Long-Term Outcomes after Stroke in Elderly Patients with Atrial Fibrillation: A Hospital-Based Follow-Up Study in China
- 1Department of Cell Biology, Harbin Medical University, Harbin, China
- 2Department of Neurology, The First Affiliated Hospital of Jiamusi University, Heilongjiang, China
- 3Department of Community Health, Land Reclamation General Hospital, Harbin, China
- 4Department of Neurology, Capital Medical University Affiliated Friendship Hospital, Beijing, China
- 5Department of Neurology, The Second Affiliated Hospital of Harbin Medical University, Harbin, China
Background: Atrial fibrillation (AF) significantly increases the risk of stroke and disease burden; it is an established predictor of poor outcomes after stroke. However, reported differences in outcomes after stroke among elderly patients between AF and non-AF group are conflicting. We aimed to compare differences in outcomes at 1 year and 3 years after stroke among elderly patients (aged ≥ 75 years old) between AF group and non-AF group.
Methods: We recruited 1070 consecutive elderly patients who experienced acute ischemic stroke between January 2008 and December 2013 in Jiamusi University First Hospital, China in this study. Information regarding stroke subtype, severity, risk factors, and outcome (mortality, dependency, and recurrence) at 3 and 12 months after stroke were recorded and assessed between AF group and non-AF group.
Results: The prevalence of AF was 16.1% overall, with a similar trend in the prevalence of AF between men and women. The AF group were more likely to experience severe stroke compared to the non-AF group (32.0 vs. 11.9%, respectively; P < 0.001). There were no obvious differences between groups regarding the prevalence of hypertension, dyslipidemia, obesity, current smoking, and alcohol drinking but there was a higher prevalence of diabetes in the non-AF group (20.3 vs. 30.1%, P = 0.010). Mortality and dependency rates were significantly higher in the AF group than in the non-AF group at 1 year after stroke (29.6 vs. 17.8%, P = 0.001 for mortality; and 59.5 vs. 36.1%, P = 0.010 for dependency) and 3 years after stroke (46.1 vs. 33.2%, P = 0.032 for mortality; and 70.7 vs. 49.2%, P = 0.010 for dependency); however, there was no significant between-groups differences in rates of recurrence across the follow-up periods. The results for dependency remained stable after adjustment for sex, stroke severity, and stroke risk factors at 3 years after stroke (OR, 2.26; 95% CI, 1.06–4.81; P = 0.034); however, the relationship between AF and mortality and recurrence disappeared after adjusting for these covariates
Conclusion: These findings suggest that it is crucial to highlight the treatment of elderly stroke patients with AF in order to reduce poor outcomes among the elderly and to reduce the burden of AF in China.
Introduction
Stroke was the second most common cause of death and the third most common cause of reduced disability-adjusted life-years (DALYs) worldwide in 2010 (Lozano et al., 2012). Stroke incidence has declined in industrialized countries over the last 30 years, but it has recently become the leading cause of death in rural areas and the third cause of death in urban areas in China (Lloyd-Jones et al., 2009, 2010; Redon et al., 2011; The Ministry of Health of the People's Republic of China, 2011).
Atrial fibrillation (AF) is the most common sustained cardiac arrhythmia. It is an independent risk factor for stroke and is associated with marked morbidity, mortality, and socioeconomic burden (Wolf et al., 1991, 1998; Chugh et al., 2001). It confers a five- to six-fold increased risk for ischemic stroke (Romero and Wolf, 2013). The prevalence of AF increases substantially with advancing age (Kannel et al., 1998). Aging is the most important non-modifiable risk factor for stroke (Murray and Lopez, 1997; Lloyd-Jones et al., 2009). Moreover, older patients reportedly have poor functional outcomes after stroke (Palnum et al., 2008; Saposnik et al., 2008; Fonarow et al., 2010; Soares et al., 2011; Deng et al., 2012). Although there is a low prevalence of AF in China, the disease burden of AF-related stroke is great due to the aging population. It is predicted that the number of people aged >60 years worldwide is estimated to increase to 1.2 billion by 2025, double the number of people who were in this age group in 1995 (Krug et al., 2002). The number of people aged ≥65 years in China was 200 million in 2014 (Peilin et al., 2014), and 3.5% of the population was ≥75 years old in 2013 (National Bureaus of Statistics of the People's Republic of China, 2014). Thus, with the aging of the worldwide population, stroke has become a major public health problem.
