- 1 Department of Neurosciences, Medical University of South Carolina, Charleston, SC, USA
- 2 Department of Emergency Medicine, Medical University of South Carolina, Charleston, SC, USA
REACH Medical University of South Carolina (MUSC) provides stroke consults via the internet in South Carolina. From May 2008 to April 2011 231 patients were treated with intravenous (IV) thrombolysis and 369 were transferred to MUSC including 42 for intra-arterial revascularization [with or without IV tissue plasminogen activator (tPA)]. Medical outcomes and hemorrhage rates, reported elsewhere, were good (Lazaridis et al., 2011). Here we report operational features of REACH MUSC which covers 15 sites with 2,482 beds and 471,875 Emergency Department (ED) visits per year. Eight Academic Faculty from MUSC worked with 165 different physicians and 325 different nurses in the conduct of 1085 consults. For the 231 who received tPA, time milestones (in minutes) were: Onset to Door: 62 (mean), 50 (median); Door to REACH Consult: 43 and 33, Consult Request to Consult Start: was 9 and 7, Consult Start to tPA Decision: 31 and 25; Decision to Infusion: 20 and 14, and total Door to Needle: 98 and 87. The comparable times for the 854 not receiving tPA were: Onset to Door: 140 and 75; Door to REACH Consult: 61 and 41; Consult Request to Consult Start: 9 and 7, Consult Start to tPA Decision: 27 and 23. While the consultants respond to consult requests in <10, there is a long delay between arrival and Consult request. Tracking of operations indicates if we target shortening Door to Call time and time from tPA decision to start of drug infusion we may be able to improve Door to Needle times to target of <60. The large number of individuals involved in the care of these patients, most of whom had no training in REACH usage, will require novel approaches to staff education in ED based operations where turnover is high. Despite these challenges, this robust system delivered tPA safely and in a high fraction of patients evaluated using the REACH MUSC system.
Introduction
South Carolina has one of the highest rates of stroke and many of the strokes occur in smaller communities that lack expert stoke care in their hospitals (Lackland et al., 1998). Stroke can be treated with a clot busting drug (Alteplase) but this drug must be initiated within 3 hours after stroke to have the best chance for benefit and in any case before 4.5 hours (del Zoppo et al., 2009). The American Stroke Association recently published evidence that supported the use of telemedicine for acute stroke (Schwamm et al., 2009a). The Stroke Systems of Care Model (SSCM) recommends implementation of telemedicine to increase access to acute stroke care in neurologically underserved areas (Schwamm et al., 2009b).
Telemedicine systems for stroke are now gaining use, and since rapid treatment is of great importance in stroke, it is of interest that their operations be analyzed to identify possible sources of treatment delays and areas where improvements can be made.
Materials and Methods
The Network, Site Selection, and Initiation
Potential sites were contacted by the Director (Robert J. Adams, MS, MD) based on a number of factors including known interest in improving stroke care, proximity to Medical University of South Carolina (MUSC), prior relationship with MUSC for provision of other services, or professional associations with neurologists in target communities. MUSC had no direct corporate ties with these sites. Service was provided to sites according to two contracts: one contract was with the platform vendor REACH Health, Inc. (Augusta, Georgia) and a separate one was with MUSC (MUSC Neurosciences) for the provision of the neurological consultation. The first contract covered the provision of the cart, technical installation, training and maintenance as well as 24/7 technical support by phone. The second spelled out the relationship whereby MUSC stroke specialists would provide, as credentialed consultants, the consultative services (REACH MUSC based in the Department of Neuroscience). The cost of neurological service (REACH MUSC) was based on total yearly ED volume, a number which we believed to be more readily available and reliable than indices more directly related to stroke. Sites paid a daily “readiness fee,” which was fixed for the term of the contract (typically 2 years) and did not vary with usage.
Remote Evaluation of Acute Ischemic Stroke (REACH) MUSC provided at start of site service initiation a half day clinical training course on stroke emphasizing acute management and given to the site in an enduring medium with the suggestion that all Emergency Department (ED) personnel view the training course when convenient. However, no systematic program of re-education or feedback to the sites as to operational performance was initiated. The sites were told at outset that our preferred mode of operation would be for them to initiate a consult based on the history of stroke like symptoms observed within 8 hours of presentation, regardless of the patient’s current status (e.g., still call even if improved) and to initiate the call at the time the patient is sent to the CT scanner (not after CT has been performed).
