Lung recruitment can improve oxygenation in patients ventilated in continuous positive airway pressure/pressure support mode
- Department of Anaesthesiology and Intensive Therapy, Faculty of Medicine, University of Szeged, Szeged, Hungary
Background: Recruitment maneuvers are often used in critical care patients with hypoxemic respiratory failure. Although continuous positive airway pressure/pressure support (CPAP/PS) ventilation is a frequently used approach, but whether lung recruitment also improves oxygenation in spontaneously breathing patients has not been investigated yet. The primary objective was to analyze the effect of recruitment maneuver on oxygenation in patients ventilated in CPAP/PS mode.
Methods: Following baseline measurements PEEP was increased by 5 cmH2O. Recruitment maneuver was applied for 40 s with 40 cmH2O of PS. Measurements of the difference in PaO2/FiO2 and airway parameters measured by the ventilator were recorded immediately after recruitment then 15 and 30 min later. Thirty patients ventilated in CPAP/PS mode with a PEEP ≥5 cmH2O were enrolled in this prospective, observational study if their PaO2/FiO2 ratio was <300 mmHg or required an FiO2 >0.5.
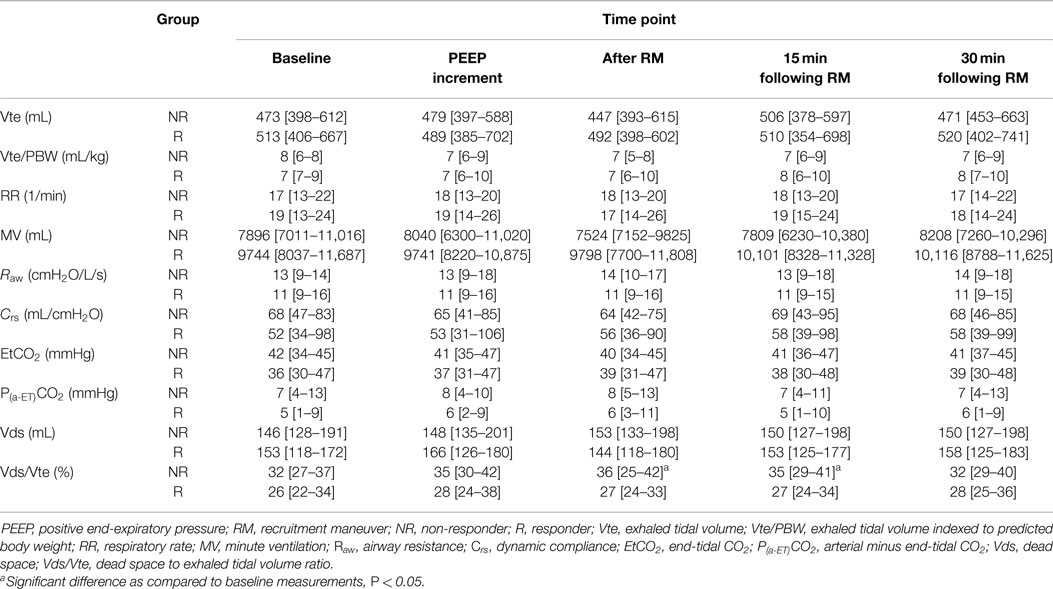
Results: Following recruitment maneuver patients were considered as non-responders (NR, n = 15) if difference of PaO2/FiO2 <20% and responders (R, n = 15) if difference of PaO2/FiO2 ≥20%. In the NR-group, PaO2/FiO2 decreased non-significantly from baseline: median [interquartile], PaO2/FiO2 = 176 [120–186] vs. after recruitment: 169 [121–182] mmHg, P = 0.307 while in the R-group there was significant improvement: 139 [117–164] vs. 230 [211–323] mmHg, P = 0.01. At the same time points, dead space to tidal volume ratio (Vds/Vte) significantly increased in the NR-group Vds/Vte = 32 [27–37] vs. 36 [25–42]%, P = 0.013 but no significant change was observed in the R-group: 26 [22–34] vs. 27 [24–33]%, P = 0.386.
Conclusion: Recruitment maneuver improved PaO2/FiO2 ratio by ≥20% in 50% of patients ventilated in CPAP/PS mode.
Introduction
Hypoxemic respiratory failure is one of the leading causes of the need for mechanical ventilation and can occur in several conditions, most often as a result of heart failure, pneumonia, and sepsis. Its most severe form is acute respiratory distress syndrome (ARDS), which still carries high risk of mortality (1). Applying increased level of PEEP (2), prone positioning (3), and lung recruitment (4) are all recommended measures to improve oxygenation and gas exchange in general.
