- 1Department of Microbiology, Faculty of Science, Prince of Songkla University, Hat Yai, Thailand
- 2Department of Internal Medicine, Faculty of Medicine, Prince of Songkla University, Hat Yai, Thailand
- 3Department of Parasitology, Faculty of Medicine, University of Malaya, Kuala Lumpur, Malaysia
Toxoplasmosis is one of the most common opportunistic parasitic diseases in patients living with HIV/AIDS. This study aimed to determine the seroprevalence of Toxoplasma infection in HIV-infected patients and to identify associated risk factors in Toxoplasma seropositive patients. This study was conducted at a regional public hospital in Hat Yai, southern Thailand during October 2009 to June 2010. Blood samples were collected from 300 HIV-infected patients. Each subject also answered a socio-demographic and risk factors associated with Toxoplasma infection. The prevalence of anti-Toxoplasma IgG antibodies in HIV-infected patients was 109 (36.3%), of which 83 (76.2%) had past infection and 26 (23.9%) had recently acquired Toxoplasma infection as indicated by their IgG avidity. Multivariate analysis using logistic regression showed that gender difference (adjusted OR = 1.69, 95% CI = 1.05–2.72) was the only factor associated with Toxoplasma infection. From the results obtained, these HIV-infected patients could be at high risk of developing clinical evidence of severe toxoplasmosis. Therefore, it is necessary to introduce primary behavioral practices to prevent Toxoplasma infection among HIV-infected patients.
Introduction
Toxoplasmosis is a clinical and/or pathological evidence of a disease caused by Toxoplasma gondii, an obligate intracellular protozoan parasite. Toxoplasma infection affects about one-third of the world population but the majority of infected individuals are asymptomatic (Montoya and Liesenfeld, 2004). In people who are living with HIV/AIDS, there is an increased risk of reactivation of latent Toxoplasma infection in several organs, particularly in the brain leading toxoplasmic encephalitis (TE) that further complicates the course of AIDS (Sukthana, 2006). Globally, the number of patients who died from AIDS has been declining over the years due to the introduction of highly active antiretroviral therapy (HAART). Toxoplasmosis, one of the HIV co-infections, has, however, contributed to the burden of medical care costs (Suwanagool et al., 1997) and to those patients who are repeatedly admitted to government hospitals (Solomon et al., 2006). Till date, approximately 10% of people living with HIV/AIDS are from the Southern part of Thailand (Ministry of Public Health [MOPH], 2011). To the best of our knowledge, there is no epidemiological surveillance reported on the opportunistic infections in HIV-infected patients including toxoplasmosis in this region. Furthermore, IgG avidity testing, a qualitative method, is the first ever serodiagnostic method to be introduced in differentiating chronic from recently acquired Toxoplasma infection in these patients. This method definitely helps in better understanding the status of Toxoplasma infection and its proper management in HIV patients. It is, therefore, relevant to conduct an epidemiological study of toxoplasmosis by determining the seroprevalence, the association with risk factors and the measurement of IgG avidity from Toxoplasma seropositive patients.
Materials and Methods
Study Population
This cross-sectional study was carried out at Songklanagarind hospital, Hat Yai, Songkhla province, Thailand with the approval from the ethical committee of the Faculty of Medicine, Prince of Songkla University, Thailand (EC 53-080-14-1-2). The study included 300 HIV-infected patients, who attended the outpatient clinic and/or admitted in the ward at the Department of Internal Medicine during October 2009 to June 2010 and their informed consents were obtained prior to this study. The study subjects were randomly selected from those HIV-infected patients in any age group who had their anti-HIV antibody status examined by screening using the ELISA test and confirmed by the western blot technique. The information on related socio-demographic such as age, sex, and occupation as well as risk factors associated with Toxoplasma infection, such as close contact with cats, consumption of uncooked meats, a history of receiving blood transfusion, and some clinical backgrounds such as receiving primary chemoprophylaxis and/or receiving HAART. A CD4 cell count was obtained from their hospital recorded.
Serum Samples
Approximately 5 mL of venous blood sample was drawn from the participating HIV patients by a venipuncture into a sterile test tube. The sera were obtained after separation by centrifugation at 2500 × g for 5 min, and subsequently kept at -20°C until use.