Consultation Process
Each spoke has a wireless “REACH cart” (a mobile unit composed of a computer, LCD screen, and camera on wheels) pre-installed in their ED. (The cart, software, and system integration is provided by REACH Health, Inc., of Augusta, Georgia – REACH 3.0 version). When a suspected stroke patient arrives in the ED, the sites are instructed to perform a rapid triage and examination similar to what any stroke center ED would provide. When the patient is sent for a cranial CT the site enters the name, time last seen normal, weight, and blood pressure into the program which then “registers” the patient as an active consult. They then call MUSC Admit Transfer Center (ATC) and request a “REACH Stroke consult.” It is key that the term “REACH” be used to distinguish these from ordinary telephone consultations for transfers and the like which may originate from any location, not just a REACH MUSC site.
The ATC sends out a page and a repeat in 5 minutes and then in 3 minutes until a consultant calls the ATC and is connected to the spoke site. ATC also receives information from sites on patients that are transferred and if needed facilitates helicopter or ambulance transfer.
While in telephone contact the consultant logs into the REACH secure website from any location with internet access. The computer must be a PC, with Active X downloaded but otherwise requires no special outfitting. Logging in requires two security steps which when they are completed delivers the consultant to a webpage where he/she selects the consult to join (if there is more than one in progress), and views the patient information and the video of the patients room in one part of the screen. The camera is equipped with fully adjustable zoom and directional change capability. With the help of the spoke RN, and a speaker phone, the consultant interviews patient, family, ED staff, whomever may be able to provide useful information relevant to the tissue plasminogen activator (tPA) decision. The nurse assists the consultant in performing the NIHSS. The CT scan is “pushed” to the REACH Health, Inc. website and is usually available by the time the NIHSS is completed. The next step is typically a conversation with the spoke ED physician and a decision, ideally a mutual one, about what the consultant will indicate in terms of the advisability of tPA.
Clicking “For tPA” displays a weight based protocol which the consultant approves and is then displayed at the spoke for their use. Clicking “Against tPA” displays a list of contraindication from which the consultant can choose one or more reasons why tPA was not recommended.
The website has spaces for a complex note in “SOAP” format. That is, if the NIHSS is not filled out, a prompt will appear requiring an override but the consultant could proceed without doing the NIHSS although this was discouraged.
Further “decision support” that is built into the REACH 3.0 version includes: (1) time remaining in 3 and 4.5 hour windows; warning if INR is >1.7; (2) reminder to fill out key fields especially NIHSS before closing; (3) reminder to sign consult before closing; (4) Procedure Decision and follow-up items were required before closing the consult; (5) REACH 3.0 software provides a prompt if blood pressure exceeds 185 mm systolic or 115 mm diastolic and informs the consultant for platelets <100 thousand, Partial Thromboplastin Time >40 s, Prothrombin Time >15 s, International Normalized Ratio >1.7 and Blood Glucose <50 mg/dL or >400 mg/dL by displaying a prompt if these limits are violated. Prompts can be manually overridden. There is also a space for entering feedback to the vendor provider or system project manager if either technical or site operational problems are encountered and these comments do not appear on the spoke side or on the final consult. Email notifications are sent at the time of patient registration, time of consult initiation, and completion to any number of prespecified addresses.
The treating physician was the ED physician on site who, after considering the formal MUSC consultants input typically decided among these options: “drip (Alteplase) and transport,” or “drip and keep (hospitalize locally),” or “evaluate (no Alteplase) and transport,” or “evaluate and keep.” Sites could also use REACH MUSC to make the Alteplase decision then send the patient to a facility other than MUSC, but this rarely happened. The REACH MUSC consultants have consulting privileges at each spoke site and include 7 board certified vascular neurologists and 1 emergency medicine physician with extensive stroke interest and experience.
Operational Analysis
The consult form and CT scan, but not the video, are stored long term by REACH Health, Inc. and are available for printing and storage at the site immediately after the consult is completed and closed or for later review as in this report. The consultant can retrieve the consult from the REACH Health, Inc. website immediately and send via email as a PDF, and selected JPEG’s from the CT if desired, to “downstream” caregivers, for example, using a group emailing of the files to physicians at the hub who will be receiving the patient in transfer and provide cell phone numbers of key family members who may be in transit when a crucial follow-up treatment decision, such as intra-arterial clot removal, need to be urgently discussed. To report operational aspects of this program we examined all the REACH consults according to an IRB approved protocol.