Stroke patients with AF have been reported to have higher mortality compared to stroke patients without AF, with rates between 30.5 and 63.0% at 12 months after stroke (Kolominsky-Rabas et al., 2001; Roquer et al., 2003; Banks and Marotta, 2007; Saposnik et al., 2008). In addition, worse neurological function has been reported in stroke patients with AF (Stuart-Shor et al., 2009). However, long-term outcomes after stroke in elderly patients with AF are uncertain in China.
Therefore, in this study, we aimed to compare differences in long-term outcomes, including mortality, dependency, and recurrence rates after stroke, between elderly stroke patients with AF and those without AF.
Materials and Methods
This study used data from a stroke registry in the Department of Neurology, Jiamusi University First Hospital, China; the inclusion criteria for stroke patients have been described in a previous study (Wu et al., 2015). Briefly, we prospectively collected data on the clinical characteristics and outcomes for all ischemic stroke patients who were admitted to the Department of Neurology, Jiamusi University First Hospital, China between January 2008 and December 2013. Stroke events were defined according to the World Health Organization's criteria, and all cases of stroke were confirmed by neuroimaging (1989). Patients with transient ischemic attack were excluded from this study, and all stroke patients aged 75 years and over were included. AF was defined as a history of AF, confirmed by at least one electrocardiogram or the presence of arrhythmia during hospitalization.
The ethics committee of Jiamusi University First Hospital approved the study, and written informed consent was obtained from all patients or their next-of-kin.
Data collection and outcome evaluation were performed by senior neurologists who used standardized variable definitions and scores. Stroke subtypes, which were classified on admission, included total anterior circulation infarcts, partial anterior circulation infarcts, lacunar infarcts, and posterior circulation infarcts, according to Oxfordshire Community Stroke Project criteria (Bamford et al., 1991). Stroke severity was categorized into three groups according to National Institutes of Health Stroke Scale (NIHSS) scores: mild (NIHSS score: ≤ 7), moderate (NIHSS score: 8–16), and severe (NIHSS score: ≥17) (Kim et al., 2010). Receiving oral anticoagulants was defined as receiving oral anticoagulants before stroke onset. General stroke risk factors, including hypertension, diabetes mellitus (DM), and hyperlipidemia, were defined according to self-reported previous medical history, and obesity was defined as a body mass index ≥30 kg/m2. The NIHSS score and Barthel Index (BI) were evaluated on admission and at discharge; the modified Rankin Scale (mRS) score was assessed on admission, at discharge, and at 3 and 12 months after stroke.
Outcomes included mortality, dependency, and recurrence rates at 3 and 12 months after stroke. Mortality was defined as all-cause cumulative death at the corresponding follow-up time point. Stroke recurrence was defined as all new-onset vascular events, including stroke, myocardial infarction, and venous thrombosis. Dependency was defined as an mRS score >2 (Banks and Marotta, 2007). Follow-up was implemented according to a predetermined procedure; the same senior neurologist collected data at 1 year and 3 years after stroke. Follow-up occurred for all patients in a face-to-face interview, except for those patients who were re-examined in their local hospitals, who completed follow-up by telephone.
