Pediatric Acute Respiratory Distress Syndrome: Fluid Management in the PICU
- 1Pediatric Intensive Care Unit, Academic Medical Center, Emma Children’s Hospital, Amsterdam, Netherlands
- 2Pediatric Intensive Care Unit, Radboud University Medical Center, Nijmegen, Netherlands
- 3Medical Library, Academic Medical Center, University of Amsterdam, Amsterdam, Netherlands
The administration of an appropriate volume of intravenous fluids, while avoiding fluid overload, is a major challenge in the pediatric intensive care unit. Despite our efforts, fluid overload is a very common clinical observation in critically ill children, in particular in those with pediatric acute respiratory distress syndrome (PARDS). Patients with ARDS have widespread damage of the alveolar–capillary barrier, potentially making them vulnerable to fluid overload with the development of pulmonary edema leading to prolonged course of disease. Indeed, studies in adults with ARDS have shown that an increased cumulative fluid balance is associated with adverse outcome. However, age-related differences in the development and consequences of fluid overload in ARDS may exist due to disparities in immunologic response and body water distribution. This systematic review summarizes the current literature on fluid imbalance and management in PARDS, with special emphasis on potential differences with adult patients. It discusses the adverse effects associated with fluid overload and the corresponding possible pathophysiological mechanisms of its development. Our intent is to provide an incentive to develop age-specific fluid management protocols to improve PARDS outcomes.
Introduction
Pediatric acute respiratory distress syndrome (PARDS) is one of the most challenging disease entities in the pediatric intensive care unit (PICU). PARDS was recently defined by the Pediatric Acute Lung Injury Consensus Conference (PALICC) group as acute-onset hypoxic respiratory failure with new infiltrate(s) on chest radiography not fully explained by cardiac failure or fluid overload (1). This definition is based on the Berlin ARDS definition (2), with several adaptations to more adequately adhere to ARDS specifically occurring in children. Importantly, this includes the use of pulse-oximetry derived data to obtain the SpO2/FiO2 (S/F) ratio and oxygen saturation index (OSI) in the many patients in whom PaO2 measurements are unavailable. Of note, due to the relative novelty of the PALICC definition, the articles included in this review still employ the Berlin or older AECC definition of ARDS.
Patients with PARDS form a heterogeneous population within the PICU. This is due to the large age distribution, as PARDS affects infants to adolescents, and the variety of underlying triggers, such as pneumonia, sepsis, trauma, and aspiration. Importantly, differences in the pathophysiology between PARDS and adult ARDS are likely. This is best illustrated by the lower incidence (2.0–12.8/100,000 person-years versus 17.9–81.0/100,000 person-years) and lower mortality (18–35% versus 27–45%) of ARDS in children as compared with adults (1). Although there are potential age-related differences in lung immune and injury responses (3–5), the precise similarities and disparities in the pathophysiological mechanisms between PARDS and adult ARDS are not fully known. At the same time, the development of treatment strategies for PARDS leans heavily on adult ARDS studies and Bayesian approaches (6), as to circumvent lack of power in pediatric studies. It is needless to say that treating children with modalities tested in adults, while the current literature suggests important differences may exist between PARDS and adult ARDS, is highly undesirable. Further exploration of the specific age-related characteristics in relation to outcomes and treatments of PARDS is therefore highly needed.
Appropriate fluid management has become an important non-pulmonary treatment in the current “best practice” care of adult patients with ARDS. To prevent aggravation of lung edema, it is now generally recommended to avoid positive cumulative fluid balance and treat fluid overload after initial hemodynamic stabilization. Several studies in adult ARDS patients have studied the effect of a restrictive fluid management protocol (7). Most importantly, in the NHLBI Fluid and Catheter Treatment Trial (FACTT), it was demonstrated that an early restrictive fluid management protocol in adults with ARDS was effective in preventing fluid overload, which was associated with improved oxygenation and shorter duration of mechanical ventilation and ICU stay (8). This appears in line with the current adult literature on sepsis, which suggests that although early goal-directed therapy including (aggressive) fluid resuscitation is generally beneficial, it does not always lead to reduced mortality (9–11), and may even be associated with longer hospitalization and higher organ failure scores (11). Hence early fluid resuscitation is most likely beneficial, whereas early fluid overload is not. Several studies in a variety of populations of critically ill children, including those in the general PICU, post heart surgery, and those receiving renal replacement therapy, have also shown a positive association between early fluid overload and adverse outcome (12–17).
In this manuscript, we review the literature on the adverse effects of fluid overload with emphasis on potential physiological differences in fluid homeostasis between children and adults. In addition, we summarize the current evidence for a restrictive fluid management protocol specifically in PARDS by a systematic literature review.
Age and Fluid Overload
In adults, multiple studies in patients with ARDS have indicated higher cumulative fluid balance is associated with worse disease outcome. There is an evident inverse correlation between number of ventilator-free days (VFDs) and cumulative fluid balance (18–23). In two randomized controlled trials comparing conservative and liberal fluid treatment, patients in the conservative fluid treatment arm were shown to have higher number of VFDs (8, 18). The correlation with mortality seems more ambiguous. Mortality has been shown to correlate with increasing cumulative fluid balance (21–23), but controversially not to a restrictive fluid treatment (8, 18). In one of the above mentioned trials, lung injury scores and oxygenation indices were also assessed, which both were significantly better when patients received a more restrictive fluid treatment. Consequently, these patients spent an average of 2.5 days less on ventilation as compared with patients treated in the liberal arm (8).
As mentioned above, there are distinct differences in incidence and outcome between adult ARDS and PARDS. As fluid overload is an important and much prevalent aspect of this disease entity, we deem it likely that physiological differences between adults and children in fluid homeostasis influence the progression and outcome of PARDS. Differences in fluid homeostasis exist between children and adults. In humans, aging is associated with a decrease in total body water (TBW) (24). The TBW exists of extracellular (ECW) and intracellular water (ICW). An often used measure to describe fluid compartments is the ECW/TBW ratio. With aging, the TBW declines from approximately 70% of body weight in infants to 60% in elderly (25). The ECW/TBW ratio initially decreases in childhood, but increases again after adulthood due to a relative increase of the ECW. While the lower ECW/TBW ratio in (young) children, together with a high metabolic rate and insensible loss, is a risk for dehydration, vice versa elderly with a higher ECW/TBW ratio may be more prone for fluid overload. For example, in elderly patients suffering from congestive heart failure, fluid overload is predominantly reflected by an increase in ECW (26). In addition, compensation mechanisms by means of redistribution of water between intracellular and extracellular compartments during fluid loss or overload may vary between children, adults, and elderly (27).
