Unbalanced Immune System: Immunodeficiencies and Autoimmunity
- Department of Translational Medical Sciences, Federico II University of Naples, Naples, Italy
Increased risk of developing autoimmune manifestations has been identified in different primary immunodeficiencies (PIDs). In such conditions, autoimmunity and immune deficiency represent intertwined phenomena that reflect inadequate immune function. Autoimmunity in PIDs may be caused by different mechanisms, including defects of tolerance to self-antigens and persistent stimulation as a result of the inability to eradicate antigens. This general immune dysregulation leads to compensatory and exaggerated chronic inflammatory responses that lead to tissue damage and autoimmunity. Each PID may be characterized by distinct, peculiar autoimmune manifestations. Moreover, different pathogenetic mechanisms may underlie autoimmunity in PID. In this review, the main autoimmune manifestations observed in different PID, including humoral immunodeficiencies, combined immunodeficiencies, and syndromes with immunodeficiencies, are summarized. When possible, the pathogenetic mechanism underlying autoimmunity in a specific PID has been explained.
Introduction
Immunodeficiencies and autoimmunity may be considered two opposite conditions, deriving from different alterations of the immune system. However, the evidence that primary immunodeficiencies (PIDs) are often associated with different autoimmune manifestations suggests that they could share common pathogenetic mechanisms, which result in a broad immune dysregulation.
Immune system becomes self-tolerant through two main mechanisms called central and peripheral tolerance. As for T cells, central tolerance takes place within the thymus and is mediated by medullary thymic epithelial cells (mTEC), which express tissue-specific antigens under the control of the the transcription factor autoimmune regulator (AIRE) (1–3). Developing T-cells recognizing self-antigens receive a signal to die via programed cell death and, thereby, are deleted, through negative selection, from the T-cell repertoire (4, 5). As for B cells, negative selection of autoreactive cells takes place within the bone-marrow. Different mechanisms, including immunological ignorance, anergy, and suppression through regulatory T cells (Treg) are implicated in the control of self-reactive cells, which escape central tolerance and reach the periphery. For example, the ligation of T-cell receptor (TCR), in the absence of costimulatory molecules, makes the cells inable to express effector functions like cytokine secretion, leading to anergy (6). The control of the expression of the costimulatory molecules CD80 and CD86 is a major mechanism of peripheral tolerance (6).
In some cases, the inability to eradicate foreign antigens may lead to an exaggerated chronic inflammatory responses and autoimmunity (7–10), through several mechanisms, including molecular mimicry, by-stander activation, epitope spreading, and cryptic antigens.
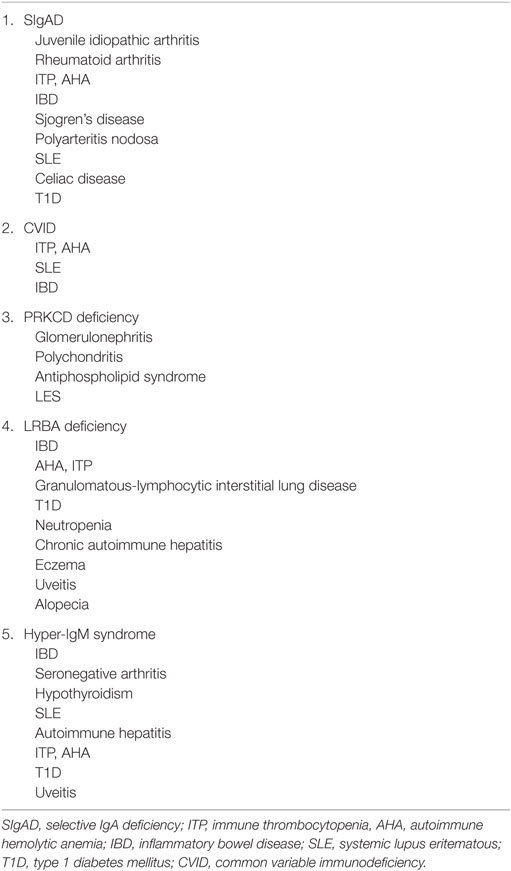
Each PID is characterized by distinct, peculiar autoimmune manifestations (Tables 1 and 2), but the mechanisms may differ.
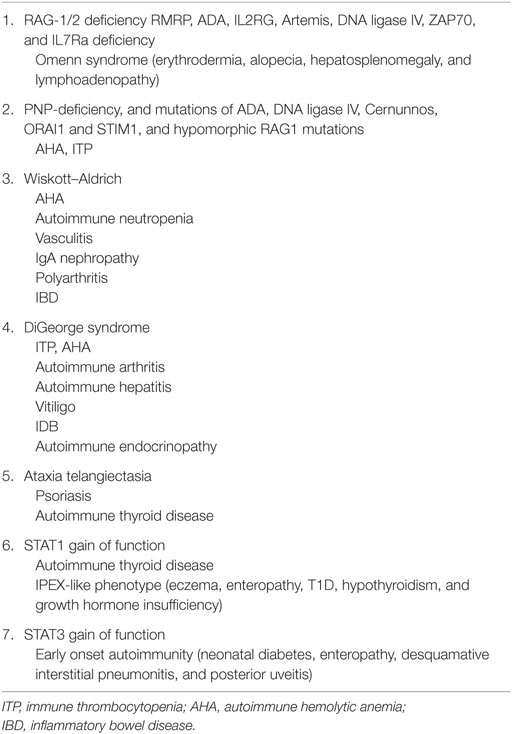
Table 2. Autoimmune manifestations in combined immunodeficiencies and in syndromes with immunodeficiency.
In this review, we will describe the main autoimmune manifestations observed in different PIDs, including humoral immunodeficiencies, combined immunodeficiencies, and syndromes with immunodeficiencies, and, when possible, we will try to explain the pathogenetic mechanism underlying autoimmunity in a specific PID.
Autoimmunity in Humoral Immunodeficiencies
Selective IgA Deficiency
Selective IgA deficiency (SIgAD) is the most common PID in humans (11). According to European Society for Immunodeficiencies (ESID) criteria, SIgAD is defined by the presence of serum IgA levels <0.07 g/l in the absence of IgG and IgM deficiencies, after the age of 4 years (12). Patients with SIgAD have an increased risk to develop allergies and autoimmune manifestations, including juvenile idiopathic arthritis, rheumatoid arthritis, thrombocytopenic purpura, hemolytic anemia, inflammatory bowel disease (IBD), Sjogren’s disease, polyarteritis nodosa, systemic lupus erythematosus (SLE), celiac disease, and insulin-dependent diabetes mellitus (T1D) (Table 1) (13). Little is known about the pathogenesis of SIgAD and the predisposition to autoimmunity in these patients. Specific human leukocyte antigen (HLA) haplotypes, including 8.1, DR7, DQ2, DR1, and DQ5 have been identified in patients with SIgAD at higher risk autoimmune diseases (14), such as SLE, autoimmune thyroiditis, and celiac disease. In a recent study, the identification of single nucleotide polymorphisms in the IF1H1 gene encoding for an interferon inducible RNA helicase 1 protein and of a mutation in the CLEC16A gene in SIgAD patients has been associated with the development of autoimmune manifestations (14). Jacob et al. hypothesized that IgA exerts a protective role against autoimmunity. In particular, the interaction between the Fc fragment of IgA receptor and the immunoreceptor tyrosine-based activation motif deactivates the pathways of immune response carrying this motif through a partial phosphorylation (15). Moreover, the evidence of antibodies to bovine milk proteins in over 60% of IgA deficient patients may help explaining the association between SIgAD and inflammatory diseases of gastrointestinal tract (16, 17).