Patients were divided into two groups—those with AF (the AF group) and those without AF (the non-AF group)—and data were compared between the two groups. Continuous variables, including age, NIHSS score, BI, mRS score, total cholesterol (TC), triglycerides (TG), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), fasting glucose, and glycosylated hemoglobin (HbA1c), were presented as means with standard deviations (or as medians with ranges where appropriate) and were compared between groups using the Student t-test or the Mann-Whitney U test. Dichotomous variables, including stroke severity, stroke risk factors, and outcomes during follow-up after stroke, were presented as number of cases (percentages); the risk factors were compared between groups with the chi-squared test. The relationship between AF and outcomes was assessed with logistic regression analyses and presented as unadjusted odds ratios (ORs) with 95% confidence intervals (CIs). A multivariate analysis between age and outcomes was carried out with a logistic regression analysis, with covariates of stroke severity, previous medical history, and risk factors, and were presented using adjusted ORs with 95% CIs. All statistical analyses were performed using SPSS version 15.0 (SPSS Inc., Chicago, IL), and a two-tailed p < 0.05 indicated statistical significance.
Results
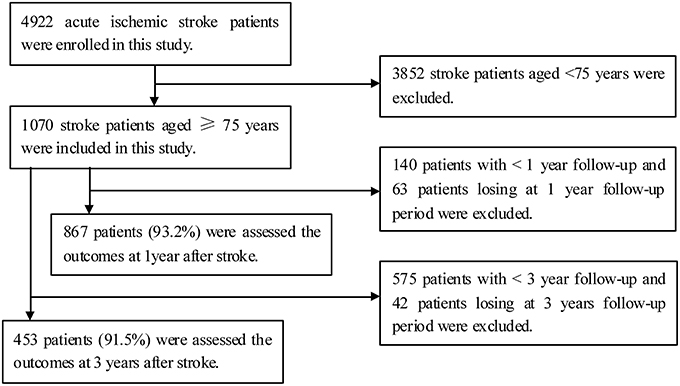
A total of 4922 patients experienced acute ischemic stroke and were hospitalized during the study period; of these, there were1070 patients aged ≥75 years. Outcomes at 1 year post-stroke were available for 867 elderly stroke patients (93.2%), after excluding 63 patients lost to follow-up, and outcomes at 3 years post-stroke were available for 453 elderly stroke patients (91.5%), after excluding 42 patients lost to follow-up (Figure 1).
Overall, 1070 elderly stroke patients were included in this study (172 in the AF group and 898 in the non-AF group); the prevalence of AF was 16.1% overall; similar for men and women (15.0 vs. 17.5%, P = 0.256). The AF group was more likely than the non-AF group to have severe stroke (32.0 vs. 11.9%, P < 0.001), and they had worse neurological function (i.e., they had higher mRS scores but lower BI scores). The levels of TC, TG, HDL-C, LDL-C, fasting glucose, and HbA1c were not significantly different between the two groups. There were no obvious differences in the prevalence of hypertension, DM, dyslipidemia, obesity, and current smoking between the two groups, but there was a higher prevalence of diabetes in the non-AF group (Table 1).
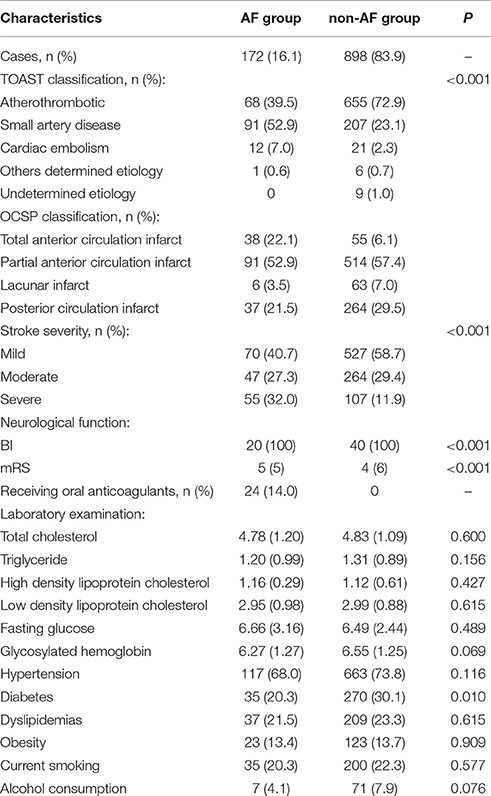
Table 1. The clinical features and previous history of diseases in elderly ischemic stroke patients by AF.