In critically ill children, including those with PARDS, it is likely, although yet hypothetical, that age-dependent changes in ICW and ECW as described above alter their susceptibility for adverse effects in end organs during fluid overload. For example, young children have a large brain to intracranial volume ratio as compared with adults, possibly making them relatively vulnerable to encephalopathy as a result of brain edema by excess of water. This is for example illustrated by the higher susceptibility for cerebral edema accompanying diabetic ketoacidosis in children when compared with adults (28, 29). In the lungs, extravascular water content normalized for body weight, and thus TBW, is higher in children as compared with adults, although it is age-independent when indexed for height (30). One could hypothesize that the relative large lung mass to body weight renders children less prone for development of lung edema by increased hydrostatic pressure during fluid overload. In addition, the rate of alveolar fluid clearance (AFC), which is important for the resolution of lung edema, may differ between children and adults. For example, regulation of expression of the epithelial sodium channel (ENaC), one of the essential epithelial channels for fluid clearance, appears age-dependent in the lungs and kidneys (31–33). ENaC is known to increase shortly before birth, and is implicated to decrease with aging. This indicates that children might have higher expression of ENaC than adults, possibly making them less vulnerable to develop lung edema. Similar age-dependent effects of keratinocyte growth factor on AFC have been suggested (34). Indeed, studies in animal models have indicated juveniles to be less prone to develop lung edema compared with their adult or senescent equivalents (4). Unfortunately, the relative paucity of human and animal studies comparing data from the whole age-spectrum with regard to mechanisms and effects of fluid overload at this point makes it undesirable to elaborate beyond speculation.
Adverse Effects of Fluid Overload
Fluid overload in children with PARDS, and more broadly in all critically ill patients, may have an adverse effect on clinical outcome by leading to interstitial edema resulting in impaired oxygenation and perfusion of several tissues in the human body. Increased hydrostatic pressure as a consequence of intravascular fluid challenge is a major mechanism of this increase in extravascular water content. However, the development of interstitial edema by fluid overload is not solely due to heightened hydrostatic pressure as explained by the Starling forces (35). In addition, it may be explained by the proinflammatory response of the endothelium to increasing intravascular pressure with mechanical stress, which by itself adds to further leakage of proteins and fluid (35–37). Lately, interest is given to a specific part of the endothelium; the glycocalyx. The glycocalyx is a layer lining the luminal side of the endothelium, which consists of a complex web of membrane-bound proteoglycans, glycoproteins, and glycosaminoglycans (GAGs) (38). Degradation of the glycocalyx with shedding of components such as GAGs into the circulation leads to activation of proinflammatory and coagulation pathways resulting in increased endothelial permeability (39, 40). Interestingly, recent studies suggest that intravascular fluid overload may also cause glycocalyx degradation; however, the extent and clinical importance of this effect is yet unclear (41, 42).
Fluid overload can have deleterious consequences for many end organs. In patients with PARDS, the lungs appear particularly affected and the aggravation of lung edema is therefore considered a key mechanism of adverse outcome by fluid overload. Extravascular accumulation of protein-rich edema in the lungs is a hallmark of PARDS and occurs by disruption of the alveolar–capillary barrier. The principal proinflammatory, cell death, and proteolytic and coagulation pathways underlying this increased lung permeability have been reviewed elsewhere (43, 44). As a consequence of this increased alveolar–capillary permeability, patients with PARDS are likely to develop lung edema at a lower hydrostatic pressure threshold as is suggested by early studies in dogs (45, 46). In addition, increased systemic venous pressure as a consequence of fluid loading diminishes the lymphatic drainage, which also decreases the absorption rate of lung edema (47). Importantly, in children with acute respiratory failure, including PARDS, the extravascular lung water content, as measured by hemodynamic volumetric monitoring, correlates with both the extent of fluid overload and lung permeability, and is predictive of survival and duration of mechanical ventilation (48).
Other tissues, especially encapsulated organs such as the kidneys and liver, may be specifically prone for adverse effects of fluid overload by lower perfusion pressures. This could be explained by the capsule acting as an unyielding shield leading to a type of compartment syndrome (49–51). For example, a number of studies have shown that a high cumulative fluid balance is associated with the development of acute kidney injury (AKI) in critically ill patients (52–56). In particular, in the setting of ongoing oliguria despite hemodynamic stabilization, fluid overload may be harmful (49). Moreover, the healing of skin and other tissues, as well as the incidence of gastro-intestinal complications such as ileus, after surgery are negatively affected by interstitial edema resulting from fluid overload (57, 58).
