An objective approach for Burkholderia pseudomallei strain selection as challenge material for medical countermeasures efficacy testing
- 1Battelle, Columbus, OH, USA
- 2Center for Microbial Genetics and Genomics, Northern Arizona University, Flagstaff, AZ, USA
Burkholderia pseudomallei is the causative agent of melioidosis, a rare disease of biodefense concern with high mortality and extreme difficulty in treatment. No human vaccines are available that protect against B. pseudomallei infection, and with the current limitations of antibiotic treatment, the development of new preventative and therapeutic interventions is crucial. Although clinical trials could be used to test the efficacy of new medical countermeasures (MCMs), the high mortality rates associated with melioidosis raises significant ethical issues concerning treating individuals with new compounds with unknown efficacies. The US Food and Drug Administration (FDA) has formulated a set of guidelines for the licensure of new MCMs to treat diseases in which it would be unethical to test the efficacy of these drugs in humans. The FDA “Animal Rule” 21 CFR 314 calls for consistent, well-characterized B. pseudomallei strains to be used as challenge material in animal models. In order to facilitate the efficacy testing of new MCMs for melioidosis using animal models, we intend to develop a well-characterized panel of strains for use. This panel will comprise of strains that were isolated from human cases, have a low passage history, are virulent in animal models, and are well-characterized phenotypically and genotypically. We have reviewed published and unpublished data on various B. pseudomallei strains to establish an objective method for selecting the strains to be included in the panel of B. pseudomallei strains with attention to five categories: animal infection models, genetic characterization, clinical and passage history, and availability of the strain to the research community. We identified 109 strains with data in at least one of the five categories, scored each strain based on the gathered data and identified six strains as candidate for a B. pseudomallei strain panel.
Introduction
Burkholderia pseudomallei is a Gram-negative bacterial pathogen responsible for the disease melioidosis, which is endemic in Southeast Asia, and northern Australia. B. pseudomallei can be cultured from tropical soils without requiring a host for environmental persistence (Kaestli et al., 2009; Currie et al., 2010). Melioidosis is historically associated with a high mortality rate due to the speed with which septicemia develops and the inherent resistance of the bacteria to several classes of antibiotics. While the overall mortality rate of melioidosis is 50% in Thailand, it is only 19% in the endemic areas of Australia (Limmathurotsakul et al., 2010). The difference between the mortality rates is most likely a result of the differing availability of efficacious treatment, though pathogen strain and host population differences may play a role. Although prolonged courses of antibiotic treatment (at least 10 days of intravenous antibiotics, followed by 12–20 weeks of oral antibiotics) are recommended, recurrent disease is common (at a rate of ≥6% in the first year; Chaowagul et al., 1993; Currie et al., 2000).
In addition to naturally occurring infections, B. pseudomallei is considered a biodefense threat because of the ease of acquiring strains from the environment, the ability to genetically manipulate the agent to be multiply antibiotic resistant, and the lack of a melioidosis vaccine (Vietri and Deshazer, 2007). Given the lengthy treatment with suboptimal outcomes, there is significant interest in developing improved medical countermeasures (MCMs) against melioidosis. In addition to improved antibiotic treatments, licensed vaccines are not currently available for melioidosis prophylaxis. In the case of B. pseudomallei, the limited number of confirmed respiratory acquired melioidosis cases each year call into question the feasibility of clinical trials for proper evaluation of therapeutics and/or vaccines. Experimental infection of humans with B. pseudomallei creates ethical concerns because therapeutic options are limited and consist of lengthy regimens. If melioidosis animal models are to be used to license new MCMs under the Food and Drug Administration (FDA) Animal Rule, well-characterized B. pseudomallei sources will be needed by the testing community. Since a number of different B. pseudomallei strains have been used in a variety of animal models, comparisons of the data are difficult. We reviewed the publicly available literature and used personal communications to gather data relevant to strain source, passage history, virulence, genotype, phenotype, and availability of B. pseudomallei strains with focus on those. Additionally, attributes of B. pseudomallei strains which apply to the FDA Animal Rule, particularly, animal infection models, genetic characterization, clinical and passage history, and the availability of strains to the research community were considered. FDA Animal Rule draft guidance from 2009 states “the challenge agent used in animal studies generally should be identical to the etiologic agent that causes the human disease (FDA, 2009).” For melioidosis, the agent is B. pseudomallei, but many different strains have been isolated from human cases. The genetic plasticity of B. pseudomallei dictates that strains with well-documented and low numbers of passages are preferred (Holden et al., 2004). Further, B. pseudomallei is known to have an unstable genome and having a reference genome sequence is desirable to monitor any genetic mutation and drift that may occur from laboratory passages. The FDA Animal Rule draft guidance also states “The disease manifestations, including the outcome (morbidity or mortality), should be compared between untreated animals and untreated humans (FDA, 2009).” Since melioidosis is a lethal disease, we also examined lethality in the animal model literature. Finally, as the development of animal models and MCMs will be an effort spanning multiple laboratories, we were interested in those B. pseudomallei strains that had the fewest impediments to wide distribution, such as licenses or restrictive material transfer agreements. We developed a scoring matrix to select six strains for inclusion in a panel to be tested in animal model development to meet the criteria of the FDA Animal Rule. Ideally, bacterial challenge material used in efficacy studies under the FDA Animal Rule would be a strain of B. pseudomallei that was recently isolated from a lethal human case of inhalational melioidosis, possess limited passage, exhibit virulence in one or more animal model of melioidosis, be well-characterized, and be freely available to laboratories licensed to work with B. pseudomallei. Using these and other criteria, a ranking system was developed and used to identify strains that will be included in a B. pseudomallei reference panel. Each section of this review will focus on B. pseudomallei strains that had the highest score for a single criterion, based on the availability of information for that criterion.