Mortality was significantly higher in the AF group than in the non-AF group at 1 year after stroke (29.6 vs. 17.8%, P = 0.010) and at 3 years after stroke (46.1 vs. 33.2%, P = 0.032), respectively. Similar trends were found for the dependency (49.5 vs. 36.1% at 1 year after stroke and 70.7 vs. 49.2% at 3 years after stroke (all P < 0.001). However, there were no significant differences in recurrence rates between the two groups across the follow-up periods. The results for dependency remained stable after adjustment for sex, stroke severity, and stroke risk factors at 3 years after stroke (OR, 2.26; 95% CI, 1.06–4.81; P = 0.034); however, the relationship between AF and mortality and recurrence disappeared after adjusting for these covariates (Table 2).
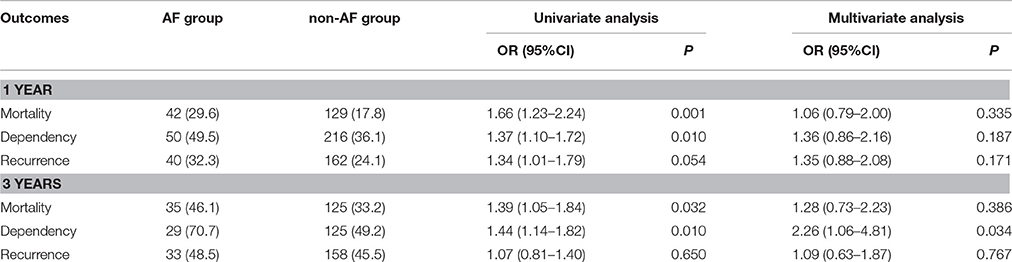
Table 2. The outcomes and OR at 1 year and 3 years after stroke among elderly stroke patients by AF.
Discussion
To our knowledge, this is the first report of the effects of AF on outcomes among elderly stroke patients in China. In this study, we compared the differences in clinical features, conventional stroke risk factors, and outcomes at 1 year and 3 years after stroke among elderly stroke patients with and without AF.
A previous study indicated that, compared to stroke patients without AF, those with AF were less likely to have conventional risk factors for stroke (including hypertension, DM, current smoking, and alcohol consumption Sun et al., 2015), were slightly more likely to experience a recurrent ischemic stroke or intracranial hemorrhage within 2 weeks, and were more than twice as likely to die within 2 weeks to 6 months (Mattle, 2003). Consistent with these studies, there was a higher frequency of severe stroke, and worse neurological function in the AF group than in the non-AF group in this study.
Regarding risk factors for stroke in patients with AF, conclusions are widely divergent due to the different study designs used. The previous study indicated that stroke patients with AF were less likely to have the conventional risk factors for stroke, including hypertension, diabetes mellitus, current smoking, and alcohol consumption habits (Lamassa et al., 2001; Mizrahi et al., 2014), but significant differences in the frequency of conventional stroke risk factors were reported in others (Andrew et al., 2014). In the present study, the prevalence of hypertension, dyslipidemia, obesity, current smoking, and alcohol consumption was not significantly different between the two groups, but there was a higher frequency of diabetes in the non-AF group, as reported in the prior study (Lamassa et al., 2001; Mizrahi et al., 2014).
Previous studies have demonstrated that elderly stroke patients were more likely, compared to younger stroke patients, to have poor outcomes after acute ischemic stroke, including increased short-term and long-term mortality rates, dependency rates, and a higher risk of stroke recurrence (Johnston et al., 2002; Kammersgaard et al., 2004; Marini et al., 2004; Rothwell et al., 2005; Palnum et al., 2008; Fonarow et al., 2010; Romero and Wolf, 2013). Elderly acute ischemic stroke patients have poorer outcomes overall (Candelise et al., 1991), these are associated with an enhanced susceptibility to the secondary degeneration in the primary ischemic lesion (Loubinoux et al., 2012). Stroke patients are at highest risk of death in the first weeks after the event, and between 20 and 50% die within the first month depending on type, severity, age, co-morbidity and effectiveness of treatment of complications. Patients who survive may be following with no disability or with mild, moderate or severe disability. However, patients with a history of stroke are at risk of a subsequent event of around 10% in the first year and 5% per year thereafter (Sandu et al., 2015). Moreover, vascular risk factors, including hypertension, obesity, diabetes, dyslipidaemia, hyperhomocystaeinemia, and systemic inflammation increase the probability of silent strokes (Burn et al., 1994).
