Exergaming as a viable therapeutic tool to improve static and dynamic balance among older adults and people with idiopathic Parkinson’s disease: a systematic review and meta-analysis
- 1Centre for Physical Activity and Nutrition Research, School of Exercise and Nutrition Sciences, Deakin University, Burwood, VIC, Australia
- 2Movement to Health (M2H) Laboratory, Euromov, University of Montpellier, Montpellier, France
- 3Clinical Exercise Science Research Program, Institute of Sport Exercise and Active Living (ISEAL), Victoria University, Melbourne, VIC, Australia
- 4The Florey Institute of Neuroscience and Mental Health, University of Melbourne, Melbourne, VIC, Australia
The use of virtual reality games (known as “exergaming”) as a neurorehabilitation tool is gaining interest. Therefore, we aim to collate evidence for the effects of exergaming on the balance and postural control of older adults and people with idiopathic Parkinson’s disease (IPD). Six electronic databases were searched, from inception to April 2015, to identify relevant studies. Standardized mean differences (SMDs) and 95% confidence intervals (CI) were used to calculate effect sizes between experimental and control groups. I2 statistics were used to determine levels of heterogeneity. 325 older adults and 56 people with IPD who were assessed across 11 studies. The results showed that exergaming improved static balance (SMD 1.069, 95% CI 0.563–1.576), postural control (SMD 0.826, 95% CI 0.481–1.170), and dynamic balance (SMD −0.808, 95% CI −1.192 to −0.424) in healthy older adults. Two IPD studies showed an improvement in static balance (SMD 0.124, 95% CI −0.581 to 0.828) and postural control (SMD 2.576, 95% CI 1.534–3.599). Our findings suggest that exergaming might be an appropriate therapeutic tool for improving balance and postural control in older adults, but more large-scale trials are needed to determine if the same is true for people with IPD.
Introduction
Idiopathic Parkinson’s disease (IPD) is the second most common neurological disease worldwide, affecting approximately 1% of all older adults aged 65 years or older (Moore et al., 2005; Lees et al., 2009). People with IPD experience tremors, rigidity, slowness of movement, and gait and balance dysfunction (Dibble et al., 2004; Lees et al., 2009; Zettergren et al., 2011). The balance impairments, which progressively worsen over time, increase the risk of falls, fall-related injuries, and mortality (Bloem et al., 2001; Wood et al., 2002) found 68.3% of people with IPD fell at least once per year, while 50.5% were recurrent fallers (two or more falls per year), while Lindholm et al. (2015) found 31% people with IPD reported nearly falling in the previous 12 months. Medications, such as levodopa, are often the first line of treatment for IPD and have shown promise in improving motor function in the early stages of the disease (Singh et al., 2007; Lees et al., 2009). However, the long-term efficacy of these treatments are poor, and levodopa therapy does little to preserve balance during the more advanced stages of the disease when balance is typically most affected (Bloem et al., 1996; Hely et al., 2005).
Exergaming, in this instance, is a term used to describe computer games that require players to physically move in response to game demands and/or an on-screen avatar (usually constructed from a sensor that records the player’s physical characteristics). Examples of exergaming models include interactive 3-Dimensional gaming modules, such as the Nintendo Wii Fit and the X-Box Kinect. Exergaming has the potential to facilitate balance improvements, including reducing standing center of pressure (CoP) variability (Rendon et al., 2012; Toulotte et al., 2012; Bieryla and Dold, 2013; Wuest et al., 2014), in a home-based setting for older adults (Miller et al., 2014) and for people recovering from spinal cord injury, brain injury (Betker et al., 2007 or stroke (Hung et al., 2014) who have severe balance impairments.
The wide variety of commercially available exergames and the scope of exergaming intensity levels allow for interventions to be tailored to target-specific aspects of balance (Kahlbaugh et al., 2011; Chao et al., 2014). Additionally, the range of exergames available to the consumer can stimulate diversity within training programs, which can aid in creating a fun and engaging “virtual” atmosphere (Barry et al., 2014; Ravenek et al., 2015). Such an environment is conducive to high levels of exercise adherence and participant motivation (Ravenek et al., 2015), which is likely to enhance the efficacy of the training. Duque et al. (2013) and Wuest et al. (2014) presented high interventional compliance rates (97 and 100%, respectively) in their exergaming interventions, though like many of the current exergaming studies, long-term exercise adherence was not reported. Moreover, some games include demanding cognitive and/or motor tasks that may be beyond the capability of people with IPD (Dos Santos Mendes et al., 2012). This may cause frustration and in turn cause people with IPD to avoid the games altogether (Dos Santos Mendes et al., 2012). This highlights the importance of individualized rehabilitation programing to effectively improve balance (Dos Santos Mendes et al., 2012).
Previous exergaming studies have attempted to quantify static and dynamic balance using the Berg balance scale (BBS) (Berg, 1989) and the Timed Up-and-Go test (TUG), for older adults (Agmon et al., 2011; Bateni, 2012; Franco et al., 2012), and for people with IPD (Zettergren et al., 2011; Mhatre et al., 2013). These tests are low-cost, simplistic assessments that are relatively quick to administer and convenient in the clinical setting. However, the subjective nature of these tests and their questionable sensitivity to detect slight changes in CoP deviation compared to posturographic technologies (Black, 2001) highlight the problematic use of these tests. Furthermore, of the current available exergaming randomized control trials (RCTs), there appears to be limited posturographic reporting of static or dynamic balance for older adults, and we know of only one RCT that has used posturography to report balance changes following exergaming for people with IPD (Yen et al., 2011).
Exergaming has the potential to increase exercise adherence, balance confidence, and exercise enjoyment (Barry et al., 2014; Miller et al., 2014; Ravenek et al., 2015), but it is unclear if it can improve the balance of people with IPD (Agmon et al., 2011; Meldrum et al., 2012; Holmes et al., 2013; Barry et al., 2014). There is limited evidence to suggest exergaming is an efficacious rehabilitation method for balance and postural issues experienced by older people and people with IPD. Therefore, we intend to systematically review exergaming RCTs and use a meta-analytical approach to compare the effects of exergaming on the balance of older adults and people with IPD.