Results
Network Configuration
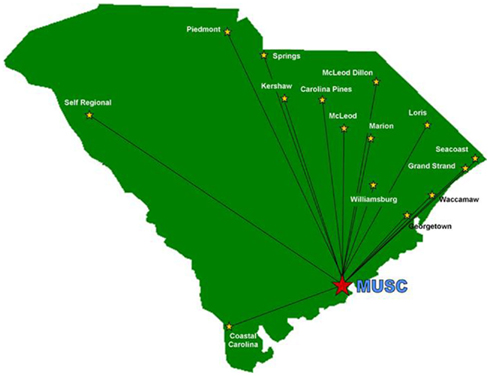
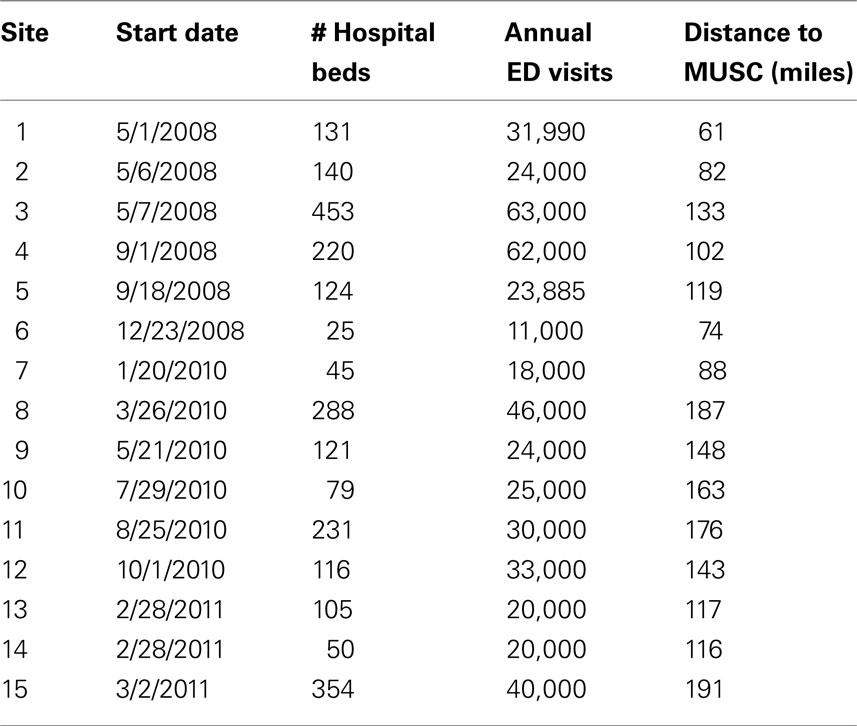
The network configuration as of June 30, 2011 is shown in Figure 1. The closest spoke was 61 miles away and the furthest 191 miles with the average 126 miles. From initial contact and expression of interest to “going live” about 6 months typically elapsed, most of that time spent in contract review and finalization and credentialing of consultants. The system expanded over time so that at the end of 2008 there were 5 spokes, at end of 2009 there were 6, by end of 2010 there were 11 and 15 as of January 3, 2011. The network sites varied in size from a small “critical access” site (Table 1) with 25 beds to a large private non-profit regional medical center with 453 beds.
Summary of Operations
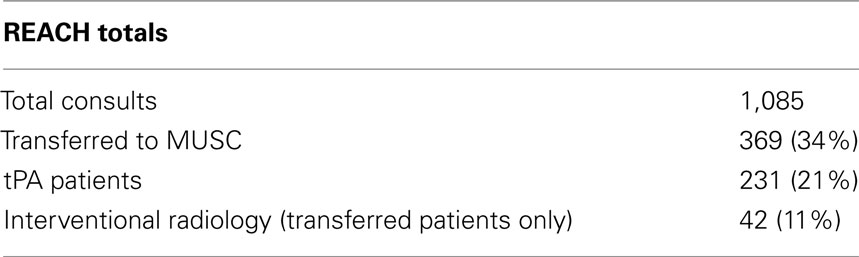
The overall consultation statistics are shown in Table 2. Of the 1,085 patients evaluated, 255 were recommended for treatment with tPA and of this set tPA was initiated in 231 cases. Of the 24 patients that were recommended to receive, but did not get tPA, 9 were the result of patient decision, 5 were due to the family’s preference, 1 had sustained high blood pressure, and 9 were due to unknown/undocumented conditions (probably a clinical improvement post consult). During the conduct of these consults, 156 different physicians initiated a consult and 346 different nurses assisted the consultant.
