- University Claude Bernard Lyon 1, UMR 5246 Centre National de la Recherche Scientifique - University Lyon 1 - Institut National des Sciences Appliquées de Lyon - École Supérieure de Chimie Physique Électronique de Lyon, Villeurbanne, France
The extracellular matrix (ECM) is a source of bioactive fragments called matricryptins or matrikines resulting from the proteolytic cleavage of extracellular proteins (e.g., collagens, elastin, and laminins) and proteoglycans (e.g., perlecan). Matrix metalloproteinases (MMPs), cathepsins, and bone-morphogenetic protein-1 release fragments, which regulate physiopathological processes including tumor growth, metastasis, and angiogenesis, a pre-requisite for tumor growth. A number of matricryptins, and/or synthetic peptides derived from them, are currently investigated as potential anti-cancer drugs both in vitro and in animal models. Modifications aiming at improving their efficiency and their delivery to their target cells are studied. However, their use as drugs is not straightforward. The biological activities of these fragments are mediated by several receptor families. Several matricryptins may bind to the same matricellular receptor, and a single matricryptin may bind to two different receptors belonging or not to the same family such as integrins and growth factor receptors. Furthermore, some matricryptins interact with each other, integrins and growth factor receptors crosstalk and a signaling pathway may be regulated by several matricryptins. This forms an intricate 3D interaction network at the surface of tumor and endothelial cells, which is tightly associated with other cell-surface associated molecules such as heparan sulfate, caveolin, and nucleolin. Deciphering the molecular mechanisms underlying the behavior of this network is required in order to optimize the development of matricryptins as anti-cancer agents.
Introduction
Matricryptins are biologically active fragments released from extracellular matrix (ECM) proteins and glycosaminoglycans by proteases (Davis et al., 2000). We have extended the definition of matricryptins to the ectodomains of membrane collagens and membrane proteoglycans, which are released in the ECM by sheddases, and to fragments of ECM-associated enzymes such as lysyl oxidase, which initiates the covalent cross-linking of collagens and elastin, and matrix metalloproteinases (MMPs), which contribute to ECM remodeling (Ricard-Blum and Salza, 2014; Ricard-Blum and Vallet, 2015). The molecular functions of matricryptins and the biological processes they regulate have been reviewed with a focus on collagen and proteoglycan matricryptins (Ricard-Blum and Ballut, 2011), on matricryptins regulating tissue repair (Ricard-Blum and Salza, 2014), angiogenesis (Sund et al., 2010; Boosani and Sudhakar, 2011; Gunda and Sudhakar, 2013), cancer (Monboisse et al., 2014), and on the proteases releasing matricryptins (Ricard-Blum and Vallet, 2015).
Synthetic peptides and/or domains derived from matricryptin sequences and recapitulating their biological roles are also able to regulate angiogenesis and/or cancer in various tumor cells and cancer models (Rosca et al., 2011). They include sequences of tumstatin (He et al., 2010; Han et al., 2012; Wang et al., 2015a), laminins (Kikkawa et al., 2013), endostatin (Morbidelli et al., 2003), endorepellin (Willis et al., 2013), and the hemopexin domain of MMP-9 (Ugarte-Berzal et al., 2012, 2014). Neither these peptides nor the ectodomains of membrane collagens and syndecans are described here due to space limitation. We focus on the major matricryptins, which control cancer, metastasis, and angiogenesis, a pre-requisite for tumor growth and a therapeutic target (Folkman, 1971; Welti et al., 2013; Huang et al., 2015), and on their receptors.
Regulation of Angiogenesis, Tumor Growth and Metastasis by Matricryptins
Matricryptins regulate wound healing, fibrosis, inflammation, angiogenesis, and cancer and are involved in infectious and neurodegenerative diseases (Ricard-Blum and Ballut, 2011; Ricard-Blum and Salza, 2014; Ricard-Blum and Vallet, 2015). Most of the matricryptins regulating angiogenesis and tumor growth are derived from collagens IV and XVIII (Monboisse et al., 2014; Walia et al., 2015), elastin (Robinet et al., 2005; Pocza et al., 2008; Heinz et al., 2010), fibronectin (Ambesi et al., 2005), laminins (Tran et al., 2008), osteopontin (Bayless and Davis, 2001; Lund et al., 2009; Yamaguchi et al., 2012), MMPs (Bello et al., 2001; Ezhilarasan et al., 2009), proteoglycans (Goyal et al., 2011), and hyaluronan (Cyphert et al., 2015; Table 1). They are released from the ECM by a variety of proteinases (matrixins, adamalysins, tolloids, cathepsins, thrombin, and plasmin; Ricard-Blum and Vallet, 2015; Wells et al., 2015).