Common Variable Immunodeficiency
Common Variable immunodeficiency (CVID) is a heterogeneous group of disorders characterized by a primary antibody deficiency, usually manifesting between the second and fourth decades of life with a mean age at onset of 26.3 years (18). It is the second most common immunodeficiency with an estimated prevalence ranging from 0.073 to 0.977 living patients per 100,000 inhabitants (19). According to the ESID diagnostic criteria, CVID should be taken into account in presence of a marked decrease of IgG and IgA with or without low IgM levels (measured at least twice; <2SD of the normal levels for their age) (http://esid.org/Working-Parties/Registry/Diagnosis-criteria). Moreover, all of the following criteria should be fullfilled: poor antibody response to vaccines (and/or absent isohemagglutinins) or low switched memory B cells (<70% of age-related normal value); secondary causes of hypogammaglobulinaemia have been excluded diagnosis is established after the 4th year of life; no evidence of profound T-cell deficiency (http://esid.org/Working-Parties/Registry/Diagnosis-criteria). More than 25% of CVID patients develop autoimmune complications (18, 20). Other medical conditions may include gastrointestinal infectious or inflammatory disease, lymphadenopathy, splenomegaly, and hematological malignancies (21). Cytopenia is the most common manifestation. Immune thrombocytopenia (ITP) has been found in up to 14% of patients and autoimmune hemolytic anemia (AHA) in up to 7% (22). In most cases (about 60%), the cytopenia precedes the identification of hypogammaglobulinemia (23). SLE has been reported in some rare CVID patient (24), predominantly females (89%). In about 50% of patients, CVID developed within 5 years of the diagnosis of SLE (24). Some patients experience an improvement in SLE symptoms when hypogammaglobulinemia appears (24). Hypogammaglobulinemia can develop because of the use of immunosuppressive treatment (i.e., corticosteroids or immunosuppressants). Unlike CVID, the cessation of therapy should solve hypogammaglobulinaemia. Nevertheless, in some occasion, the duration of post-cessation hypogammaglobulinaemia can be very prolonged, making difficult to understand its origin (25). IBD has been reported in 6–10% of CVID patients (Table 1) (22). Many different alterations could help explain the predisposition to autoimmune manifestations. In a subgroup of CVID patients, IL-7 levels were found to be increased (26, 27). IL-7 plays a key role in the expansion of autoreactive T-cell clones in the lymphopenic host (26, 27). Moreover, reduced levels of switched memory B cells and increased levels of activated CD21-low B cells have been associated with autoimmune manifestations in CVID. Increased levels of CD21-low B cells have been identified in SLE, rheumatoid arthritis, and cryoglobulinemia, suggesting a role for these cells in the pathogenesis of autoimmunity (28–30). Most CVID patients present with elevated BAFF levels (27). Of note, increased BAFF levels sustain the expansion of CD21-low B cells in CVID (31). Moreover, studies show that overexpression of BAFF in mice leads to B-cell hyperplasia, splenomegaly, and autoimmunity (32, 33). Different genetic mutations, including TACI, ICOS, BAFF-R, CD20, and CD21 have been associated with increased risk of developing CVID (34–40). Among these genetic alterations, autoimmunity is most common in TACI alterations [18/50 (36%) vs. 112/490 (23%) in wt TACI CVID], in particular, heterozygous C104R mutations (11/20 patients, 55%) (41).
PRKCD Deficiency
A CVID-like disorder associated with multiple features of immune dysregulation, including glomerulonephritis, lymphadenopathy, relapsing polychondritis, and antiphospholipid syndrome has been recently described in a 12-year-old patient born to consanguineous parents of Turkish origin (42). Genetic studies revealed a mutation of PRKCD gene, leading to a complete absence of the protein. PRKCD deficiency has also been reported in three siblings with LES (Table 1) (43). PRKCD plays a key role in the regulation of cell survival, proliferation, and apoptosis (44). PRKCD deficiency in mice seems to be related to a defective deletion of autoreactive B cells during B-cell development, due to impaired proapoptotic extracellular signal-regulated kinase signaling (45, 46).
LRBA Deficiency
LPS-responsive beige-like anchor protein (LRBA) deficiency is a novel PID caused by either homozygous or compound heterozygous mutations in LRBA that abolish LRBA protein expression. This PID is characterized by early onset hypogammaglobulinemia, autoimmune manifestations, susceptibility to IBD, and recurrent infections (47). However, it has been also described in patients with IBD with or without antibody deficiency (48, 49), in patients with autoimmune manifestations without hypogammaglobulinemia (50), or in patients with immune dysregulation, polyendocrinopathy, enteropathy, and X-linked syndrome (IPEX)-like disorder (51). The main clinical manifestations of LRBA deficiency are immune dysregulation (95%), followed by organomegaly (86%) and recurrent infections (71%). The most common autoimmune manifestations are enteropathy (59%), AHA (50%), and ITP (50%). A lower number of patients presented granulomatous-lymphocytic interstitial lung disease (36%), T1D or neutropenia (22%), chronic autoimmune hepatitis (13%), eczema and uveitis (9%), and alopecia (4.5%) (Table 1). LRBA is a highly conserved multidomain protein implicated in regulating endosomal trafficking, cell proliferation, and survival. LRBA deficiency is associated with increased apoptosis and altered phenotype of Treg cells, which express lower levels of key effector proteins involved in Treg cell suppression, such as CD25 and CTLA-4. This results in decreased frequency, aberrant phenotype, and decreased suppressive function of such cells. These alterations might play a critical role in the ubiquitous autoimmune manifestations of the disease.
CTLA-4 Haploinsufficiency
CTLA-4 haploinsufficiency has been recently associated with lymphoproliferation, lymphocytic infiltration, autoimmunity, peripheral B-cell lymphopenia, hypogammaglobulinemia, and increased CD21lo B cells (52). In mouse models, homozygous CTLA-4 deficiency leads to a lethal autoimmune phenotype characterized by multiorgan lymphocytic infiltration and destruction (53, 54) resambling FOXP3 deficiency (55–57). CTLA-4 plays a key role in immune tolerance. Recent studies show that CTLA-4 is able to suppress the expression of CD80 and CD86 from antigen presenting cells (APCs) via transendocytosis (58). The depletion of the costimulatory ligands reduces T cell activation (59).
Activated Phosphoinositide 3-Kinase δ Syndrome
Activated phosphoinositide 3-kinase δ syndrome (APDS) 1 and 2 are PID resulting from autosomal dominant mutations in PI3KCD and PIK3R1, respectively (60, 61). Autoimmune manifestations are reported in 34% of APDS1 patients. The clinical manifestations included cytopenias (AHA or tri-lineage cytopenia), glomerulonephritis, exocrine pancreatic insufficiency, autoimmune thyroid disease, seronegative arthritis, recurrent pericarditis, sclerosing cholangitis, and gastrointestinal nodular mucosal lymphoid hyperplasia (61). Autoimmune manifestations have been reported in the 17% of the APDS2 patients. They included ITP, AHA, Evans syndrome, T1D, chronic arthritis, autoimmune hepatitis, and chronic eczema (60). PI3Kδ is implicated in the regulation of Treg cell function. Studies suggest that PI3K is an important target for the treatment of different autoimmune conditions.