Isolation and Passage History
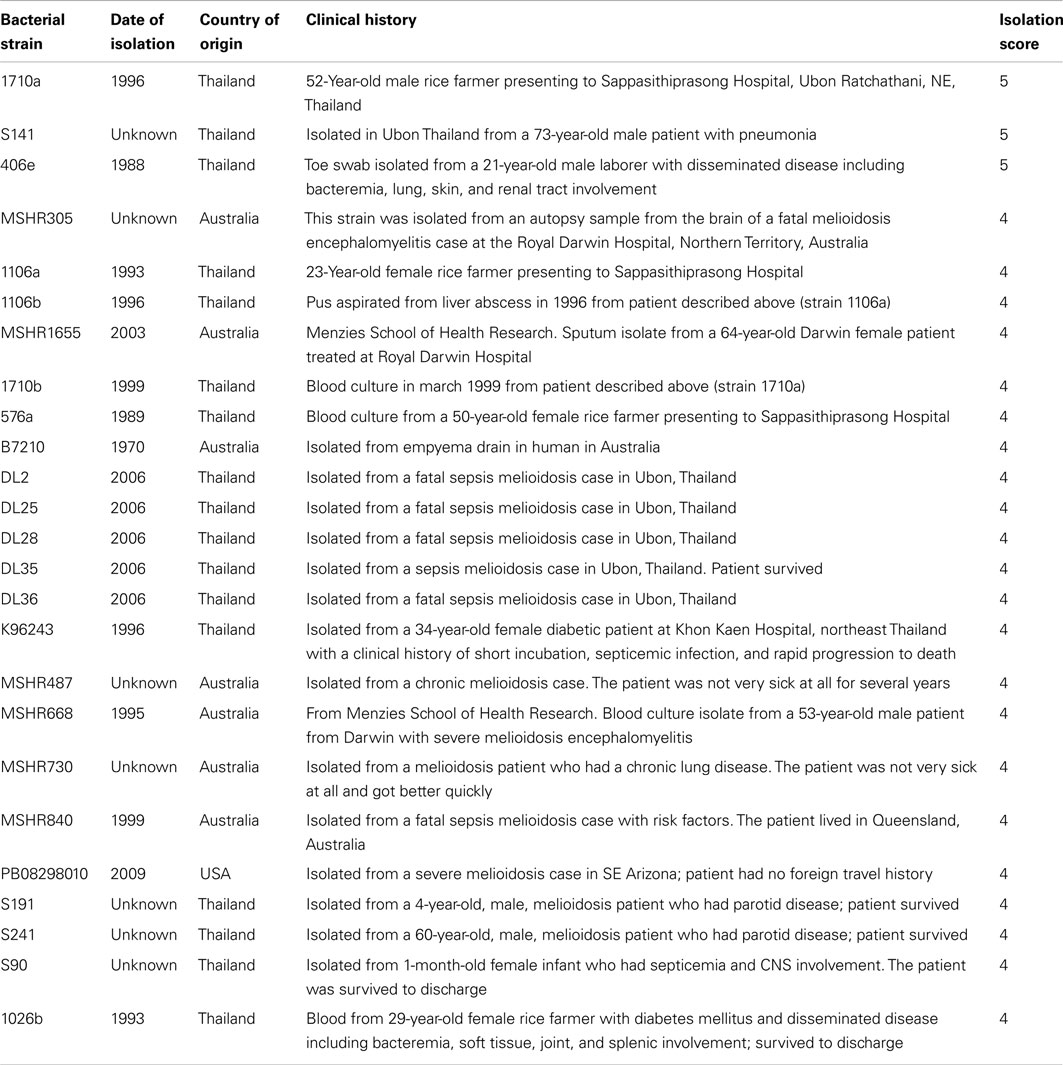
We had two criteria associated with the strain history; the patient history associated with the isolate and documented laboratory passage history. For isolation, strains were assigned a score on a scale of zero through five using the following six criteria:
0 points for no data on isolation
1 point for environmental isolate
2 points for isolation from an animal infection
3 points for isolation from a human clinical case, with no other data available
4 points for isolation from a human clinical case without pulmonary presentation
5 points for isolation from a human case with pulmonary presentation.
Using the above scoring matrix, three strains were assigned the highest score of 5 (isolated from an acute human case with pulmonary presentation, Table 1). Strain S141 was isolated in Ubon Ratchathani, NE, Thailand from a 73-year-old male patient with pneumonia. Strain 1710a was isolated from the blood culture in 1996 from a 52-year-old male rice farmer with a new diagnosis of diabetes mellitus presenting to Sappasithiprasong Hospital, Ubon Ratchathani, NE, Thailand (http://pathema.Jcvi.org/cgi-bin/Burkholderia/shared/HtmlPage.cgi?page=strains). The patient had disseminated disease, including bacteremia, lung involvement, and soft tissue involvement. The patient survived to discharge, but was readmitted in 1999 and died 1 day after readmission (http://pathema.jcvi.org/cgi-bin/Burkholderia/shared/HtmlPage.cgi?page=strains). Strain 406e was isolated from a toe swab in 1988 from a 21-year-old male laborer presenting to Sappasithiprasong Hospital (http://pathema.jcvi.org/cgi-bin/Burkholderia/shared/HtmlPage.cgi?page=strains). The patient had disseminated disease including bacteremia, lung, skin, and renal tract involvement. The patient succumbed to infection on the second day of admission (http://pathema.jcvi.org/cgi-bin/Burkholderia/shared/HtmlPage.cgi?page=strains; M. Wolcott, personal communication).
With only three strains receiving the highest score, other strains that did not score as highly are included because of other qualities making them attractive for animal model research. Strain K96243 was isolated from a 34-year-old female diabetic patient in Thailand. Strain 1106a was isolated from a 23-year-old female rice farmer in Thailand in 1996. Strain 1106b was isolated from the liver abscess in 1996 from the same rice farmer from which strain 1106a was isolated. Strain MSHR305 was isolated from an autopsy sample from the brain of a melioidosis encephalomyelitis case at the Royal Darwin Hospital, Northern Territory, Australia (http://pathema.jcvi.org/cgi-bin/Burkholderia/shared/HtmlPage.cgi?page=strains). Strain MSHR668 was isolated from the blood culture of a 53-year-old male patient with severe melioidosis encephalomyelitis at the Royal Darwin Hospital in 1995. The patient required prolonged ventilation, but survived. Strain 1026b was isolated from blood culture in 1993 from 29-year-old female rice farmer with a known diagnosis of diabetes mellitus presenting to Sappasithiprasong Hospital. The patient had disseminated disease including bacteremia, soft tissue, joint, and splenic involvement (http://pathema.jcvi.org/cgi-bin/Burkholderia/shared/HtmlPage.cgi?page=strains).