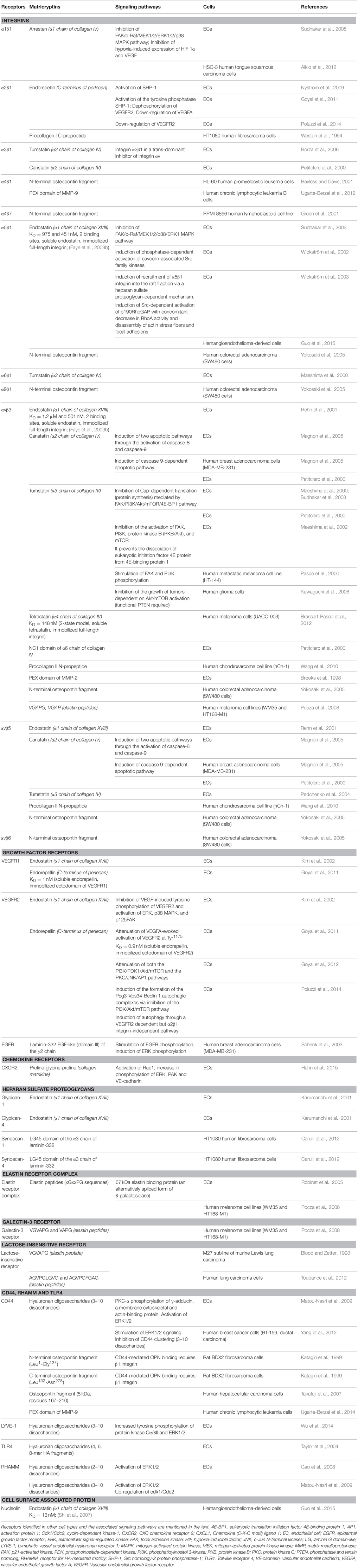
Table 1. Matricryptins, receptors, and signaling pathways regulated by matricryptins in endothelial and tumor cells.
Matricryptins regulating angiogenesis and tumor growth target endothelial cells and/or tumor cells (Robinet et al., 2005; Tran et al., 2008; Sund et al., 2010; Boosani and Sudhakar, 2011; Ricard-Blum and Ballut, 2011; Toupance et al., 2012; Kikkawa et al., 2013; Monboisse et al., 2014; Ricard-Blum and Salza, 2014; Monslow et al., 2015; Nikitovic et al., 2015; Ricard-Blum and Vallet, 2015; Walia et al., 2015). Several matricryptins inhibit the proliferation and the migration of endothelial cells, block cell cycle at G1 as shown for anastellin (Ambesi et al., 2005) and endostatin (Hanai et al., 2002) and induce apoptosis. Arresten, derived from the C-terminus of the α1 chain of collagen IV, activates FasL mediated apoptosis for example (Verma et al., 2013). Endostatin and endorepellin, a matricryptin of perlecan, induce autophagy of endothelial cells, the autophagic activity of endorepellin being mediated by a VEGFR2-dependent pathway (Nguyen et al., 2009; Poluzzi et al., 2014). A modified endostatin (Endostar) induces autophagy in hepatoma cells (Wu et al., 2008). Matricryptins normalize tumor vasculature, which improves the delivery of cytotoxic drugs to the tumor and hence the response to anti-cancer treatments (Jain, 2005). Endostatin contributes to the normalization of tumor vasculature in a lung cancer model (Ning et al., 2012), and in esophageal squamous cell carcinoma, where it enhances the effect of radiotherapy and reduces hypoxia (Zhu et al., 2015), possibly by a crosstalk between cancer and endothelial cells mediated by the Hypoxia-Inducible Factor and VEGF expression.