Hyper-IgM Syndrome
Hyper-IgM syndrome (HIGM) is a group of disorders characterized by alterations of immunoglobulin receptor isotype switching, leading to normal or elevated IgM antibody and very low IgA, IgG, and IgE antibodies (62). Alterations in different genes implicated in CD40-CD40L pathway involved in B cell activation, class switch recombination or somatic hypermutation have been identified in HIGM. Seven different forms of HIGM have been till now described. Most of the cases (65–70%) are due to mutations of the gene encoding for CD40 ligand (CD40L) on the X chromosome, leading to HIGM1 (63). The other forms are due to mutations of AID (HIGM2), CD40 (HIGM3), UNG (HIGM5), NEMO (HIGM6), and IkBα (HIGM7). No genetic defect has been so far identified for HIGM4.
Autoimmunity has been described in all forms of HIGM. HIGM1 patients have an increased risk to develop IBD, seronegative arthritis, hypothyroidism, and SLE (64). In the 21% of patients affected with HIGM2 autoimmune hepatitis, ITP, T1D, IDB, and uveitis have been described (65). In addition, in patients with NEMO defects, AHA, IBD, and arthritis have been described (Table 1) (66). Studies on transgenic mouse models suggest that CD40–CD40L interactions is involved in the elimination of autoreactive B cells (67). In fact, an increase of circulating polyreactive B cells and a significant decrease of CD25+Foxp3+Treg cells have been reported in CD40L-deficient patients suggesting defects of the peripheral B-cell tolerance mechanism. An imbalanced production of cytokines, including as IL-1, IL-8, IL-6, IL-10, IL-12, and tumor necrosis factor (TNF)-α may be observed in CD40-deficient patients (68). This impairment is the consequence of the involvement of CD40–CD40L interaction in T-cell dependent macrophage-mediated immune response, implicated in the maturation of dendritic cells and regulation of the T-cell activation. The transcription factor NFkB plays a key role in the regulation of pro-inflammatory responses. Recent studies suggest that gut epithelial cells are directly implicated in the control of epithelial integrity and the regulation of the interaction between the mucosal immune system and gut microflora. In mice, NEMO deficiency causes a severe chronic intestinal inflammation, which has been associated with apoptosis of colonic epithelial cells, impaired expression of antimicrobial peptides, and translocation of bacteria into the mucosa. The chronic inflammatory response observed within the colon, is dominated by innate immune cells, as suggested by the upregulation of IL1b, IL6, TNF, and Ccl2 and by the infiltration of large numbers of dendritic cells and granulocytes in the colon. Eventually, also T lymphocytes are involved, as suggested by the presence of lymphoid follicles and a massive infiltration with CD4+ T cells in the gut mucosa.
Combined Immunodeficiecies
Severe combined immunodeficiency (SCID) is a group of different PIDs characterized by a severe deficiency of the cellular and humoral immune system. SCID phenotype may be due to a variety of different mutations. From a clinical point of view, SCID is characterized by recurrent severe infections, chronic diarrhea, and failure to thrive (69, 70). The clinical presentation may drive the diagnosis toward a specific molecular cause of SCID (69). Patients affected with SCID often develop autoimmune manifestations. This may appear surprising in that SCID patients, who are unable to mount any immune response to foreign pathogens, may paradoxically develop autoimmune phenomena. Alterations in both central and peripheral tolerance have been described in SCID patients (71).
Autoimmunity in Omenn Syndrome
Omenn syndrome (OS) is a SCID inherited in an autosomal recessive manner, caused by homozygous or compound heterozygous mutations in recombinase activating gene 1 (RAG1) or RAG2, implicated in V(D)J recombination, which represents a crucial step in T- and B-cell differentiation. OS has also been associated with hypomorphic mutations in other different genes, including RMRP, ADA, IL2RG, Artemis, DNA ligase IV, ZAP70, and IL-7Ra deficiency (72, 73). Signs of OS, including oligoclonal T-cell expansion, generalized rash, and lymphadenopathy have been reported in some patient affected with DiGeorge syndrome. This rare condition is known as atypical complete DiGeorge syndrome (74). Apart from recurrent infections, patients affected with OS also show features of autoimmunity, including erythrodermia, alopecia, hepatosplenomegaly, and lymphadenopathy (Table 2). The hallmark of the syndrome is the expansion and activation of a peripheral oligoclonal population of autoreactive T cells, due to defective central (75, 76) and peripheral tolerance mechanisms (77). Studies suggest that in OS, defective AIRE expression may lead to inadequate expression of tissue-specific self-antigens by mTEC, impairing central tolerance. In these patients, the T-cell compartment is composed by a high proportion of autoreactive T cells, which are able to expand in peripheral tissues leading to the clinical symptoms. Similarly, alterations in central tolerance may be implicated in the pathogenesis of immune manifestations also in PIDs characterized by ineffective thymopoiesis, such as the DiGeorge syndrome or in SCID characterized by partial defects of the T-cell maturation, such as IL-7alfa, common γ chain, or ARTEMIS defects. The persistent infectious/inflammatory state and the presence of immunologic “space,” which increases the ability of T cells to respond to an excess of cytokines or antigens, impairs peripheral tolerance in SCID patients. Treg population may be also affected in SCID patients.
Autoimmune Manifestations in SCID Due to IL7R Mutations
IL7Ra deficiency is responsible of the majority of T-B+NK+ cases (72) characterized by an increased susceptibility to severe and opportunistic infections. In a few cases, autoimmune manifestations have been reported (72, 73). Autoimmune manifestations presented with OS in one infant (73), and cytopenias in three other cases. Autoimmune cytopenias have been also described in some patients with PNP-deficiency, and mutations of ADA, DNA ligase IV, Cernunnos, and hypomorphic RAG1 mutations (Table 2) (69, 78–82).
Ca++ Channellopathies Due to Mutations in ORAI1 and STIM1
Null or loss-of-function mutations in ORAI1 or STIM1 are associated with a SCID-like disease characterized by recurrent and chronic infections, autoimmunity, ectodermal dysplasia, and muscular hypotonia in the presence of numerically intact T, B, and NK cells. Symptoms usually manifest in the first year of life. Lymphoproliferation, AHA, and ITP are very common in patients with STIM1 mutations (Table 2). Autoimmunity may derive from alterations of negative selection of autoreactive T cells and/or B cells during their development. In fact, Ca2+ signals are implicated in TCR and BCR signaling and thus potentially influence the selection thresholds in immature T and B cells. Moreover, a reduced frequency of Treg cells has been observed in STIM1-deficient patients (83, 84) and in one patient with ORAI1 p.R91W mutation.
Syndromes with Immunodeficiency
Wiskott–Aldrich
Wiskott–Aldrich syndrome is a very rare immunodeficiency, characterized by thrombocytopenia, eczema, and recurrent bacterial infections appearing in the first months of life. Other features includes humoral and cellular immunodeficiency, defects of the innate immunity (85–87), increased risk to develop autoimmune manifestation and malignancies, impaired apoptosis (88, 89), and defective cell motility (90). The gene responsible for WAS (WASP) is located on the X chromosome and encode for WASP protein, which is only expressed in the cytoplasm of hematopoietic cells. WASP protein plays a major role in the transduction of the signals from the cell surface to the actin cytoskeleton, which regulates actin polymerizationand the formation of actin filament (91, 92). WAS patients are at a higher risk of developing autoimmunity and most of WAS patients (about 40%) are affected by at least one autoimmune manifestation (93, 94). The most common autoimmune manifestations include AHA, autoimmune neutropenia, vasculitis, and IgA nephropathy with or without the association with Henoch–Schönlein purpura, polyarthritis and IBD (Table 2) (87, 93–95). Studies suggest that a defect in Treg cells could be implicated in the pathogenesis of autoimmune manifestations (96, 97). In fact, Treg cells, isolated from WAS patients, show a reduced ability to suppress effector T-cell proliferation and IFN-γ production (98, 99). On the contrary, Treg cell development is not impaired in these patients. In addition, Treg cells from WASp−/− mouse show a reduced granzyme B secretion, which results in the inability to suppress B-cell proliferation and apoptosis. Furthermore, studies on mouse models show that Treg cells from WASp−/−mouse are not able to prevent the development of autoimmunity in scurfy mice (Foxp3-deficient) (98–100). Also B cells may be implicated in the pathogenesis of autoimmune manifestations in WAS patients. Studies show that selective deletion of WASP in B cells leads to the production of autoantibodies and the development of autoimmunity (101, 102).