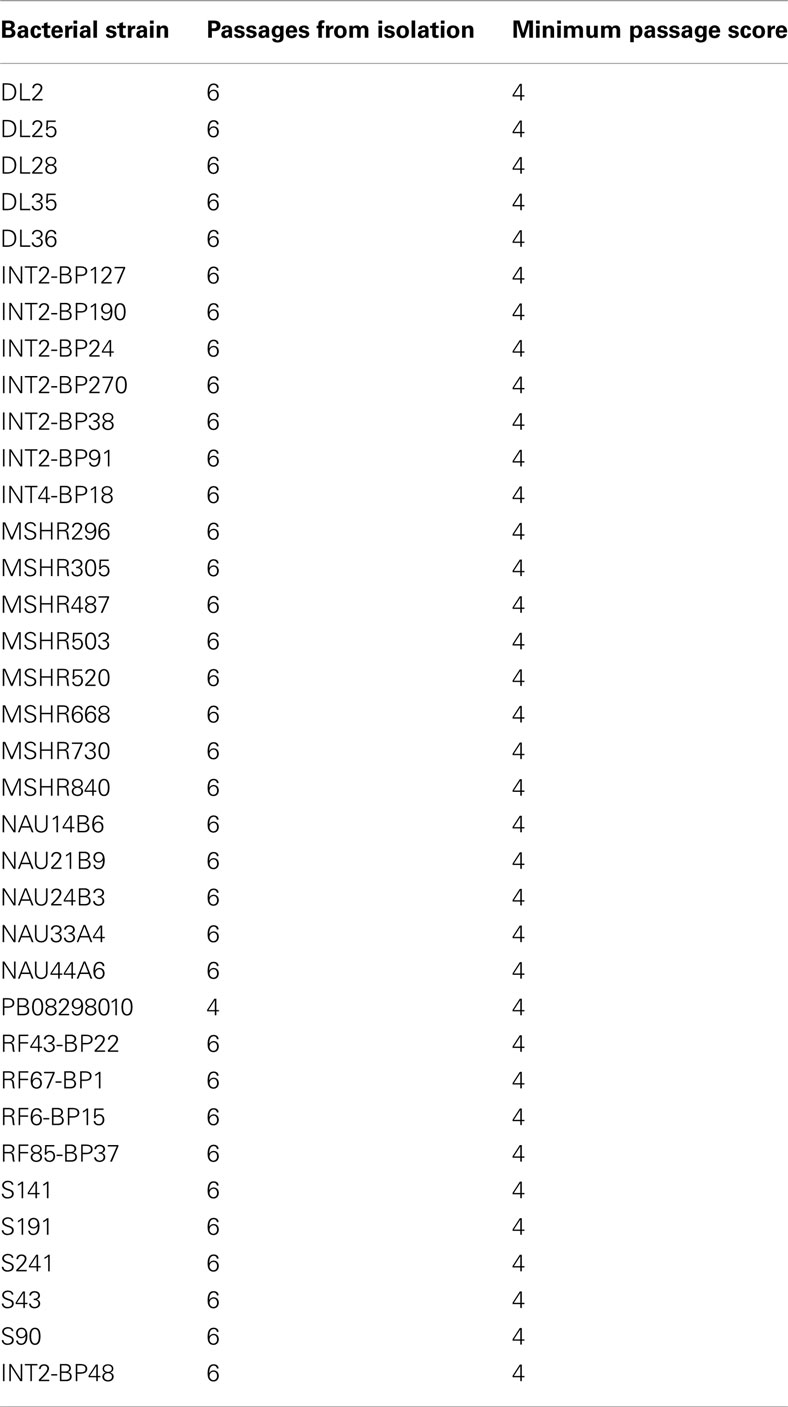
The second criterion is passage history. Strains with the lowest number of passages from clinical isolation were given the highest scores. Due to the genetic plasticity of B. pseudomallei, passage on artificial media or through animals could readily select for genetic variants with unknown impact on pathogenicity (Ulett et al., 2001), complicating data comparisons from studies using different sources of B. pseudomallei with different or unknown passage histories. Therefore, available B. pseudomallei strains were assigned scores based on the number of passages from isolation. High scoring B. pseudomallei strains are shown in Table 2. Strains were assigned a score on a scale of zero through five using the following six criteria:
0 points for no passage data
1 point for >11 passages since isolation
2 points for 9–10 passages since isolation
3 points for 7–8 passages since isolation
4 points for 4–6 passages since isolation
5 points for 3 or fewer passages since isolation.
No strain was identified with 3 or fewer passages from isolation, although strains passaged as few as 6 times were identified.