Detection of anti-Toxoplasma IgG antibodies
The serostatus of Toxoplasma infection was screened using a standard ELISA commercial kit (IgG-NovaLisaTM, Dietzenbach, Germany) in accordance with the manufacturer’s instructions.
Measurement of IgG avidity
A positive sample for anti-Toxoplasma IgG antibody was also tested for its avidity using a standard ELISA commercial kit (IgG-NovaLisaTM, Dietzenbach, Germany); high avidity (>40%) indicated a past infection while a low avidity (<40%) indicated a recently acquired infection.
Statistical Analysis
Data obtained from both the questionnaire and laboratory tests were entered and analyzed using the statistical software SPSS version 10 (SPSS Inc., Chicago, IL, USA). The data with quantitative variables were expressed as a mean (±SD) and range, whereas, qualitative variables were estimated and presented as frequencies and percentages. The Chi-square (χ2) test or Fisher exact probability test was chosen to determine the association between possible risk factors and disease transmission. Multivariate analysis adjusted by multiple logistic regressions was used to determine significant differences between demographics or confounding risk factors associated with Toxoplasma infection among study subjects. The p-value of ≤0.05 was regarded as statistically significant.
Results
Demographic Profile of Study Subjects
Table 1 shows the age range of these HIV-infected patients was 21–78 with a mean of 40.4 ± 8.4 years. Majority of these patients were in the age group of 20–39 years (150, 50%), in addition, they were predominantly married (196, 65.3%), and were laborers (174, 58%). About half of these patients had completed secondary school level of education (153, 51%).
