replication is important as Assari et al. mentioned: “… the duration of follow up was 25 years, which may have caused selective deaths in the population, particularly among Blacks and those with high baseline chronic medical conditions. Future reports may consider replication of the current findings using shorter follow-up periods.” (7). These studies provide longitudinal support for the Black–White health paradox (6, 7, 22, 34, 35), defined as lower prevalence of depression or depressive symptoms (4) despite higher prevalence of CMC and other social and economic adversities (1, 2).
Capistrant and colleagues have shown that the link between baseline depressive symptoms and subsequent mortality due to cardiovascular causes was significant for Whites but not Blacks, after adjusting for potential confounders (36). There are other studies that have documented racial differences in depression associated with specific CMC types (20, 21, 37). For instance, Lewis and colleagues found evidence suggesting that depressive symptoms may have different effect on cardiovascular risk for Blacks and Whites (8, 38).
There are multiple explanations for Black–White differences in the link between depression and CMC. Jackson and colleagues have attributed these findings to racial differences in engagement in a number of unhealthy behaviors such as smoking or overeating that help Blacks cope with psychological distress but impose physiological damages at the same time (37, 39). Such ineffective coping behaviors may increase the physical toll associated with stress and distress among Blacks (19, 37, 39–41).
Literature has also provided results that are either inconsistent (11, 12, 37) or unexpected (10, 11, 42). As compared to Whites, Blacks have more CMC but less depression, we intuitively expect weaker depressive symptoms – CMC link for Blacks. That is, any incremental increase in CMC is expected to have a smaller effect on depressive symptoms among Blacks compared to Whites. Hankerson and colleagues, however, documented a stronger association between major depressive disorder (MDD) and hypertension, obesity, and liver disease among Blacks compared to Whites (42), and Assari found cross-sectional positive association between MDD and cardiovascular diseases among Blacks that could not be replicated for Whites (10). Further, using the National Survey of American Life (NSAL) data, Watkins, Assari, and Johnson-Lawrence showed that lifetime MDD was associated with at least one CMC among Blacks, but not Whites (12). A few existing studies have failed to show any moderating effect of race on the association between CMC and depression (11, 14). As several of the above findings contradict the expected stronger association between depression and CMC among Whites than Blacks, we still need more research that explores racial variations in the cross-sectional and longitudinal links between CMC and depression.
Previous research has shown that the link between depression and CMC is bidirectional (43–49). While baseline CMC predicts subsequent depression (43–47), baseline depression also increases risk of CMC in the future (48, 49). However, this literature has mainly enrolled White middle class individuals (43, 47–49) and more is yet to be known on population variations in these associations (50).
Depression is known to be more chronic and disabling for Blacks in comparison to Whites (10, 12). Among those with lifetime MDD, frequency of 12-month MDD is higher for Blacks (56%) than Whites (39%) (4). Higher chronicity of depression for Blacks (4, 10, 12) may be in part due to low access and trust to the health care system as well as high stigma for Blacks than Whites (4, 10, 12). Negative beliefs regarding pharmaceutical treatment (4), preference of non-pharmacologic approaches (e.g., counseling and prayer) (51), and the belief that antidepressants are addictive (51) may also operate as barriers against depression treatment among Blacks. Higher comorbidity of CMC among Blacks with depression also adds to the complexity of diagnosis of depression among Blacks (1, 2, 52, 53). Differential presentation of depression (more somatic among Blacks) may also be another barrier for diagnosis (54). Given the worse trajectory of depression among Blacks, one would expect stronger effects of depression and negative emotions on CMC for Blacks (7).
Improving screening, diagnoses, and treatment of emotional problems such as depression among Blacks require major investment (4, 55, 56). Still, the primary care setting should be regarded as a unique opportunity for depression screening among Blacks who receive care for their medical conditions (57–59). However, quality improvement programs should also enhance quality of psychiatric services in primary care settings, particularly for Blacks (12, 60).