Methods
Search Strategy
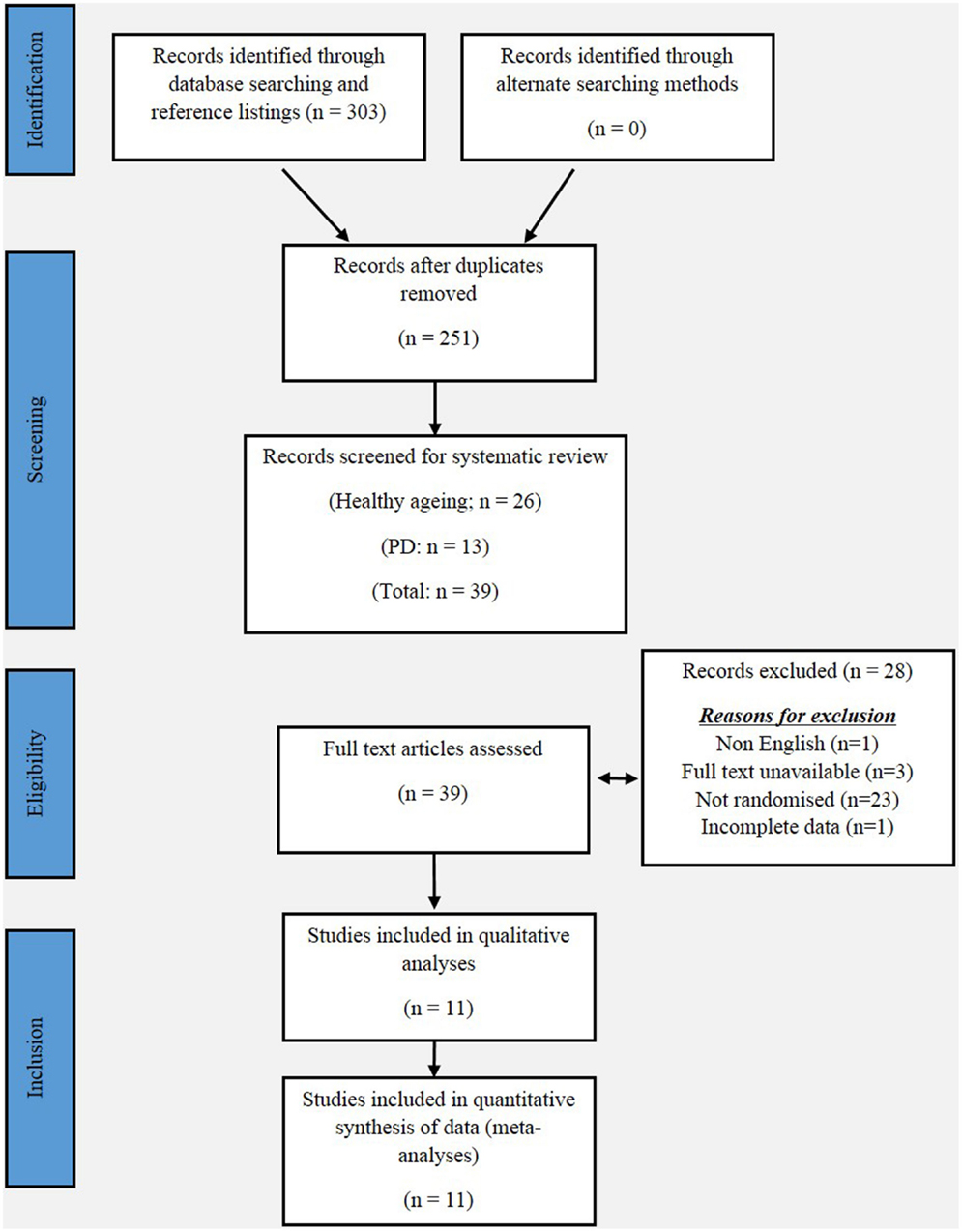
This review has been informed by the PRISMA statement. The following electronic databases were searched from their inception to April 2015: PubMed, MEDLINE, PsycINFO, Embase, Google Scholar, and Scopus. The following keywords were used in combinations: Parkinson, Parkinson’s disease, Parkinsonism, exergaming, gaming, virtual reality gaming, series gaming, gait, balance, aged, and elderly. Additionally, the reference lists of the included studies were also searched. Figure 1 shows a flow diagram of the processing of search results from initial searches to the final included studies.
Inclusion Criteria
To determine the eligibility of each study, the title and abstract were screened independently by a single reviewer (Dale M. Harris). Studies were included if (1) it was printed in full English text, (2) the aim of the study was to examine the effects of exergaming on the static and dynamic balance of older adults and/or people with IPD, (3) the target population was aged 65 years or older, (4) the main intervention was exergaming, serious gaming, or virtual reality gaming, and (5) the effects of the gaming intervention were compared to either a control group, or an alternative training/rehabilitation intervention, including other forms of exercise, balance training, or scheduled general physical activity. All studies included were randomized, and only published articles (including articles in press) were included. All duplicate articles were removed.
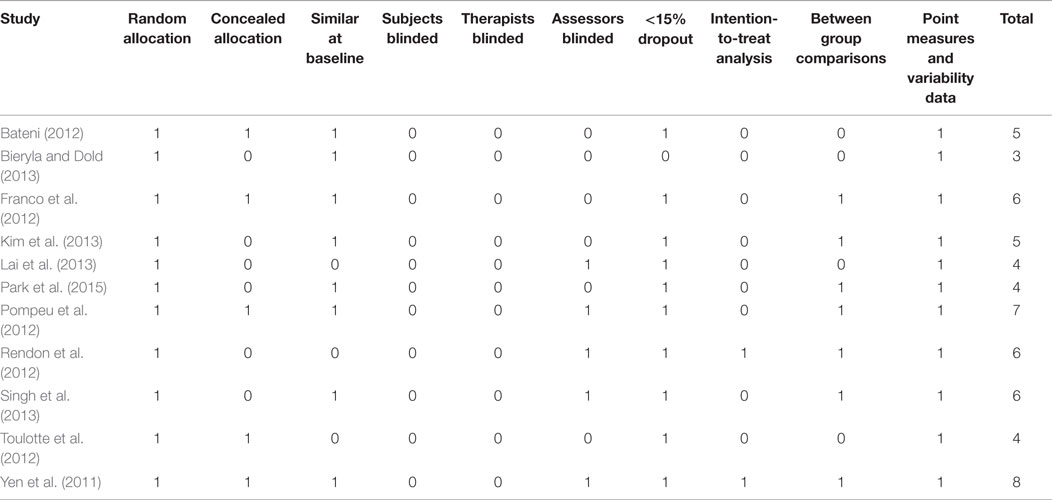
Quality Assessment of Studies
Data were extracted by an independent reviewer (Dale M. Harris), and revised by a second reviewer (Wei-Peng Teo). The methodological quality of each study was independently assessed by two reviewers (Liam Johnson and Timo Rantalainen) using the physiotherapy evidence database (PEDro) scale (ranging from 0 to 10 points). The PEDro scale is an assessment tool for evaluating methodological quality of RCTs conducted in the field of physiotherapy with fair-to-good reliability (Maher et al., 2003). Any disagreements in scores were resolved by discussion between reviewers, with the judgment of the primary author (Dale M. Harris) being sought if consensus could not be reached. All scores assigned to each study were agreed upon by unanimity and are presented in Table 4.
Selection of Outcome Measures
For the purpose of our meta-analysis, we categorized the balance outcome measures into static and dynamic assessments. We chose the BBS (Berg et al., 1991) as our measure of static balance. The BBS (Berg et al., 1991) consists of 14 balance-challenging tasks, whereby the participants base of support remained fixed, or moved marginally, and each task is scored on a 0–4 scale (maximum score = 56). A higher score is indicative of better balance (Thorbahn and Newton, 1996).