DiGeorge Syndrome
Autoimmune manifestations have been reported in about the 10% of patients with DiGeorge syndrome (103–105). Autoimmune disorders include mainly autoimmune cytopenias (ITP, AHA) (106–108), autoimmune arthritis (107), autoimmune hepatitis, vitiligo, IDB, and autoimmune endocrinopathy (Table 2) (109). Impaired T-cell development in an abnormal thymus may result in altered central tolerance and escape of self-reactive T. Thymic abnormality may also result in impaired generation of Treg (96, 110, 111).
Ataxia Telangiectasia
Patients with ataxia telangiectasia (A-T) have increased frequency of autoimmune disorders (112), including psoriasis and autoimmune thyroid disease (Table 2). Loss of suppressor T-cell function has been described as responsible for the development of autoimmune disease.
STAT1 Gain of Function
Increased incidence of autoimmunity has been reported in heterozygous STAT1 gain-of-function (GOF) mutations (113). The main clinical features of the syndrome include chronic mucocutaneous candidiasis (CMC) (114–118), disseminated coccidioidomycosis, and histoplasmosis (116, 119), recurrent sinopulmonary infections and pneumonias (with or without bronchiectasis), herpes virus infections, blood-borne infections, squamous cell cancer, and cerebral aneurysms (116, 120). The most common autoimmune manifestation is thyroiditis, but in some case patient may show an IPEX-like phenotype (121). Number and function of Treg cells are usually normal and the pathogenesis of IPEX-like disease remains unclear (121).
STAT3 Gain of Function
Recent studies show that activating STAT3 mutations may lead to autoimmunity, hypogammaglobulinemia, lymphoproliferation, and mycobacterial disease (122). The autoimmune manifestations are early onset and include neonatal diabetes and some rare disorders, such as desquamative interstitial pneumonitis and posterior uveitis (123). Patients with activating STAT3 mutations show a reduced number of Th17 cells, decreased IL-17 production, and deficiency of Treg, NK, and dendritic cells (123). Autoimmunity may develop as a consequence of the impaired Treg development.
Conclusion
Autoimmunity and immunodeficiencies represent two opposite conditions, which may coexist in the context of a general immune dysregulation. Even though different mechanisms have been identified to explain autoimmunity in PIDs, the pathogenesis of autoimmunity remains unexplained in most of the cases. Considering this strong association, underlying immunodifiency should be always excluded in particular in presence of early onset or multiple autoimmune manifestations (124).
Author Contributions
All authors listed, have made substantial, direct and intellectual contribution to the work, and approved it for publication.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Capalbo D, Giardino G, Martino LD, Palamaro L, Romano R, Gallo V, et al. Genetic basis of altered central tolerance and autoimmune diseases: a lesson from AIRE mutations. Int Rev Immunol (2012) 31:344–62. doi:10.3109/08830185.2012.697230
2. Gallo V, Giardino G, Capalbo D, Palamaro L, Romano R, Santamaria F, et al. Alterations of the autoimmune regulator transcription factor and failure of central tolerance: APECED as a model. Expert Rev Clin Immunol (2013) 9:43–51. doi:10.1586/eci.12.88
3. Capalbo D, De Martino L, Giardino G, Di Mase R, Di Donato I, Parenti G, et al. Autoimmune polyendocrinopathy candidiasis ectodermal dystrophy: insights into genotype-phenotype correlation. Int J Endocrinol (2012) 2012:9. doi:10.1155/2012/353250
4. DeFranco S, Bonissoni S, Cerutti F, Bona G, Bottarel F, Cadario F, et al. Defective function of Fas in patients with type 1 diabetes associated with other autoimmune diseases. Diabetes (2001) 50:483–8. doi:10.2337/diabetes.50.3.483
5. Pignata C, Alessio M, Ramenghi U, Bonissoni S, Difranco D, Brusco A, et al. Clustering of distinct autoimmune diseases associated with functional abnormalities of T cell survival in children. Clin Exp Immunol (2000) 121:53–8. doi:10.1046/j.1365-2249.2000.01275.x
6. Miller SD, Turley DM, Podojil JR. Antigen-specific tolerance strategies for the prevention and treatment of autoimmune disease. Nat Rev Immunol (2007) 7:665–77. doi:10.1038/nri2153
7. Aloj G, Giardino G, Valentino L, Maio F, Gallo V, Esposito T, et al. Severe combined immunodeficiences: new and old scenarios. Int Rev Immunol (2012) 31:43–65. doi:10.3109/08830185.2011.644607
8. Münz C, Lünemann JD, Getts MT, Miller SD. Antiviral immune responses: triggers of or triggered by autoimmunity? Nat Rev Immunol (2009) 4:246–58. doi:10.1038/nri2527
9. Fairweather D, Kaya Z, Shellam GR, Lawson CM, Rose NR. From infection to autoimmunity. J Autoimmun (2001) 3:175–86. doi:10.1006/jaut.2000.0492
10. Panoutsakopoulou V, Cantor H. On the relationship between viral infection and autoimmunity. J Autoimmun (2001) 3:341–5. doi:10.1006/jaut.2000.0480
12. Conley ME, Notarangelo LD, Etzioni A. Diagnostic criteria for primary immunodeficiencies. Representing PAGID (Pan-American Group for Immunodeficiency) and ESID (European Society for Immunodeficiencies). Clin Immunol (1999) 3:190–7. doi:10.1006/clim.1999.4799
13. Singh K, Chang C, Gershwin ME. IgA deficiency and autoimmunity. Autoimmun Rev (2014) 2:163–77. doi:10.1016/j.autrev.2013.10.005
14. Jorgensen GH, Ornolfsson AE, Johannesson A, Gudmundsson S, Janzi M, Wang N, et al. Association of immunoglobulin A deficiency and elevated thyrotropin-receptor autoantibodies in two Nordic countries. Hum Immunol (2011) 2:166–72. doi:10.1016/j.humimm.2010.10.014
15. Jacob CM, Pastorino AC, Fahl K, Carneiro-Sampaio M, Monteiro RC. Autoimmunity in IgA deficiency: revisiting the role of IgA as a silent housekeeper. J Clin Immunol (2008) 28:S56–61. doi:10.1007/s10875-007-9163-2
16. Cunningham-Rundles C, Brandeis WE, Pudifin DJ, Day NK, Good RA. Autoimmunity in selective IgA deficiency: relationship to anti-bovine protein antibodies, circulating immune complexes and clinical disease. Clin Exp Immunol (1981) 45:299–304.