Findings related to the effects of AF on outcomes in stroke patients have been inconsistent, but most previous studies have reported that AF is associated with higher mortality rates (Candelise et al., 1991; Gustaffson and Britton, 1991; Jørgensen et al., 1996; Lin et al., 1996). A few studies indicated a higher recurrence rate in stroke patients with AF (Sandercock et al., 1992; Lin et al., 1996) and a markedly increased dependency (Karataş et al., 2000). In the present study, we found that there was higher rate of dependency among elderly patients with AF at 3 years after stroke. However, in contrast to previous reports, we found no differences in mortality and recurrence rates between the groups at 1 year and 3 years after stroke. The higher frequency of severe stroke may contribute to the higher rate of dependency among elderly stroke patients with AF, but similar rates of mortality and recurrence among elderly stroke patients across AF groups may be a result of older age (Karataş et al., 2000), and similar frequency of conventional stroke risk factors between the AF group and the non-AF group may partly explain the identical rates of mortality and recurrence among elderly patients (Sandu et al., 2015).
The limitation of this study is that it was a hospital-based study, which might not reflect the general population in China. Furthermore, patients for whom the stroke was fatal, i.e., who died before being hospitalized, were not included in this study. Therefore, there was a relatively low prevalence of AF in this study.
Conclusion
In this single-hospital-based stroke registry, we compared differences in clinical features, risk factors, and outcomes at 1 year and 3 years post-stroke among elderly stroke patients with and without AF. There was a higher frequency of severe stroke in the AF group than in the non-AF group. While the prevalence of hypertension, dyslipidemia, obesity, current smoking, and alcohol consumption was not obviously different between the two groups, there was a higher frequency of DM in the non-AF group. There was a significantly higher dependency rate at 3 years after stroke in the AF group, but not in mortality rates or recurrence rates across the follow-up periods. These findings suggest that it is crucial to highlight the treatment of elderly stroke patients with AF in order to reduce poor outcomes among the elderly and to reduce the burden of AF in China.
Author Contributions
SW, CZ, and YGZ contributed to the conception and design of the work; YGZ, CZ, CW, YBZ, and SW contributed the data acquisition; YGZ and CZ contributed the analysis and interpretation of data for the work; YGZ contributed to the drafting of the work; and CZ and SW revised the work for important intellectual content. All authors approved of the final version to be submitted and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Funding
This study was supported by Scientific Research Item of Health Department in Heilongjiang Province (contract number: 2011-076) and Youth Science Funds of Heilongjiang Province (contract number: QC2011C130).
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Abbreviations
AF, atrial fibrillation; BI, Barthel Index; CI, confidence interval; DM, diabetes mellitus; HbA1c, glycosylated hemoglobin; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; mRS, modified Rankin scale; NIHSS, National Institutes of Health Stroke Scale; OR, odds ratio; TC, total cholesterol; TG, triglycerides.
References
Andrew, N., Kilkenny, M., Harris, D., Price, C., and Cadilhac, D. A. (2014). Outcomes for people with atrial fibrillation in an Australian national audit of stroke care. Int. J. Stroke 9, 270–277. doi: 10.1111/ijs.12087
Bamford, J., Sandercock, P., Dennis, M., Burn, J., and Warlow, C. (1991). Classification and natural history of clinically identifiable subtypes of cerebral infarction. Lancet 337, 1521–1526. doi: 10.1016/0140-6736(91)93206-O
Banks, J. L., and Marotta, C. A. (2007). Outcomes validity and reliability of the modified Rankin scale: implications for stroke clinical trials: a literature review and synthesis. Stroke 38, 1091–1096. doi: 10.1161/01.STR.0000258355.23810.c6
Burn, J., Dennis, M., Bamford, J., Sandercock, P., Wade, D., and Warlow, C. (1994). Long-term risk of recurrent stroke after a first-ever stroke. The Oxfordshire Community Stroke Project. Stroke 25, 333–337. doi: 10.1161/01.STR.25.2.333
Candelise, L., Pinardi, G., Moratibo, A., and the Italian Stroke Study Group (1991). Mortality in acute stroke with atrial fibrillation. Stroke 22, 169–174.