We have also used postural control (PC) measures as assessments of static balance because they required no (or limited) movement of the participants base of support. Studies employing motion capture technology that were capable of quantifying the amount of postural sway circumference or CoP deviation, including posturographic measures, force plates, digital sway meters, virtual avatars, or Wii balance-board technology, were included as measures of PC.
We identified the TUG test, which involves the purposeful movement of the participants base of support, as a measure of dynamic balance. The TUG measures the total time (seconds) that an individual takes to rise from a chair, walk at a fast pace for 3-m, turn around, walk back and sit on the same chair (Podsiadlo and Richardson, 1991).
Data Synthesis and Analysis
A random effects meta-analysis was conducted with MedCalc Statistical Software v14.12.0 (MedCalc Software bvba, Ostend, Belgium; http://www.medcalc.org: 2015). Continuous measures extrapolation yielded standardized mean difference (SMD) results, which were used as a measure of effect size, along with 95% confidence intervals (CI). Heterogeneity across studies was tested based on I2 statistics, which indicates the percentage of variance that is attributable to study heterogeneity. Studies with I2 < 40% was considered to have low heterogeneity, I2 = 40–75% was considered to have moderate heterogeneity, and I2 > 75% was considered to have high heterogeneity. Fisher’s method of combining p-values was applied to test for overall effects for each outcome measure.
Results
Study Selection
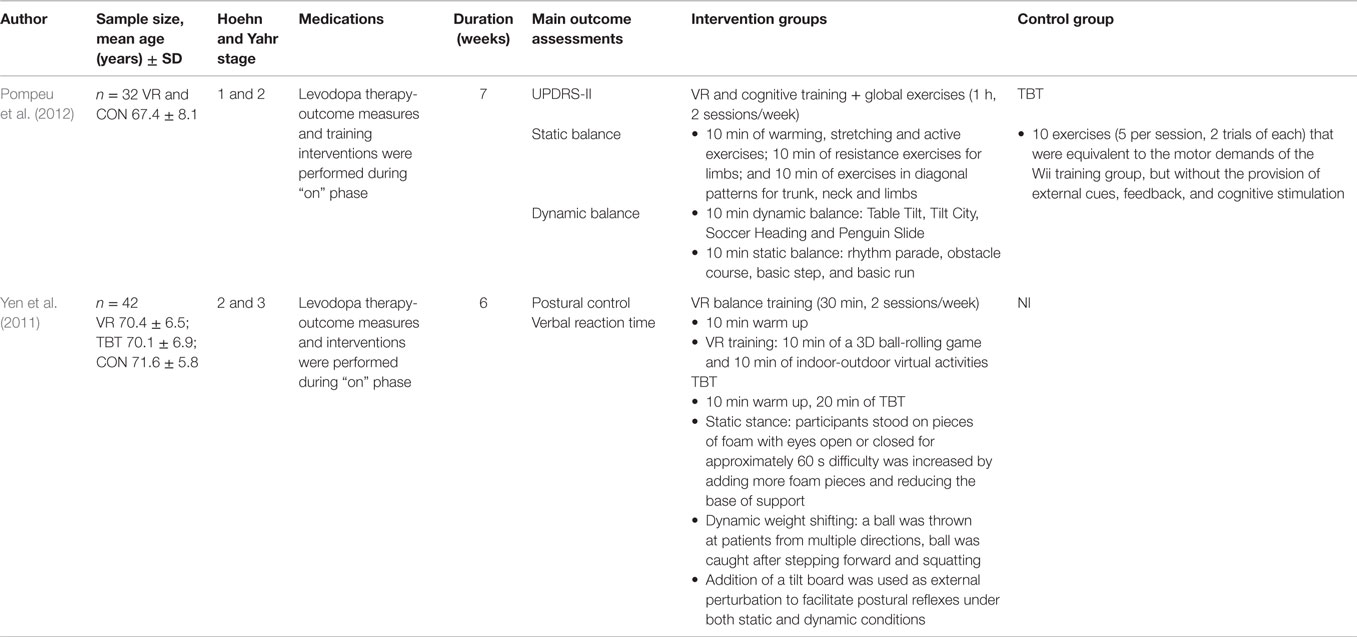
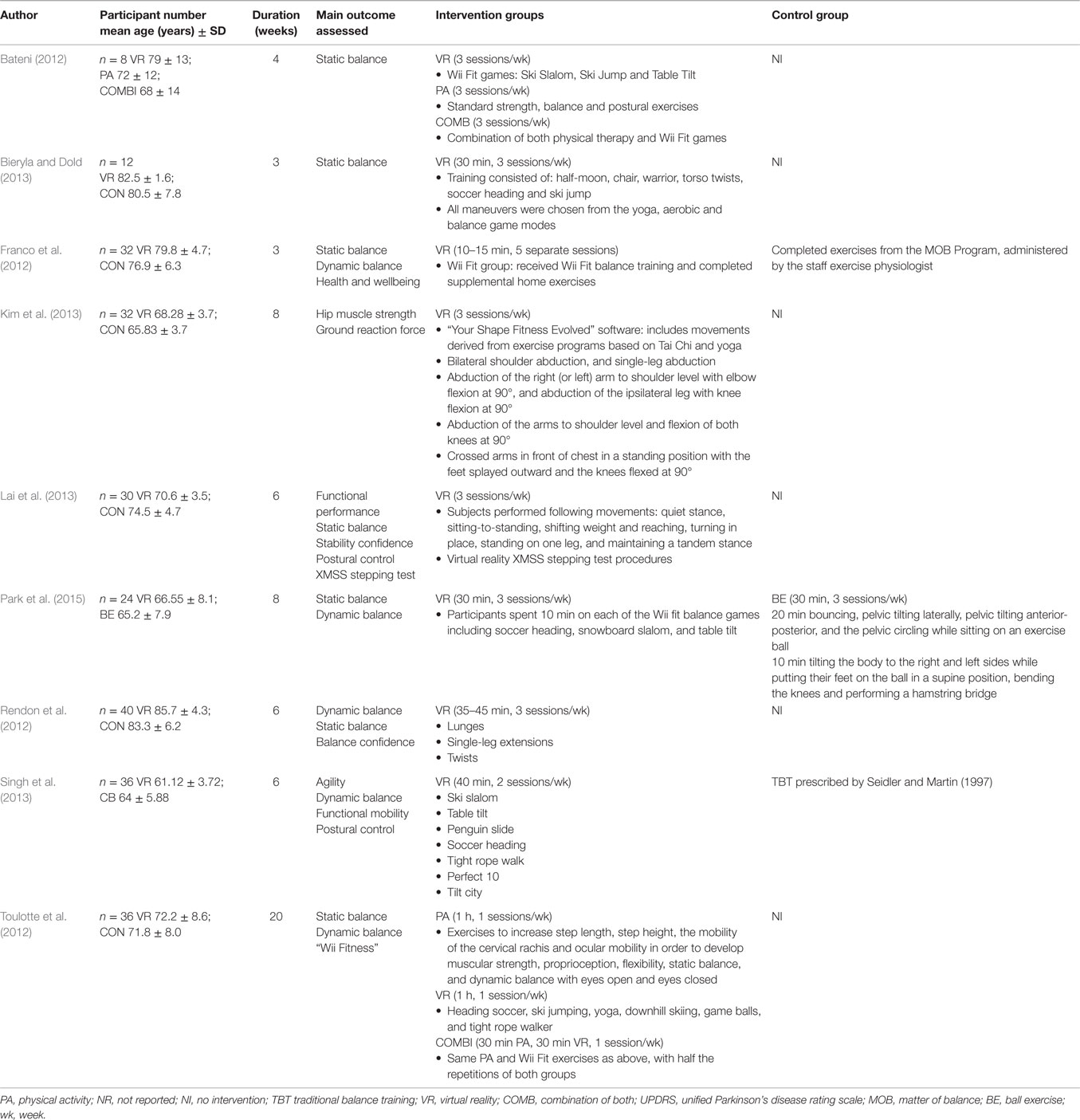
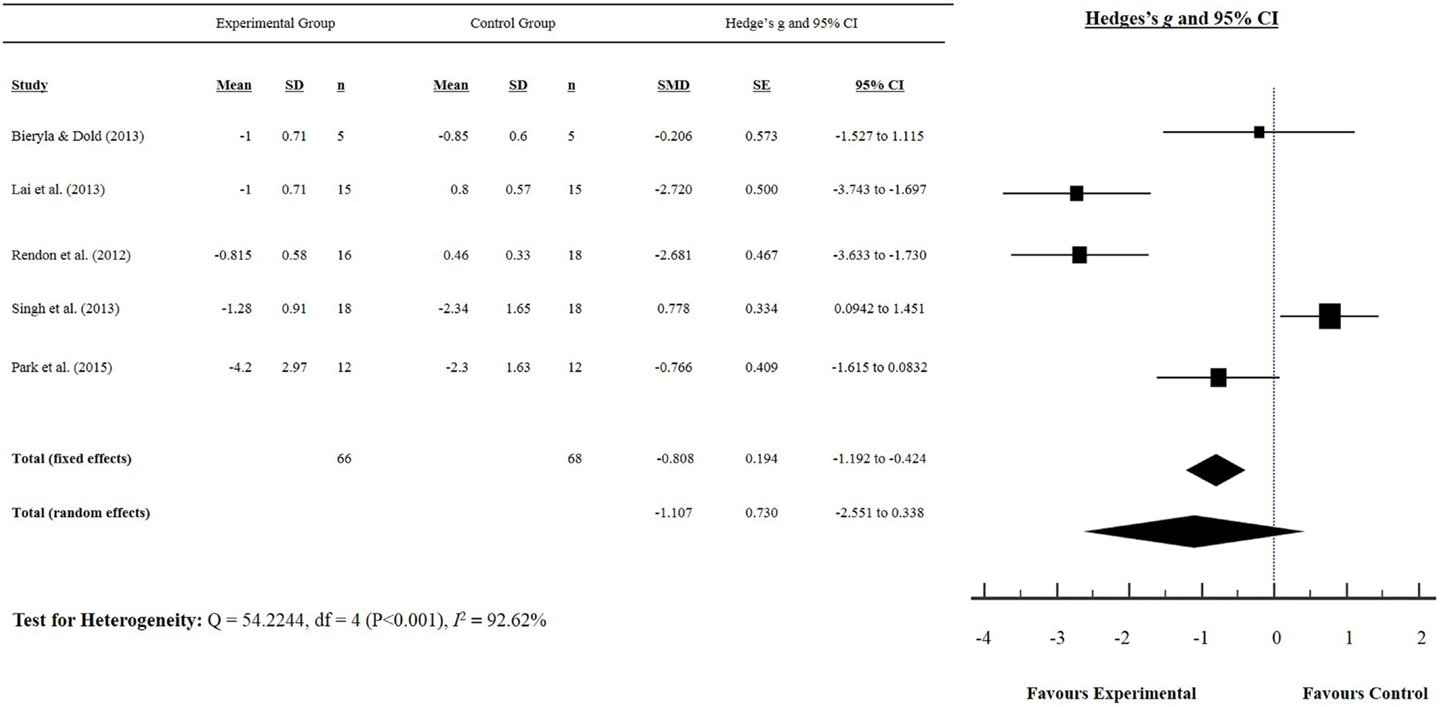
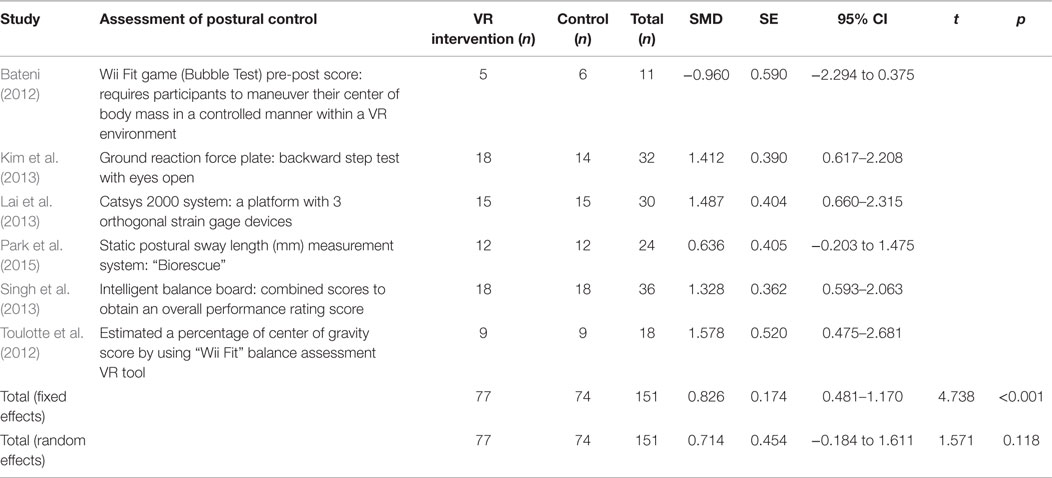
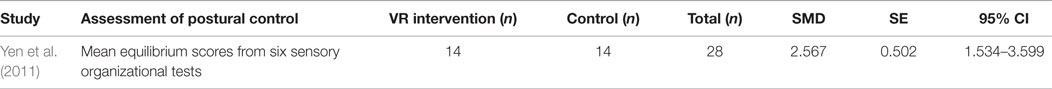
Our initial search yielded 303 articles. Following screening of the title and abstract, and removal of duplicates, 11 studies were included in our meta-analysis, and are summarized in Tables 1 and 2. Five studies reported a measurement of static balance (BBS) (Bateni, 2012; Franco et al., 2012; Pompeu et al., 2012; Bieryla and Dold, 2013; Lai et al., 2013) (Figure 2), and five studies reported a measurement of dynamic balance (TUG) (Rendon et al., 2012; Bieryla and Dold, 2013; Lai et al., 2013; Singh et al., 2013; Park et al., 2015) (Figure 3). Seven studies reported a measurement of PC (Yen et al., 2011; Bateni, 2012; Toulotte et al., 2012; Kim et al., 2013; Lai et al., 2013; Singh et al., 2013; Park et al., 2015) (Table 3).