One of the main reasons of hypoxemia, characterized by low partial arterial oxygen tension/fraction of inspired oxygen (PaO2/FiO2), is diffuse atelectasis of the alveoli (5). Therefore, resolving atelectatic lung areas could reduce intrapulmonary shunt and venous admixture and hence improve oxygenation (6). This can be achieved by applying increased intrathoracic pressures for a short period of time and keep the alveoli open by titrating the adequate level of PEEP. This procedure of opening up atelectatic alveoli and keep them open is called as the “open lung concept” (7). However, it is also well known that not every lung responds for recruitment maneuvers (8). Although most recruitment strategies were tested under controlled mechanical ventilation (9), there is also increasing evidence that maintaining spontaneous breathing during mechanical ventilation may provide advantageous ventilation/perfusion ratio and prevents alveolar shearing (6, 10). Applying continuous positive airway pressure (CPAP) with or without pressure support (PS) and allowing the patient to breathe spontaneously is an often used ventilation mode, both during non-invasive and invasive ventilation. Although theoretically alveolar recruitment may also have a place in these patients ventilated invasively this has only been investigated during non-invasive ventilation (11). Sophisticated methods of assessing lung recruitment, like computer tomography (CT) scanning, esophageal pressure measurements, etc., are rarely available in the everyday routine in most countries and these are especially difficult to perform in spontaneously breathing patients (12). Nevertheless, one of the benefits of effective recruitment is improved oxygenation after the maneuver. Therefore, the purpose of the current study was to investigate the effects of recruitment on the PaO2/FiO2 ratio in patients ventilated in CPAP/PS mode suffering from moderate and severe hypoxemic respiratory failure.
Materials and Methods
Patients
Following ethics committee approval of the Human Investigation Review Board of University of Szeged, informed consent was obtained from the patients’ next of kin. All mechanically ventilated patients with maintained spontaneous breathing, ventilated in CPAP/PS mode with a PEEP ≥5 cmH2O, were enrolled in this prospective, observational study if their PaO2/FiO2 ratio <300 mmHg or required an FiO2 >0.5, regardless of the etiology of respiratory failure (13, 14). Exclusion criteria were age <18, pregnancy, pulmonectomy/lobectomy, or spontaneous pneumothorax in past-medical history, emphysematous bullae, clinically diagnosed end stage chronic obstructive pulmonary disease, and vasopressor refractory hemodynamic instability.
Measurements and Experimental Protocol
All patients who were eligible for the study had a radial arterial and an internal jugular or subclavian central venous catheter inserted on admission to the intensive care unit as part of our standard care. Patients were sedated with continuous infusion of propofol and fentanyl reaching a Richmond Agitation Sedation Scale score of −1 to −2. Electrocardiogram, invasive blood pressure, and SpO2 were continuously monitored by Dräger Infinity Gamma XL Monitor (Telford, PA, USA). Patients were ventilated with Dräger Evita® XL respirators (Lübeck, Germany). The level of PS was adjusted to achieve adequate arterial pCO2 level to maintain pH ≥7.30. Respiratory parameters, airway pressures, dynamic respiratory compliance, airway resistance, end-tidal carbon dioxide (EtCO2), dead space (Vds), and dead space to exhaled tidal volume ratio (Vds/Vte) were all continuously monitored by the respirator and its own volumetric capnography.
Once inclusion criteria were fulfilled respirator settings, cardio-respiratory and airway parameters were recorded at baseline. Then PEEP was increased by 5 cmH2O and after 5 min measurements were repeated to investigate the effect of any PEEP-induced recruitment. For alveolar recruitment, PS was increased to 40 cmH2O for 40 s to limit the undesirable side effects of volutrauma. After which peak inspiratory pressure was reduced to the initial value as at baseline while maintaining the increased level of PEEP (by 5 cmH2O) according to the open lung concept (7). Measurements were repeated immediately after recruitment then 15 and 30 min later with constant respirator settings as at baseline. Arterial blood gas samples were analyzed by a Roche cobas b 221 (Mannheim, Germany) blood gas system at each measurement points and central venous samples were taken at baseline and at the final time point to determine central venous oxygen saturation (ScvO2).
Primary outcome parameter was the change in oxygenation (PaO2/FiO2) after the recruitment maneuver. Patients were considered as non-responders (NR) if difference of PaO2/FiO2 <20% and responders (R) if difference of PaO2/FiO2 ≥20% between baseline and following recruitment measurements.