This study contributes to a growing literature that has documented Black–White differences in how psychological factors contribute to a wide range of physical health outcomes including but not limited to CMC and mortality (7, 61, 62). Lucas and colleagues have shown that psychological as well as biological processes that contribute to cardiovascular health disparities are not simply the consequence of individual level exposures but the interplay between individual-level and contextual factors (e.g., views about justice) (63). Mezuk et al. have suggested that behaviors may explain why the links between emotional and physical health problems are weaker among Blacks (41). Keyes et al. have attributed such differences to flourishing of Blacks in the face of social inequality and discrimination (5, 6). Kitayama et al. have attributed these findings to cultural differences in tolerance and affordance of emotional dysregulation (64–66). Other researchers have attributed these group differences to stereotypes and schemas such as strong Black Woman ideology (67–69). Such differential effects are not specific to depression and negative affect (16) and have been seen for self-rated health as well (17). These findings are also consistent with findings by Stewart and colleagues that suggest depressive symptoms predict inflammatory markers among Whites but not Blacks (70–72). Boyle, Williams, and others have also shown Black–White differences in the link between psychological and biological markers of serotonin with insulin sensitivity (73–76).
The results reported here should be interpreted with the following limitations in mind. First, this study measured number of CMC, regardless of their type. Second, CMC measurement was based on self-reported data. As race may alter associations between depression and particular types of CMC (8, 9, 14, 20, 21, 37, 38, 43), there is a need to determine CMC types that may differently correlate with depression and negative emotions based on race. Third, this study measured negative affect, not clinical depression. Some studies have suggested that clinical diagnosis of depression is differently associated with CMC than depressive symptoms (8, 9, 14, 20, 21, 37, 38, 43). Negative emotions may also differently predict MDD across racial groups (70). The study did not control for access to health care, insurance, and function, as well as behaviors that may influence CMC, depression, or both. Forth, Whites were over-represented in the sample. Despite these limitations, this study still makes a unique contribution to the literature as only a handful of studies have compared Blacks and Whites for reciprocal associations between affect and CMC over time (7).
Our findings advocate for designing and implementing tailored rather than universal programs that screen for combined physical and emotional health problems at the community as well as in primary health-care settings. As racial groups differ in how physical and mental health problems co-exist and develop, race should be in the center of comprehensive protocols that focus simultaneously on multiple health aspects of diverse populations. Race groups with similar level of CMC may have different emotional needs. Integrative care may particularly benefit from adjustment to culture, race, and ethnicity (77). Findings may also have implications for the health-care reform, also known as Obama care (78).
In summary, we found racial differences in reciprocal associations between CMC and negative affect over a 10-year period. Comorbidity between physical and emotional health problems is not independent of context, and the inter-relations between the trajectories of these health problems may be context specific.
Author Contributions
SA was responsible for the design and analysis of the data and revisions. ML drafted the manuscript. Both authors approved the final draft.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
SA is supported by the Heinz C. Prechter Bipolar Research Fund and the Richard Tam Foundation at the University of Michigan Depression Center.
Funding
This research was supported by a grant from the National Institute on Aging (P01-AG020166) to conduct a longitudinal follow-up of the MIDUS investigation. The original study was supported by the John D. and Catherine T. MacArthur Foundation Research Network on Successful Midlife Development.
References
1. Johnson-Lawrence VD, Griffith DM, Watkins DC. The effects of race, ethnicity and mood/anxiety disorders on the chronic physical health conditions of men from a national sample. Am J Mens Health (2013) 7:58S–67S. doi:10.1177/1557988313484960
2. Cabassa LJ, Humensky J, Druss B, Lewis-Fernández R, Gomes AP, Wang S, et al. Do race, ethnicity, and psychiatric diagnoses matter in the prevalence of multiple chronic medical conditions? Med Care (2013) 51:540–7. doi:10.1097/MLR.0b013e31828dbb19
3. González HM, Tarraf W, Whitfield KE, Vega WA. The epidemiology of major depression and ethnicity in the United States. J Psychiatr Res (2010) 44:1043–51. doi:10.1016/j.jpsychires.2010.03.017
4. Williams DR, González HM, Neighbors H, Nesse R, Abelson JM, Sweetman J, et al. Prevalence and distribution of major depressive disorder in African Americans, Caribbean Blacks, and non-Hispanic Whites: results from the National Survey of American Life. Arch Gen Psychiatr (2007) 64:305–15. doi:10.1001/archpsyc.64.3.305
5. Barnes DM, Keyes KM, Bates LM. Racial differences in depression in the United States: how do subgroup analyses inform a paradox? Soc Psychiatry Psychiatr Epidemiol (2013) 48:1941–9. doi:10.1007/s00127-013-0718-7
6. Keyes CL. The Black–White paradox in health: flourishing in the face of social inequality and discrimination. J Pers (2009) 77:1677–706. doi:10.1111/j.1467-6494.2009.00597.x
7. Assari S, Burgard S, Zivin K. Long-term reciprocal associations between depressive symptoms and number of chronic medical conditions: longitudinal support for black-white health paradox. J Racial Ethn Health Disparities (2015) 2:589–97. doi:10.1007/s40615-015-0116-9
8. Lewis TT, Guo H, Lunos S, Mendes de Leon CF, Skarupski KA, Evans DA, et al. Depressive symptoms and cardiovascular mortality in older black and white adults: evidence for a differential association by race. Circ Cardiovasc Qual Outcomes (2011) 4:293–9. doi:10.1161/CIRCOUTCOMES.110.957548
9. Gottlieb SS, Khatta M, Friedmann E, Einbinder L, Katzen S, Baker B, et al. The influence of age, gender, and race on the prevalence of depression in heart failure patients. J Am Coll Cardiol (2004) 43:1542–9. doi:10.1016/j.jacc.2003.10.064
10. Gonzalez HM, Tarraf W. Comorbid cardiovascular disease and major depression among ethnic and racial groups in the United States. Int Psychogeriatr (2013) 25:833–41. doi:10.1017/S1041610212002062
11. Assari S. Chronic medical conditions and major depressive disorder: differential role of positive religious coping among African Americans, Caribbean Blacks and Non-Hispanic Whites. Int J Prev Med (2014) 5:405–13.