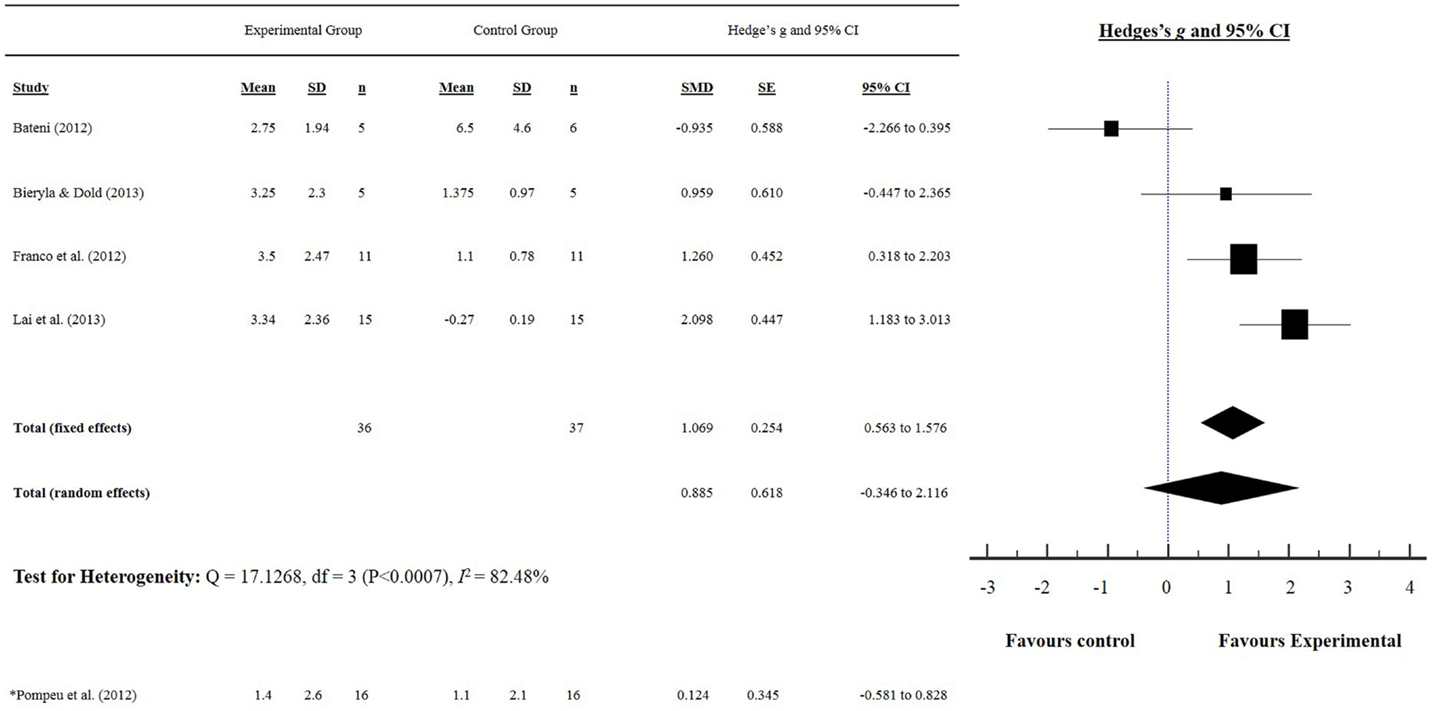
Figure 2. Static balance: Berg balance scale score. (*) indicates only IPD study that used the BBS as a measure of static balance.
Participant Characteristics
In total, 225 older adults (experimental = 115, control = 110) and 56 people with IPD (experimental = 28, control = 28) were assessed across 11 studies. The mean age ±SD for the older adults was 73.32 ± 7.35 (experimental 73.97 ± 8.19 years, control 72.67 ± 6.84 years), while the mean age for people with IPD was 69.8 ± 2.16 (experimental 68.9 ± 2.12, control 71.6 ± 5.8). The mean duration of IPD was 6.9 ± 1.27 years, and disease severity, as assessed by the Hoehn and Yahr scale(Hoehn and Yahr, 1998), ranged from 1 to 3 (mild to moderate disease severity).
Methodological Quality
The scores for each criterion using the PEDro scale are presented in Table 5. The mean score for all 11 trials was 5.3 ± 1.5. Across the 11 studies, neither the participants nor the therapists administering the program were blinded to the intervention. Only one study concealed the allocation of all participants, used blinded assessors, and employed intention-to-treat analysis (Yen et al., 2011).
Static Balance: Berg Balance Scale
The effects of exergaming on static balance were examined by pooling post-intervention data from the five studies that reported BBS results from older adults and people with IPD (experimental n = 52, control n = 53) (Figure 2). Overall, the pooled results showed a significant improvement in static balance for older adults, as evidenced by increased BBS scores post-intervention (SMD 1.069, 95% CI 0.563–1.576). Pompeu et al. (2012) was the only study to examine the effect of exergaming on the balance of people with IPD and showed a favorable effect (i.e., an improvement in BBS score) (SMD 0.124, 95% CI −0.581 to 0.828). Only Bateni (2012) showed a non-favorable effect (i.e., a reduction in BBS score) for the exergaming intervention group (SMD −0.935, 95% CI −2.266 to 0.395) of older adults.
Dynamic Balance: Timed Up and Go Test
The effects of exergaming on dynamic balance were examined by pooling post-intervention data from the five studies that reported TUG test results of older adults and people with IPD (experimental n = 66, control n = 68) (Rendon et al., 2012; Bieryla and Dold, 2013; Lai et al., 2013; Singh et al., 2013; Park et al., 2015) (Figure 3). Our findings showed a significant improvement in TUG (SMD −0.808, 95% CI −1.192 to −0.424), as indicated by a negative score (i.e., reduction in TUG time). Singh et al. (2013) was the only study to show a non-favorable effect following a 6-week exergaming intervention for older adults (SMD 0.778, 95% CI 0.0898–1.466).
Postural Control
Tables 3 and 4 summarize each study and their effect sizes regarding exergaming and PC in older adults (Table 3) and people with IPD (Table 4). Collectively, our results suggest that exergaming improves PC in older adults (SMD 0.826, 95% CI 0.481–1.170). Only Bateni (2012) reported a non-favorable effect following a 4-week exergaming and physical therapy training intervention for older adults (SMD −0.960, 95% CI −2.294 to 0.375). Yen et al. (2011) was the only study to investigate exergaming and PC of people with IPD, and found a significant improvement in PC for people with IPD (SMD 2.576, 95% CI 1.534–3.599).