Statistics
Based on a preliminary analysis of our data (15), the mean PaO2/FiO2 ratio before recruitment was 156 mmHg with a SD of 43 mmHg. In order the study to have an 80% power with a P < 0.05 and to observe an increase in the PaO2/FiO2 of 10 or 20% (which corresponds to a PaO2/FiO2 of 171 and 186 mmHg, respectively) after recruitment, the required minimal sample size was calculated to be 51 or 13. Therefore, we decided that a sample size of 30 should be feasible and provide adequate statistical power.
All data in the tables are presented as median [interquartile range]. Figures are presented as boxplots: 5th–95th percentile, interquartile range, and median. After testing for normality with Shapiro–Wilk test data were analyzed between groups with Mann–Whitney U test or Kruskal–Wallis test as suitable. Matched pairs were investigated with Wilcoxon signed rank test and relationship was analyzed with Spearman’s correlation coefficient. For evaluating goodness of fit and independence, Pearson’s chi-square test was used. The “P” value was considered significant if <0.05. For statistical analysis, IBM SPSS Statistics Version 20 (Armonk, NY, USA) software was used.
Results
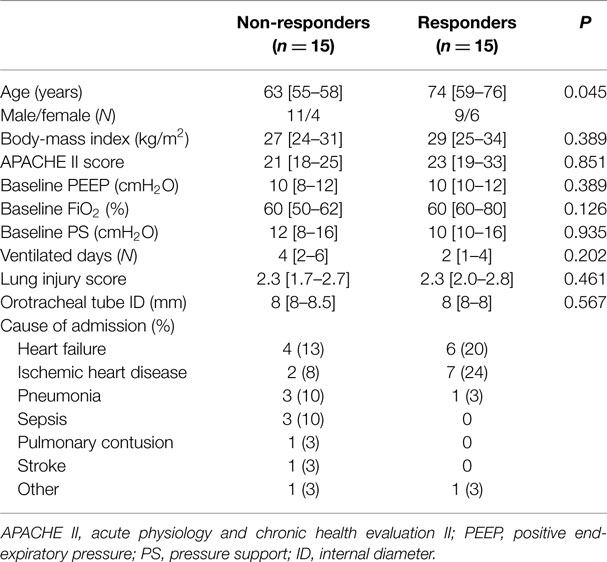
Over the study period 30 patients were enrolled, of whom 15 (50%) patients turned out to be NR and 15 (50%) responders. There was no significant difference between groups in baseline respirator settings and demographic characteristics except of age. Out of the 19 patients with admission diagnosis of cardiac origin 13 (68%) were responders (Table 1). Serious adverse effects of recruitment maneuver like pneumothorax and worsening hemodynamic instability were not detected.
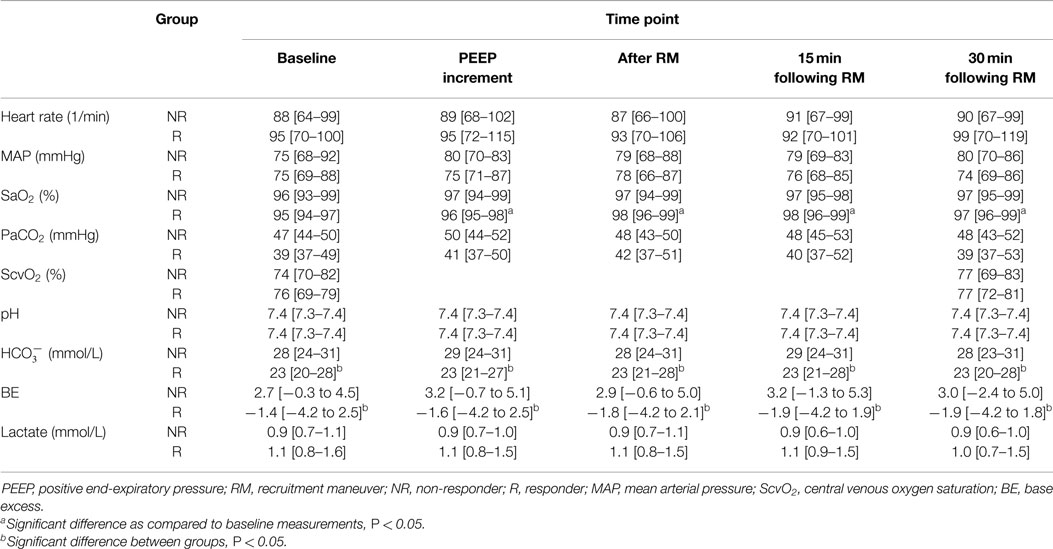
There was a non-significant decrease in PaO2/FiO2 from baseline to 30 min following recruitment in the NR-group. In the R-group, PaO2/FiO2 significantly improved after the recruitment maneuver as compared to baseline results and remained elevated throughout the observation period. There was significant improvement in SaO2 among responders, while there was no significant change in the NR-group. Bicarbonate and base excess levels showed significant difference between groups at all time points. Hemodynamic parameters and ScvO2 did not show any significant change over time (Table 2; Figure 1).