Effect of Fluid Overload in Pards
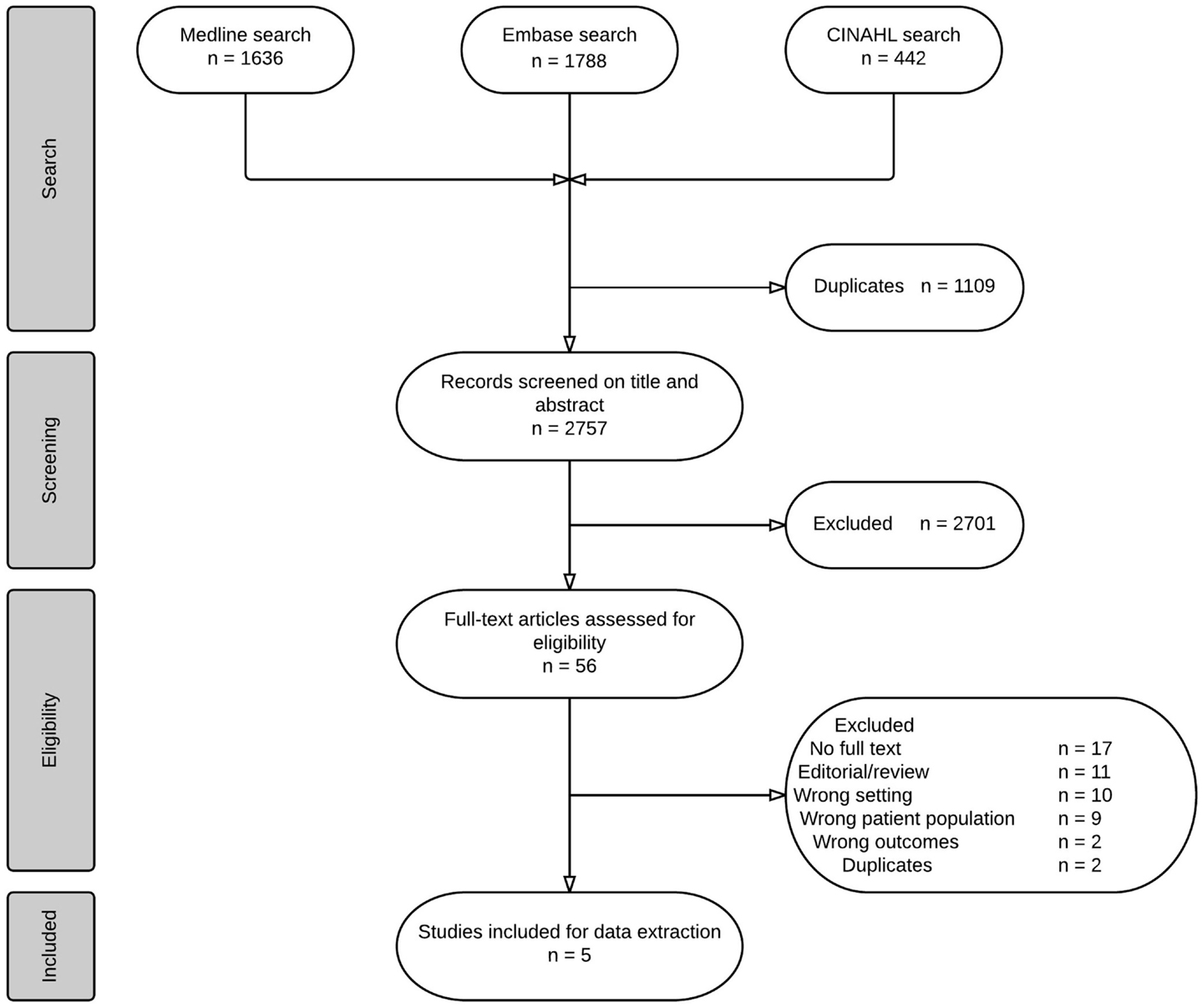
In summary, fluid overload may be associated with negative outcome in critically ill children including those with PARDS, although important differences between children and adults in susceptibility and pathophysiology may exist. In order to address the current evidence that advocates or would support a restrictive fluid management specifically in PARDS, we performed a systematic review as described below. An overview of the search, screening and selection process of the studies can be found in Figure 1. Due to heterogeneity of the data, a meta-analysis was not deemed possible. The systematic literature search and critical appraisal are presented in the supplemental material of this manuscript.
Overview of Included Studies
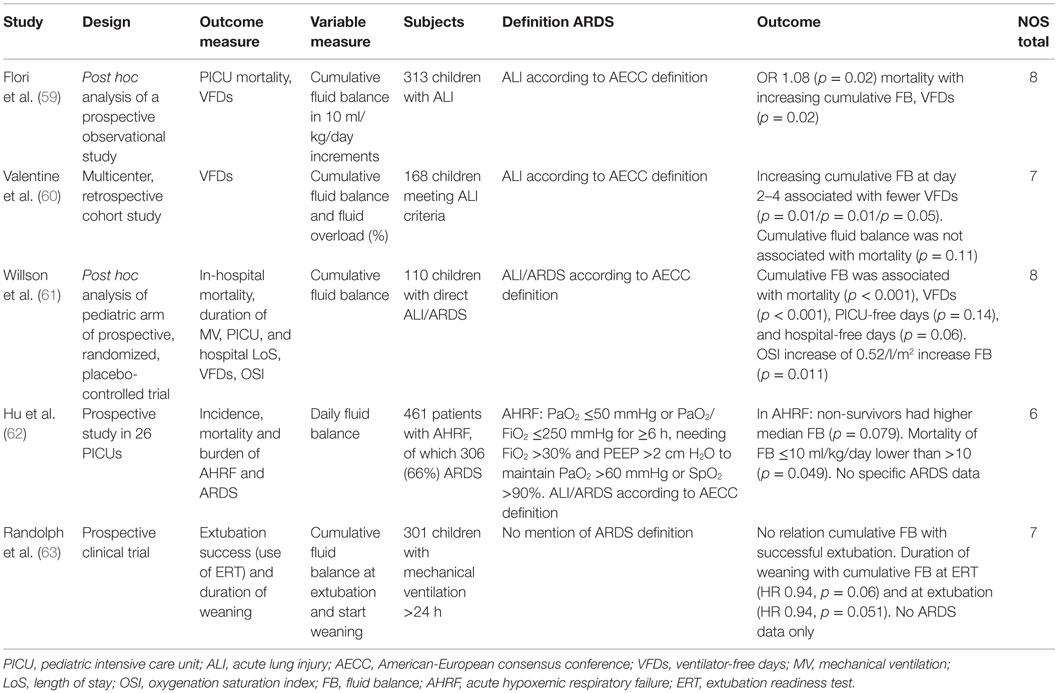
All studies included in this systematic review were part of a prospective or retrospective observational cohort or post hoc analysis. Table 1 holds the descriptions of the included studies. The correlations found between fluid balance and outcomes were broadly similar across the included articles. Table 2 provides a summary of the overall findings.
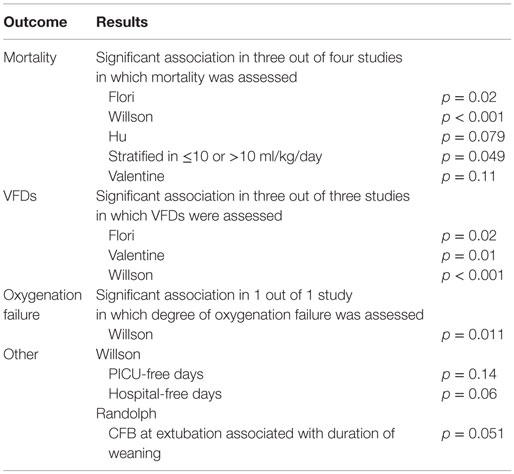
Table 2. Description of findings on correlation between cumulative fluid balance and clinical outcomes.