17. Pignata C, Budillon G, Monaco G, Nani E, Cuomo R, Parrilli G, et al. Jejunal bacterial overgrowth and intestinal permeability in children with immunodeficiency syndromes. Gut (1990) 31:879–82. doi:10.1136/gut.31.8.879
18. Chapel H, Lucas M, Lee M, Bjorkander J, Webster D, Grimbacher B, et al. Common variable immunodeficiency disorders: division into distinct clinical phenotypes. Blood (2008) 112:277–86. doi:10.1182/blood-2007-11-124545
19. Gathmann B, Binder N, Ehl S, Kindle G, ESID Registry Working Party. The European internet-based patient and research database for primary immunodeficiencies: update 2011. Clin Exp Immunol (2012) 167:479–91. doi:10.1111/j.1365-2249.2011.04542.x
20. Cunningham-Rundles C. Common variable immunodeficiency. Curr Allergy Asthma Rep (2001) 1:421–9. doi:10.1007/s11882-001-0027-1
21. Agarwal S, Cunningham-Rundles C. Autoimmunity in common variable immunodeficiency. Curr Allergy Asthma Rep (2009) 9:347–52. doi:10.1007/s11882-009-0051-0
22. Cunningham-Rundles C, Bodian C. Common variable immunodeficiency: clinical and immunological features of 248 patients. Clin Immunol (1999) 92:34–48. doi:10.1006/clim.1999.4725
23. Wang J, Cunningham-Rundles C. Treatment and outcome of autoimmune hematologic disease in common variable immunodeficiency (CVID). J Autoimmun (2005) 25:57–62. doi:10.1016/j.jaut.2005.04.006
24. Fernández-Castro M, Mellor-Pita S, Citores MJ, Muñoz P, Tutor-Ureta P, Silva L, et al. Common variable immunodeficiency in systemic lupus erythematosus. Semin Arthritis Rheum (2007) 36:238–45. doi:10.1016/j.semarthrit.2006.09.005
25. Yong PF, Aslam L, Karim MY, Khamashta MA. Management of hypogammaglobulinaemia occurring in patients with systemic lupus erythematosus. Rheumatology (Oxford) (2008) 47:1400–5. doi:10.1093/rheumatology/ken255
26. Holm AM, Aukrust P, Damås JK, Muller F, Halvorsen B, Frøland SS. Abnormal interleukin-7 function in common variable immunodeficiency. Blood (2005) 105:2887–90. doi:10.1182/blood-2004-06-2423
27. Kreuzaler M, Rauch M, Salzer U, Birmelin J, Rizzi M, Grimbacher B, et al. Soluble BAFF levels inversely correlate with peripheral B cell numbers and the expression of BAFF receptors. J Immunol (2012) 188:497–503. doi:10.4049/jimmunol.1102321
28. Warnatz K, Wehr C, Dräger R, Schmidt S, Eibel H, Schlesier M, et al. Expansion of CD19hlCD21lo/mg B cells in common variable immunodeficiency (CVID) patients with autoimmune cytopenia. Immunobiology (2002) 206:502–13. doi:10.1078/0171-2985-00198
29. Berglund LJ, Wong SW, Fulcher DA. B-cell maturation defects in common variable immunodeficiency and association with clinical features. Pathology (2008) 40:288–94. doi:10.1080/00313020801911470
30. Moratto D, Gulino AV, Fontana S, Mori L, Pirovano S, Soresina A, et al. Combined decrease of defined B and T cell subsets in a group of common variable immunodeficiency patients. Clin Immunol (2006) 121:203–14. doi:10.1016/j.clim.2006.07.003
31. Wehr C, Eibel H, Masilamani M, Illges H, Schlesier M, Peter HH, et al. A new CD21low B cell population in the peripheral blood of patients with SLE. Clin Immunol (2004) 2004:161–71. doi:10.1016/j.clim.2004.05.010
32. Mackay F, Woodcock SA, Lawton P, Ambrose C, Baetscher M, Schneider P, et al. Mice transgenic for BAFF develop lymphocytic disorders along with autoimmune manifestations. J Exp Med (1999) 190:1697–710. doi:10.1084/jem.190.11.1697
33. Thien M, Phan TG, Gardam S, Amesbury M, Basten A, Mackay F, et al. Excess BAFF rescues self-reactive B cells from peripheral deletion and allows them to enter forbidden follicular and marginal zone niches. Immunity (2004) 20:785–98. doi:10.1016/j.immuni.2004.05.010
34. Castigli E, Wilson SA, Garibyan L, Rachid R, Bonilla F, Schneider L, et al. TACI is mutant in common variable immunodeficiency and IgA deficiency. Nat Genet (2005) 37:829–34. doi:10.1038/ng1601
35. Salzer U, Chapel HM, Webster AD, Pan-Hammarström Q, Schmitt-Graeff A, Schlesier M, et al. Mutations in TNFRSF13B encoding TACI are associated with common variable immunodeficiency in humans. Nat Genet (2005) 37:820–8. doi:10.1038/ng1600
36. Grimbacher B, Hutloff A, Schlesier M, Glocker E, Warnatz K, Dräger R, et al. Homozygous loss of ICOS is associated with adult-onset common variable immunodeficiency. Nat Immunol (2003) 4:261–8. doi:10.1038/ni902
37. Salzer U, Maul-Pavicic A, Cunningham-Rundles C, Urschel S, Belohradsky BH, Litzman J, et al. ICOS deficiency in patients with common variable immunodeficiency. Clin Immunol (2004) 113:234–40. doi:10.1016/j.clim.2004.07.002
38. van Zelm MC, Reisli I, van der Burg M, Castaño D, van Noesel CJ, van Tol MJ, et al. An antibody-deficiency syndrome due to mutations in the CD19 gene. N Engl J Med (2006) 354:1901–12. doi:10.1056/NEJMoa051568
39. Kanegane H, Agematsu K, Futatani T, Sira MM, Suga K, Sekiguchi T, et al. Novel mutations in a Japanese patient with CD19 deficiency. Genes Immun (2007) 8:663–70. doi:10.1038/sj.gene.6364431
40. Schäffer AA, Salzer U, Hammarström L, Grimbacher B. Deconstructing common variable immunodeficiency by genetic analysis. Curr Opin Genet Dev (2007) 17:201–12. doi:10.1016/j.gde.2007.04.002
41. Salzer U, Bacchelli C, Buckridge S, Pan-Hammarstrom Q, Jennings S, Lougaris V, et al. Relevance of biallelic versus monoallelic TNFRSF13B mutations in distinguishing disease-causing from risk-increasing TNFRSF13B variants in antibody deficiency syndromes. Blood (2009) 113:1967–76. doi:10.1182/blood-2008-02-141937
42. Salzer E, Santos-Valente E, Klaver S, Ban SA, Emminger W, Prengemann NK, et al. B-cell deficiency and severe autoimmunity caused by deficiency of protein kinase C delta. Blood (2013) 121:3112–6. doi:10.1182/blood-2012-10-460741
43. Belot A, Kasher PR, Trotter EW, Foray A-P, Debaud A-L, Rice GI, et al. Protein kinase Cδ deficiency causes mendelian systemic lupus erythematosus with B cell-defective apoptosis and hyperproliferation. Arthritis Rheum (2013) 65:2161–71. doi:10.1002/art.38008
44. Griner EM, Kazanietz MG. Protein kinase C and other diacylglycerol effectors in cancer. Cancer (2007) 7:281–94. doi:10.1038/nrc2110
45. Limnander A, Depeille P, Freedman TS, Liou J, Leitges M, Kurosaki T, et al. STIM1, PKC-delta and RasGRP set a threshold for proapoptotic Erk signaling during B cell development. Nat Immunol (2011) 12:425–33. doi:10.1038/ni.2016