Animal Infection Models
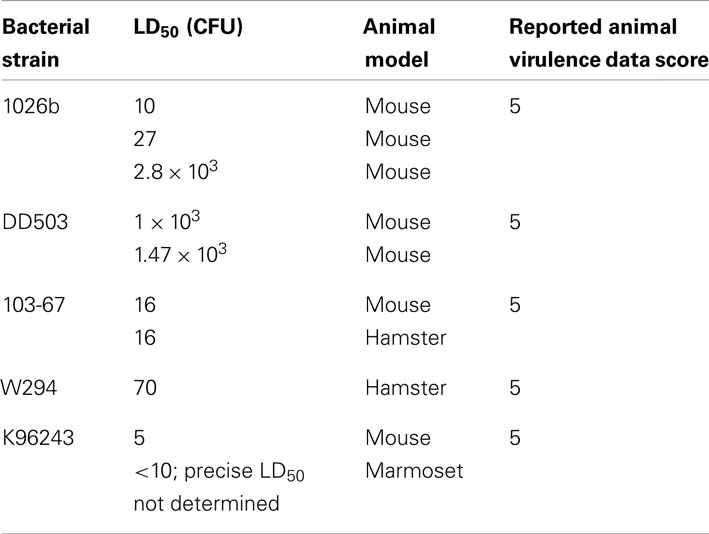
Strains selected for this reference panel should have a low lethal dose with aerosol delivery in animal models for testing biodefense MCMs. As mentioned above, the ideal etiologic agent for an FDA Animal Rule study will cause lethality in both animals and humans in an acute manner. For the purposes of this review, we considered acute lethality to be death within 28 days of infection. Therefore, we examined published literature for reports of B. pseudomallei strains being used to experimentally infect animals. The strain reference panel is to be used to test the efficacy of MCMs against inhalational melioidosis models, so emphasis was given to strains shown to be virulent in inhalation animal models. Strains were assigned a score on a scale of zero through five using the following six criteria:
0 points for no data on animal infection
1 point for infection of animal cell cultures
2 points for animal infection indicated but no route of infection reported
3 points for acute lethality in one or more mammals via a route not intranasal (IN) or aerosol
4 points for acute lethality in one mammal with IN or aerosol route
5 points for acute lethality in multiple mammals via IN or aerosol route.
Strains 1026b, DD503, 103-67, W294, and K96423 received the highest score in this rating system (Table 3) and are discussed below.
Strain 1026b
There is substantial literature on the virulence of B. pseudomallei 1026b in animal models of melioidosis. In murine models of pneumonic melioidosis, Jeddeloh et al. (2003) exposed BALB/c and C57BL/6 mice to whole-body aerosols. The LD50 of B. pseudomallei 1026b via this aerosol challenge method in BALB/c and C57BL/6 mice was 10 ± 8 and 27 ± 20 colony-forming units (CFU), respectively. The results suggest that both mouse strains have similar susceptibilities to the aerosolized B. pseudomallei. However, previous studies showed that the LD50 of IN challenge (an alternative to aerosol challenge) with 1026b was 2 logs higher in the resistant C57BL6 mouse when compared with the sensitive BALB/c mouse (Liu et al., 2002). Using a nose-only inhalational challenge system we showed that the LD50 in BALB/c mice was 2,772 CFUs (Sanford et al., 2010). Goodyear et al. (2009) reported that the LD50 of an IN challenge in BALB/c mice was 1 × 103 CFUs. These results suggest that B. pseudomallei 1026b has an LD50 between 10 and 2,772 CFUs, depending on the route of infection and strain of mouse infected. The difference in the LD50 for inhalational melioidosis in BALB/c mice could reflect differences in the method of aerosol challenge, whole-body, IN, or nose-only and/or differences in the virulence of the 1026b strains used in each of these studies and may be of interest in future investigations.
Strain DD503
Strain DD503 (ΔamrR-oprA) is a multi-drug efflux mutant strain derived from 1026b, which is hypersensitive to aminoglycosides and macrolides (Moore et al., 1999). In a whole-body inhalation BALB/c mouse model, the LD50 was determined to be 1 × 103 CFUs. Jeddeloh et al. (2003) reported the LD50 of strain DD503 to be 1,467 ± 301 CFUs in BALB/c mice following whole-body aerosol exposure. It is interesting that the mouse LD50 of DD503 is 100 times higher than 1026b. The reduced virulence of DD503 appears to be due to a mutation in the rpsL gene (Jeddeloh et al., 2003).
Strain 103-67
Dannenberg et al. (1958) challenged Syrian golden hamsters with an inhaled dose 3–600 LD50S (50–10,000 CFUs), and the inhalational LD50 of B. pseudomallei 103-67 in the hamster model appears to be approximately 17 CFUs. The lethality of inhaled B. pseudomallei strain 103-67 in albino mice was also examined, and in mice that succumbed to infection with an inhaled does of 18–600 LD50s (300–10,000 CFUs), the inhalational LD50 in mice of approximately 17 CFUs.
Strain W294
Miller et al. (1948) determined the virulence of IP challenges of B. pseudomallei strain W294 in hamsters, guinea pigs, ferrets, rabbits, mice, rats, and non-human primates. However, the aerosol LD50 of W294 was determined to be 70 CFU in the hamster. Black and white mice were infected with B. pseudomallei W294 and 60–75% of the animals died, but the LD50 was not evaluated.
Strain K96243
The vast majority of animal work done with strain K96243 was performed in mice (C57Bl/6 and BALB/c). In an effort to examine the differential susceptibility to infection between the two most commonly used mouse strains (C57Bl/6 and BALB/c), Tan et al. (2008) infected both mouse strains via various routes including the IN (nose-only aerosol). The calculated IN LD50 was 226 CFU in BALB/c mice and 1.5 × 104 CFU in C57Bl/6 mice. Their data indicates that BALB/c mice are significantly more susceptible to infection with B. pseudomallei than the C57Bl/6 strain.
While large animal models of infection with B. pseudomallei have not yet been extensively examined, one recent study by Nelson et al. (2011) aimed to determine if the common marmoset would be a viable large animal model of infection. A lethal infection was established with aerosol challenge doses below 10 CFU. Because of the extreme lethality, a precise LD50 was not able to be determined. They concluded that the common marmoset should be considered as a suitable model for further studies of inhalational melioidosis.