Mortality was one of the primary outcomes in this systematic review and was reported in most of the included studies. Flori et al. showed that mortality was associated with increasing cumulative fluid balance (grouped in sets of 10 ml/kg/day) in both bivariate and multivariate regression (OR 1.12, 95% CI 1.06–1.20, p < 0.001 and 1.08, 95% CI 1.01–1.15, p = 0.02, respectively) (59). Valentine et al. examined the same association in critically ill children with acute lung injury (ALI) according to the AECC definition of ALI (60). A trend of difference in cumulative fluid balance between survivors and non-survivors was found (p = 0.11). In the post hoc analysis by Willson et al. the increased cumulative fluid balance (as averaged per meter squared of body surface) was associated with in-hospital mortality on days 1–7 (p < 0.001) in children with ALI/ARDS (61). Hu et al. examined children with acute hypoxemic respiratory failure (AHRF) in China (62). A subgroup of these patients (n = 306, 66%) was identified according to the AECC criteria of ARDS. With regard to fluid data, they showed that non-survivors of AHRF had higher median fluid balances, although this was statistically not significant (p = 0.079). The mortality of patients with a daily fluid balance ≤10 ml/kg/day was lower than the group with a balance of >10 ml/kg/day (p = 0.049). There were no fluid data presented of only the ARDS subgroup. The last included study by Randolph et al. on the relation between weaning duration and fluid balance in mechanically ventilated children in the PICU held no data on mortality (63).
The other primary and important outcome measure was the number of VFDs measured at day 28 after admission or duration of ventilation. VFDs were used in three of the five included studies (59–61) and in all three fewer VFDs were associated with higher cumulative fluid balance. Valentine et al. reported that in days 2–4 of admission in the PICU, a higher cumulative fluid balance was associated with fewer VFDs (p = 0.01, 0.01, and 0.05 for days 2, 3, and 4, respectively) (60). Likewise, Willson et al. found the number of VFDs to be significantly inversely related to fluid balance (p < 0.001) (61). The study of Randolph et al. looked at fluid balance during weaning of ventilation and at the time of extubation (63). Their primary outcome was extubation success and secondary outcome was duration of weaning. Fluid balance was assessed at the time when an extubation readiness test (ERT) was performed or at the time of extubation, thus late in the course of disease. Cumulative fluid balance was neither at time of ERT nor at time of extubation associated with successful extubation (p = 0.56 and p = 0.77, respectively). Duration of weaning showed a non-significant relation with higher cumulative fluid balances at ERT (Hazard ratio 0.94, 95% CI 0.87–1.00, p = 0.06); however, it was (marginally) significant when predicted by the cumulative fluid balance values at extubation (Hazard ratio 0.94, 95% CI 0.87–1.00, p = 0.051). An important note to be taken into account when comparing the study of Randolph et al. to the others is that ARDS was not defined explicitly or analyzed separately.
One study found that a higher cumulative fluid balance showed a trend of an association with longer duration of stay in the PICU and hospital (61). This outcome was not addressed in other studies. These authors also compared the oxygenation saturation index (OSI) and fluid balance and found that for every liter per meter square body surface increase in fluid balance, the OSI increased with 0.52 point (p = 0.011) (61).
Clinical Implications
Fluid overload early in PARDS progression seems to have a major impact on recovery. In particular early fluid overload is of main interest, as this seems to negatively affect clinical outcome. Late fluid overload may have a more modest effect on outcome (63), potentially because the cumulative fluid balance curve flattens out after the first few days of admission. Children with other causes of critical illness, such as shock or post-cardiac surgery, have shown the same trend of effect (56, 64). Likewise, in the general PICU population, early fluid overload is associated with longer duration of mechanical ventilation and worse oxygenation (13). The peak of illness, which is usually at or a few days after admission, coincides with the presence of early fluid overload. During this period of critical illness, one could speculate that children are especially vulnerable to the effects of fluid overload. Even more so, the positive fluid balance might enhance inflammatory processes (65), which may contribute to the association with adverse outcomes seen mainly in this first period. Vice versa, inflammation in itself could also worsen fluid accumulation by causing (endothelial) tissue damage (e.g., to the glycocalyx) and increasing permeability in the lungs. For pediatric critical care specialists, it is important to realize that children with PARDS appear particularly vulnerable for developing fluid overload already in the early phase of admission (15, 60). In order to prevent and/or adequately handle early fluid overload in daily practice, it is important to be very aware of the significance of this phenomenon. In particular, fluid treatment should probably be tailored more to the actual needs of patients, taking into account fluid responsiveness not only during resuscitation but also with regard to maintenance fluid therapy during the recovery phase (66).
Even though prevention is always more desirable than treatment, fluid overload is a common problem and needs to be treated. Fluid overload could be partially caused by an excess of fluid treatment or nutrients, which is an important pointer to base new fluid protocols on. To treat fluid overload, critically ill patients, both children and adults, often receive diuretics. In the population of critically ill children, furosemide has been shown to effectively achieve diuresis (67). In the particular setting of hypoproteinemic adult patients with ALI, treatment with the combination of furosemide and albumin improved oxygenation, hemodynamics, and fluid balance (19, 20). In animal models of ALI, furosemide also improved lung injury scores and oxygenation (68). The downside to diuretics is that patients are prone to become drug resistant, in which case increased amounts of the drug, a change of the administration route, or more drugs are needed. Moreover, loop diuretics such as furosemide are not compatible with all drugs, which must be taken into account when prescribing them (69).
Another more invasive method of reducing fluid overload is continuous renal replacement therapy (CRRT) (70). In multiple distinct populations of critically ill children, greater fluid overload at start of CRRT has been associated with mortality, even after adjusting for disease severity (14, 71–74). It is suggested that an earlier start of CRRT may result in better outcome as survivors have significantly less days in the PICU prior to start of CRRT than non-survivors do (71, 74). Sutherland et al. discuss the possibility of a threshold for CRRT initiation. For example, based on the recommendation by the American College of Critical Care Medicine, a threshold of >10% fluid overload is suggested for “an intervention” (14, 75). It seems that the choice of using CRRT to treat fluid overload can be defended; however, the optimal timing for initiation still remains to be elucidated and potential complications should be taken into account.