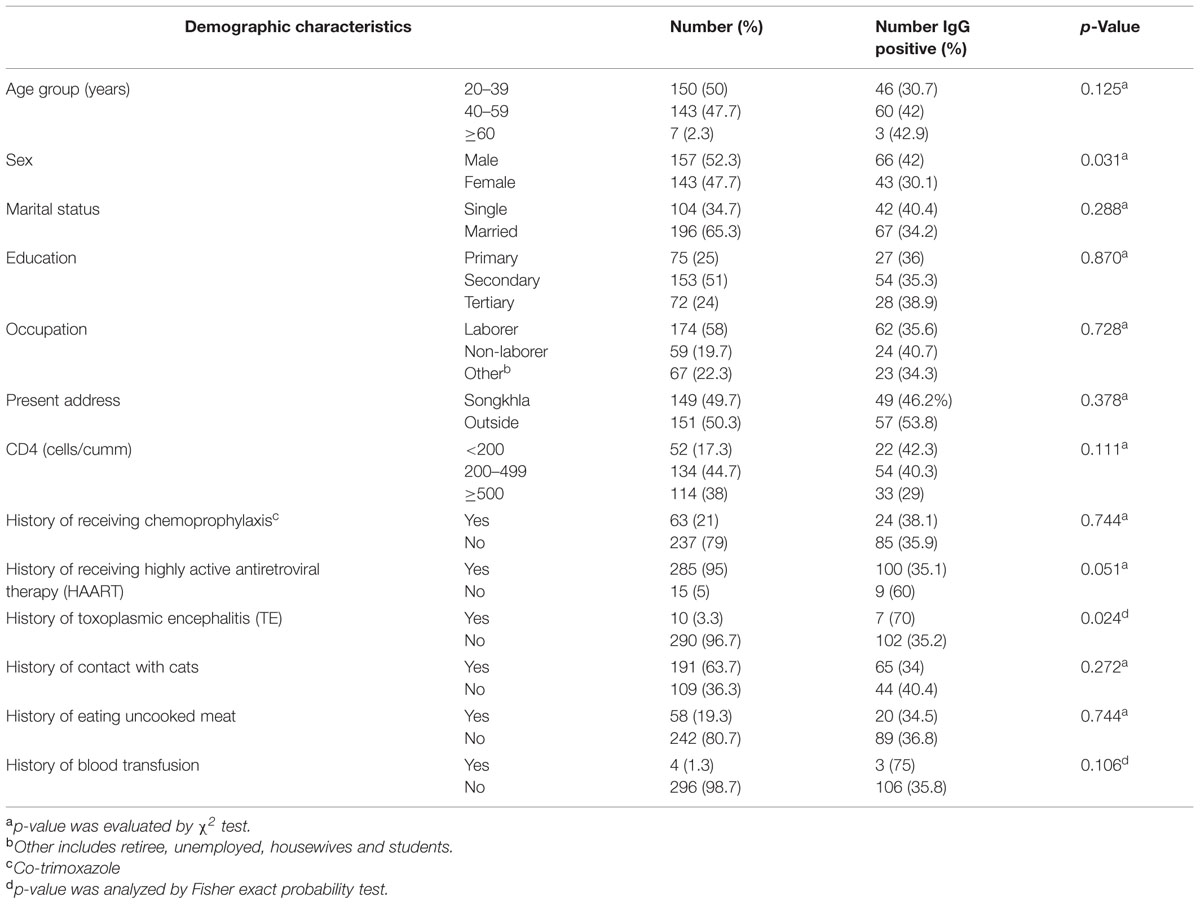
TABLE 1. Univariate analysis of plausible demographic characteristics, clinical profiles, and other possible risk factors associated with Toxoplasma seropositive HIV-infected patients.
Seroprevalence of Toxoplasmosis in HIV/AIDS Patients and in Association with Demographic Characteristics
The seroprevalence of Toxoplasma infection in these patients was 109 (36.3%). Measurement of IgG avidity among Toxoplasma seropositive patients showed 83 (76.2%) had high avidity indicates past infection while 26 (23.9%) patients had low avidity indicates recently acquired Toxoplasma infection.
Using univariate analysis, this study identified that gender and a history of having cerebral toxoplasmosis were statistically significant factors associated with Toxoplasma seropositivity (p < 0.05). The data further showed that majority of male patients were significantly found in the age group of 40–59 years, and they make their living through their labor works. It is also shown that these male patients had not received high education, stayed outside the main city and eating of uncooked meat; however, there was no significant association (Table 2). Further analysis using multivariate logistic regression showed that gender (male) plays a significant role in Toxoplasma seropositivity with adjusted odds ratio of 1.69 (95% CI = 1.05–2.72; Table 3).
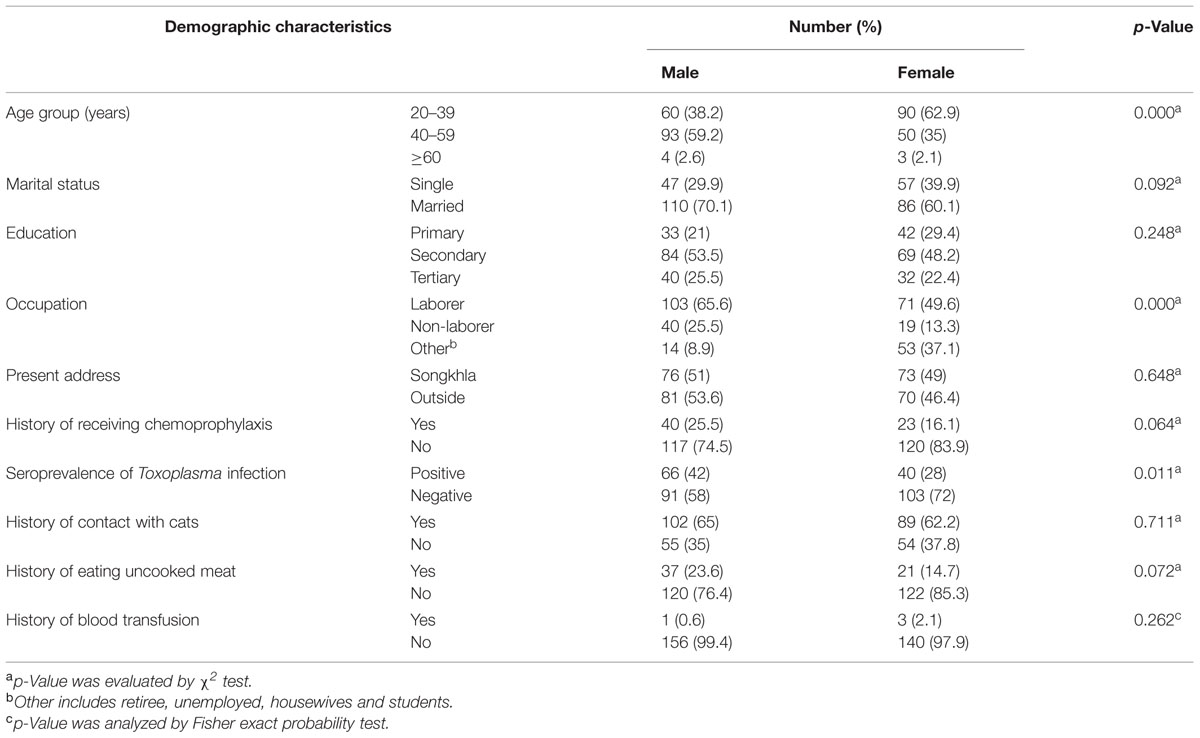
TABLE 2. Comparison of plausible demographic characteristics, clinical profiles, and other possible risk factors between male and female HIV-infected patients.