46. Miyamoto A, Nakayama K, Imaki H, Hirose S, Jiang Y, Abe M, et al. Increased proliferation of B cells and auto-immunity in mice lacking protein kinase C delta. Nature (2002) 416:865–9. doi:10.1038/416865a
47. Lopez-Herrera G, Tampella G, Pan-Hammarström Q, Herholz P, Trujillo-Vargas CM, Phadwal K, et al. Deleterious mutations in LRBA are associated with a syndrome of immune deficiency and autoimmunity. Am J Hum Genet (2012) 90:986–1001. doi:10.1016/j.ajhg.2012.04.015
48. Alangari A, Alsultan A, Adly N, Massaad MJ, Kiani IS, Aljebreen A, et al. LPS-responsive beige-like anchor (LRBA) gene mutation in a family with inflammatory bowel disease and combined immunodeficiency. J Allergy Clin Immunol (2012) 130:481–8. doi:10.1016/j.jaci.2012.05.043
49. Serwas NK, Kansu A, Santos-Valente E, Kuloglu Z, Demir A, Yaman A, et al. Atypical manifestation of LRBA deficiency with predominant IBD-like phenotype. Inflamm Bowel Dis (2015) 21:40–7. doi:10.1097/MIB.0000000000000266
50. Burns SO, Zenner HL, Plagnol V, Curtis J, Mok K, Eisenhut M, et al. LRBA gene deletion in a patient presenting with autoimmunity without hypogammaglobulinemia. J Allergy Clin Immunol (2012) 130:1428–32. doi:10.1016/j.jaci.2012.07.035
51. Charbonnier LM, Janssen E, Chou J, Ohsumi TK, Keles S, Hsu JT, et al. Regulatory T-cell deficiency and immune dysregulation, polyendocrinopathy, enteropathy, X-linked-like disorder caused by loss-of-function mutations in LRBA. J Allergy Clin Immunol (2015) 135:217.e–27.e. doi:10.1016/j.jaci.2014.10.019
52. Kuehn HS, Ouyang W, Lo B, Deenick EK, Niemela JE, Avery DT, et al. Immune dysregulation in human subjects with heterozygous germline mutations in CTLA4. Science (2014) 345:1623–7. doi:10.1126/science.1255904
53. Tivol EA, Borriello F, Schweitzer AN, Lynch WP, Bluestone JA, Sharpe AH. Loss of CTLA-4 leads to massive lymphoproliferation and fatal multiorgan tissue destruction, revealing a critical negative regulatory role of CTLA-4. Immunity (1995) 3:541–7. doi:10.1016/1074-7613(95)90125-6
54. Waterhouse P, Penninger JM, Timms E, Wakeham A, Shahinian A, Lee KP, et al. Lymphoproliferative disorders with early lethality in mice deficient in Ctla-4. Science (1995) 270:985–8. doi:10.1126/science.270.5238.985
55. Hori S, Nomura T, Sakaguchi S. Control of regulatory T cell development by the transcription factor Foxp3. Science (2003) 299:1057–61. doi:10.1126/science.1079490
56. Fontenot JD, Gavin MA, Rudensky AY. Foxp3 programs the development and function of CD4+CD25+ regulatory T cells. Nat Immunol (2003) 4:330–6. doi:10.1038/ni904
57. Khattri R, Cox T, Yasayko S-A, Ramsdell F. An essential role for scurfin in CD4+CD25+ T regulatory cells. Nat Immunol (2003) 4:337–42. doi:10.1038/ni909
58. Qureshi OS, Zheng Y, Nakamura K, Attridge K, Manzotti C, Schmidt EM, et al. Trans-endocytosis of CD80 and CD86: a molecular basis for the cell-extrinsic function of CTLA-4. Science (2011) 332:600–3. doi:10.1126/science.1202947
59. Walker LSK, Sansom DM. The emerging role of CTLA4 as a cell-extrinsic regulator of T cell responses. Nat Rev Immunol (2011) 11:852–63. doi:10.1038/nri3108
60. Elkaim E, Neven B, Bruneau J, Mitsui-Sekinaka K, Stanislas A, Heurtier L, et al. Clinical and immunologic phenotype associated with activated phosphoinositide 3-kinase δ syndrome 2: a cohort study. J Allergy ClinImmunol (2016) 138:210.e–8.e. doi:10.1016/j.jaci.2016.03.022
61. Deau MC, Heurtier L, Frange P, Suarez F, Bole-Feysot C, Nitschke P, et al. A human immunodeficiency caused by mutations in the PIK3R1 gene. J Clin Invest (2014) 124:3923–8. doi:10.1172/JCI75746
62. Lehman HK. Autoimmunity and immune dysregulation in primary immune deficiency disorders. Curr Allergy Asthma Rep (2015) 15:53. doi:10.1007/s11882-015-0553-x
63. Hess S, Engelmann H. A novel function of CD40: induction of cell death in transformed cells. J Exp Med (1996) 183:159–67. doi:10.1084/jem.183.1.159
64. Levy J, Espanol-Boren T, Thomas C, Fischer A, Tovo P, Bordigoni P, et al. Clinical spectrum of X-linked hyper-IgM syndrome. J Pediatr (1997) 131:47–54. doi:10.1016/S0022-3476(97)70123-9
65. Quartier P, Bustamante J, Sanal O, Plebani A, Debré M, Deville A, et al. Clinical, immunologic and genetic analysis of 29 patients with autosomal recessive hyper-IgM sundrome due to activation-induced cytidine deaminase deficiency. Clin Immunol (2004) 110:22–9. doi:10.1016/j.clim.2003.10.007
66. Orange JS, Levy O, Geha RS. Human disease resulting from gene mutations that interfere with appropriate nuclear factor-κB activation. Immunol Rev (2005) 203:21–37. doi:10.1111/j.0105-2896.2005.00221.x
67. Hervé M, Isnardi I, Ng YS, Bussel JB, Ochs HD, Cunningham-Rundles C, et al. CD40 ligand and MHC class II expression are essential for human peripheral B cell tolerance. J Exp Med (2007) 204:1583–93. doi:10.1084/jem.20062287
68. Lougaris V, Badolato R, Ferrari S, Plebani A. Hyper immunoglobulin M syndrome due to CD40 deficiency: clinical, molecular, and immunological features. Immunol Rev (2005) 203:48–66. doi:10.1111/j.0105-2896.2005.00229.x
69. Griffith LM, Cowan MJ, Notarangelo LD, Puck JM, Buckley RH, Candotti F, et al. Improving cellular therapy for primary immune deficiency diseases: recognition, diagnosis, and management. J Allergy Clin Immunol (2009) 6:1152–60. doi:10.1016/j.jaci.2009.10.022
70. Cirillo E, Giardino G, Gallo V, D’Assante R, Grasso F, Romano R, et al. Severe combined immunodeficiency – an update. Ann N Y Acad Sci (2015) 1356:90–106. doi:10.1111/nyas.12849
71. Kelly BT, Tam JS, Verbsky JW, Routes JM. Screening for severe combined immunodeficiency in neonates. Clin Epidemiol (2013) 5:363–9. doi:10.2147/CLEP.S48890
72. Yu GP, Nadeau KC, Berk DR, de Saint Basile G, Lambert N, Knapnougel P, et al. Genotype, phenotype, and outcomes of nine patients with T-B+NK+SCID. Pediatr Transplant (2011) 15:733–41. doi:10.1111/j.1399-3046.2011.01563.x
73. Giliani S, Bonfim C, de Saint Basile G, Lanzi G, Brousse N, Koliski A, et al. Omenn syndrome in an infant with IL7RA gene mutation. J Pediatr (2006) 148:272–4. doi:10.1016/j.jpeds.2005.10.004
74. Vu QV, Wada T, Toma T, Tajima H, Maeda M, Tanaka R, et al. Clinical and immunophenotypic features of atypical complete DiGeorge syndrome. Pediatr Int (2013) 55:2–6. doi:10.1111/j.1442-200X.2012.03722.x