Genetic Characterization
Burkholderia pseudomallei is a soil-dwelling saprophyte and with genetic diversity resulting from horizontal gene transfer (Tuanyok et al., 2008; Zhu et al., 2011). These transfers are recognized as regions in the genome [genomic island (GI) regions] with lower G/C content and that encode a broad array of functions. Genetic variability has been demonstrated in strains isolated from a single patient and isolates from different tissues within the patient (Hayden et al., 2012). This genetic variability makes it essential that the genomes of each strain in the panel be genetically characterized. B. pseudomallei strains have been genotyped using PCR methods, such as random amplified polymorphic DNA (RAPD; Leelayuwat et al., 2000) and multilocus sequence typing (MLST; Godoy et al., 2003; McCombie et al., 2006). RAPD detects differences in genomes by amplifying segments of unknown DNA. These PCR fragments are separated based upon electrophoretic mobility and the strains are compared by the presence or absence of bands. The production of PCR artifacts makes this genotyping method less robust than MLST genotyping. MLST compares the sequence of artificially concatenated amplicons of seven housekeeping genes. These genes are assumed to be selectively neutral or under purifying selection. MLST provides nucleotide data for multiple haplotypes, is amenable to phylogenetic analyses. Currie et al. (2007) reported that the MLST genotypes of strains from Australia were distinct from strains isolated in Thailand. Another PCR-based method variable number tandem repeat (VNTR) loci has been shown as a useful tool for genotyping B. pseudomallei. A VNTR locus consists of tandemly repeated sequences of DNA that vary in copy number, creating PCR amplicon size polymorphisms that are easily detected with gel electrophoresis. Due to increased mutation rates when compared to other regions of DNA and their multi-allelic nature, VNTRs allow superior discrimination between closely related isolates. Variations in VNTR can be observed in serially passed isolates (U’Ren et al., 2007; Price et al., 2010).
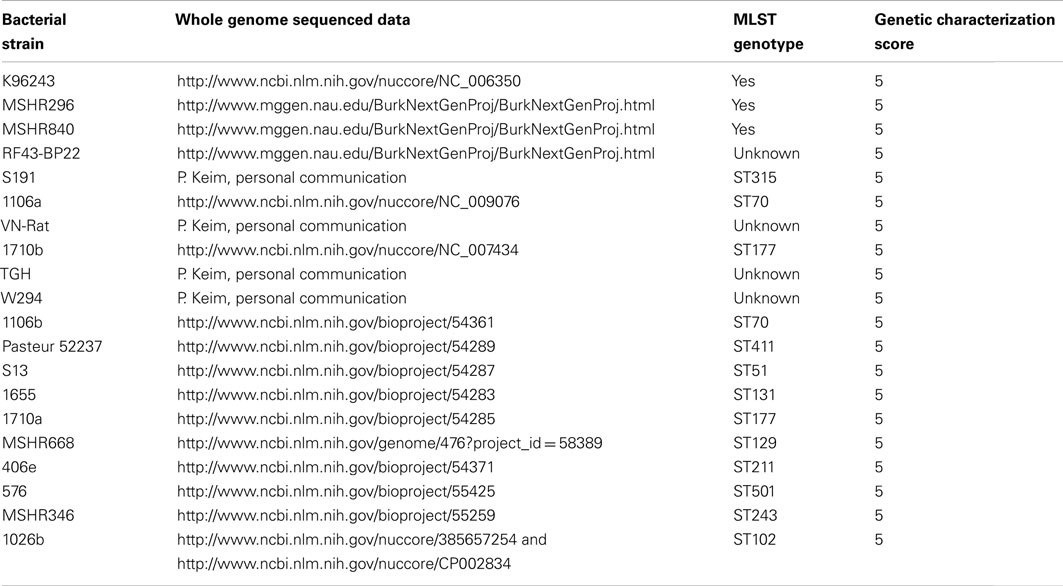
Finally, the rapid reduction in the cost of whole genome sequencing makes it feasible to compare the genomic sequence of different strains and to identify any genetic changes occurring due to in vitro or in vivo passage. Therefore, the scoring for genetic characterization was:
0 points for no genetic data (note that there are no criteria under which we assigned 1 or 2 points, given the importance of genetic characterization)
3 points for MLST
4 points for sequencing of GIs
5 points for sequenced genome data.
Twenty strains received the highest score in this rating system (Table 4) although a discussion of the features of the sequencing efforts is beyond the scope of this review.
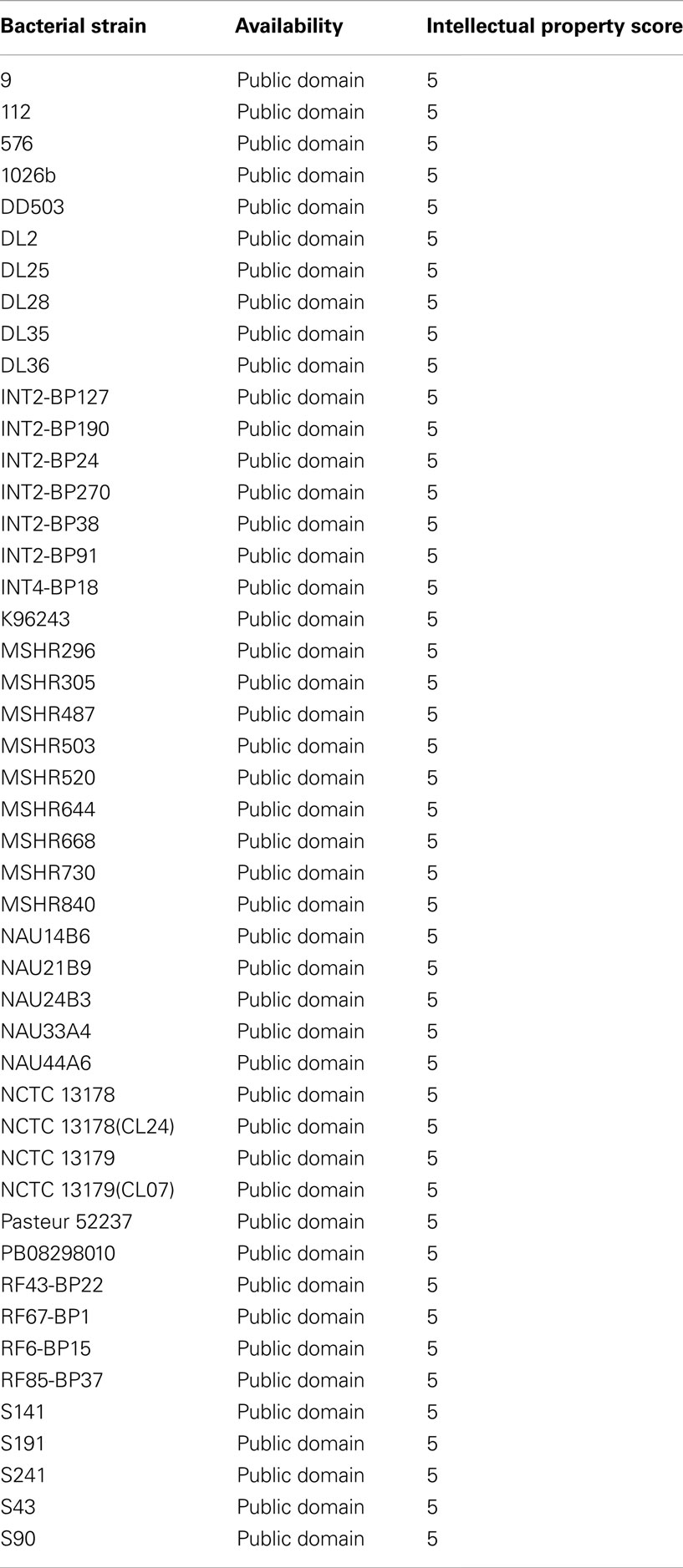
Strain Availability
Because an overarching objective of our B. pseudomallei research is to find common animal models that are acceptable to the FDA for Animal Rule research, common, well-characterized strains would ideally be made available to the B. pseudomallei research community. Therefore, we reviewed the legal constraints for individual B. pseudomallei strains in publicly available data and personnel communications. Strains were assigned a score on a scale of zero through five using the following six criteria. While the grading scale used encompassed five through zero, no score of three was assigned to increase the distinction between restricted and unrestricted strains.
0 points for no information identified