Although fluid restriction could be one of the strategies to prevent or overcome fluid overload, it is at the same time one of the main impeding factors in achieving energy requirements (76). Accomplishing sufficient nutrition is particularly important to prevent nutritional depletion, muscle wasting, and decreased immune function (70, 76) and is associated with better outcome (77). The development of clear fluid and nutritional protocols will be greatly beneficial in achieving optimal balance in both strategies. A Bayesian statistical approach could be the key to designing a randomized controlled trial in children with enough power to adequately assess the optimal fluid (and nutritional) protocol in children with PARDS. The gross effect of fluid overload seems similar in children and adults; however, the size of the effect cannot be readily compared due to the nature of the retrospective studies in children and lack of prospective randomized trials.
Conclusion
Pediatric acute respiratory distress syndrome is a complex disease entity in need of multimodal therapy, of which fluid treatment is a major component. The current literature on fluid balance in PARDS is sparse but demonstrates that fluid overload is associated with worsening clinical outcome, such as fewer VFDs and worse oxygenation. Varying evidence was found on the relation with mortality and increasing fluid balance. In particular, early fluid overload was found to be of main influence. However, definite evidence by randomizing liberal versus restrictive fluid treatment in PARDS is lacking. This systematic review indicates the overall effect of fluid overload on outcomes is rather similar to the effect seen in adults; however, the size of effect cannot be compared at this time. Given the accumulating evidence for differences in (patho)physiology and outcome between children with PARDS and adults with ARDS, as well as known differences in fluid homeostasis related to aging, further study of the effects of specific tailor made fluid maintenance strategies in PARDS is highly warranted. In particular, the place for early diuretic and renal replacement therapy in order to limit fluid overload need to be explored. Further studies are needed to determine whether development of specific age-related fluid management protocols, taking into account all aspects of PARDS, is essential for optimal treatment of this patient group.
Author Contributions
SI designed the review, conceptualized the systematic literature search, conducted the eligibility screening, assessed the quality of selected studies, extracted data from the selected studies, and drafted the initial manuscript. RA conceptualized the design of the review and critically revised the manuscript. JD conceptualized and performed the systematic literature search and critically revised the manuscript. JL conceptualized the design of the review and critically revised the manuscript. RB designed the review, conducted the eligibility screening, assessed the quality of selected studies, supervised the data extraction, collaborated in drafting the initial manuscript and critically revised the manuscript. JW designed the review, supervised the literature search and data collection, and critically revised the manuscript.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Funding
This research was supported by the Ammodo Foundation and the Foundation Pediatric Intensive Care (SKIC) in the Netherlands. The sponsor had no role in the design of the review, literature search and analysis, the writing of the report or the decision to submit the manuscript for publication.
Supplementary Material
The Supplementary Material for this article can be found online at https://www.frontiersin.org/article/10.3389/fped.2016.00021
References
1. Khemani RG, Smith LS, Zimmerman JJ, Erickson S, Pediatric Acute Lung Injury Consensus Conference Group. Pediatric acute respiratory distress syndrome: definition, incidence, and epidemiology: proceedings from the pediatric acute lung injury consensus conference. Pediatr Crit Care Med (2015) 16(5 Suppl 1):S23–40. doi:10.1097/PCC.0000000000000432
2. Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, Fan E, et al. Acute respiratory distress syndrome: the Berlin definition. JAMA (2012) 307(23):2526–33. doi:10.1001/jama.2012.5669
3. Sapru A, Flori H, Quasney MW, Dahmer MK, Pediatric Acute Lung Injury Consensus Conference Group. Pathobiology of acute respiratory distress syndrome. Pediatr Crit Care Med (2015) 16(5 Suppl 1):S6–22. doi:10.1097/PCC.0000000000000431
4. Schouten LR, Schultz MJ, van Kaam AH, Juffermans NP, Bos AP, Wosten-van Asperen RM. Association between maturation and aging and pulmonary responses in animal models of lung injury: a systematic review. Anesthesiology (2015) 123(2):389–408. doi:10.1097/ALN.0000000000000687
5. Bem RA, Bos AP, Matute-Bello G, van Tuyl M, van Woensel JB. Lung epithelial cell apoptosis during acute lung injury in infancy. Pediatr Crit Care Med (2007) 8(2):132–7. doi:10.1097/01.PCC.0000269376.51877.12