75. Rucci F, Poliani PL, Caraffi S, Paganini T, Fontana E, Giliani S, et al. Abnormalities of thymic stroma may contribute to immune dysregulation in murine models of leaky severe combined immunodeficiency. Front Immunol (2011) 2:15. doi:10.3389/fimmu.2011.00015
76. Cavadini P, Vermi W, Facchetti F, Fontana S, Nagafuchi S, Mazzolari E, et al. AIRE deficiency in thymus of 2 patients with Omenn syndrome. J Clin Invest (2005) 115:728–32. doi:10.1172/JCI200523087
77. Cassani B, Poliani PL, Moratto D, Sobacchi C, Marrella V, Imperatori L, et al. Defect of regulatory T cells in patients with Omenn syndrome. J Allergy Clin Immunol (2010) 125(1):209–16. doi:10.1016/j.jaci.2009.10.023
79. Buck D, Malivert L, de Chasseval R, Barraud A, Fondanèche MC, Sanal O, et al. Cernunnos, a novel nonhomologous end-joining factor, is mutated in human immunodeficiency with microcephaly. Cell (2006) 124:287–99. doi:10.1016/j.cell.2005.12.030
80. de Villartay JP, Lim A, Al-Mousa H, Dupont S, Déchanet-Merville J, Coumau-Gatbois E, et al. A novel immunodeficiency associated with hypomorphic RAG1 mutations and CMV infection. J Clin Invest (2005) 115:3291–9. doi:10.1172/JCI25178
81. Enders A, Fisch P, Schwarz K, Duffner U, Pannicke U, Nikolopoulos E, et al. A severe form of human combined immunodeficiency due to mutations in DNA ligase IV. J Immunol (2006) 176(8):5060–8. doi:10.4049/jimmunol.176.8.5060
82. Pasic SD, Dijuricic S, Ristic G, Slavkovic B. Recombinase-activating gene 1immunodeficiency: different immunological phenotypes in three siblings. Acta Paediatr (2009) 98:1062–4. doi:10.1111/j.1651-2227.2009.01250.x
83. Picard C, McCarl CA, Papolos A, Khalil S, Luthy K, Hivroz C, et al. STIM1 mutation associated witha syndrome of immunodeficiency and autoimmunity. N Engl J Med (2009) 360:1971–80. doi:10.1056/NEJMoa0900082
84. Fuchs S, Rensing-Ehl A, Speckmann C, Bengsch B, Schmitt-Graeff A, Bondzio I, et al. Antiviral and regulatory T cell immunity in a patient with stromal interaction molecule 1 deficiency. J Immunol (2012) 188:1523–33. doi:10.4049/jimmunol.1102507
85. Binder V, Albert MH, Kabus M, Bertone M, Meindl A, Belohradsky BH. The genotype of the originalWiskott phenotype. N Engl J Med (2006) 355:1790–3. doi:10.1056/NEJMoa062520
86. Kirchhausen T, Rosen FS. Disease mechanism: unravelling Wiskott-Aldrich syndrome. Curr Biol (1996) 6:676–8. doi:10.1016/S0960-9822(09)00447-3
87. Sullivan KE, Mullen CA, Blaese RM, Winkelstein JA. A multiinstitutional survey of the Wiskott-Aldrich syndrome. J Pediatr (1994) 125:876–85. doi:10.1016/S0022-3476(05)82002-5
88. Ancliff PJ, Blundell MP, Cory GO, Calle Y, Worth A, Kempski H, et al. Two novel activating mutations in theWiskott-Aldrich syndrome protein result in congenital neutropenia. Blood (2006) 108:2182–9. doi:10.1182/blood-2006-01-010249
89. Zhu Q, Zhang M, Blaese RM, Derry JM, Junker A, Francke U, et al. The Wiskott-Aldrich syndrome and X-linked congenital thrombocytopenia are caused by mutations of the same gene. Blood (1995) 86:3797–804.
90. Beel K, Cotter MM, Blatny J, Bond J, Lucas G, Green F, et al. A large kindred with X-linked neutropenia with an I294T mutation of the Wiskott-Aldrich syndrome gene. Br J Haematol (2009) 144:120–6. doi:10.1111/j.1365-2141.2008.07416.x
91. Miki H, Sasaki T, Takai Y, Takenawa T. Induction of filopodium formation by aWASP-related actin-depolymerizing proteinN-WASP. Nature (1998) 391:93–6. doi:10.1038/34208
92. Bear JE, Rawls JF, Saxe CL. SCAR, aWASPrelated protein, isolated as a suppressor of receptor defects in late Dictyostelium development. J Cell Biol (1998) 142:1325–35. doi:10.1083/jcb.142.5.1325
93. Dupuis S, Jouanguy E, Al-Hajjar S, Fieschi C, Al-Mohsen IZ, Al-Jumaah S, et al. Impaired response to interferon-α/β and lethal viral disease in human STAT1 deficiency. Nat Genet (2003) 33:388–91. doi:10.1038/ng1097
94. Schurman SH, Candotti F. Autoimmunity in Wiskott-Aldrich syndrome. Curr Opin Rheumatol (2003) 15:446–53. doi:10.1097/00002281-200307000-00012
95. Imai K, Morio T, Zhu Y, Jin Y, Itoh S, Kajiwara M, et al. Clinical course of patients withWASP gene mutations. Blood (2004) 103:456–64. doi:10.1182/blood-2003-05-1480
96. Sakaguchi S. Naturally arising Foxp3-expressing CD25+CD4+ regulatory T cells in immunological tolerance to self and non-self. Nat Immunol (2005) 6:345–52. doi:10.1038/ni1178
97. Shevach EM. CD4+CD25+suppressorTcells: more questions than answers. Nat Rev Immunol (2002) 2:389–400. doi:10.1038/nri821
98. Adriani M, Aoki J, Horai R, Thornton AM, Konno A, Kirby M, et al. Impaired in vitro regulatory T cell function associated with Wiskott-Aldrich syndrome. Clin Immunol (2007) 124:41–8. doi:10.1016/j.clim.2007.02.001
99. Marangoni F, Trifari S, Scaramuzza S, Panaroni C, Martino S, Notarangelo LD, et al. WASP regulates suppressor activity of human and murine CD4(+)CD25(+)FOXP3(+) natural regulatory T cells. J Exp Med (2007) 204:369–80. doi:10.1084/jem.20061334
100. Maillard MH, Cotta de Almeida V, Takeshima F, Nguyen DD, Michetti P, Nagler C, et al. The Wiskott-Aldrich syndrome protein is required for the function of CD4(+)CD25(+)Foxp3(+) regulatory T cells. J Exp Med (2007) 204:381–91. doi:10.1084/jem.20061338
101. Shimizu M, Nikolov NP, Ueno K, Ohta K, Siegel RM, Yachie A, et al. Development of IgA nephropathylike glomerulonephritis associated with Wiskott-Aldrich syndrome protein deficiency. Clin Immunol (2011) 142:160–6. doi:10.1016/j.clim.2011.10.001
102. Recher M, Burns SO, de la Fuente MA, Volpi S, Dahlberg C, Walter JE, et al. B cell-intrinsic deficiency of the Wiskott-Aldrich syndrome protein (WASp) causes severe abnormalities of the peripheral B-cell compartment in mice. Blood (2012) 119:2819–28. doi:10.1182/blood-2011-09-379412
104. Jawad AF, McDonald-McGinn DM, Zackai E, Sullivan KE. Immunologic features of chromosome 22q11.2 deletion syndrome (DiGeorge syndrome/velocardiofacial syndrome). J Pediatr (2001) 139:715–23. doi:10.1067/mpd.2001.118534
105. Giardino G, Cirillo E, Maio F, Gallo V, Esposito T, Naddei R, et al. Gastrointestinal involvement in patients affected with 22q11.2 deletion syndrome. Scand J Gastroenterol (2014) 49:274–9. doi:10.3109/00365521.2013.855814
106. Sullivan KE, McDonald-McGinn D, Driscoll DA, Emanuel BS, Zackai EH, Jawad AF. Longitudinal analysis of lymphocyte function and numbers in the first year of life in chromosome 22q11.2 deletion syndrome (DiGeorge syndrome/velocardiofacial syndrome). Clin Diagn Lab Immunol (1999) 6:906–11.