Discussion
This study is the first to cohesively present the effects of exergaming on the balance of older adults and people with IPD. Our systematic review of the literature found limited robust evidence for the effects of exergaming on the balance of older adults and people with IPD. Of the RCTs included in our meta-analysis, the methodologies are not comprehensive enough to definitively elucidate if exergaming affects the balance of older adults or people with IPD. Our meta-analysis showed that no RCTs used the TUG as a measure of dynamic balance of people with IPD, and only two RCTs measured static balance using the BBS (Pompeu et al., 2012) or PC measures (Yen et al., 2011) for people with IPD. However, we found exergaming improves the static (BBS and PC measures) and dynamic (TUG) balance of older adults, despite the variability in PC measures used. Therefore, while our meta-analysis might suggest that exergaming can improve the balance of older adults, it remains largely unknown if the same is true for people with IPD due to a lack of sufficient evidence.
Only Bateni (2012) and Singh et al. (2013) found the static and dynamic balance of older adults was not improved by exergaming. An explanation for this could arise from their respective methodologies; the control groups for both studies included exercise interventions that specifically targeted balance (i.e., one-leg standing, free leg swinging, and moving objects), which may have contributed to the lack of effects found. These results might indicate that exergaming can improve balance as much as balance-specific training among older adults, which has previously been reported (Bateni, 2012; Franco et al., 2012; Toulotte et al., 2012; Singh et al., 2013).
It is beyond the scope of this study to determine the mechanisms responsible for the improvements in balance indicated by our meta-analysis. However, we can speculate that exergaming might provide a novel setting conducive to enhancing an individual’s ability to learn and perform new skills. For people with IPD who experience difficulties learning new skills (Scandalis et al., 2001; Dos Santos Mendes et al., 2012), the stimulus provided by exergaming might be strong enough to induce implicit learning (Mirelman et al., 2011). Additionally, immediate biofeedback of performance may also account for the augmented balance improvements of older adults (Bisson et al., 2007; Heiden and Lajoie, 2010; Franco et al., 2012; Cho et al., 2014; Wuest et al., 2014). Caudron et al. (2014) postulated that visual immersion provides a strong biofeedback cue for improving PC for people with IPD, although the effects of biofeedback on the balance of people with IPD is not clear. However, speculation of the opposite that certain exergames considered too challenging (i.e., exergames requiring dual tasking or decisive movements) might impair balance improvements for people with IPD has also been suggested (Dos Santos Mendes et al., 2012; Galna et al., 2014). Moreover, many interventions conducted in the clinical setting are unlikely to be replicated in the home setting, highlighting the importance of selecting appropriate exergames so that people with IPD can safely and effectively perform the tasks from home.
We have identified that static balance, indicative of PC changes, among older adults can be improved by exergaming, and Yen et al. (2011) demonstrated improvements in the PC of people with IPD. Interestingly, there were inconsistencies in effect sizes seen in both IPD studies compared with the pooled effects of older adults, with Yen et al. (2011) having a much larger effect size compared with Pompeu et al. (2012). To provide some explanations, Pompeu et al. (2012) contrasted an exergaming group against a traditional balance training group, while Yen et al. (2011) did not adopt an intervention for their control group providing a sound reason for the disparate results. Yen and colleagues used a combination of exergaming and traditional balance training in their intervention group. Furthermore, it is likely that the study by Yen and colleagues used participants that are between Hoehn–Yahr stages II and III, which may have allowed for the larger balance effects seen in Yen et al. (2011). Finally, IPD participants in both studies were using medication at the time of intervention, which can improve functional balance in the early stages of the disease (Nova et al., 2004), potentially reducing the effects of exergaming on balance in Pompeu et al. (2012).
The use of simplistic assessments to quantify static and dynamic balance presents as a limitation in the current exergaming literature, with posturography not commonly used. Posturography provides a more valid tool for effectively measuring static and dynamic balance, but can be costly and inaccessible for many clinicians. Alternatively, Wii balance-board technology is commercially accessible, and has previously shown high validity and reliability in mapping CoP deviation for older adults during static stance (Clark et al., 2010; Chang et al., 2013), but no evidence exists validating Wii balance-board technology and CoP deviation for people with IPD.
Our average PEDro score of 5.3 suggests that the studies included were of moderate methodological quality (Moseley et al., 2002). A lack of concealed allocation of participants, double blinding, and intention-to-treat analysis present as limitations of the methodology of the current exergaming literature. Furthermore, non-English studies were excluded here, and this presents as another limitation in the applicability of non-English exergaming literature. Lastly, only two of the studies included targeted people with IPD. Resultantly, our findings may not represent the larger community of people with IPD. Nevertheless, we deliberately included only RCT studies in an attempt to raise the standard of methodological quality. As such, while the IPD studies included were underwhelming, we have shown that there is a need for more robust, comprehensive studies on exergaming for people with IPD.
Our systematic review and meta-analysis demonstrates that exergaming can improve the balance of older adults. However, with the current available studies, the efficacy of exergaming cannot be sufficiently determined for people with IPD. While a non-favorable training effect was identified in two studies included in our meta-analysis, both studies implemented balance-specific training interventions for the control group. We interpret this to indicate exergaming has similar effects on balance as balance-specific training. Whether or not this training response is caused by physiological adaptation or neural adaptation is unknown, with the effects of exergaming on balance for people with IPD speculative to this point. As such, more robust RCT evidence is required to validate our findings.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Funding Source
This study was supported by the Central Research Grant Scheme (RM29471) and the School of Exercise and Nutrition Sciences, Deakin University. TR is supported by an Alfred Deakin Postdoctoral Fellowship. LJ is supported by the Australian Government’s Collaborative Research Networks program. MM is supported by a Labex NUMEV Fellowship (Digital and Hardware Solutions, Environmental and Organic Life Modeling, ANR-10-LABX-20).
Acknowledgments
All authors are acknowledged for their contributions to this study.
References
Agmon, M., Perry, C., Phelan, E., Demiris, G., and Nguyen, H. (2011). A pilot study of Wii Fit exergames to improve balance in older adults. J. Geriatr. Phys. Ther. 34, 161–167. doi: 10.1519/JPT.0b013e3182191d98
Barry, G., Galna, B., and Rochester, L. (2014). The role of exergaming in Parkinson’s disease rehabilitation: a systematic review of the evidence. J. Neuroeng. Rehabil. 11, 1–17. doi:10.1186/1743-0003-11-33
Bateni, H. (2012). Changes in balance in older adults based on use of physical therapy vs the Wii Fit gaming system: a preliminary study. Physiotherapy 98, 211–216. doi:10.1016/j.physio.2011.02.004
Berg, K. (1989). Measuring balance in the elderly: preliminary development of an instrument. Physiother. Can. 41, 304–311. doi:10.3138/ptc.41.6.304
Berg, K. O., Wood-Dauphinee, S. L., Williams, J. I., and Maki, B. (1991). Measuring balance in the elderly: validation of an instrument. Can. J. Public Health 83, S7–S11.