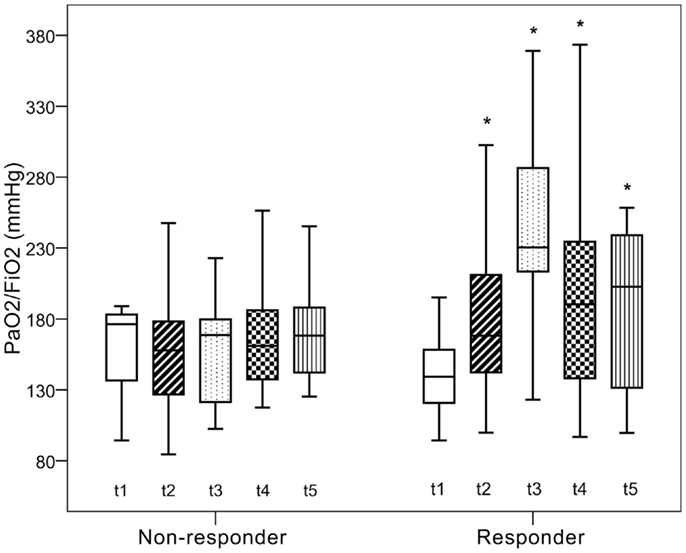
Figure 1. Changes in PaO2/FiO2. t0, baseline measurements; t1, increasing PEEP by 5 cmH2O; t2, after recruitment; t3 and t4, 15 and 30 min after recruitment. *Significant difference as compared to baseline measurements, P < 0.05.
There was no significant change in tidal volume, Vte indexed for predicted bodyweight, respiratory rate, and minute ventilation between groups and throughout the study as compared to baseline parameters. In the NR-group dynamic compliance, a parameter indicated on the ventilator dropped non-significantly after the recruitment maneuver but there was a significant increase in Vds/Vte following recruitment and 15 min later as compared to baseline in the same group. There was no other significant change in the examined respiratory and airway parameters in the NR- and R-group (Table 3).
Improvement in oxygenation was detected in 74% of all patients, and in 26% arterial oxygenation did not improve or even deteriorated. Testing in a contingency table the change in PaO2/FiO2 and dynamic compliance after the recruitment maneuver is shown in Figure 2. Improvement (≥0) or deterioration (<0) of dynamic compliance gave high sensitivity and specificity with a positive predictive value of 0.89 to differentiate patients with worsening as compared to those with improved PaO2/FiO2.
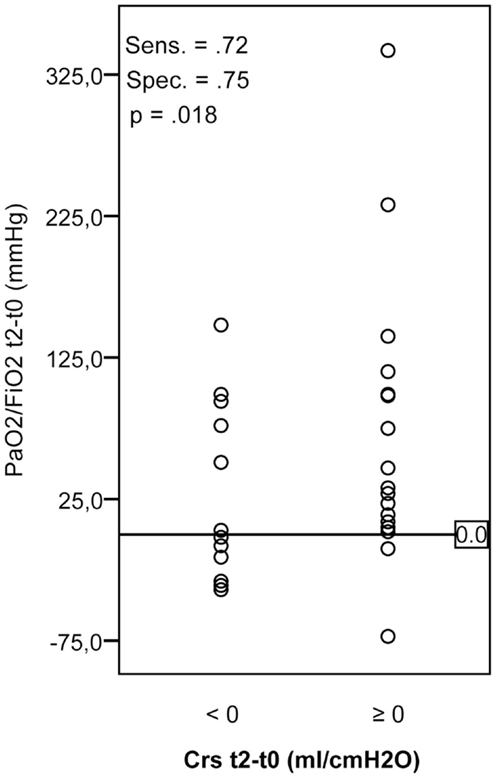
Figure 2. Changes in PaO2/FiO2 and dynamic compliance after recruitment maneuver as compared to baseline parameters. Crs, dynamic compliance, Sens., sensitivity; Spec., specificity.