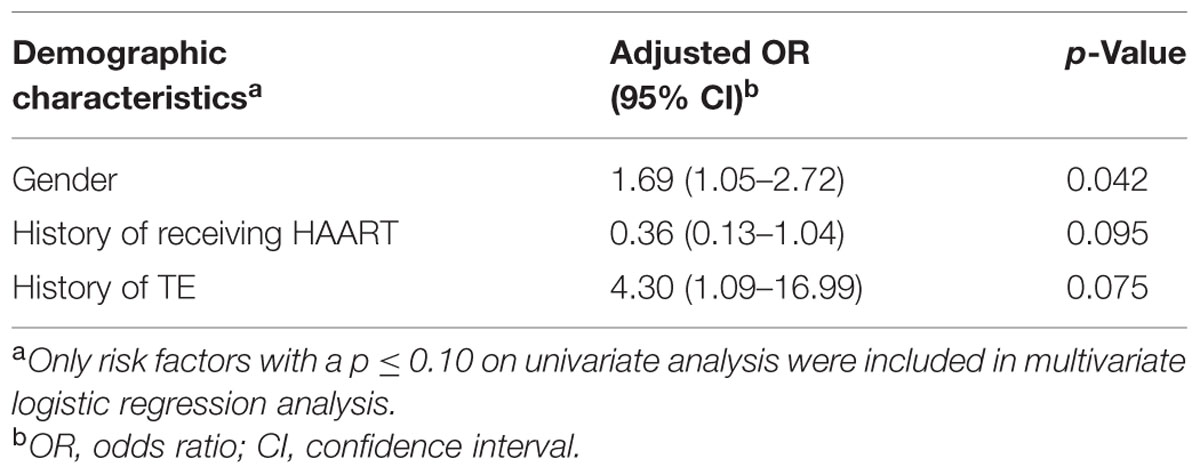
TABLE 3. Multivariate logistic regression analysis of risk factors associated with Toxoplasma seropositivity.
The Prevalence of TE in Patients with AIDS
The past clinical history of these patients showed that 10/300 (3.3%) of HIV/AIDS patients, aged between 28 and 52 years, 5 males, and 5 females, were diagnosed with TE prior to this study. Our study confirmed statistically significant (p = 0.024) sero-evidence of anti-Toxoplasma (IgG) antibodies in seven cases (data were not shown).
Other Co-opportunistic Infections in HIV/AIDS Patients
During the time of this study, there was no new diagnosis of TE reported from our patients. However, patients with Toxoplasma seropositivity and other concurrent opportunistic diseases were found as follow: 24/72 patients with tuberculosis (TB) had Toxoplasma seropositivity and 18 of these TB patients subsequently developed immune reconstitution inflammatory syndrome (IRIS-TB). Toxoplasma seropositivity was also found in: 15 patients with herpes virus infections (herpes simplex (HS) and herpes zoster (HZ) viruses), 2 patients with cytomegalovirus (CMV) infections, 2 patients with salmonellosis, 3 patients with histoplasmosis, 5 patients with cryptococcal meningitis, 6 patients with penicillosis, and 4 patients with non-tuberculous meningitis (NTM). Overall, there was no fatal case reported at the end of this study.