1 point for license required for use or distribution
2 points for MTA required
4 points for strains available through a collaborator’s collection without restriction
5 points for strains available in the public domain.
Many of the strains we investigated were available, and we identified 52 strains available in the public domain as listed in Table 5. Further discussion of availability of strains is beyond the scope of this review.
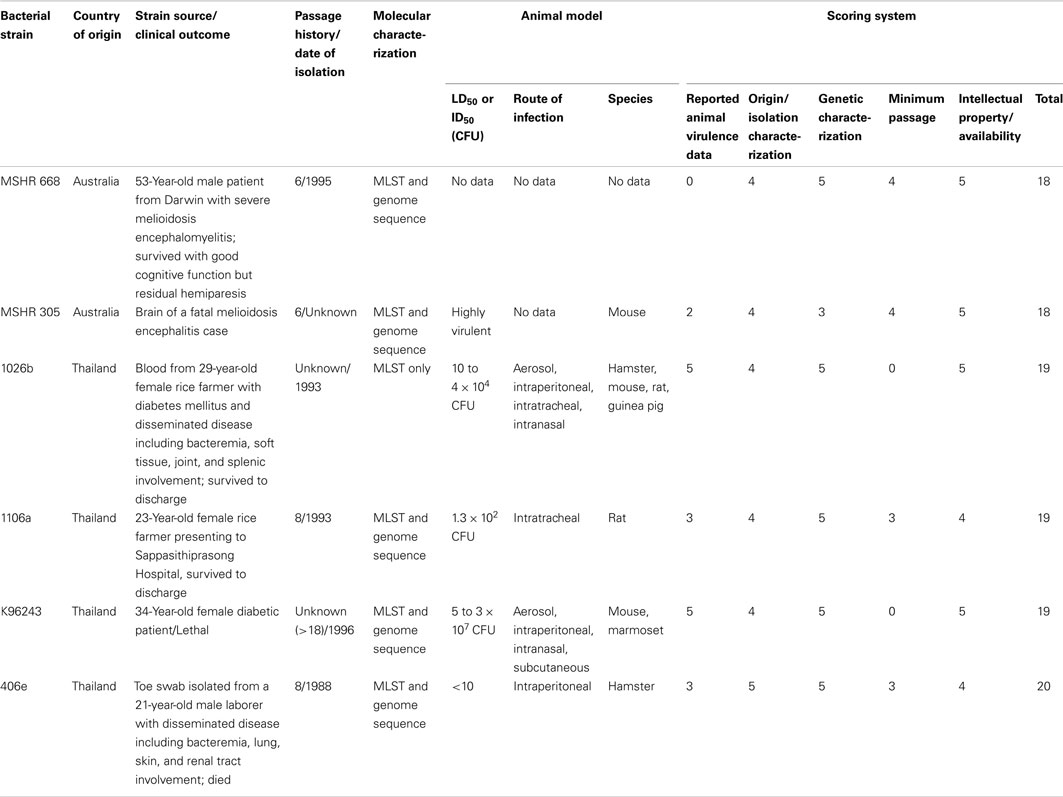
Panel Selection and Discussion
With the overall objective of creating a panel of well-characterized B. pseudomallei strains for use in animal model development, we totaled the scores for strain source, passage history, virulence, genotype, phenotype, and availability for each strain. We then selected the six strains with the highest scores to develop into a panel of B. pseudomallei reference strains, with the intention of using these strains to develop animal models (Table 6). The selected strains were 1026b, MSHR668, K96243, MSHR305, 1106a, and 406e. MSHR668 was isolated from a human encephalomyelitis case. Strain 1026b has been used extensively in animal infection models of melioidosis, is available in the public domain, and has a published annotated genome sequence. Furthermore, 1026b was isolated from a human case without pulmonary involvement. However, a low passage stock of 1026b was not located. Nonetheless, the extensive animal research conducted with 1026b as well as an annotated genome sequence makes it a good choice for the reference panel. While it was not isolated from a pulmonary presentation case and had no animal virulence data, the relatively low passage number, availability of genome sequence data, and availability to laboratories made MSHR668 a good choice for the reference panel. Strain K96243 is a well-studied laboratory strain of B. pseudomallei isolated from a human case. While this strain was not isolated from a pulmonary case and had an unknown passage history, it has sequence data and extensive mouse virulence data, including studies indicating a very low LD50. In addition, K96243 is readily available, making it a good choice for a panel of B. pseudomallei strains for animal models of melioidosis. MSHR305 was also isolated from a human encephalomyelitis case, but with low passage, MLST data and some animal virulence data in mice, this strain also may prove useful in animal models of melioidosis. Strain 1106a was isolated from a human case but details on pulmonary presentation were not available. However, the 1106a genome is sequenced and the intratracheal infection of rats resulted in a lethal disease. Furthermore, a low passage isolate could be obtained, making 1106a a good candidate for inclusion on the panel. Finally, 406e was isolated from a human case with pulmonary involvement, genome sequence data, a low LD50 in intraperitoneal infection of hamsters and the availability of a relatively low passage isolate made 406e the highest scoring B. pseudomallei strain in our literature review and a very good candidate for inclusion in a panel of reference strains for animal models of melioidosis. With these data, it is our intention to develop a set of cell banks to serve as a reference panel of B. pseudomallei strains for use in animal models of melioidosis.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We would like to acknowledge Dr. James Rogers and Dr. Matt Metz for critical reviews of this manuscript. This work was supported in part by funds from the Biomedical Advanced Research and Development Authority under Task Order HHSO10033001T of contract HHSO1002011000005I.