Discussion
The most important finding of this study is that recruitment maneuver improved oxygenation by more than 20% in half of the patients with moderate and severe hypoxemic respiratory failure ventilated in CPAP/PS mode. We also found that patients in whom hypoxemia was due to cardiac origin seemed to benefit the most, as nearly 70% of these patients were found to be responders.
Patients, according to the change in the PaO2/FiO2 ratio after recruitment, were divided to non-responder and responder groups. Regarding the demographic data, it is an interesting finding that patients in the NR-group were significantly younger than those in the R-group. There were also more patients with ischemic heart disease and heart failure in the R-group, while there were only four patients with heart failure in the NR-group. One of the possible explanations is that although lung compliance decreases with age in general but success of recruitment depends on other factors like co-morbidities and it may be more successful in patients with heart disease as compared to patients with pneumonia. The beneficial effects of PEEP-induced alveolar recruitment with improved compliance and oxygenation are well known phenomenon in patients with ischemic heart disease (16). PEEP can also decrease intrapulmonary shunt such as hypoxic pulmonary vasoconstriction with a reduced pulmonary artery pressure among patients with heart failure (17). Therefore, it is not the age per se but the accompanying higher number of patients with heart condition that caused the observed difference in the current study. Our results draw the attention of the importance of the etiology of acute lung injury and co-morbidities, at least as far as improvement in oxygenation is concerned after the recruitment maneuver. These results are also in accord with those reported in patients on controlled mechanical ventilation (18) but it also contradicts those in which etiology did not seem to matter (19). However, in this recent study by Grasso et al., the sample size was small (11/group) and none of the patients were admitted due to acute heart failure. Nevertheless, the success of recruitment as far as oxygenation is concerned in spontaneously breathing patients having developed hypoxemic respiratory failure due to acute heart failure is an important finding and should be investigated further.
Although it is not the most accurate way to assess lung recruitment, but measuring changes in arterial oxygenation is one of the commonly used methods to detect the efficacy of recruitment (20, 21). Furthermore, there is no consensus on how to define responders and NR based on the PaO2/FiO2 values, which vary between 30 and 50% in the literature (19, 22). Due to the lack of well-defined values, we have chosen an arbitrary threshold of difference in PaO2/FiO2 ≥20% to define as responders and <20% as NR following recruitment. Nevertheless, we detected an improvement of oxygenation in 74% of all patients, and in 26% arterial oxygenation did not improve or even deteriorated. Taking the 20% improvement in oxygenation as a clinically significant change, 50% of patients still responded, which is similar to that of reported in recently published studies (23, 24). However, it is important to note that the ratio of responders is highly dependent on the defined threshold. Furthermore, the improvement in arterial oxygenation among responders lasted longer than in studies where controlled ventilation was applied. In the investigation by Oczenski et al., after the initial improvement, PaO2/FiO2 returned to the baseline values after 30 min (25) while in our trial the significant improvement in oxygenation persisted throughout, suggesting that the effects of recruitment may last longer in spontaneous assisted modes as compared to controlled modes of ventilation in hypoxemic respiratory failure. Although the sample size is too small for an outcome study, which holds true for all of the above mentioned investigations, but our data suggest that CPAP/PS ventilation and lung recruitment may have benefits in patients suffering from moderate to severe acute lung injury, especially due to acute heart failure, which should be investigated further.
It may also be important to note, that prior to intervention patients were ventilated for a median of 4 days in the NR-group while it was only 2 days in the R-group. Although it was not statistically significant, but these results are similar to that of reported by Grasso et al., where the length of mechanical ventilation was significantly shorter in those patients who responded for recruitment maneuvers (19).
It is well known that not every lung responds for recruitment and unnecessary maneuvers may lead to adverse effects (8, 26). Several methods had been evaluated of which chest CT scan remains the gold standard warranting the direct visualization of the recruitable lung tissue (8). However, this method requires the transport of the critically ill patients to the CT scanner and exposes them to radiation (27). Other bed-side measurements to assess recruitability are pressure–volume curve assessment and end-expiratory lung volume/functional residual capacity ratio measurement (28, 29). Unfortunately, due to financial and ethical reasons, these methods were not applied in our study therefore we only have limited proof on the change in lung volume after the recruitment.