Matricryptins derived from collagens IV and XVIII target tumoral cells. Arresten inhibits migration and invasion of squamous cell carcinoma and induces their death (Aikio et al., 2012). Endostatin inhibits the proliferation of some cancer cells (e.g., the HT29 human colorectal adenocarcinoma cell line) but not of others (e.g., the MDA-MB-231 human mammary adenocarcinoma cell line) (Ricard-Blum et al., 2004). Matricryptins enhance the sensitivity of tumor cells to a cytotoxic drug and even reverse in part their resistance to this drug. A tumstatin peptide increases the sensitivity of non-small cell lung carcinoma cells to cisplatin (Wang et al., 2015c) and Endostar enhances the sensitivity to radiation of nasopharyngeal carcinoma and lung adenocarcinoma xenografts in mice (Wen et al., 2009).
Matricryptins regulate angiogenesis, tumor growth, and metastasis by various molecular mechanisms. The anti-angiogenic activities of tumstatin and endostatin contribute to tumor suppression by p53 via the upregulation of the α(II) collagen prolylyl hydroxylase (Folkman, 2006; Teodoro et al., 2006). Endostatin inhibits proliferation and migration of glioblastoma cells by inhibiting T-type Ca2+ channels (Zhang et al., 2012), and its ATPase activity contributes to its anti-angiogenic and antitumor properties (Wang et al., 2015b). This matricryptin inhibits hemangioendothelioma by downregulating chemokine (C-X-C motif) ligand 1 via the inactivation of NF–κB (Guo et al., 2015).
Receptors and Co-receptors of Matricryptins
Matricryptins regulating angiogenesis, tumor growth and metastasis bind to several receptors, and co-receptors (Figure 1, Faye et al., 2009a) to modulate signaling pathways and fulfill their biological functions (Table 1). The other ligands of the receptors (e.g., ECM proteins, proteoglycans, growth factors, and chemokines) are not represented in Figure 1 for the sake of clarity. Pathways regulated by matricryptins in endothelial or tumor cells via unidentified receptors and/or in other cell types are mentioned below but are not listed in Table 1.
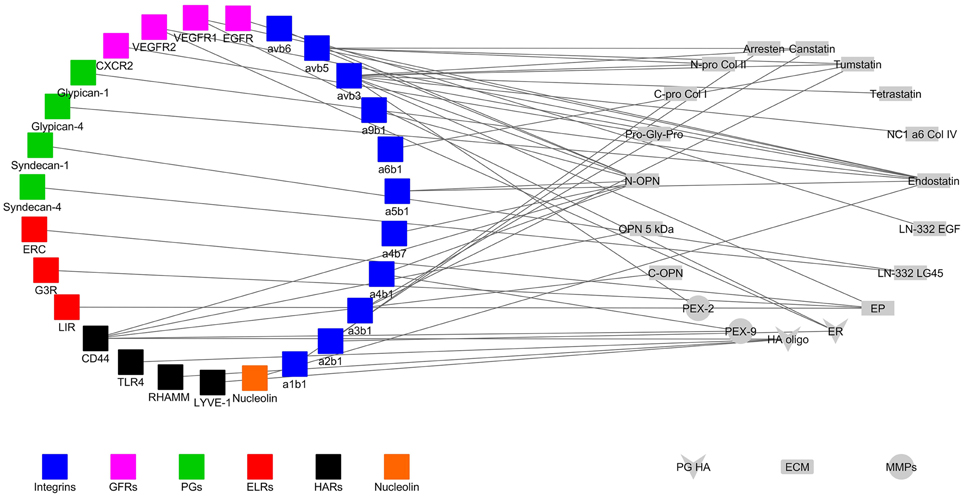
Figure 1. Interaction network of matricryptins (right) and their receptors (left) expressed at the surface of endothelial and cancer cells. ab, alpha and beta integrin subunits; C-Pro Col, C-propeptide of procollagen; CXCR, chemokine CXC receptor; ECM, extracellular matrix; EGF, epidermal growth factor; EGFR, epidermal growth factor receptor; EP, elastin peptide; ER, endorepellin; ERC, elastin receptor complex; ELR, elastin receptor; ES, endostatin; G3R, galectin-3 receptor; GFR, growth factor receptor; HA oligo, hyaluronan oligosaccharide; HAR, hyaluronan receptor; LN LG45, laminin domain LG45; LIR, lactose insensitive receptor; LYVE-1, lymphatic vessel endothelial hyaluronan receptor 1; N-Pro Col, N-propeptide of procollagen; MMP, matrix metalloproteinase; NC1, non-collagenous domain; OPN, osteopontin; PEX, hemopexin domain; PG, proteoglycan; RHAMM, receptor for hyaluronic acid-mediated motility; TLR4, toll-like receptor; VEGFR, vascular endothelial growth factor receptor.