Chugh, S. S., Blackshear, J. L., Shen, W. K., Hammill, S. C., and Gersh, B. J. (2001). Epidemiology and natural history of atrial fibrillation: clinical implications. J. Am. Coll. Cardiol. 37, 371–378. doi: 10.1016/S0735-1097(00)01107-4
Deng, Y. X., Wang, Y. L., Gao, B. Q., Wang, C. X., Zhao, X. Q., Liu, L. P., et al. (2012). Age differences in clinical characteristics, health care, and outcomes after ischemic stroke in China. CNS Neurosci. Ther. 18, 819–826. doi: 10.1111/j.1755-5949.2012.00378.x
Fonarow, G. C., Reeves, M. J., Zhao, X., Olson, D. M., Smith, E. E., Saver, J. L., et al. (2010). Age-related differences in characteristics, performance measures, treatment trends, and outcomes in patients with ischemic stroke. Circulation 121, 879–891. doi: 10.1161/CIRCULATIONAHA.109.892497
Gustaffson, C., and Britton, M. (1991). Pathogenetic mechanism of stroke in non-valvular atrial fibrillation: follow-up of stroke patients with and without atrial fibrillation. J. Intern. Med. 230, 11–16.
Johnston, S. C., Gress, D. R., Browner, W. S., and Sidney, S. (2002). Short-term prognosis after emergency diagnosis of TIA. JAMA 284, 2901–2906. doi: 10.1001/jama.284.22.2901
Jørgensen, H. S., Nakayama, H., Raaschau, H. O., and Olsen, T. S. (1996). Acute stroke with atrial fibrillation: the copenhagen stroke study. Stroke 27, 1765–1769. doi: 10.1161/01.STR.27.10.1765
Kammersgaard, L. P., Jørgensen, H. S., Reith, J., Nakayama, H., Pedersen, P. M., Olsen, T. S., et al. (2004). Short- and long-term prognosis for very old stroke patients: copenhagen stroke study. Age Ageing 33, 149–154. doi: 10.1093/ageing/afh052
Kannel, W. B., Wolf, P. A., Benjamin, E. J., and Levy, D. (1998). Prevalence, incidence, prognosis, and predisposing conditions for atrial fi brillation: population-based estimates. Am. J. Cardiol. 82, 2N–9N. doi: 10.1016/S0002-9149(98)00583-9
Karataş, M., Dilek, A., Erkan, H., Yavuz, N., Sözay, S., and Akman, N. (2000). Functional outcome in stroke patients with atrial fibrillation. Arch. Phys. Med. Arch. Phys. Med. Rehabil. 81, 1025–1029. doi: 10.1053/apmr.2000.6981
Kim, J. S., Lee, K. B., Roh, H., Ahn, M. Y., and Hwang, H. W. (2010). Gender differences in the functional recovery after acute stroke. J. Clin. Neurol. 6, 183–188. doi: 10.3988/jcn.2010.6.4.183
Kolominsky-Rabas, P. L., Weber, M., Gefeller, O., Neundoerfer, B., and Heuschmann, P. U. (2001). Epidemiology of ischemic stroke subtypes according to TOAST criteria—incidence, recurrence, and long-term survival in ischemic stroke subtypes: a population-based study. Stroke 32, 2735–2740. doi: 10.1161/hs1201.100209
Krug, E. G., Mercy, J. A., Dahlberg, L. L., and Zwi, A. B. (2002). The world report on violence and health. Lancet. 360, 1083–1088. doi: 10.1016/S0140-6736(02)11133-0
Lamassa, M., Di Carlo, A., Pracucci, G., Basile, A. M., Trefoloni, G., Vanni, P., et al. (2001). Characteristics, outcome, and care of stroke associated with atrial fibrillation in Europe data from a multicenter multinational hospital–based registry (the european community stroke project). Stroke 32, 392–398. doi: 10.1161/01.STR.32.2.392
Lin, H. J., Wolf, P. A., Kelly-Hayes, M., Beiser, A. S., 38. Kase, C. S., Benjamin, E. J., et al. (1996). Stroke severity in atrial fibrillation: the Framingham Study. Stroke 27, 1760–1764.