12. Watkins DC, Assari S, Johnson-Lawrence V. Race and ethnic group differences in comorbid major depressive disorder, generalized anxiety disorder, and chronic medical conditions. J Racial Ethn Health Disparities (2015) 2:385–94. doi:10.1007/s40615-015-0085-z
13. Assari S. Race and ethnic differences in associations between cardiovascular diseases, anxiety, and depression in the United States. Int J Travel Med Glob Health (2014) 2(3):107–13.
14. Assari S. Chronic kidney disease, anxiety and depression among American blacks; does ethnicity matter? Int J Travel Med Glob Health (2014) 2(4):133–9.
15. Assari S, Sonnega A, Pepin R, Leggett A. Residual effects of restless sleep over depressive symptoms on chronic medical conditions: race by gender differences. J Racial Ethn Health Disparities (2016). doi:10.1007/s40615-015-0202-z
16. Assari S, Burgard S. Black-White differences in the effect of baseline depressive symptoms on deaths due to renal diseases: 25 year follow up of a nationally representative community sample. J Renal Inj Prev (2015) 4:127–34. doi:10.12861/jrip.2015.27
17. Assari S, Lankarani MM, Burgard S. Black-white difference in long-term predictive power of self-rated health on all-cause mortality in United States. Ann Epidemiol (2016) 26:106–14. doi:10.1016/j.annepidem.2015.11.006
18. Assari S. Race and ethnic differences in additive and multiplicative effects of depression and anxiety on cardiovascular risk. Int J Prev Med (2016) 7:22. doi:10.4103/2008-7802.173931
19. Jackson JS, Knight KM, Rafferty JA. Race and unhealthy behaviors: chronic stress, the HPA axis, and physical and mental health disparities over the life course. Am J Public Health (2010) 100:933–9. doi:10.2105/AJPH.2008.143446
20. Assari S. Additive effects of anxiety and depression on body mass index among blacks: role of ethnicity and gender. Int Cardiovasc Res J (2014) 8:44–51.