Integrins
There are 24 integrins comprised of an α subunit and a β subunit (Barczyk et al., 2010). They lack intrinsic kinase activity and are the major adhesion receptors of the ECM, controlling ECM assembly, cell-matrix interactions, cell migration, and tumor growth (Missan and DiPersio, 2012; Xiong et al., 2013). A number of matricryptins bind to integrins at the surface of tumor and/or endothelial cells (Table 1). Matricryptins also interact with purified integrins (e.g., αvβ5 integrin for endostatin; Rehn et al., 2001; Faye et al., 2009b), or on other cell types. The αvβ3 integrin is the main receptor targeted by matricryptins (Figure 1).
Anastellin decreases the activation state of α5β1 integrin on endothelial cells (Ambesi and McKeown-Longo, 2014). Arresten interacts with α3β1/αvβ3 and α1β1/α2β1 integrins at the surface of HPV-16-immortalized proximal tubular epithelial cells and mesangial cells respectively, whereas tumstatin binds to immortalized glomerular epithelial cells through α3β1 and α2β1 integrins (Aggeli et al., 2009). The above integrins are also involved in the effects of matricryptins on other cell types. Endostatin, generated by cerebellar Purkinje cells, contributes to the organization of climbing fiber terminals in these neurons by binding and signaling through α3β1 integrin (Su et al., 2012). The adhesion of smooth muscle cells to anastellin is mediated by both β1 integrins and cell surface heparan sulfate proteoglycans, which triggers ERK1/2 activation in these cells (Mercurius and Morla, 2001) and the induction of osteoclast apoptosis by the N-propeptide of procollagen II is mediated by αv or β3 integrin subunits (Hayashi et al., 2011).
Growth Factor and Chemokine Receptors
Growth factor receptors belong to the tyrosine kinase receptor family. They regulate cell proliferation, differentiation, cell cycle, survival and apoptosis and play a role in cancer (McDonell et al., 2015). VEGR receptors 1–3 (Roskoski, 2008; Grünewald et al., 2010; Simons, 2012) and EGF receptor (Lemmon et al., 2014) interact with matricryptins (Table 1). Two endostatin peptides bind to VEGFR3 (Han et al., 2012, 2015) and EGF-like repeats of tenascin C interact with EGFR, inducing phosphorylation of the receptor and of ERK MAP kinases in NR6 mouse fibroblasts (Swindle et al., 2001). Endorepellin simultaneously engages VEGFR2 and α2β1 integrin, both expressed by endothelial cells, and regulate angiogenesis and autophagy through a dual receptor antagonism (Goyal et al., 2011; Poluzzi et al., 2014). Anastellin inhibits lysophospholipid (Ambesi and McKeown-Longo, 2009) and VEGF165-dependent signaling in endothelial cells by preventing the formation of the complex containing VEGFR2 and neuropilin-1 at the surface of endothelial cells (Ambesi and McKeown-Longo, 2014). One matricryptin of collagen I interacts with a member of the chemokine receptor family, the CXC chemokine receptor 2 (Stadtmann and Zarbock, 2012; Veenstra and Ransohoff, 2012).