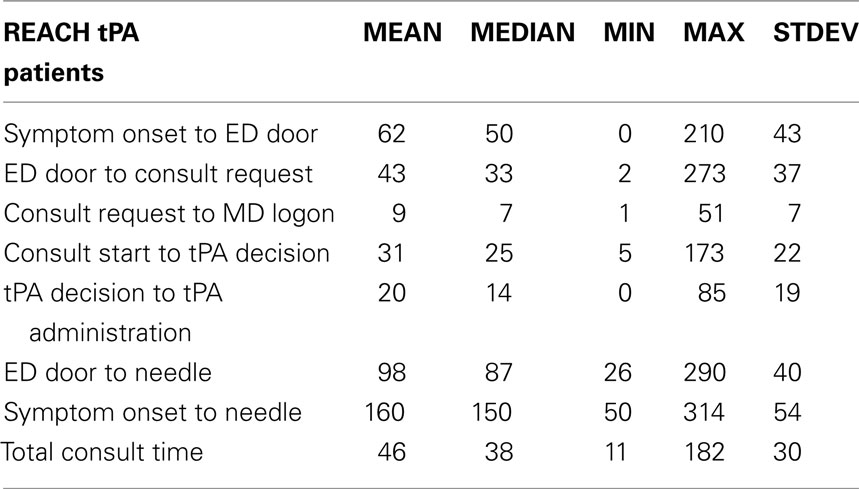
Time milestones are shown in Table 3. We separated the consults into those getting tPA and those who did not to examine the possible impact of informal early “curbside” decisions by the spoke team regarding tPA use (possibly moving more slowly since tPA was not going to be used). The outcomes of those treated with tPA and hemorrhage rates are reported elsewhere. The symptomatic hemorrhage rate was 3% and just over 50% went home. Asymptomatic hemorrhage was discovered in an additional 7% of patients.
Early afternoon during the hour of 12–1:00 pm (n = 76, 7%) was the most likely time for a consult to occur, and the least was 5:00–6:00 am (n = 8, 0.7%; nominal fraction expected would be 4.2%).
For the 231 who received tPA, key time milestones (in minutes) were: Onset to Door: 62 (mean), 50 (median); From when they arrived to when the ATC was called by the spoke (Door to REACH Consult) 43 and 33, Consult Request to Consult Start was 9 and 7, Consult Start to tPA Decision: 31 and 25; Decision to Infusion: 20 and 14, and Door to Needle: 98 and 87. The comparable times for the 854 not receiving tPA were: Onset to Door: 140 and 75; Door To REACH Consult: 61 and 41; Consult Request to Consult Start: 9 and 7, Consult Start to tPA Decision: 27 and 23.
Discussion
These data suggest that tPA facilitated by REACH MUSC, while associated with hemorrhage rates that are well within accepted benchmarks, falls short of reaching the NIHSS guideline of 60 minute Door to Needle time. This analysis pinpoints the operational problems. The symptom onset to door average of 58 minutes means that if we could bring our door to needle time to 60 minutes or less we would be initiating treatment at a median of 2 hours, which would probably lead to better outcomes given what we know about the impact of time to treatment on outcome (Wardlaw et al., 1997).
The main task is reducing the Door to Consult time. The goal over the next year is to bring this key operational value to 15 minutes or less. At the outset a yearly retraining was envisioned but this did not happen because the administrative capacity was consumed in building out the network. As a result there are many individuals involved in the consults who were not part of the initial training. To address this, a newsletter was published in December 2011 and REACH MUSC sites were invited in 2011 to a series of 6 stroke lectures video cast through the statewide Area Health Education Consortium but spoke participation was not tracked.
Conclusion
Door to Needle times in the REACH MUSC network are beyond the target of 60 minutes and need to be reduced. The most likely targets are reduction in “door to call time” and the delay to infusion after tPA is recommended. The many individuals involved in using the service at the spoke end pose special training challenges that may require novel methods.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We are very grateful for the initial support from the Duke Endowment and the Health Sciences of South Carolina (HSSC) and the ongoing support from the Medical University Hospital Authority (MUHA) the Center of Economic Excellence in Stroke (CoEE), MUSC Department of Neurosciences and the Southeastern Virtual Institute for Health Equity and Wellness (SEVIEW) (This research and development project/program is conducted by the Medical University of South Carolina and is made possible by a cooperative agreement that was awarded and administered by the U.S. Army Medical Research and Materiel Command (USAMRMC) and the Telemedicine and Advanced Technology Research Center (TATRC), Fort Detrick, Maryland 21702, under Contract Number: W81XWH-10-2-0057 and W81XWH-11-2-0164) who were all crucial in getting this program underway. The program depends on the dedicated participation and support of nurses, physicians and administrators at the partner sites and also in our own ED at MUSC, on our Neurology residents, on the MUSC Stroke Center team supporting the administrative, clinical and training functions of REACH especially Project Manager Ellen Debenham RN, Project Administrator and Manuscript Developer Corinne Hilbert, Implementation Specialist Lynn Brown and Stroke Program Manager Perette Sabatino RN, the Department of Neuroscience at MUSC especially Monica Gardner and Sunil Patel MD, the Medical University Hospital Authority, the staff of nine East, nine West and the NSICU, the ATC Staff, the MUSC Physician Liaisons, the Neuroscience Service Line, and the REACH MUSC on-call physician team, comprised of the following physicians: Dr. Chalela, Dr. Chimowitz, Dr. Hays, Dr. Holmstedt, Dr. Jauch, Dr. Lazaridis, Dr. Papamitsakis, Dr. Turan, and Dr. Adams. We are also grateful to Genentech, Inc. for providing educational materials to the REACH sites. We express our deep appreciation to our Network partners who have cooperated to improve stroke care in South Carolina including: Carolina Pines Regional Medical Center, Coastal Carolina Hospital, Georgetown Memorial Hospital, Grand Strand Regional Medical Center, Kershaw Medical Center, Loris Community Hospital, Marion County Medical Center, McLeod Regional Medical Center, McLeod Medical Center-Dillon, Piedmont Medical Center, Seacoast Medical Center, Self Regional Healthcare, Springs Memorial Hospital, Waccamaw Community Hospital, Williamsburg Regional Hospital.