References
Chaowagul, W., Suputtamongkol, Y., Dance, D. A., Rajchanuvong, A., Pattara-arechachai, J., and White, N. J. (1993). Relapse in melioidosis: incidence and risk factors. J. Infect. Dis. 168, 1181–1185.
Currie, B. J., Fisher, D. A., Anstey, N. M., and Jacups, S. P. (2000). Melioidosis: acute and chronic disease, relapse and re-activation. Trans. R. Soc. Trop. Med. Hyg. 94, 301–304.
Currie, B. J., Thomas, A. D., Godoy, D., Dance, D. A., Cheng, A. C., Ward, L., Mayo, M., Pitt, T. L., and Spratt, B. G. (2007). Australian and Thai isolates of Burkholderia pseudomallei are distinct by multilocus sequence typing: revision of a case of mistaken identity. J. Clin. Microbiol. 45, 3828–3829.
Currie, B. J., Ward, L., and Cheng, A. C. (2010). The epidemiology and clinical spectrum of melioidosis: 540 cases from the 20 year Darwin prospective study. PLoS Negl. Trop. Dis. 4, e900. doi:10.1371/journal.pntd.0000900
Dannenberg, A. M. Jr., and Scott, E. M. (1958). Melioidosis: pathogenesis and immunity in mice and hamsters. I. Studies with virulent strains of Malleomyces pseudomallei. J. Exp. Med. 107, 153–166.
FDA. (ed.). (2009). Guidance for Industry Animal Models – Essential Elements to Address Efficacy Under the Animal Rule. Rockville, MD: F.a.D.A, U.S. Department of Health and Human Services, Center for Drug Evaluation and Research (CDER) & Center for Biologics Evaluation and Research (CBER).
Godoy, D., Randle, G., Simpson, A. J., Aanensen, D. M., Pitt, T. L., Kinoshita, R., and Spratt, B. G. (2003). Multilocus sequence typing and evolutionary relationships among the causative agents of melioidosis and glanders, Burkholderia pseudomallei and Burkholderia mallei. J. Clin. Microbiol. 41, 2068–2079.
Goodyear, A., Kellihan, L., Bielefeldt-Ohmann, H., Troyer, R., Propst, K., and Dow, S. (2009). Protection from pneumonic infection with Burkholderia species by inhalational immunotherapy. Infect. Immun. 77, 1579–1588.
Hayden, H. S., Lim, R., Brittnacher, M. J., Sims, E. H., Ramage, E. R., Fong, C., Wu, Z., Crist, E., Chang, J., Zhou, Y., Radey, M., Rohmer, L., Haugen, E., Gillett, W., Wuthiekanun, V., Peacock, S. J., Kaul, R., Miller, S. I., Manoil, C., and Jacobs, M. A. (2012). Evolution of Burkholderia pseudomallei in recurrent melioidosis. PLoS ONE 7, e36507. doi:10.1371/journal.pone.0036507
Holden, M. T., Titball, R. W., Peacock, S. J., Cerdeno-Tarraga, A. M., Atkins, T., Crossman, L. C., Pitt, T., Churcher, C., Mungall, K., Bentley, S. D., Sebaihia, M., Thomson, N. R., Bason, N., Beacham, I. R., Brooks, K., Brown, K., ABrown, N. F., Challis, G. L., Cherevach, I., Chillingworth, T., Cronin, A., Crossett, B., Davis, P., DeShazer, D., Feltwell, T., Fraser, A., Hance, Z., Hauser, H., Holroyd, S., Jagels, K., Keith, K. E., Maddison, M., Moule, S., Price, C., Quail, M. A., Rabbinowitsch, E., Rutherford, K., Sanders, M., Simmonds, M., Songsivilai, S., Stevens, K., Tumapa, S., Vesaratchavest, M., Whitehead, S., Yeats, C., Barrell, B. G., Oyston, P. C., and Parkhill, J. (2004). Genomic plasticity of the causative agent of melioidosis, Burkholderia pseudomallei. Proc. Natl. Acad. Sci. U.S.A. 101, 14240–14245.
Jeddeloh, J. A., Fritz, D. L., Waag, D. M., Hartings, J. M., and Andrews, G. P. (2003). Biodefense-driven murine model of pneumonic melioidosis. Infect. Immun. 71, 584–587.