Discussion
Approximately half of HIV-infected patients are co-infected with T. gondii (Shimelis et al., 2009; Daryani et al., 2011). In Thailand, previous studies of the prevalence of Toxoplasma infection among HIV-infected patients found the prevalence ranging from 22.4 to 53.7% (Wongkamchai et al., 1995; Chintana et al., 1998; Sukthana et al., 2000; Nissapatorn et al., 2001; Wanachiwanawin et al., 2001). In our study, 36.3% of subjects were infected with Toxoplasma. This is higher than a study among immunocompetent pregnant women (28.3%) in a study conducted in the same location at the same time (Nissapatorn et al., 2011). Differences in the sensitivity of the ELISA test kit may account for the differences in the prevalence of Toxoplasma infection (Chemoh et al., 2013).
IgG avidity testing was developed to avoid the need of conducting confirmatory tests with a second serum sample to determine, if there is a recently acquired infection (Pour Abolghasem et al., 2011). A positive Toxoplasma IgG test with a low avidity suggests a recently acquired infection (Liesenfeld et al., 2001; Reis et al., 2006). Based on IgG avidity testing, 8.7% of our subjects had a newly acquired Toxoplasma infection and these patients were closely monitored. However, none developed clinical toxoplasmosis during the study.
Using multivariate analysis, male gender was found to be the only significant risk factor for Toxoplasma infection. This is consistent with other studies (Nissapatorn et al., 2007; Akanmu et al., 2010). Males were found to be more susceptible to acquire several infections due to their sex steroid hormones that decrease immune responses and influence disease resistance genes and their behaviors (Klein, 2000). These may be the reasons, why the seropositivity of male HIV/AIDS patients to Toxoplasma infection was significantly higher than the female HIV/AIDS patients (Roberts et al., 2001). Previously identified risk factors, such as close contact with cats, consumption of uncooked meats and history of receiving a blood transfusion were not significantly associated with Toxoplasma infection in our study.
Reactivation of latent Toxoplasma infection is common in immunocompromised hosts (Dahnert, 2003) making HIV patients at higher risk for clinical toxoplasmosis. TE is the most common neurological condition (42%) in HIV-infected patients (Ramirez-Crescencio and Velasquez-Perez, 2011). Ten subjects (3.3%) in our study had a previous history of TE as diagnosed by a combination of clinical TE: headaches, seizure, focal neurological deficits, histology and response of therapy, of these 70% (7) were seropositive for Toxoplasma infection. This finding is similar to another study who found some of the patients with confirmed TE were not positive for Toxoplasma antibodies (Skiest et al., 2000).
Conclusion
Latent toxoplasmosis is still prevalent in our study population. Gender was the only significant risk factor for Toxoplasma infection in our study. Although the number of HIV infected patients in Thailand has decreased nationwide (Ministry of Public Health [MOPH], 2011), we recommend newly infected HIV patients be warned about this opportunistic parasitic disease during the counseling period since both newly acquired and chronic Toxoplasma infections in patients with AIDS are occasionally developed clinical toxoplasmosis (Centers for Disease Control and Prevention [CDC], 2009).
Author Contributions
VN, NS, and PS designed the study. WC, HA, TH, NS, and BC carried out the experiment. WC, NS, and VN helped in manuscript writing and editing. VN, NS, and PS provided opinions and suggestions about this manuscript. All authors read and approved the final version of the manuscript.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
This study was supported by the Office of the Higher Education Commission (OHEC), Thailand; Faculty of Medicine Research Foundation (No: 53-080-14-1-2), Prince of Songkla University, Songkhla province, Thailand and the University of Malaya Research Grant (UMRG 544/14HTM and UMRG 362/15AFR). We thank Dr. Brian Hodgson for his assistance and comments on this manuscript and Dr. Noodchanath Kongchouy for valuable suggestions in statistical analysis.