Betker, A. L., Desai, A., Nett, C., Kapadia, N., and Szturm, T. (2007). Game-based exercises for dynamic short-sitting balance rehabilitation of people with chronic spinal cord and traumatic brain injuries. Phys. Ther. 87, 1389–1398. doi:10.2522/ptj.20060229
Bieryla, K. A., and Dold, N. M. (2013). Feasibility of Wii Fit training to improve clinical measures of balance in older adults. Clin. Interv. Aging 8, 775. doi:10.2147/CIA.S46164
Bisson, E., Contant, B., Sveistrup, H., and Lajoie, Y. (2007). Functional balance and dual-task reaction times in older adults are improved by virtual reality and biofeedback training. Cyberpsychol. Behav. 10, 16–23. doi:10.1089/cpb.2006.9997
Black, F. O. (2001). Clinical status of computerized dynamic posturography in neurotology. Curr. Opin. Otolaryngol. Head Neck Surg. 9, 314–318. doi:10.1097/00020840-200110000-00011
Bloem, B. R., Beckley, D. J., Van Dijk, J. G., Zwinderman, A. H., Remler, M. P., and Roos, R. A. (1996). Influence of dopaminergic medication on automatic postural responses and balance impairment in Parkinson’s disease. Mov. Disord. 11, 509–521. doi:10.1002/mds.870110506
Bloem, B. R., Grimbergen, Y. A., Cramer, M., Willemsen, M., and Zwinderman, A. H. (2001). Prospective assessment of falls in Parkinson’s disease. J. Neurol. 248, 950–958. doi:10.1007/s004150170047
Caudron, S., Guerraz, M., Eusebio, A., Gros, J. P., Azulay, J. P., and Vaugoyeau, M. (2014). Evaluation of a visual biofeedback on the postural control in Parkinson’s disease. Clin. Neurophys 44, 77–86. doi:10.1016/j.neucli.2013.10.134
Chang, W.-D., Chang, W.-Y., Lee, C.-L., and Feng, C.-Y. (2013). Validity and reliability of Wii Fit balance board for the assessment of balance of healthy young adults and the elderly. J. Phys. Ther. Sci. 25, 1251. doi:10.1589/jpts.25.1251
Chao, Y.-Y., Scherer, Y. K., and Montgomery, C. A. (2014). Effects of using Nintendo Wii™ exergames in older adults: a review of the literature. J. Aging Health. 27, 379–402. doi:10.1177/0898264314551171
Cho, G. H., Hwangbo, G., and Shin, H. S. (2014). The effects of virtual reality-based balance training on balance of the elderly. J. Phys. Ther. Sci. 26, 615–617. doi:10.1589/jpts.26.615
Clark, R. A., Bryant, A. L., Pua, Y., Mccrory, P., Bennell, K., and Hunt, M. (2010). Validity and reliability of the Nintendo Wii balance board for assessment of standing balance. Gait. Posture 31, 307–310. doi:10.1016/j.gaitpost.2009.11.012
Dibble, L. E., Nicholson, D. E., Shultz, B., Macwilliams, B. A., Marcus, R. L., and Moncur, C. (2004). Maximal speed gait initiation of healthy elderly individuals and persons with Parkinson disease. J. Neurol. Phys. Ther. 28, 2–11. doi:10.1097/01.NPT.0000284772.09932.dc
Dos Santos Mendes, F. A., Pompeu, J. E., Lobo, A. M., Da Silva, K. G., De Paula Oliveira, T., Zomignani, A. P., et al. (2012). Motor learning, retention and transfer after virtual-reality-based training in Parkinson’s disease – effect of motor and cognitive demands of games: a longitudinal, controlled clinical study. Physiotherapy 98, 217–223. doi:10.1016/j.physio.2012.06.001
Duque, G., Boersma, D., Loza-Diaz, G., Hassan, S., Suarez, H., Geisinger, D., et al. (2013). Effects of balance training using a virtual-reality system in older fallers. Clin. Interv. Aging 8, 257–263. doi:10.2147/cia.s41453
Franco, J. R., Jacobs, K., Inzerillo, C., and Kluzik, J. (2012). The effect of the Nintendo Wii Fit and exercise in improving balance and quality of life in community dwelling elders. Technol. Health Care 20, 95–115. doi:10.3233/THC-2011-0661
Galna, B., Jackson, D., Schofield, G., Mcnaney, R., Webster, M., Barry, G., et al. (2014). Retraining function in people with Parkinson’s disease using the microsoft kinect: game design and pilot testing. J. Neuroeng. Rehabil. 11, 60. doi:10.1186/1743-0003-11-60
Heiden, E., and Lajoie, Y. (2010). Games-based biofeedback training and the attentional demands of balance in older adults. Aging Clin. Exper. Res. 22, 367–373. doi:10.3275/6733
Hely, M. A., Morris, J. G., Reid, W. G., and Trafficante, R. (2005). Sydney multicenter study of parkinson’s disease: non-L-dopa-responsive problems dominate at 15 years. Mov Disord 20, 190–199.
Hoehn, M. M., and Yahr, M. D. (1998). Parkinsonism: onset, progression, and mortality. Neurology 50, 318–318. doi:10.1212/WNL.50.2.318
Holmes, J. D., Gu, M. L., Johnson, A. M., and Jenkins, M. E. (2013). The effects of a home-based virtual reality rehabilitation program on balance among individuals with Parkinson’s disease. Phys. Occup. Ther. Geriatr. 31, 241–253. doi:10.3109/02703181.2013.814743
Hung, J. W., Chou, C. X., Hsieh, Y. W., Wu, W. C., Yu, M. Y., Chen, P. C., et al. (2014). Randomized comparison trial of balance training by using exergaming and conventional weight-shift therapy in patients with chronic stroke. Arch. Phys. Med. Rehabil. 95, 1629–1637. doi:10.1016/j.apmr.2014.04.029
Kahlbaugh, P. E., Sperandio, A. J., Carlson, A. L., and Hauselt, J. (2011). Effects of playing Wii on well-being in the elderly: physical activity, loneliness, and mood. Activ. Adapt Aging 35, 331–344. doi:10.1080/01924788.2011.625218
Kim, J., Son, J., Ko, N., and Yoon, B. (2013). Unsupervised virtual reality-based exercise program improves hip muscle strength and balance control in older adults: a pilot study. Arch. Phys. Med. Rehabil. 94, 937–943. doi:10.1016/j.apmr.2012.12.010
Lai, C.-H., Peng, C.-W., Chen, Y.-L., Huang, C.-P., Hsiao, Y.-L., and Chen, S.-C. (2013). Effects of interactive video-game based system exercise on the balance of the elderly. Gait Posture 37, 511–515. doi:10.1016/j.gaitpost.2012.09.003
Lees, A. J., Hardy, J., and Revesz, T. (2009). Parkinson’s disease. Lancet 373, 2055–2066. doi:10.1016/S0140-6736(09)60492-X
Lindholm, B., Hagell, P., Hansson, O., and Nilsson, M. H. (2015). Prediction of falls and/or near falls in people with mild Parkinson’s disease. Plos one 10, e0117018.
Maher, C. G., Sherrington, C., Herbert, R. D., Moseley, A. M., and Elkins, M. (2003). Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys ther 83, 713–721.