Lloyd-Jones, D., Adams, R., Carnethon, M., De Simone, G., Ferguson, T. B., Flegal, K., et al. (2009). Heart disease and stroke statistics–2009 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 119, 480–486. doi: 10.1161/CIRCULATIONAHA.108.191261
Lloyd-Jones, D. M., Hong, Y., Labarthe, D., Mozaffarian, D., Appel, L. J., Van Horn, L., et al. (2010). Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association's strategic Impact Goal through 2020 and beyond. Circulation 121, 586–613. doi: 10.1161/CIRCULATIONAHA.109.192703
Loubinoux, I., Kronenberg, G., Endres, M., Schumann-Bard, P., Freret, T., Filipkowski, R. K., et al. (2012). Post-stroke depression: mechanisms, translation and therapy. J. Cell. Mol. Med. 16, 1961–1969. doi: 10.1111/j.1582-4934.2012.01555.x
Lozano, R., Naghavi, M., Foreman, K., Lim, S., Shibuya, K., Aboyans, V., et al. (2012). Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380, 2095–2128. doi: 10.1016/S0140-6736(12)61728-0
Marini, C., Baldassarre, M., Russo, T., De Santis, F., Sacco, S., Ciancarelli, I., et al. (2004). Burden of first-ever ischemic stroke in the oldest old: evidence from a population-based study. Neurology 62, 77–81. doi: 10.1212/01.WNL.0000101461.61501.65
Mattle, H. P. (2003). Long-term outcome after stroke due to atrial fibrillation. Cerebrovasc. Dis. 16, 3–8. doi: 10.1159/000069934
Mizrahi, E. H., Fleissig, Y., Arad, M., and Adunsky, A. (2014). Short-term functional outcome of ischemic stroke in the elderly: a comparative study of atrial fibrillation and non-atrial fibrillation patients. Arch. Gerontol. Geriatr. 58, 121–124. doi: 10.1016/j.archger.2013.07.015
Murray, C. J. L., and Lopez, A. D. (1997). Alternative projections of mortality and disability by cause 1990–2020: global burden of disease study. Lancet 349, 1498–1504.
National Bureaus of Statistics of the People's Republic of China (2014). China Statistical Yearbook 2013. Beijing: China Statistics Press.
Palnum, K. D., Petersen, P., Sørensen, H. T., Ingeman, A., Mainz, J., Bartels, P., et al. (2008). Older patients with acute stroke in Denmark: quality of care and shortterm mortality. A nationwide follow-up study. Age Ageing 37, 90–95. doi: 10.1093/ageing/afm134
Peilin, L., Guangjin, C., and Zhang, J. (2014). Social Blue Book: China Social Situation Analysis and Prediction in 2014. Beijing: Social Sciences Academic Press.