References
Akanmu, A. S., Osunkalu, V. O., Ofomah, J. N., and Olowoselu, F. O. (2010). Pattern of demographic risk factors in the seroprevalence of anti-Toxoplasma gondii antibodies in HIV infected patients at the Lagos University Teaching Hospital. Nig. Q. J. Hosp. Med. 20, 1–4. doi: 10.4314/nqjhm.v20i1.57974
Centers for Disease Control and Prevention [CDC] (2009). Guidelines for Prevention and Treatment of Opportunistic Infections in HIV-Infected Adults and Adolescents. MMWR. 58 (No. RR04). Available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/rr5804a1.htm [accessed April 10, 2009].
Chemoh, W., Sawangjaroen, N., Nissapatorn, V., Suwanrath, C., Chandeying, V., Hortiwakul, T., et al. (2013). Toxoplasma gondii infection: what is the real situation? Exp. Parasitol. 135, 685–689. doi: 10.1016/j.exppara.2013.10.001
Chintana, T., Sukthana, Y., Bunyakai, B., and Lekkla, A. (1998). Toxoplasma gondii antibody in pregnant women with and without HIV infection. Southeast Asian J. Trop. Med. Public Health 29, 383–386.
Dahnert, W. (2003). Radiology Review Manual: Central Nervous System, 5th Edn. Philadelphia, PA: Lippincott Williams and Wilkins.
Daryani, A., Sharif, M., and Meigouni, M. (2011). Seroprevalence of IgG and IgM anti-Toxoplasma antibodies in HIV/AIDS patients, Northern Iran. Asian Pac. J. Trop. Med. 4, 271–274. doi: 10.1016/S1995-7645(11)60084-9
Klein, S. L. (2000). The effects of hormones on sex differences in infection: from genes to behavior. Neurosci. Biobehav. Rev. 24, 627–638. doi: 10.1016/S0149-7634(00)00027-0
Liesenfeld, O., Montoya, J. G., Kinney, S., Press, C., and Remington, J. S. (2001). Effect of testing for IgG avidity in the diagnosis of Toxoplasma gondii infection in pregnant women: experience in a US reference laboratory. J. Infect. Dis. 183, 1248–1253. doi: 10.1086/319672
Ministry of Public Health [MOPH] (2011). Epidemiological Information Section Bureau of Epidemiology, Department of Disease Control: AIDS surveillance, Thailand. Available at: http://www.boe.moph.go.th/files/report/20110401_95211316.pdf [accessed March 31, 2011].
Montoya, J. G., and Liesenfeld, O. (2004). Toxoplasmosis. Lancet 363, 1965–1976. doi: 10.1016/S0140-6736(04)16412-X
Nissapatorn, V., Lee, C. K. C., Lim, Y. A. L., Tan, K. S., Jamaiah, I., Rohela, M., et al. (2007). Toxoplasmosis: a silent opportunistic disease in HIV/AIDS patients. Res. J. Parasitol. 2, 23–31. doi: 10.3923/jp.2007.23.31
Nissapatorn, V., Suwanrath, C., Sawangjaroen, N., Ling, L. Y., and Chandeying, V. (2011). Toxoplasmosis-serological evidence and associated risk factors among pregnant women in Southern Thailand. Am. J. Trop. Med. Hyg. 85, 243–247. doi: 10.4269/ajtmh.2011.10-0633
Nissapatorn, V., Wattanagoon, Y., Pungpak, S., Supanaranond, W., Bowonwatnuwong, C., Sukthana, Y., et al. (2001). Seroprevalence of toxoplasmosis in HIV infected patients in Chonburi regional hospital, Chonburi, Thailand. Trop. Biomed. 18, 123–129.
Pour Abolghasem, S., Bonyadi, M. R., Babaloo, Z., Porhasan, A., Nagili, B., Gardashkhani, O. A., et al. (2011). IgG avidity test for the diagnosis of acute Toxoplasma gondii infection in early pregnancy. Iran. J. Immunol. 8, 251–255.