Meldrum, D., Glennon, A., Herdman, S., Murray, D., and Mcconn-Walsh, R. (2012). Virtual reality rehabilitation of balance: assessment of the usability of the Nintendo Wii((R)) Fit plus. Disabil. Rehabil. Assist. Technol. 7, 205–210. doi:10.3109/17483107.2011.616922
Mhatre, P. V., Vilares, I., Stibb, S. M., Albert, M. V., Pickering, L., Marciniak, C. M., et al. (2013). Wii Fit balance board playing improves balance and gait in Parkinson disease. PM R 5, 769–777. doi:10.1016/j.pmrj.2013.05.019
Miller, K. J., Adair, B. S., Pearce, A. J., Said, C. M., Ozanne, E., and Morris, M. M. (2014). Effectiveness and feasibility of virtual reality and gaming system use at home by older adults for enabling physical activity to improve health-related domains: a systematic review. Age Ageing 43, 188–195. doi:10.1093/ageing/aft194
Mirelman, A., Maidan, I., Herman, T., Deutsch, J. E., Giladi, N., and Hausdorff, J. M. (2011). Virtual reality for gait training: can it induce motor learning to enhance complex walking and reduce fall risk in patients with Parkinson’s disease? J. Gerontol. A Biol. Sci. Med. Sci. 66, 234–240. doi:10.1093/gerona/glq201
Moore, D. J., West, A. B., Dawson, V. L., and Dawson, T. M. (2005). Molecular pathophysiology of Parkinson’s disease. Annu. Rev. Neurosci. 28, 57–87. doi:10.1146/annurev.neuro.28.061604.135718
Moseley, A. M., Herbert, R. D., Sherrington, C., and Maher, C. G. (2002). Evidence for physiotherapy practice: a survey of the physiotherapy evidence database (PEDro). Aust. J. Phys. 48, 43–49. doi:10.1016/S0004-9514(14)60281-6
Nova, I. C., Monica, R. P., and Henrique, B. F. (2004). Levodopa effect upon functional balance of Parkinson’s disease patients. Park. Rel. Dis. 10, 411–415. doi:10.1016/j.parkreldis.2004.04.004
Park, E.-C., Kim, S.-G., and Lee, C.-W. (2015). The effects of virtual reality game exercise on balance and gait of the elderly. J. Phys. Ther. Sci. 27, 1157–1159. doi:10.1589/jpts.27.1157
Podsiadlo, D., and Richardson, S. (1991). The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J. Am. Geriatr. Soc. 39, 142–148. doi:10.1111/j.1532-5415.1991.tb01616.x
Pompeu, J. E., Dos Santos Mendes, F. A., Da Silva, K. G., Lobo, A. M., De Paula Oliveira, T., Zomignani, A. P., et al. (2012). Effect of Nintendo Wii™-based motor and cognitive training on activities of daily living in patients with Parkinson’s disease: a randomised clinical trial. Physiotherapy 98, 196–204. doi:10.1016/j.physio.2012.06.004
Ravenek, K. E., Wolfe, D. L., and Hitzig, S. L. (2015). A scoping review of video gaming in rehabilitation. Disabil. Rehabil. Assist. Technol. 1–9. doi:10.3109/17483107.2015.1029538
Rendon, A. A., Lohman, E. B., Thorpe, D., Johnson, E. G., Medina, E., and Bradley, B. (2012). The effect of virtual reality gaming on dynamic balance in older adults. Age Ageing 41, 549–552. doi:10.1093/ageing/afs053
Scandalis, T. A., Bosak, A., Berliner, J. C., Helman, L. L., and Wells, M. R. (2001). Resistance training and gait function in patients with Parkinson’s disease. Am J Phys Med Rehab 80, 38–43.
Seidler, R. D., and Martin, P. E. (1997). The effects of short term balance training on the postural control of older adults. Gait Posture 6, 224–236. doi:10.1016/S0966-6362(97)00012-X
Singh, D. K., Rajaratnam, B. S., Palaniswamy, V., Raman, V. P., Bong, P. S., and Pearson, H. (2013). Effects of balance-focused interactive games compared to therapeutic balance classes for older women. Climacteric 16, 141–146. doi:10.3109/13697137.2012.664832
Singh, N., Pillay, V., and Choonara, Y. E. (2007). Advances in the treatment of Parkinson’s disease. Prog. Neurobio. 81, 29–44. doi:10.1016/j.pneurobio.2006.11.009
Thorbahn, L. D. B., and Newton, R. A. (1996). Use of the Berg balance test to predict falls in elderly persons. Phys. Ther. 76, 576–583.
Toulotte, C., Toursel, C., and Olivier, N. (2012). Wii Fit® training vs. adapted physical activities: which one is the most appropriate to improve the balance of independent senior subjects? A randomized controlled study. Clin. Rehabil. 26, 827–835. doi:10.1177/0269215511434996
Wood, B., Bilclough, J., Bowron, A., and Walker, R. (2002). Incidence and prediction of falls in Parkinson’s disease: a prospective multidisciplinary study. J. Neurol. Neurosurg. Psych. 72, 721–725. doi:10.1136/jnnp.72.6.721
Wuest, S., Borghese, N. A., Pirovano, M., Mainetti, R., Van De Langenberg, R., and De Bruin, E. D. (2014). Usability and effects of an exergame-based balance training program. Games Health J. 3, 106–114. doi:10.1089/g4h.2013.0093
Yen, C. Y., Lin, K. H., Hu, M. H., Wu, R. M., Lu, T. W., and Lin, C. H. (2011). Effects of virtual reality-augmented balance training on sensory organization and attentional demand for postural control in people with Parkinson disease: a randomized controlled trial. Phys. Ther. 91, 862–874. doi:10.2522/ptj.20100050
Keywords: Parkinson’s, balance, exergaming, older, adults
Citation: Harris DM, Rantalainen T, Muthalib M, Johnson L and Teo W-P (2015) Exergaming as a viable therapeutic tool to improve static and dynamic balance among older adults and people with idiopathic Parkinson’s disease: a systematic review and meta-analysis. Front. Aging Neurosci. 7:167. doi: 10.3389/fnagi.2015.00167
Received: 03 July 2015; Accepted: 17 August 2015;
Published: 07 September 2015
Edited by:
Atsushi Takeda, National Hospital Organization, JapanReviewed by:
Hideyuki Sawada, Clinical Research Center, JapanPatrick Ragert, Max Planck Institute for Human Cognitive and Brain Sciences Leipzig, Germany
Copyright: © 2015 Harris, Rantalainen, Muthalib, Johnson and Teo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wei-Peng Teo, Centre for Physical Activity and Nutrition Research, School of Exercise and Nutrition Science, Deakin University, 221 Burwood Highway, Burwood, VIC 3125, Australia, weipeng.teo@deakin.edu.au
 Dale M. Harris
Dale M. Harris Timo Rantalainen1
Timo Rantalainen1
 Makii Muthalib
Makii Muthalib Liam Johnson
Liam Johnson Wei-Peng Teo
Wei-Peng Teo