We did not observe any significant change neither in the PaCO2 nor in any other blood gas variables throughout the study. However, there was a significant difference in bicarbonate and base excess levels between groups this observation had no effect on the investigation of recruitment. One of the potential alternatives for assessing alveolar recruitment may be the change in the difference between the arterial and end-tidal CO2 (Pa-ETCO2) (30). In our study, Pa-ETCO2 although did not change significantly over time in neither of the groups but in the R-group its value was lower than in the NR-group. Therefore, it may be a promising parameter but its relevance requires further studies.
Another important parameter is compliance, which is determined by volume/pressure relationships. Theoretically, in recruitable patients increasing pressures will increase volume hence compliance should improve or remain unchanged. While in non-recruitable patients increased pressures during recruitment can lead to the overdistension without gaining lung volumes, hence result in a consecutive fall in respiratory compliance (31). Although, in a recent study by Oczenski et al., in patients with ARDS who were ventilated in controlled mode and underwent recruitment after a PEEP trial there was no significant change in compliance 3 min after the maneuver what was accompanied by a significant improvement in oxygenation (25). This approach cannot be evaluated in our study as the value of the ventilator indicated compliance in spontaneously breathing patients has not been validated yet.
Finally, hemodynamic changes during the recruitment maneuver have been widely investigated (32, 33). Although we did not apply advanced hemodynamic monitoring in this study but as far as heart rate, mean arterial pressure, lactate, and ScvO2 are concerned there was no significant change after the recruitment procedure as compared to baseline therefore it is likely that patients remained hemodynamically stable, suggesting that performing recruitment maneuver in CPAP/PS ventilation is a safe strategy in patients with severe acute respiratory failure.
Limitations
There are several limitations of our study. In the absence of lung CT scans, recruitment and the degree of the recruited lung area cannot be estimated. Although the investigation of Gattinoni et al. still remains the reference method to assess lung recruitment (8) we considered it difficult to be accepted ethically because of the potential dangers of transport and radiation. Furthermore, esophageal and herewith transpulmonary pressures were not monitored therefore we could not conclude if pleural pressure was swinging in spontaneously breathing patients hereby producing different recruitment effects during the time course of the maneuver. Finally, neither the sample size, which was too small, nor the protocol (with one single recruitment maneuver only) allowed us to draw any conclusion regarding hard clinical end-points such as ventilator free days, length of stay or outcome. However, based on the current findings, a study designed to answer these questions is certainly warranted. Nevertheless, the significant tendency what we observed has never been reported before and these preliminary results may provide important information for those who are interested in applying spontaneous assisted/supported modes of ventilation for patients with severe acute respiratory failure.
Conclusion
Alveolar recruitment maneuver can improve oxygenation in patients suffering from moderate and severe acute hypoxemic respiratory failure and ventilated in CPAP/PS mode as indicated by the significant improvement in oxygenation after recruitment in 74% of all patients. The decrease in dynamic compliance as displayed on the ventilator after the recruitment maneuver proved to be a simple bed-side indicator of failure in improving oxygenation in spontaneously breathing patients.
Author Note
The results of this investigation were presented as a poster at the 35th International Symposium on Intensive Care and Emergency Medicine.
Author Contributions
ZM and AL designed the trial, interpreted the results, and drafted the manuscript. MN gave substantial contributions to the conception and design of the study. AL carried out the statistical analysis. AL, MN, and DT participated in coordination and have made substantial contributions to analysis of data. AL, MN, and DT contributed with data collection and ZM, AL, MN and DT assisted in the critical revision of the manuscript. All authors have read and approved the final version of the manuscript.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Eastwood G, Bellomo R, Bailey M, Taori G, Pilcher D, Young P, et al. Arterial oxygen tension and mortality in mechanically ventilated patients. Intensive Care Med (2012) 38:91–8. doi:10.1007/s00134-011-2419-6
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
2. Briel M, Meade M, Mercat A, Brower RG, Talmor D, Walter SD, et al. Higher vs lower positive end-expiratory pressure in patients with acute lung injury and acute respiratory distress syndrome: systematic review and meta-analysis. JAMA (2010) 303:865–73. doi:10.1001/jama.2010.218
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
3. Guérin C, Reignier J, Richard JC, Beuret P, Gacouin A, Boulain T, et al. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med (2013) 368:2159–68. doi:10.1056/NEJMoa1214103
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
4. Suzumura EA, Figueiró M, Normilio-Silva K, Laranjeira L, Oliveira C, Buehler AM, et al. Effects of alveolar recruitment maneuvers on clinical outcomes in patients with acute respiratory distress syndrome: a systematic review and meta-analysis. Intensive Care Med (2014) 40:1227–40. doi:10.1007/s00134-014-3413-6
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
5. Cortés I, Peñuelas O, Esteban A. Acute respiratory distress syndrome: evaluation and management. Minerva Anestesiol (2012) 78:343–57.