21. Assari S, Caldwell CH. Gender and ethnic differences in the association between obesity and depression among black adolescents. J Racial Ethn Health Disparities (2015) 2:481–93. doi:10.1007/s40615-015-0096-9
22. Keyes CLM, Simoes EJ. To flourish or not: positive mental health and all-cause mortality. Am J Public Health (2012) 102(11):2164–72. doi:10.2105/AJPH.2012.300918
23. Radler BT, Ryff CD. Who participates? Accounting for longitudinal retention in the MIDUS national study of health and well-being. J Aging Health (2010) 22:307–31. doi:10.1177/0898264309358617
24. Dienberg Love G, Seeman TE, Weinstein M, Ryff CD. Bioindicators in the MIDUS national study: protocol, measures, sample, and comparative context. J Aging Health (2010) 22:1059–80. doi:10.1177/0898264310374355
25. Midlife in the United States (MIDUS) (2016). Available from: http://www.midus.wisc.edu
26. National Institute on Aging Database of Longitudinal Studies. Available from: http://nihlibrary.ors.nih.gov/nia/ps/niadb.asp
27. Piazza JR, Charles ST, Almeida DM. Living with chronic health conditions: age differences in affective well-being. J Gerontol B Psychol Sci Soc Sci (2007) 62:313–21. doi:10.1093/geronb/62.6.P313
28. Marmot M, Ryff CD, Bumpass LL, Shipley M, Marks NF. Social inequalities in health: next questions and converging evidence. Soc Sci Med (1997) 44:901–10. doi:10.1016/S0277-9536(96)00194-3
29. Leventhal EA, Hansell S, Diefenbach M, Leventhal H, Glass DC. Negative affect and self-reports of physical symptoms: two longitudinal studies of older adults. Health Psychol (1996) 15:282–8. doi:10.1037/0278-6133.15.3.193
30. Diefenbach MA, Leventhal EA, Leventhal H, Patrick-Miller L. Negative affect relates to cross-sectional but not longitudinal symptom reporting: data from elderly adults. Health Psychol (1996) 15(4):282–8. doi:10.1037/0278-6133.15.4.282
31. Mroczek DK, Kolarz CM. The effect of age on positive and negative affect: a developmental perspective on happiness. J Pers Soc Psychol (1998) 75(5):1333–49. doi:10.1037/0022-3514.75.5.1333
32. Kessler RC, Andrews G, Colpe L, Hiripi E, Mroczek DK, Normand SL, et al. Short screening scales to monitor population prevalences and trends in nonspecific psychological distress. Psychol Med (2002) 32:959–76. doi:10.1017/S0033291702006074
33. Charles ST, Almeida DM. Daily reports of symptoms and negative affect: not all symptoms are the same. Psychol Health (2006) 21(1):1–7. doi:10.1080/14768320500129239
34. Watkins DC, Hudson DL, Caldwell CH, Siefert K, Jackson JS. Discrimination, mastery, and depressive symptoms among African American men. Res Soc Work Pract (2011) 21:269–77. doi:10.1177/1049731510385470
35. Williams DR, Earl TR. Commentary: race and mental health – more questions than answers. Int J Epidemiol (2007) 36(4):758–60. doi:10.1093/ije/dym114
36. Capistrant BD, Gilsanz P, Moon JR, Kosheleva A, Patton KK, Glymour MM. Does the association between depressive symptoms and cardiovascular mortality risk vary by race? Evidence from the Health and Retirement Study. Ethn Dis (2013) 23:155–60.
37. Assari S. Association between obesity and depression among American Blacks: role of ethnicity and gender. J Racial Ethn Health Disparities (2014) 1:36–44. doi:10.1007/s40615-014-0007-5
38. Lewis TT, Everson-Rose SA, Colvin A, Matthews K, Bromberger JT, Sutton-Tyrrell K. Interactive effects of race and depressive symptoms on calcification in African American and white women. Psychosom Med (2009) 71:163–70. doi:10.1097/PSY.0b013e31819080e5
39. Jackson JS, Knight KM. Race and self-regulatory health behaviors: the role of the stress response and the HPA axis in physical and mental health disparities. In: Schaie KW, Carstensen LL, editors. Social Structures, Aging, and Self-Regulation in the Elderly. New York, NY: Springer (2006). p. 189–207.
40. Mezuk B, Rafferty JA, Kershaw KN, Hudson D, Abdou CM, Lee H, et al. Reconsidering the role of social disadvantage in physical and mental health: stressful life events, health behaviors, race, and depression. Am J Epidemiol (2010) 172(11):1238–49. doi:10.1093/aje/kwq283
41. Mezuk B, Abdou CM, Hudson D, Kershaw KN, Rafferty JA, Lee H, et al. “White Box” epidemiology and the social neuroscience of health behaviors: the environmental affordances model. Soc Ment Health (2013) 3. doi:10.1177/2156869313480892
42. Hankerson SH, Fenton MC, Geier T, Keyes KM, Weissman MM, Hasin DS. Racial differences in symptoms, comorbidity, and treatment for major depressive disorder among Black and White adults. J Nat Med Assoc (2011) 103:576–84. doi:10.1016/S0027-9684(15)30383-7
43. Matheson FI, Smith KL, Fazli GS, Moineddin R, Dunn JR, Glazier RH. Physical health and gender as risk factors for usage of services for mental illness. J Epidemiol Community Health (2014) 68:971–8. doi:10.1136/jech-2014-203844
44. Patten SB. Long-term medical conditions and major depression in the Canadian population. Can J Psychiatry (1999) 44:151–7.
45. Kim JM, Stewart R, Kim SW, Yang SJ, Shin IS, Yoon JS. Insomnia, depression, and physical disorders in late life: a 2-year longitudinal community study in Koreans. Sleep (2009) 32:1221–8.