Cell Surface Proteoglycans
Proteoglycans are divided into intracellular, pericellular, extracellular, and cell-surface families (Iozzo and Schaefer, 2015). Syndecans are transmembrane heparan sulfate proteoglycans (Couchman et al., 2015), which play a role in cell adhesion, migration, receptor trafficking, growth factor interactions, angiogenesis (De Rossi and Whiteford, 2014) and cancer (Barbouri et al., 2014). They are enzymatically shed from the cell surface and compete with their membrane forms for ligand binding (Manon-Jensen et al., 2010). They act in synergy with integrins to control cell adhesion and other biological processes (Morgan et al., 2007; Roper et al., 2012; Humphries et al., 2015), and the binding of heparan sulfate chains to integrin α5β1 promotes cell adhesion and spreading (Faye et al., 2009b). Syndecans act as co-receptors of VEGF and control tumor progression in association with integrins (Grünewald et al., 2010; Soares et al., 2015). Glypicans, membrane-associated proteoglycans with a glycosylphosphatidyl anchor, regulate Wnt, Hedgehog, fibroblast growth factor, and bone morphogenetic protein signaling (Filmus et al., 2008; Iozzo and Schaefer, 2015). One matricryptin, endostatin, binds to glypicans via their heparan sulfate chains (Karumanchi et al., 2001).
Elastin Receptors
The Elastin Receptor Complex (ERC) is composed of two membrane associated proteins (the protective protein/cathepsin A and neuraminidase-1) and of the elastin-binding protein, an inactive spliced variant of lysosomal β-galactosidase (Blanchevoye et al., 2013). Elastin peptides activate extracellular signal-regulated kinase 1/2 via a Ras-independent mechanism in fibroblasts (Duca et al., 2005), the enzymatic activity of neuraminidase-1 being responsible for signal transduction (Duca et al., 2007). Another, still unidentified, receptor of elastin peptides exists at the surface of macrophages (Maeda et al., 2007). Furthermore, elastin peptides regulate tumor cell migration and invasion through an Hsp90-dependent mechanism (Donet et al., 2014).
CD44, Receptor for HA-Mediated Motility (RHAMM) and Toll-Like Receptors (TLRs)
Hyaluronan, a non-sulfated glycosaminoglycan, has two major receptors, CD44 and RHAMM, which mediate its roles in inflammation and cancer (Toole, 2009; Misra et al., 2015; Nikitovic et al., 2015). The binding to, and activation of, receptors depend on the size of HA, its oligosaccharides stimulating angiogenesis (Gao et al., 2008). CD44, which has several isoforms regulates cell proliferation, adhesion and migration, and is involved in tumorigenesis (Jordan et al., 2015). A sequence in the hemopexin domain of MMP-9 (PEX9) impairs tumor cell adhesion to PEX9/MMP9 through interaction with CD44 (Ugarte-Berzal et al., 2014). RHAMM has splicing variants and is located inside the cell and on the cell surface, where it is anchored via a glycosylphosphatidylinositol (Tolg et al., 2014; Misra et al., 2015). Toll-like receptors are pattern recognition receptors involved in innate immunity (Rakoff-Nahoum and Medzhitov, 2009). Low-molecular weight hyaluronan induces the formation of a complex containing CD44, TLR2/TLR4, the actin filament-associated protein AFAP-110, and a myeloid differentiation factor MyD88, which triggers cytoskeleton activation and results in tumor invasion (Bourguignon et al., 2011).
Other Membrane and Cell Surface-Associated Proteins
Matricryptins form complexes with membrane or membrane-associated proteins. Caveolin- participates in the formation of membrane caveolae, which are platforms for signal transduction (Fridolfsson et al., 2014) and forms a complex with α5β1 integrin and endostatin in lipid rafts at the endothelial cell surface (Wickström et al., 2002) (Table 1). Nucleolin, a multifunctional protein, localized inside the cell and at the cell surface (Berger et al., 2015), binds to endostatin and triggers its internalization in endothelial cells in association with the urokinase plasminogen activator receptor and the α5β1integrin (Shi et al., 2007; Song et al., 2012).