6. Schoenfeld DA, Hui Z, Finkelstein DM. Bayesian design using adult data to augment pediatric trials. Clin Trials (2009) 6(4):297–304. doi:10.1177/1740774509339238
7. Roch A, Guervilly C, Papazian L. Fluid management in acute lung injury and ards. Ann Intensive Care (2011) 1(1):16. doi:10.1186/2110-5820-1-16
8. Wiedemann HP, Wheeler AP, Bernard GR, Thompson BT, Hayden D, deBoisblanc B, et al. Comparison of two fluid-management strategies in acute lung injury. N Engl J Med (2006) 354(24):2564–75. doi:10.1056/NEJMoa062200
9. Peake SL, Delaney A, Bailey M, Bellomo R, Cameron PA, Cooper DJ, et al. Goal-directed resuscitation for patients with early septic shock. N Engl J Med (2014) 371(16):1496–506. doi:10.1056/NEJMoa1404380
10. Yealy DM, Kellum JA, Huang DT, Barnato AE, Weissfeld LA, Pike F, et al. A randomized trial of protocol-based care for early septic shock. N Engl J Med (2014) 370(18):1683–93. doi:10.1056/NEJMoa1401602
11. Mouncey PR, Osborn TM, Power GS, Harrison DA, Sadique MZ, Grieve RD, et al. Trial of early, goal-directed resuscitation for septic shock. N Engl J Med (2015) 372(14):1301–11. doi:10.1056/NEJMoa1500896
12. Seguin J, Albright B, Vertullo L, Lai P, Dancea A, Bernier PL, et al. Extent, risk factors, and outcome of fluid overload after pediatric heart surgery*. Crit Care Med (2014) 42(12):2591–9. doi:10.1097/CCM.0000000000000517
13. Sinitsky L, Walls D, Nadel S, Inwald DP. Fluid overload at 48 hours is associated with respiratory morbidity but not mortality in a general PICU: retrospective cohort study*. Pediatr Crit Care Med (2015) 16(3):205–9. doi:10.1097/PCC.0000000000000318
14. Sutherland SM, Zappitelli M, Alexander SR, Chua AN, Brophy PD, Bunchman TE, et al. Fluid overload and mortality in children receiving continuous renal replacement therapy: the prospective pediatric continuous renal replacement therapy registry. Am J Kidney Dis (2010) 55(2):316–25. doi:10.1053/j.ajkd.2009.10.048
15. Arikan AA, Zappitelli M, Goldstein SL, Naipaul A, Jefferson LS, Loftis LL. Fluid overload is associated with impaired oxygenation and morbidity in critically ill children. Pediatr Crit Care Med (2012) 13(3):253–8. doi:10.1097/PCC.0b013e31822882a3
16. Hazle MA, Gajarski RJ, Yu S, Donohue J, Blatt NB. Fluid overload in infants following congenital heart surgery. Pediatr Crit Care Med (2013) 14(1):44–9. doi:10.1097/PCC.0b013e3182712799
17. Soler YA, Nieves-Plaza M, Prieto M, Garcia-De Jesus R, Suarez-Rivera M. Pediatric risk, injury, failure, loss, end-stage renal disease score identifies acute kidney injury and predicts mortality in critically ill children: a prospective study. Pediatr Crit Care Med (2013) 14(4):e189–95. doi:10.1097/PCC.0b013e3182745675
18. Grissom CK, Hirshberg EL, Dickerson JB, Brown SM, Lanspa MJ, Liu KD, et al. Fluid management with a simplified conservative protocol for the acute respiratory distress syndrome*. Crit Care Med (2015) 43(2):288–95. doi:10.1097/CCM.0000000000000715
19. Martin GS, Mangialardi RJ, Wheeler AP, Dupont WD, Morris JA, Bernard GR. Albumin and furosemide therapy in hypoproteinemic patients with acute lung injury. Crit Care Med (2002) 30(10):2175–82. doi:10.1097/00003246-200210000-00001
20. Martin GS, Moss M, Wheeler AP, Mealer M, Morris JA, Bernard GR. A randomized, controlled trial of furosemide with or without albumin in hypoproteinemic patients with acute lung injury. Crit Care Med (2005) 33(8):1681–7. doi:10.1097/01.CCM.0000171539.47006.02
21. Rosenberg AL, Dechert RE, Park PK, Bartlett RH; NIH NHLBI ARDS Network. Review of a large clinical series: association of cumulative fluid balance on outcome in acute lung injury: a retrospective review of the ARDSnet tidal volume study cohort. J Intensive Care Med (2009) 24(1):35–46. doi:10.1177/0885066608329850
22. Sakr Y, Vincent JL, Reinhart K, Groeneveld J, Michalopoulos A, Sprung CL, et al. High tidal volume and positive fluid balance are associated with worse outcome in acute lung injury. Chest (2005) 128(5):3098–108. doi:10.1378/chest.128.5.3098
23. Simmons RS, Berdine GG, Seidenfeld JJ, Prihoda TJ, Harris GD, Smith JD, et al. Fluid balance and the adult respiratory distress syndrome. Am Rev Respir Dis (1987) 135(4):924–9. doi:10.1164/arrd.1987.135.4.924
24. Aloia JF, Vaswani A, Flaster E, Ma R. Relationship of body water compartments to age, race, and fat-free mass. J Lab Clin Med (1998) 132(6):483–90. doi:10.1016/S0022-2143(98)90126-3
25. Tai R, Ohashi Y, Mizuiri S, Aikawa A, Sakai K. Association between ratio of measured extracellular volume to expected body fluid volume and renal outcomes in patients with chronic kidney disease: a retrospective single-center cohort study. BMC Nephrol (2014) 15:189. doi:10.1186/1471-2369-15-189
26. Sergi G, Lupoli L, Volpato S, Bertani R, Coin A, Perissinotto E, et al. Body fluid distribution in elderly subjects with congestive heart failure. Ann Clin Lab Sci (2004) 34(4):416–22.
27. Morgan AL, Sinning WE, Weldy DL. Age effects on body fluid distribution during exercise in the heat. Aviat Space Environ Med (2002) 73(8):750–7.