46. Patten SB. Long-term medical conditions and major depression in a Canadian population study at waves 1 and 2. J Affect Disord (2001) 63:35–41. doi:10.1016/S0165-0327(00)00186-5
47. Husaini BA. Predictors of depression among the elderly: racial differences over time. Am J Orthopsychiatry (1997) 67:48–58. doi:10.1037/h0080210
48. Tsai TY, Livneh H, Lu MC, Tsai PY, Chen PC, Sung FC. Increased risk and related factors of depression among patients with COPD: a population-based cohort study. BMC Public Health (2013) 19(13):976. doi:10.1186/1471-2458-13-976
49. Patten SB, Williams JV, Lavorato DH, Modgill G, Jetté N, Eliasziw M. Major depression as a risk factor for chronic disease incidence: longitudinal analyses in a general population cohort. Gen Hosp Psychiatry (2008) 30:407–13. doi:10.1016/j.genhosppsych.2008.05.001
50. Read JNG, Emerson MO. Racial context, black immigration and the US black/white health disparity. Soc Forces (2005) 84:181–99. doi:10.1353/sof.2005.0120
51. Givens JL, Katz IR, Bellamy S, Holmes WC. Stigma and the acceptability of depression treatments among African Americans and Whites. J Gen Intern Med (2007) 22:1292–7. doi:10.1007/s11606-007-0276-3
52. Assari S, Watkins DC, Caldwell CH. Race attribution modifies the association between daily discrimination and major depressive disorder among blacks: the role of gender and ethnicity. J Racial Ethn Health Disparities (2015) 2:1–11. doi:10.1007/s40615-014-0064-9
53. Kessler RC, Gruber M, Hettema JM, Hwang I, Sampson N, Yonkers KA. Co-morbid major depression and generalized anxiety disorders in the national comorbidity survey follow-up. Psychol Med (2008) 38:365–74. doi:10.1017/S0033291707002012
54. Bailey RK, Blackmon HL, Stevens FL. Major depressive disorder in the African American population: meeting the challenges of stigma, misdiagnosis, and treatment disparities. J Natl Med Assoc (2009) 101:1084–9. doi:10.1016/S0027-9684(15)31102-0
55. Bell C, Williamson J, Chien P. Cultural, racial and ethnic competence and psychiatric diagnosis. Ethn Inequal Health Soc Care (2008) 1:34–41. doi:10.1108/17570980200800006
56. Williams DR, Haile R, González HM, Neighbors H, Baser R, Jackson JS. The mental health of Black Caribbean immigrants: results from the national survey of American life. Am J Public Health (2007) 97:52–9. doi:10.2105/AJPH.2006.088211
57. Horvitz-Lennon M, Kilbourne AM, Pincus HA. From silos to bridges: meeting the general health care needs of people with mental illness. Health Aff (2006) 25:659–69. doi:10.1377/hlthaff.25.3.659
58. Woltmann E, Grogan-Taylor A, Perron B, Georges H, Kilbourne AM, Bauer MS. Comparative effectiveness of collaborative chronic care models for mental health conditions across primary, specialty, and behavioral health care settings: systematic review and meta-analysis. Am J Psychiatry (2012) 169:790–804. doi:10.1176/appi.ajp.2012.11111616
59. Pirraglia PA, Kilbourne AM, Lai Z, Friedmann PD, O’Toole TP. Colocated general medical care and preventable hospital admissions for veterans with serious mental illness. Psychiatr Serv (2011) 62:554–7. doi:10.1176/appi.ps.62.5.554
60. Agyemang AA, Mezuk B, Perrin P, Rybarczyk B. Quality of depression treatment in Black Americans with major depression and comorbid medical illness. Gen Hosp Psychiatry (2014) 36:431–6. doi:10.1016/j.genhosppsych.2014.02.011
61. Assari S, Moazen-Zadeh E, Lankarani MM, Micol-Foster V. Race, depressive symptoms, and all-cause mortality in the United States. Front Public Health (2016) 4:40. doi:10.3389/fpubh.2016.00040
62. Moazen-Zadeh E, Assari S. Depressive symptoms predict major depressive disorder after 15 years among whites but not blacks. Front Public Health (2016) 4:13. doi:10.3389/fpubh.2016.00013
63. Lucas T, Lumley MA, Flack JM, Wegner R, Pierce J, Goetz S. A preliminary experimental examination of worldview verification, perceived racism, and stress reactivity in African Americans. Health Psychol (2016) 35:366–75. doi:10.1037/hea0000284