Redon, J., Olsen, M. H., Cooper, R. S., Zurriaga, O., Martinez-Beneito, M. A., Laurent, S., et al. (2011). Stroke mortality and trends from 1990 to 2006 in 39 countries from Europe and Central Asia: implications for control of high blood pressure. Eur. Heart J. 32, 1424–1431. doi: 10.1093/eurheartj/ehr045
Romero, J. R., and Wolf, P. A. (2013). Epidemiology of stroke: legacy of the Framingham Heart Study. Glob. Heart 8, 67–75. doi: 10.1016/j.gheart.2012.12.007
Roquer, J., Campello, A. R., and Gomis, M. (2003). Sex differences in first-ever acute stroke. Stroke 34, 1581–1585. doi: 10.1161/01.STR.0000078562.82918.F6
Rothwell, P. M., Coull, A. J., Silver, L. E., Fairhead, J. F., Giles, M. F., Lovelock, C. E., et al. (2005). Population-based study of event-rate, incidence, case fatality, and mortality for all acute vascular events in all arterial territories (Oxford Vascular Study). Lancet 366, 1773–1783. doi: 10.1016/S0140-6736(05)67702-1
Sandercock, P., Bamford, J., Dennis, M., Burn, J., Stattery, J., Jones, L., et al. (1992). Atrial fibrillation and stroke prevalence in different types of stroke and influence on early- and long-term prognosis (Oxfordshire Community Stroke Project). Br. Med. J. 305, 1460–1465. doi: 10.1136/bmj.305.6867.1460
Sandu, R. E., Buga, A. M., Uzoni, A., Petcu, E. B., and Popa-Wagner, A. (2015). Neuroinflammation and comorbidities are frequently ignored factors in CNS pathology. Neural Regen. Res. 10, 1349–1355. doi: 10.4103/1673-5374.165208
Saposnik, G., Hill, M. D., O'Donnell, M., Fang, J., Hachinski, V., Kapral, M. K., et al. (2008). Variables associated with 7-day, 30-day, and 1-year fatality after ischemic stroke. Stroke 39, 2318–2324. doi: 10.1161/STROKEAHA.107.510362
Soares, I., Abecasis, P., and Ferro, J. M. (2011). Outcome of first-ever acute ischemic stroke in the elderly. Arch. Gerontol. Geriat. 53, e81–e87. doi: 10.1016/j.archger.2010.06.019
Stroke-1989, Recommendations on stroke prevention, diagnosis, therapy. (1989). Report of the WHO task force on stroke and other cerebrovascular disorders. Stroke 20, 1407–1431.
Stuart-Shor, E. M., Wellenius, G. A., DelloIacono, D. M., and Mittleman, M. A. (2009). Gender differences in presenting and prodromal stroke symptoms. Stroke 40, 1121–1126. doi: 10.1161/STROKEAHA.108.543371
Sun, G. Z., Guo, L., Wang, X. Z., Song, H. J., Li, Z., Wang, J., et al. (2015). Prevalence of atrial fibrillation and its risk factors in rural China: a cross-sectional study. Int. J. Cardiol. 182, 13–17. doi: 10.1016/j.ijcard.2014.12.063
The Ministry of Health of the People's Republic of China (2011). China Health Statistics Yearbook 2011. Beijing: China Union Medical University Press.
Wolf, P. A., Abbott, R. D., and Kannel, W. B. (1991). Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke 22, 983–988.
Wolf, P. A., Mitchell, J. B., Baker, C. S., Kannel, W. B., and D'Agostino, R. B. (1998). Impact of atrial fibrillation on mortality, stroke, and medical costs. Arch. Intern. Med. 158, 229–234.
Keywords: ischemic stroke, atrial fibrillation, outcomes, risk factors, elderly
Citation: Zhao Y, Zou C, Wang C, Zhang Y and Wang S (2016) Long-Term Outcomes after Stroke in Elderly Patients with Atrial Fibrillation: A Hospital-Based Follow-Up Study in China. Front. Aging Neurosci. 8:56. doi: 10.3389/fnagi.2016.00056
Received: 10 January 2016; Accepted: 08 March 2016;
Published: 29 March 2016.
Edited by:
Ying Xu, The State University of New York at Buffalo, USAReviewed by:
Aurel Popa-Wagner, University of Medicine Rostock, GermanyLaura Lorenzo-López, University of A Coruña, Spain
Copyright © 2016 Zhao, Zou, Wang, Zhang and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shuang Wang, wangshuang99@126.com
†These authors have contributed equally to this work.
 Yuguang Zhao
Yuguang Zhao Chunying Zou
Chunying Zou Cui Wang
Cui Wang Yongbo Zhang4
Yongbo Zhang4  Shuang Wang
Shuang Wang