28. Edge JA. Cerebral oedema during treatment of diabetic ketoacidosis: are we any nearer finding a cause? Diabetes Metab Res Rev (2000) 16(5):316–24. doi:10.1002/1520-7560(2000)9999:9999<::AID-DMRR143>3.0.CO;2-R
29. Rosenbloom AL. Intracerebral crises during treatment of diabetic ketoacidosis. Diabetes Care (1990) 13(1):22–33. doi:10.2337/diacare.13.1.22
30. Nusmeier A, Cecchetti C, Blohm M, Lehman R, van der Hoeven J, Lemson J. Near-normal values of extravascular lung water in children. Pediatr Crit Care Med (2015) 16(2):e28–33. doi:10.1097/PCC.0000000000000312
31. Tian Y, Riazi S, Khan O, Klein JD, Sugimura Y, Verbalis JG, et al. Renal ENaC subunit, Na-K-2Cl and Na-Cl cotransporter abundances in aged, water-restricted F344 x Brown Norway rats. Kidney Int (2006) 69(2):304–12. doi:10.1038/sj.ki.5000076
32. Tiwari S, Li L, Riazi S, Halagappa VK, Ecelbarger CM. Sex and age result in differential regulation of the renal thiazide-sensitive NaCl cotransporter and the epithelial sodium channel in angiotensin II-infused mice. Am J Nephrol (2009) 30(6):554–62. doi:10.1159/000252776
33. Voilley N, Lingueglia E, Champigny G, Mattei MG, Waldmann R, Lazdunski M, et al. The lung amiloride-sensitive Na+ channel: biophysical properties, pharmacology, ontogenesis, and molecular cloning. Proc Natl Acad Sci U S A (1994) 91(1):247–51. doi:10.1073/pnas.91.1.247
34. Smith LS, Zimmerman JJ, Martin TR. Mechanisms of acute respiratory distress syndrome in children and adults: a review and suggestions for future research. Pediatr Crit Care Med (2013) 14(6):631–43. doi:10.1097/PCC.0b013e318291753f
35. Staub NC. Pulmonary edema: physiologic approaches to management. Chest (1978) 74(5):559–64. doi:10.1378/chest.74.5.559
36. Calfee CS, Gallagher D, Abbott J, Thompson BT, Matthay MA; NHLBI ARDS Network. Plasma angiopoietin-2 in clinical acute lung injury: prognostic and pathogenetic significance. Crit Care Med (2012) 40(6):1731–7. doi:10.1097/CCM.0b013e3182451c87
37. Kuebler WM, Ying X, Singh B, Issekutz AC, Bhattacharya J. Pressure is proinflammatory in lung venular capillaries. J Clin Invest (1999) 104(4):495–502. doi:10.1172/JCI6872
38. Woodcock TE, Woodcock TM. Revised starling equation and the glycocalyx model of transvascular fluid exchange: an improved paradigm for prescribing intravenous fluid therapy. Br J Anaesth (2012) 108(3):384–94. doi:10.1093/bja/aer515
39. Schmidt EP, Yang Y, Janssen WJ, Gandjeva A, Perez MJ, Barthel L, et al. The pulmonary endothelial glycocalyx regulates neutrophil adhesion and lung injury during experimental sepsis. Nat Med (2012) 18(8):1217–23. doi:10.1038/nm.2843
40. Yang Y, Schmidt EP. The endothelial glycocalyx: an important regulator of the pulmonary vascular barrier. Tissue Barriers (2013) 1(1):23494. doi:10.4161/tisb.23494
41. Chappell D, Bruegger D, Potzel J, Jacob M, Brettner F, Vogeser M, et al. Hypervolemia increases release of atrial natriuretic peptide and shedding of the endothelial glycocalyx. Crit Care (2014) 18(5):538. doi:10.1186/s13054-014-0538-5
42. Guidet B, Ait-Oufella H. Fluid resuscitation should respect the endothelial glycocalyx layer. Crit Care (2014) 18(6):707. doi:10.1186/s13054-014-0707-6
43. Matthay MA, Ware LB, Zimmerman GA. The acute respiratory distress syndrome. J Clin Invest (2012) 122(8):2731–40. doi:10.1172/JCI60331
44. Ware LB, Matthay MA. The acute respiratory distress syndrome. N Engl J Med (2000) 342(18):1334–49. doi:10.1056/NEJM200005043421806
45. Guyton AC. Interstitial fluid presure. II. Pressure-volume curves of interstitial space. Circ Res (1965) 16:452–60. doi:10.1161/01.RES.16.5.452
46. Prewitt RM, McCarthy J, Wood LD. Treatment of acute low pressure pulmonary edema in dogs: relative effects of hydrostatic and oncotic pressure, nitroprusside, and positive end-expiratory pressure. J Clin Invest (1981) 67(2):409–18. doi:10.1172/JCI110049
47. Laine GA, Allen SJ, Katz J, Gabel JC, Drake RE. Effect of systemic venous pressure elevation on lymph flow and lung edema formation. J Appl Physiol (1985) (1986) 61(5):1634–8.
48. Lubrano R, Cecchetti C, Elli M, Tomasello C, Guido G, Di Nardo M, et al. Prognostic value of extravascular lung water index in critically ill children with acute respiratory failure. Intensive Care Med (2011) 37(1):124–31. doi:10.1007/s00134-010-2047-6
49. Besen BA, Gobatto AL, Melro LM, Maciel AT, Park M. Fluid and electrolyte overload in critically ill patients: an overview. World J Crit Care Med (2015) 4(2):116–29. doi:10.5492/wjccm.v4.i2.116
50. Damman K, van Deursen VM, Navis G, Voors AA, van Veldhuisen DJ, Hillege HL. Increased central venous pressure is associated with impaired renal function and mortality in a broad spectrum of patients with cardiovascular disease. J Am Coll Cardiol (2009) 53(7):582–8. doi:10.1016/j.jacc.2008.08.080
51. Stone HH, Fulenwider JT. Renal decapsulation in the prevention of post-ischemic oliguria. Ann Surg (1977) 186(3):343–55. doi:10.1097/00000658-197709000-00012
52. Neyra JA, Li X, Yessayan L, Adams-Huet B, Yee J, Toto RD, et al. Dipstick albuminuria and acute kidney injury recovery in critically ill septic patients. Nephrology (2015). doi:10.1111/nep.12637
53. Palmieri T, Lavrentieva A, Greenhalgh DG. Acute kidney injury in critically ill burn patients. Risk factors, progression and impact on mortality. Burns (2010) 36(2):205–11. doi:10.1016/j.burns.2009.08.012
54. Bagshaw SM, Cruz DN. Fluid overload as a biomarker of heart failure and acute kidney injury. Contrib Nephrol (2010) 164:54–68. doi:10.1159/000313721
55. Macedo E, Bouchard J, Soroko SH, Chertow GM, Himmelfarb J, Ikizler TA, et al. Fluid accumulation, recognition and staging of acute kidney injury in critically-ill patients. Crit Care (2010) 14(3):R82. doi:10.1186/cc9004
56. Hassinger AB, Wald EL, Goodman DM. Early postoperative fluid overload precedes acute kidney injury and is associated with higher morbidity in pediatric cardiac surgery patients. Pediatr Crit Care Med (2014) 15(2):131–8. doi:10.1097/PCC.0000000000000043