Matricryptins as Potential Drugs
Matricryptins are potential anti-cancer drugs, either alone, or in combination with other treatments, but their use in pre-clinical and clinical studies remains challenging. Indeed matricryptins may display opposite activities depending on the context. The anti-tumoral effect of endostatin is enhanced by silencing of the proteoglycan versican, which decreases the inflammatory and immunosuppressive changes triggered by anti-angiogenic therapy (Wang et al., 2015d). However, endostatin may induce the proliferation of carcinoma cells, whereas its effect on cancer invasion is modulated by the tumor microenvironment (Alahuhta et al., 2015). Endorepellin stimulates angiogenesis in a stroke model by increasing VEGF levels, and exerts a neuroprotective effect in this model via α5β1 integrin and VEGFR2 (Lee et al., 2011). In addition, endostatin exhibits a biphasic response curve both for its anti-angiogenic and anti-tumoral properties (Celik et al., 2005; Javaherian et al., 2011), which requires to test a large range of concentrations to determine the optimal dose for treatment. Another challenge is that matricryptins may themselves contain cryptic sequences displaying opposite activities as reported for the anti-angiogenic matricryptin endostatin, which contains an embedded pro-angiogenic sequence (Morbidelli et al., 2003). Different matricryptins regulate the same biological process in an opposite way as reported for the regulation of the angiogenic signaling in choroidal endothelial cells by hexastatin and elastokines (Gunda and Sudhakar, 2013), or distinct steps of a biological process as described for anastellin and endostatin (Neskey et al., 2008).
Matricryptins can be modified to extend the half-life, and their efficacy (Xu et al., 2007; Zheng, 2009; Ricard-Blum and Ballut, 2011; Ricard-Blum and Salza, 2014). Most of the examples detailed below concern endostatin, which is extensively studied and has been approved for the treatment of non-small-cell lung cancer in China (Biaoxue et al., 2012) under a recombinant form, Endostar, which contains an extra metal chelating sequence (MGGSHHHHH) at the N-terminus enhancing its solubility and stability (Jiang et al., 2009). PEGylation (Nie et al., 2006; Tong et al., 2010; Tan et al., 2012; Guo et al., 2014), and the fusion of endostatin to low molecular weight heparin or to the Fc region of an IgG enhance its half-life and its anti-angiogenic, or anti-tumoral activities (Lee et al., 2008; Jing et al., 2011; Ning et al., 2012; Tan et al., 2012; Li et al., 2015b).
Tumors may escape from anti-tumoral and anti-angiogenic matricryptins by upregulating factors, which stimulate angiogenesis (Fernando et al., 2008). The combination of matricryptins with inhibitors of pro-angiogenic pathways, chemotherapy, or radiotherapy enhance their therapeutic efficacy. Tumstatin has been fused to another endogenous inhibitor of angiogenesis, vasostatin (Gu et al., 2014) and to tumor necrosis factor α, which has anti-tumoral and anti-angiogenic properties, which results in a more effective fusion protein than tumstatin alone (Luo et al., 2006). Endostatin has been fused to the proapoptotic domain (BH3) of the BAX protein (Chura-Chambi et al., 2014), to tumor necrosis factor-related apoptosis-inducing ligand (Zheng et al., 2013) and one of its anti-angiogenic sequences to an heptapeptide inhibitor of MMPs (Qiu et al., 2013). Endostatin has also been fused to protein sequences targeting it to tumors and/or tumor vasculature such as humanized antibodies against tyrosine kinase-type receptor HER2 (Shin et al., 2011) or against tumor-associated glycoprotein 72 highly expressed in human tumor tissues (Lee et al., 2015), the RGD integrin-binding sequence (Jing et al., 2011), and a liver-targeting peptide (circumsporozoite protein CSP I-plus (Ma et al., 2014; Bao et al., 2015).