References
del Zoppo, G. J., Saver, J. L., Jauch, E. C., and Adams, H. P. (2009). Expansion of the time window for treatment of acute ischemic stroke with intravenous tissue plasminogen activator – an advisory statement from the stroke council, american heart association and american stroke association. Stroke 40, 2945–2948.
Lackland, D. T., Bachman, D. L., Carter, T. D., Barker, D. L., Timms, S., and Kohli, H. (1998). The geographic variation in stroke incidence in two areas of the southeastern stroke belt: The Anderson and Pee Dee stroke study. Stroke 29, 2061–2068.
Lazaridis, C., Desantis, S. M., Jauch, E. C., and Adams, R. J. (2011). Telestroke in South Carolina. J. Stroke Cerebrovasc Dis. [Epub ahead of print].
Schwamm, L. H., Holloway, R. G., Amarenco, P., Audebert, H. J., Bakas, T., Chumbler, N. R., Handschu, R., Jauch, E. C., Knight, W. A. IV, Levine, S. R., Mayberg, M., Meyer, B. C., Meyers, P. M., Skalabrin, E., Wechsler, L. R., American Heart Association Stroke Council, and Interdisciplinary Council on Peripheral Vascular Disease. (2009a). A review of the evidence for the use of telemedicine within stroke systems of care: a scientific statement from the American Heart Association/American Stroke Association. Stroke 40, 2616–2634.
Schwamm, L. H., Audebert, H. J., Amarenco, P., Chumbler, N. R., Frankel, M. R., George, M. G., Gorelick, P. B., Horton, K. B., Kaste, M., Lackland, D. T., Levine, S. R., Meyer, B. C., Meyers, P. M., Patterson, V., Stranne, S. K., White, C. J., American Heart Association Stroke Council; Council on Epidemiology and Prevention, Interdisciplinary Council on Peripheral Vascular Disease, and Council on Cardiovascular Radiology and Intervention (2009b). Recommendations for the implementation of telemedicine within stroke systems of care: a policy statement from the American Heart Association. Stroke 40, 2635–2660.
Keywords: telemedicine, stroke, thrombolysis, thrombectomy, network, access to care
Citation: Adams RJ, Debenham E, Chalela J, Chimowitz M, Hays A, Hill C, Holmstedt C, Jauch E, Kitch A, Lazaridis C and Turan TN (2012) REACH MUSC: a telemedicine facilitated network for stroke: initial operational experience. Front. Neur. 3:33. doi: 10.3389/fneur.2012.00033
Received: 05 October 2011; Accepted: 19 February 2012;
Published online: 14 March 2012.
Edited by:
Bart M. Demaerschalk, Mayo Clinic, USAReviewed by:
Bart M. Demaerschalk, Mayo Clinic, USATimothy Ingall, Mayo Clinic, USA
Salah Keyrouz, University of Arkansas for Medical Sciences, USA
Copyright: © 2012 Adams, Debenham, Chalela, Chimowitz, Hays, Hill, Holmstedt, Jauch, Kitch, Lazaridis and Turan. This is an open-access article distributed under the terms of the Creative Commons Attribution Non Commercial License, which permits non-commercial use, distribution, and reproduction in other forums, provided the original authors and source are credited.
*Correspondence: Robert J. Adams, Department of Neurosciences, MUSC Stroke Center, Medical University of South Carolina, 19 Hagood Avenue, Suite 501, Charleston, SC 29425, USA. e-mail: adamsrj@musc.edu