Ramirez-Crescencio, M. A., and Velasquez-Perez, L. (2011). Epidemiology and trend of neurological diseases associated to HIV/AIDS. Experience of Mexican patients 1995-2009. Clin. Neurol. Neurosurg. 115, 1322–1325. doi: 10.1016/j.clineuro.2012.12.018
Reis, M. M., Tessaro, M. M., and D’Azevedo, P. A. (2006). Toxoplasma-IgM and IgG-avidity in single samples from areas with a high infection rate can determine the risk of mother-to-child transmission. Rev. Inst. Med. Trop. Sao Paulo 48, 93–98. doi: 10.1590/S0036-46652006000200007
Roberts, C. W., Walker, W., and Alexander, J. (2001). Sex-associated hormones and immunity to protozoan parasites. Clin. Microbiol. Rev. 14, 476–488. doi: 10.1128/CMR.14.3.476-488.2001
Shimelis, T., Tebeje, M., Tadesse, E., Tegbaru, B., and Terefe, A. (2009). Sero-prevalence of latent Toxoplasma gondii infection among HIV-infected and HIV-uninfected people in Addis Ababa, Ethiopia: a comparative cross-sectional study. BMC Res. Notes 2:213. doi: 10.1186/1756-0500-2-213
Skiest, D. J., Erdman, W., Chang, W. E., Oz, O. K., Ware, A., and Fleckenstein, J. (2000). SPECT thallium-201 combined with Toxoplasma serology for the presumptive diagnosis of focal central nervous system mass lesions in patients with AIDS. J. Infect. 40, 274–281. doi: 10.1053/jinf.2000.0664
Solomon, S. S., Kumarasamy, N., Celentano, D. D., Yepthomi, T. H., Arvind, V. P., and Solomon, S. (2006). Trends in HIV-related morbidity among patients admitted to a South Indian tertiary hospital between 1997 and 2003. AIDS Care 18, 366–370. doi: 10.1080/09540120500201755
Sukthana, Y. (2006). Toxoplasmosis: beyond animals to humans. Trends Parasitol. 22, 137–142. doi: 10.1016/j.pt.2006.01.007
Sukthana, Y., Chintana, T., and Lekkla, A. (2000). Toxoplasma gondii antibody in HIV-infected persons. J. Med. Assoc. Thai. 83, 681–684.
Suwanagool, S., Ratanasuwan, W., and Techasathit, W. (1997). The mounting medical care cost for adult AIDS patients at the Faculty of Medicine, Siriraj Hospital: consideration for management. J. Med. Assoc. Thai. 80, 431–439.
Wanachiwanawin, D., Sutthent, R., Chokephaibulkit, K., Mahakittikun, V., Ongrotchanakun, J., and Monkong, N. (2001). Toxoplasma gondii antibodies in HIV and non-HIV infected Thai pregnant women. Asian Pac. J. Allergy Immunol. 19, 291–293.
Keywords: HIV, IgG avidity, seroprevalence, risk factors, toxoplasmosis
Citation: Chemoh W, Sawangjaroen N, Siripaitoon P, Andiappan H, Hortiwakul T, Sermwittayawong N, Charoenmak B and Nissapatorn V (2015) Toxoplasma gondii – Prevalence and Risk Factors in HIV-infected Patients from Songklanagarind Hospital, Southern Thailand. Front. Microbiol. 6:1304. doi: 10.3389/fmicb.2015.01304
Received: 27 January 2015; Accepted: 09 November 2015;
Published: 25 November 2015.
Edited by:
Ute Frevert, New York University School of Medicine, USAReviewed by:
Hridayesh Prakash, University of Hyderabad, IndiaHeinrich Korner, Menzies Research Institute Tasmania, Australia
Copyright © 2015 Chemoh, Sawangjaroen, Siripaitoon, Andiappan, Hortiwakul, Sermwittayawong, Charoenmak and Nissapatorn. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Veeranoot Nissapatorn, veeranoot@um.edu.my; nissapat@gmail.com; Nongyao Sawangjaroen, nongyao.s@psu.ac.th
 Waenurama Chemoh
Waenurama Chemoh Nongyao Sawangjaroen
Nongyao Sawangjaroen Pisut Siripaitoon2
Pisut Siripaitoon2 Hemah Andiappan
Hemah Andiappan Veeranoot Nissapatorn
Veeranoot Nissapatorn