6. Vimlati L, Kawati R, Hedenstierna G, Larsson A, Lichtwarck-Aschoff M. Spontaneous breathing improves shunt fraction and oxygenation in comparison with controlled ventilation at a similar amount of lung collapse. Anesth Analg (2011) 113:1089–95. doi:10.1213/ANE.0b013e31822ceef8
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
7. Lachman B. Open up the lung and keep the lung open. Intensive Care Med (1992) 18:319–21. doi:10.1007/BF01694358
8. Gattinoni L, Caironi P, Cressoni M, Chiumello D, Ranieri VM, Quintel M, et al. Lung recruitment in patients with the acute respiratory distress syndrome. N Engl J Med (2006) 354:1775–86. doi:10.1056/NEJMoa052052
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
9. Sassoon CS, Zhu E, Caiozzo VJ. Assist-control mechanical ventilation attenuates ventilator-induced diaphragmatic dysfunction. Am J Respir Crit Care Med (2004) 170:626–32. doi:10.1164/rccm.200401-042OC
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
10. Putensen C, Muders T, Varelmann D, Wrigge H. The impact of spontaneous breathing during mechanical ventilation. Curr Opin Crit Care (2006) 12:13–8. doi:10.1097/01.ccx.0000198994.37319.60
11. Cammarota G, Vaschetto R, Turucz E, Dellapiazza F, Colombo D, Blando C, et al. Influence of lung collapse distribution on the physiologic response to recruitment maneuvers during noninvasive continuous positive airway pressure. Intensive Care Med (2011) 37:1095–102. doi:10.1007/s00134-011-2239-8
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
12. Brochard L, Martin GS, Blanch L, Pelosi P, Belda FJ, Jubran A, et al. Clinical review: respiratory monitoring in the ICU – a consensus of 16. Crit Care (2012) 16:219. doi:10.1186/cc11146
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
13. Murray JF, Matthay MA, Luce JM, Flick MR. An expanded definition of the adult respiratory distress syndrome. Am Rev Respir Dis (1988) 138:720–3. doi:10.1164/ajrccm/138.3.720
14. Ferguson ND, Fan E, Camporota L, Antonelli M, Anzueto A, Beale R, et al. The Berlin definition of ARDS: an expanded rationale, justification, and supplementary material. Intensive Care Med (2012) 38:1573–82. doi:10.1007/s00134-012-2682-1
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
15. Lovas A, Trasy D, Nemeth M, Laszlo I, Molnar Z. Effect of lung recruitment on oxygenation in patients with acute lung injury ventilated in CPAP/pressure support mode. Crit Care (2015) 19:226. doi:10.1186/cc14306
16. Wiesen J, Ornstein M, Tonelli AR, Menon V, Ashton RW. State of the evidence: mechanical ventilation with PEEP in patients with cardiogenic shock. Heart (2013) 99:1812–7. doi:10.1136/heartjnl-2013-303642
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
17. Pinsky MR. Cardiovascular issues in respiratory care. Chest (2005) 128:592S–7S. doi:10.1378/chest.128.5_suppl_2.592S
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
18. Rocco PR, Pelosi P. Pulmonary and extrapulmonary acute respiratory distress syndrome: myth or reality? Curr Opin Crit Care (2008) 14:50–5. doi:10.1097/MCC.0b013e3282f2405b
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
19. Grasso S, Mascia L, Del Turco M, Malacarne P, Giunta F, Brochard L, et al. Effects of recruiting maneuvers in patients with acute respiratory distress syndrome ventilated with protective ventilatory strategy. Anesthesiology (2002) 96:795–802. doi:10.1097/00000542-200204000-00005
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
20. Esan A, Hess DR, Raoof S, George L, Sessler CN. Severe hypoxemic respiratory failure: part 1 – ventilatory strategies. Chest (2010) 137:1203–16. doi:10.1378/chest.09-2415
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
21. Schreiter D, Reske A, Stichert B, Seiwerts M, Bohm SH, Kloeppel R, et al. Alveolar recruitment in combination with sufficient positive end-expiratory pressure increases oxygenation and lung aeration in patients with severe chest trauma. Crit Care Med (2004) 32:968–75. doi:10.1097/01.CCM.0000120050.85798.38
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
22. Reutershan J, Schmitt A, Dietz K, Unertl K, Fretschner R. Alveolar recruitment during prone position: time matters. Clin Sci (Lond) (2006) 110:655–63. doi:10.1042/CS20050337