107. Sullivan KE, McDonald-McGinn DM, Driscoll DA, Zmijewski CM, Ellabban AS, Reed L, et al. Juvenile rheumatoid arthritis-like polyarthritis in chromosome 22q11.2 deletion syndrome (DiGeorge anomalad/velocardiofacial syndrome/conotruncal anomaly face syndrome). Arthritis Rheum (1997) 40:430–6. doi:10.1002/art.1780400307
108. Davies JK, Telfer P, Cavenagh JD, Foot N, Neat M. Autoimmune cytopenias in the 22q11.2 deletion syndrome. Clin Lab Haematol (2003) 25:195–7. doi:10.1046/j.1365-2257.2003.00508.x
109. Brown JJ, Datta V, Browning MJ, Swift PG. Graves’ disease in DiGeorge syndrome: patient report with a review of endocrine autoimmunity associated with 22q11.2 deletion. J Pediatr Endocrinol Metab (2004) 17:1575–9. doi:10.1515/JPEM.2004.17.11.1575
110. Markert ML. Treatment of infants with complete DiGeorge anomaly. J Allergy Clin Immunol (2008) 121:1063. doi:10.1016/j.jaci.2007.12.1181
111. Markert ML, Marques J, Neven B, Devlin B, McCarthy E, Chinn I, et al. First use of thymus transplantation therapy for Foxn1 deficiency (nude/SCID): a report of two cases. Blood (2011) 117:688–96. doi:10.1182/blood-2010-06-292490
112. Hong R, Ammann AJ. Ataxia telangiectasia. N Engl J Med (1970) 283:660. doi:10.1056/NEJM197009172831220
113. Hori T, Ohnishi H, Teramoto T, Tsubouchi K, Naiki T, Hirose Y, et al. Autosomal-dominant chronic mucocutaneous candidiasis with STAT1-mutation can be complicated with chronic active hepatitis and hypothyroidism. J Clin Immunol (2012) 32:1213–20. doi:10.1007/s10875-012-9744-6
114. Liu L, Okada S, Kong X-F, Kreins AY, Cypowyj S, Abhyankar A, et al. Gain-of-function human STAT1 mutations impair IL-17 immunity and underlie chronic mucocutaneous candidiasis. J Exp Med (2011) 208:1635–48. doi:10.1084/jem.20110958
115. Dotta L, Scomodon O, Padoan R, Timpano S, Plebani A, Soresina A, et al. Clinical heterogeneity of dominant chronic mucocutaneous candidiasis disease: presenting as treatment-resistant candidiasis and chronic lung disease. Clin Immunol (2016) 164:1–9. doi:10.1016/j.clim.2015.12.010
116. Toubiana J, Okada S, Hiller J, Oleastro M, Lagos Gomez M, Aldave Becerra JC, et al. Heterozygous STAT1 gain-of-function mutations underlie an unexpectedly broad clinical phenotype. Blood (2016) 127:3154–64. doi:10.1182/blood-2015-11-679902
117. Giardino G, Somma D, Cirillo E, Ruggiero G, Terrazzano G, Rubino V, et al. Novel STAT1 gain-of-function mutation and suppurative infections. Pediatr Allergy Immunol (2016) 27:220–3. doi:10.1111/pai.12496
118. Dotta L, Scomodon O, Padoan R, Timpano S, Plebani A, Soresina A, et al. Clinical and immunological data of nine patients with chronic mucocutaneous candidiasis disease. Data Brief (2016) 7:311–5. doi:10.1016/j.dib.2016.02.040
119. Sampaio EP, Hsu AP, Pechacek J, Bax HI, Dias DL, Paulson ML, et al. Signal transducer and activator of transcription 1 (STAT1) gain-of-function mutations and disseminated coccidioidomycosis and histoplasmosis. J Allergy Clin Immunol (2013) 131:1624–34. doi:10.1016/j.jaci.2013.01.052
120. Frans G, Moens L, Schaballie H, Van Eyck L, Borgers H, Wuyts M, et al. Gain-of-function mutations in signal transducer and activator of transcription 1 (STAT1): chronic mucocutaneous candidiasis accompanied by enamel defects and delayed dental shedding. J Allergy Clin Immunol (2014) 134:1209–13. doi:10.1016/j.jaci.2014.05.044
121. Uzel G, Sampaio EP, Lawrence MG, Hsu AP, Hackett M, Dorsey MJ, et al. Dominant gain-of-function STAT1 mutations in FOXP3(WT) IPEX-like syndrome. J Allergy Clin Immunol (2013) 131:1611.e–23.e. doi:10.1016/j.jaci.2012.11.054
122. Flanagan SE, Haapaniemi E, Russell MA, Caswell R, Allen HL, De Franco E, et al. Activating germline mutations in STAT3 cause early-onset multi-organ autoimmune disease. Nat Genet (2014) 46:812–4. doi:10.1038/ng.3040
123. Haapaniemi EM, Kaustio M, Rajala HLM, van Adrichem AJ, Kainulainen L, Glumoff V, et al. Autoimmunity, hypogammaglobulinemia, lymphoproliferation, and mycobacterial disease in patients with activating mutations in STAT3. Blood (2015) 125:639–48. doi:10.1182/blood-2014-04-570101
Keywords: autoimmunity, immunodeficiency, autoimmune hemolytic anemia, immune thrombocytopenia, systemic lupus erytematous
Citation: Giardino G, Gallo V, Prencipe R, Gaudino G, Romano R, De Cataldis M, Lorello P, Palamaro L, Di Giacomo C, Capalbo D, Cirillo E, D’Assante R and Pignata C (2016) Unbalanced Immune System: Immunodeficiencies and Autoimmunity. Front. Pediatr. 4:107. doi: 10.3389/fped.2016.00107
Received: 11 June 2016; Accepted: 20 September 2016;
Published: 06 October 2016
Edited by:
Rita Consolini, University of Pisa, ItalyReviewed by:
Lisa Renee Forbes, Baylor College of Medicine, USAJustin Wahlstrom, University of California San Francisco, USA
Copyright: © 2016 Giardino, Gallo, Prencipe, Gaudino, Romano, De Cataldis, Lorello, Palamaro, Di Giacomo, Capalbo, Cirillo, D’Assante and Pignata. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Claudio Pignata, pignata@unina.it
 Giuliana Giardino
Giuliana Giardino Vera Gallo
Vera Gallo Rosaria Prencipe
Rosaria Prencipe Giovanni Gaudino
Giovanni Gaudino Roberta Romano
Roberta Romano Marco De Cataldis
Marco De Cataldis Paola Lorello
Paola Lorello
 Loredana Palamaro
Loredana Palamaro Chiara Di Giacomo
Chiara Di Giacomo Emilia Cirillo
Emilia Cirillo Roberta D’Assante
Roberta D’Assante Claudio Pignata
Claudio Pignata