64. Park J, Kitayama S, Markus HR, Coe CL, Miyamoto Y, Karasawa M, et al. Social status and anger expression: the cultural moderation hypothesis. Emotion (2013) 13:1122–31. doi:10.1037/a0034273
65. Boiger M, Mesquita B, Uchida Y, Feldman Barrett L. Condoned or condemned: the situational affordance of anger and shame in the United States and Japan. Pers Soc Psychol Bull (2013) 39:540–53. doi:10.1177/0146167213478201
66. Kitayama S, Park J, Boylan JM, Miyamoto Y, Levine CS, Markus HR, et al. Expression of anger and ill health in two cultures: an examination of inflammation and cardiovascular risk. Psychol Sci (2015) 26:211–20. doi:10.1177/0956797614561268
67. Miyamoto Y, Boylan JM, Coe CL, Curhan KB, Levine CS, Markus HR, et al. Negative emotions predict elevated interleukin-6 in the United States but not in Japan. Brain Behav Immun (2013) 34:79–85. doi:10.1016/j.bbi.2013.07.173
68. Watson NN, Hunter CD. “I had to be strong” tensions in the strong black woman schema. J Black Psychol (2015) 1–29. doi:10.1177/0095798415597093
69. Woods-Giscombé CL. Superwoman schema: African American women’s views on stress, strength, and health. Qual Health Res (2010) 20:668–83. doi:10.1177/1049732310361892
70. Vrany EA, Berntson JM, Khambaty T, Stewart JC. Depressive symptoms clusters and insulin resistance: race/ethnicity as a moderator in 2005-2010 NHANES data. Ann Behav Med (2016) 50:1–11. doi:10.1007/s12160-015-9725-0
71. Case SM, Stewart JC. Race/ethnicity moderates the relationship between depressive symptom severity and C-reactive protein: 2005-2010 NHANES data. Brain Behav Immun (2014) 41:101–8. doi:10.1016/j.bbi.2014.04.004
72. Stewart JC. One effect size does not fit all-is the depression-inflammation link missing in racial/ethnic minority individuals? JAMA Psychiatry (2016) 73:301–2. doi:10.1001/jamapsychiatry.2015.3205
73. Boyle SH, Georgiades A, Brummett BH, Barefoot JC, Siegler IC, Matson WR, et al. Associations between central nervous system serotonin, fasting glucose, and hostility in African American females. Ann Behav Med (2015) 49:49–57. doi:10.1007/s12160-014-9626-7
74. Surwit RS, Williams RB, Siegler IC, Lane JD, Helms M, Applegate KL, et al. Hostility, race, and glucose metabolism in nondiabetic individuals. Diabetes Care (2002) 25:835–9. doi:10.2337/diacare.25.5.835
75. Kodama K, Tojjar D, Yamada S, Toda K, Patel CJ, Butte AJ. Ethnic differences in the relationship between insulin sensitivity and insulin response: a systematic review and meta-analysis. Diabetes Care (2013) 36:1789–96. doi:10.2337/dc12-1235
76. Georgiades A, Lane JD, Boyle SH, Brummett BH, Barefoot JC, Kuhn CM, et al. Hostility and fasting glucose in African American women. Psychosom Med (2009) 71:642–5. doi:10.1097/PSY.0b013e3181acee3a
77. Kilbourne AM, Switzer G, Hyman K, Crowley-Matoka M, Fine MJ. Advancing health disparities research within the health care system: a conceptual framework. Am J Public Health (2006) 96:2113–21. doi:10.2105/AJPH.2005.077628
Keywords: population groups, ethnic groups, African Americans, chronic medical conditions, depression
Citation: Assari S and Lankarani MM (2016) Chronic Medical Conditions and Negative Affect; Racial Variation in Reciprocal Associations Over Time. Front. Psychiatry 7:140. doi: 10.3389/fpsyt.2016.00140
Received: 15 March 2016; Accepted: 29 July 2016;
Published: 24 August 2016
Edited by:
Marco Torrado, University of Lisbon, PortugalReviewed by:
Gabriel Rubio, Hospital Universitario 12 De Octubre, SpainTariq Munshi, Queen’s University, Canada
Pedro Paim Santos, University of São Paulo, Brazil
Copyright: © 2016 Assari and Lankarani. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shervin Assari, assari@umich.edu
 Shervin Assari
Shervin Assari Maryam Moghani Lankarani
Maryam Moghani Lankarani