Several approaches improve the delivery of matricryptins to tumors and endothelial cells (Xu et al., 2007; Ricard-Blum and Ballut, 2011) such as conditionally replicating oncolytic adenoviral vector for arresten (Li et al., 2015a), naked plasmid electrotransfer in muscle for tumstatin overexpression (Thevenard et al., 2013), and the nonpathogenic and anaerobic bacterium, Bifidobacterium longum, which proliferates in the hypoxic zones within tumors for tumstatin expression (Wei et al., 2015). Endostatin has been delivered in polylactic acid nanoparticles (Hu and Zhang, 2010), in gold nanoshells, which are very efficient on lung cancer cells when associated with near-infrared thermal therapy (Luo et al., 2015) and into microbubbles in combination with ultrasonic radiation in a cancer model (Zhang et al., 2014). Dendrimers mimicking the surface structure of endostatin and loaded with anticancer drug, result in both angiogenesis inhibition by endostatin and death of cancer cells by the anticancer drug (Jain and Jain, 2014).
Clinical trials of endostatin mostly focus on solid tumors in association with cytotoxic drugs (https://clinicaltrials.gov/). These trials include phase I (Lin et al., 2007; Chen et al., 2014), II (Lu et al., 2015), and III trials (Wang et al., 2005). Although endostatin did not improve overall survival, progression-free survival, and objective response rate when combined with etoposide and carboplatin in patients with extensive-stage small-cell lung cancer phase II trial (Lu et al., 2015), it significantly improves the response rate and median time to tumor progression when combined with vinorelbine and cisplatin in advanced non-small cell lung cancer patients compared to chemotherapy alone (Wang et al., 2005). Promising results have been obtained with endostatin associated with paclitaxel and 5-fluorouracile in patients with refractory malignant ascites secondary to ovarian cancer (Zhao et al., 2014).
Concluding Remarks
Several matricryptins such as the propeptide of lysyl oxidase, which is a tumor suppressor (Min et al., 2007; Ozdener et al., 2015) and the netrin-like domain of procollagen C-proteinase enhancer-1, a new anti-angiogenic matricryptin (Salza et al., 2014), warrant further investigation in angiogenesis, and tumor models to decipher their mechanisms of action at the molecular and cellular levels. Matricryptins are useful for treating fibroproliferative disorders (Yamaguchi et al., 2012; Wan et al., 2013) and fundus oculi angiogenesis diseases (Zhang et al., 2015). The finding that a peptide derived from endostatin can be delivered orally in vivo and exerts anti-fibrotic activity (Nishimoto et al., 2015) paves the way for the development of new matricryptin drugs with oral bioavailability, which is a preferred administration route for long-term treatment. Matricryptins are also used as biomarkers in serum and in cerebrospinal fluid (Ricard-Blum and Vallet, 2015; Salza et al., 2015) and may serve as imaging agents when labeled with (99m)Tc as shown for endostatin (Leung, 2004) and tumstatin (He et al., 2015) and for tumstatin conjugated to iron oxide nanoparticles (Ho et al., 2012).
Author Contributions
SV drafted the Section Receptors and Co-receptors of Matricryptins and Table 1 and made the figure. SB made bibliographical searches for all the sections and wrote the manuscript.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Abbreviations
ECM, extracellular matrix; EGF, epidermal growth factor; ERK, extracellular signal-regulated kinase; FAK, focal adhesion kinase; HA, hyaluronan; MAPK, mitogen-associated protein kinase; MMP, matrix metalloproteinase; mTOR, mammalian target of rapamycin; RHAMM, receptor for hyaluronic acid-mediated motility; TLR, toll-like receptor; VEGF, vascular endothelial growth factor; VEGFR, vascular endothelial growth factor receptor.
References
Aggeli, A. S., Kitsiou, P. V., Tzinia, A. K., Boutaud, A., Hudson, B. G., and Tsilibary, E. C. (2009). Selective binding of integrins from different renal cell types to the NC1 domain of alpha3 and alpha1 chains of type IV collagen. J. Nephrol. 22, 130–136.