57. Brandstrup B, Tonnesen H, Beier-Holgersen R, Hjortso E, Ording H, Lindorff-Larsen K, et al. Effects of intravenous fluid restriction on postoperative complications: comparison of two perioperative fluid regimens: a randomized assessor-blinded multicenter trial. Ann Surg (2003) 238(5):641–8. doi:10.1097/01.sla.0000094387.50865.23
58. Macafee DA, Allison SP, Lobo DN. Some interactions between gastrointestinal function and fluid and electrolyte homeostasis. Curr Opin Clin Nutr Metab Care (2005) 8(2):197–203. doi:10.1097/00075197-200503000-00015
59. Flori HR, Church G, Liu KD, Gildengorin G, Matthay MA. Positive fluid balance is associated with higher mortality and prolonged mechanical ventilation in pediatric patients with acute lung injury. Crit Care Res Pract (2011) 2011:854142. doi:10.1155/2011/854142
60. Valentine SL, Sapru A, Higgerson RA, Spinella PC, Flori HR, Graham DA, et al. Fluid balance in critically ill children with acute lung injury. Crit Care Med (2012) 40(10):2883–9. doi:10.1097/CCM.0b013e31825bc54d
61. Willson DF, Thomas NJ, Tamburro R, Truemper E, Truwit J, Conaway M, et al. The relationship of fluid administration to outcome in the pediatric calfactant in acute respiratory distress syndrome trial. Pediatr Crit Care Med (2013) 14(7):666–72. doi:10.1097/PCC.0b013e3182917cb5
62. Hu X, Qian S, Xu F, Huang B, Zhou D, Wang Y, et al. Incidence, management and mortality of acute hypoxemic respiratory failure and acute respiratory distress syndrome from a prospective study of Chinese paediatric intensive care network. Acta Paediatr (2010) 99(5):715–21. doi:10.1111/j.1651-2227.2010.01685.x
63. Randolph AG, Forbes PW, Gedeit RG, Arnold JH, Wetzel RC, Luckett PM, et al. Cumulative fluid intake minus output is not associated with ventilator weaning duration or extubation outcomes in children. Pediatr Crit Care Med (2005) 6(6):642–7. doi:10.1097/00130478-200511000-00027
64. Bhaskar P, Dhar AV, Thompson M, Quigley R, Modem V. Early fluid accumulation in children with shock and ICU mortality: a matched case-control study. Intensive Care Med (2015) 41(8):1445–53. doi:10.1007/s00134-015-3851-9
65. Avila-Diaz M, Ventura MD, Valle D, Vicente-Martinez M, Garcia-Gonzalez Z, Cisneros A, et al. Inflammation and extracellular volume expansion are related to sodium and water removal in patients on peritoneal dialysis. Perit Dial Int (2006) 26(5):574–80.
66. Marik PE. Fluid responsiveness and the six guiding principles of fluid resuscitation. Crit Care Med (2015). doi:10.1097/CCM.0000000000001483
67. Miller JL, Thomas AN, Johnson PN. Use of continuous-infusion loop diuretics in critically ill children. Pharmacotherapy (2014) 34(8):858–67. doi:10.1002/phar.1443
68. Reising CA, Chendrasekhar A, Wall PL, Paradise NF, Timberlake GA, Moorman DW. Continuous dose furosemide as a therapeutic approach to acute respiratory distress syndrome (ARDS). J Surg Res (1999) 82(1):56–60. doi:10.1006/jsre.1998.5513
69. Martin SJ, Danziger LH. Continuous infusion of loop diuretics in the critically ill: a review of the literature. Crit Care Med (1994) 22(8):1323–9. doi:10.1097/00003246-199408000-00017
70. Valentine SL, Nadkarni VM, Curley MA; Pediatric Acute Lung Injury Consensus Conference G. Nonpulmonary treatments for pediatric acute respiratory distress syndrome: proceedings from the pediatric acute lung injury consensus conference. Pediatr Crit Care Med (2015) 16(5 Suppl 1):S73–85. doi:10.1097/PCC.0000000000000435
71. Foland JA, Fortenberry JD, Warshaw BL, Pettignano R, Merritt RK, Heard ML, et al. Fluid overload before continuous hemofiltration and survival in critically ill children: a retrospective analysis. Crit Care Med (2004) 32(8):1771–6. doi:10.1097/01.CCM.0000132897.52737.49
72. Goldstein SL, Somers MJ, Baum MA, Symons JM, Brophy PD, Blowey D, et al. Pediatric patients with multi-organ dysfunction syndrome receiving continuous renal replacement therapy. Kidney Int (2005) 67(2):653–8. doi:10.1111/j.1523-1755.2005.67121.x
73. Hayes LW, Oster RA, Tofil NM, Tolwani AJ. Outcomes of critically ill children requiring continuous renal replacement therapy. J Crit Care (2009) 24(3):394–400. doi:10.1016/j.jcrc.2008.12.017
74. Selewski DT, Cornell TT, Lombel RM, Blatt NB, Han YY, Mottes T, et al. Weight-based determination of fluid overload status and mortality in pediatric intensive care unit patients requiring continuous renal replacement therapy. Intensive Care Med (2011) 37(7):1166–73. doi:10.1007/s00134-011-2231-3
75. Brierley J, Carcillo JA, Choong K, Cornell T, Decaen A, Deymann A, et al. Clinical practice parameters for hemodynamic support of pediatric and neonatal septic shock: 2007 update from the American College of Critical Care Medicine. Crit Care Med (2009) 37(2):666–88. doi:10.1097/CCM.0b013e31819323c6
76. Rogers EJ, Gilbertson HR, Heine RG, Henning R. Barriers to adequate nutrition in critically ill children. Nutrition (2003) 19(10):865–8. doi:10.1016/S0899-9007(03)00170-9
Keywords: PARDS, fluid balance, management, critical care, children, lung edema
Citation: Ingelse SA, Wösten-van Asperen RM, Lemson J, Daams JG, Bem RA and van Woensel JB (2016) Pediatric Acute Respiratory Distress Syndrome: Fluid Management in the PICU. Front. Pediatr. 4:21. doi: 10.3389/fped.2016.00021
Received: 03 December 2015; Accepted: 07 March 2016;
Published: 21 March 2016
Edited by:
John McGuire, University of Washington School of Medicine, USAReviewed by:
Rajit Basu, Cincinnati Children’s Hospital Medical Center, USALincoln S. Smith, University of Washington, USA
Copyright: © 2016 Ingelse, Wösten-van Asperen, Lemson, Daams, Bem and van Woensel. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sarah A. Ingelse, s.a.ingelse@amc.uva.nl
 Sarah A. Ingelse
Sarah A. Ingelse Roelie M. Wösten-van Asperen1
Roelie M. Wösten-van Asperen1
 Reinout A. Bem
Reinout A. Bem