Kaestli, M., Mayo, M., Harrington, G., Ward, L., Watt, F., Hill, J. V., Cheng, A. C., and Currie, B. J. (2009). Landscape changes influence the occurrence of the melioidosis bacterium Burkholderia pseudomallei in soil in northern Australia. PLoS Negl. Trop. Dis. 3, e364. doi:10.1371/journal.pntd.0000364
Leelayuwat, C., Romphruk, A., Lulitanond, A., Trakulsomboon, S., and Thamlikitkul, V. (2000). Genotype analysis of Burkholderia pseudomallei using randomly amplified polymorphic DNA (RAPD): indicative of genetic differences amongst environmental and clinical isolates. Acta Trop. 77, 229–237.
Limmathurotsakul, D., Wongratanacheewin, S., Teerawattanasook, N., Wongsuvan, G., Chaisuksant, S., Chetchotisakd, P., Chaowagul, W., Day, N. P., and Peacock, S. J. (2010). Increasing incidence of human melioidosis in Northeast Thailand. Am. J. Trop. Med. Hyg. 82, 1113–1117.
Liu, B., Koo, G. C., Yap, E. H., Chua, K. L., and Gan, Y. H. (2002). Model of differential susceptibility to mucosal Burkholderia pseudomallei infection. Infect. Immun. 70, 504–511.
McCombie, R. L., Finkelstein, R. A., and Woods, D. E. (2006). Multilocus sequence typing of historical Burkholderia pseudomallei isolates collected in Southeast Asia from 1964 to 1967 provides insight into the epidemiology of melioidosis. J. Clin. Microbiol. 44, 2951–2962.
Miller, W. R., Pannell, L., and Ingalls, M. S. (1948). Experimental chemotherapy in glanders and melioidosis. Am. J. Hyg. 47, 205–213.
Moore, R. A., DeShazer, D., Reckseidler, S., Weissman, A., and Woods, D. E. (1999). Efflux-mediated aminoglycoside and macrolide resistance in Burkholderia pseudomallei. Antimicrob. Agents Chemother. 43, 465–470.
Nelson, M., Dean, R. E., Salguero, F. J., Taylor, C., Pearce, P. C., Simpson, A. J., and Lever, M. S. (2011). Development of an acute model of inhalational melioidosis in the common marmoset (Callithrix jacchus). Int. J. Exp. Pathol. 92, 428–435.
Price, E. P., Hornstra, H. M., Limmathurotsakul, D., Max, T. L., Sarovich, D. S., Vogler, A. J., Dale, J. L., Ginther, J. L., Leadem, B., Colman, R. E., Foster, J. T., Tuanyok, A., Wagner, D. M., Peacock, S. J., Pearson, T., and Keim, P. (2010). Within-host evolution of Burkholderia pseudomallei in four cases of acute melioidosis. PLoS Pathog. 6, e1000725. doi:10.1371/journal.ppat.1000725
Sanford, D. C., Pak, D., Fisher, D. A., and Xu, Z. (2010). “Characterization of the rodent aerosol exposure system for delivery of Burkholderia pseudomallei and determination of the inhaled median lethal dose (LD50) in BALB/c mice,” in American Society for Microbiology Biodefense and Emerging Diseases Research Meeting, Baltimore.
Tan, G. Y., Liu, Y., Sivalingam, S. P., Sim, S. H., Wang, D., Paucod, J. C., Gauthier, Y., and Ooi, E. E. (2008). Burkholderia pseudomallei aerosol infection results in differential inflammatory responses in BALB/c and C57Bl/6 mice. J. Med. Microbiol. 57, 508–515.
Tuanyok, A., Leadem, B. R., Auerbach, R. K., Beckstrom-Sternberg, S. M., Beckstrom-Sternberg, J. S., Mayo, M., Wuthiekanun, V., Brettin, T. S., Nierman, W. C., Peacock, S. J., Currie, B. J., Wagner, D. M., and Keim, P. (2008). Genomic islands from five strains of Burkholderia pseudomallei. BMC Genomics 9, 566. doi:10.1186/1471-2164-9-566
Ulett, G. C., Currie, B. J., Clair, T. W., Mayo, M., Ketheesan, N., Labrooy, J., Gal, D., Norton, R., Smith, C. A., Barnes, J., Warner, J., and Hirst, R. G. (2001). Burkholderia pseudomallei virulence: definition, stability, and association with clonality. Microbes Infect. 3, 621–631.
U’Ren, J. M., Schupp, J. M., Pearson, T., Hornstra, H., Friedman, C. L., Smith, K. L., Daugherty, R. R., Rhoton, S. D., Leadem, B., Georgia, S., Cardon, M., Huynh, L. Y., DeShazer, D., Harvey, S. P., Robison, R., Gal, D., Mayo, M. J., Wagner, D., Currie, B. J., and Keim, P. (2007). Tandem repeat regions within the Burkholderia pseudomallei genome and their application for high resolution genotyping. BMC Microbiol. 7, 23. doi:10.1186/1471-2180-7-23
Keywords: pseudomallei, aerosol, biodefense, animal models, virulence, genome, sequencing, passage history
Citation: Van Zandt KE, Tuanyok A, Keim PS, Warren RL and Gelhaus HC (2012) An objective approach for Burkholderia pseudomallei strain selection as challenge material for medical countermeasures efficacy testing. Front. Cell. Inf. Microbio. 2:120. doi: 10.3389/fcimb.2012.00120
Received: 05 June 2012; Accepted: 29 August 2012;
Published online: 26 September 2012.
Edited by:
Mark Estes, University of Georgia, USAReviewed by:
Mark Estes, University of Georgia, USALisa A. Morici, Tulane University School of Medicine, USA
Copyright: © 2012 Van Zandt, Tuanyok, Keim, Warren and Gelhaus. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits use, distribution and reproduction in other forums, provided the original authors and source are credited and subject to any copyright notices concerning any third-party graphics etc.
*Correspondence: H. Carl Gelhaus, Battelle, Battelle Biomedical Research Center, 505 King Avenue, JM-7, Columbus, OH 43201-2693, USA. e-mail: gelhaush@battelle.org
†Present address: Richard L. Warren, 375 E Street, S. W., Patriot Plaza II, Room 12-3711, Washington, DC 20024, USA.