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
23. Di Marco F, Devaquet J, Lyazidi A, Galia F, da Costa NP, Fumagalli R, et al. Positive end-expiratory pressure-induced functional recruitment in patients with acute respiratory distress syndrome. Crit Care Med (2010) 38:127–32. doi:10.1097/CCM.0b013e3181b4a7e7
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
24. Huh JW, Hong SB, Lim CM, Koh Y. Effect of the alveolar recruitment manoeuvre on haemodynamic parameters in patients with acute respiratory distress syndrome: relationship with oxygenation. Respirology (2010) 15:1220–5. doi:10.1111/j.1440-1843.2010.01852.x
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
25. Oczenski W, Hörmann C, Keller C, Lorenzl N, Kepka A, Schwarz S. Recruitment maneuvers after a positive end-expiratory pressure trial do not induce sustained effects in early adult respiratory distress syndrome. Anesthesiology (2004) 101:620–5. doi:10.1097/00000542-200409000-00010
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
26. Dueck R. Alveolar recruitment versus hyperinflation: a balancing act. Curr Opin Anaesthesiol (2006) 19:650–4. doi:10.1097/ACO.0b013e328011015d
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
27. Waydhas C. Intrahospital transport of critically ill patients. Crit Care (1999) 3:R83–9. doi:10.1186/cc362
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
28. Patroniti N, Bellani G, Cortinovis B, Foti G, Maggioni E, Manfio A, et al. Role of absolute lung volume to assess alveolar recruitment in acute respiratory distress syndrome patients. Crit Care Med (2010) 38:1300–7. doi:10.1097/CCM.0b013e3181d8cb51
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
29. Dellamonica J, Lerolle N, Sargentini C, Beduneau G, Di Marco F, Mercat A, et al. PEEP-induced changes in lung volume in acute respiratory distress syndrome. Two methods to estimate alveolar recruitment. Intensive Care Med (2011) 37:1595–604. doi:10.1007/s00134-011-2333-y
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
30. Blanch L, Fernández R, Benito S, Mancebo J, Net A. Effect of PEEP on the arterial minus end-tidal carbon dioxide gradient. Chest (1978) 92:451–4. doi:10.1378/chest.92.3.451
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
31. Schumann S, Vimlati L, Kawati R, Guttmann J, Lichtwarck-Aschoff M. Analysis of dynamic intratidal compliance in a lung collapse model. Anesthesiology (2011) 114:1111–7. doi:10.1097/ALN.0b013e31820ad41b
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
32. Toth I, Leiner T, Mikor A, Szakmany T, Bogar L, Molnar Z. Hemodynamic and respiratory changes during lung recruitment and descending optimal positive end-expiratory pressure titration in patients with acute respiratory distress syndrome. Crit Care Med (2007) 35:787–93. doi:10.1097/01.CCM.0000257330.54882.BE
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
33. Villagrá A, Ochagavía A, Vatua S, Murias G, Del Mar Fernández M, Lopez Aguilar J, et al. Recruitment maneuvers during lung protective ventilation in acute respiratory distress syndrome. Am J Respir Crit Care Med (2002) 165:165–70. doi:10.1164/ajrccm.165.2.2104092
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
Keywords: capnography, CPAP ventilation, lung compliance, lung recruitment, positive end-expiratory pressure
Citation: Lovas A, Németh MF, Trásy D and Molnár Z (2015) Lung recruitment can improve oxygenation in patients ventilated in continuous positive airway pressure/pressure support mode. Front. Med. 2:25. doi: 10.3389/fmed.2015.00025
Received: 13 February 2015; Accepted: 05 April 2015;
Published: 21 April 2015
Edited by:
Takashi Tagami, Nippon Medical School, JapanReviewed by:
Vsevolod V. Kuzkov, Northern State Medical University, RussiaPieter Roel Tuinman, VU Medical Center, Netherlands
Copyright: © 2015 Lovas, Németh, Trásy and Molnár. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zsolt Molnár, Department of Anaesthesiology and Intensive Therapy, Faculty of Medicine, University of Szeged, Semmelweis Utca 6, Szeged 6722, Hungary zsoltmolna@gmail.com
 András Lovas
András Lovas Márton Ferenc Németh
Márton Ferenc Németh Domonkos Trásy
Domonkos Trásy Zsolt Molnár
Zsolt Molnár