Aikio, M., Alahuhta, I., Nurmenniemi, S., Suojanen, J., Palovuori, R., Teppo, S., et al. (2012). Arresten, a collagen-derived angiogenesis inhibitor, suppresses invasion of squamous cell carcinoma. PLoS ONE 7:e51044. doi: 10.1371/journal.pone.0051044
Alahuhta, I., Aikio, M., Väyrynen, O., Nurmenniemi, S., Suojanen, J., Teppo, S., et al. (2015). Endostatin induces proliferation of oral carcinoma cells but its effect on invasion is modified by the tumor microenvironment. Exp. Cell Res. 336, 130–140. doi: 10.1016/j.yexcr.2015.06.012
Ambesi, A., Klein, R. M., Pumiglia, K. M., and McKeown-Longo, P. J. (2005). Anastellin, a fragment of the first type III repeat of fibronectin, inhibits extracellular signal-regulated kinase and causes G(1) arrest in human microvessel endothelial cells. Cancer Res. 65, 148–156.
Ambesi, A., and McKeown-Longo, P. J. (2009). Anastellin, the angiostatic fibronectin peptide, is a selective inhibitor of lysophospholipid signaling. Mol. Cancer Res. 7, 255–265. doi: 10.1158/1541-7786.MCR-08-0195
Ambesi, A., and McKeown-Longo, P. J. (2014). Conformational remodeling of the fibronectin matrix selectively regulates VEGF signaling. J. Cell Sci. 127, 3805–3816. doi: 10.1242/jcs.150458
Bao, D., Jin, X., Ma, Y., and Zhu, J. (2015). Comparison of the structure and biological activities of wild-type and mutant liver-targeting peptide modified recombinant human endostatin (rES-CSP) in human hepatocellular carcinoma HepG2 Cells. Protein Pept. Lett. 22, 470–479. doi: 10.2174/0929866522666150302125218
Barbouri, D., Afratis, N., Gialeli, C., Vynios, D. H., Theocharis, A. D., and Karamanos, N. K. (2014). Syndecans as modulators and potential pharmacological targets in cancer progression. Front. Oncol. 4:4. doi: 10.3389/fonc.2014.00004
Barczyk, M., Carracedo, S., and Gullberg, D. (2010). Integrins. Cell Tissue Res. 339, 269–280. doi: 10.1007/s00441-009-0834-6
Bayless, K. J., and Davis, G. E. (2001). Identification of dual alpha 4beta1 integrin binding sites within a 38 amino acid domain in the N-terminal thrombin fragment of human osteopontin. J. Biol. Chem. 276, 13483–13489. doi: 10.1074/jbc.M011392200
Bello, L., Lucini, V., Carrabba, G., Giussani, C., Machluf, M., Pluderi, M., et al. (2001). Simultaneous inhibition of glioma angiogenesis, cell proliferation, and invasion by a naturally occurring fragment of human metalloproteinase-2. Cancer Res. 61, 8730–8736.
Berger, C. M., Gaume, X., and Bouvet, P. (2015). The roles of nucleolin subcellular localization in cancer. Biochimie 113, 78–85. doi: 10.1016/j.biochi.2015.03.023
Biaoxue, R., Shuanying, Y., Wei, L., Wei, Z., and Zongjuan, M. (2012). Systematic review and meta-analysis of Endostar (rh-endostatin) combined with chemotherapy versus chemotherapy alone for treating advanced non-small cell lung cancer. World J. Surg. Oncol. 10:170. doi: 10.1186/1477-7819-10-170
Blanchevoye, C., Floquet, N., Scandolera, A., Baud, S., Maurice, P., Bocquet, O., et al. (2013). Interaction between the elastin peptide VGVAPG and human elastin binding protein. J. Biol. Chem. 288, 1317–1328. doi: 10.1074/jbc.M112.419929
Blood, C. H., and Zetter, B. R. (1993). Laminin regulates a tumor cell chemotaxis receptor through the laminin-binding integrin subunit alpha 6. Cancer Res. 53, 2661–2666.
Boosani, C. S., and Sudhakar, Y. A. (2011). Proteolytically derived endogenous angioinhibitors originating from the extracellular matrix. Pharm. Basel Switz. 4, 1551–1577. doi: 10.3390/ph4121551
Borza, C. M., Pozzi, A., Borza, D.-B., Pedchenko, V., Hellmark, T., Hudson, B. G., et al. (2006). Integrin alpha3beta1, a novel receptor for alpha3(IV) noncollagenous domain and a trans-dominant Inhibitor for integrin alphavbeta3. J. Biol. Chem. 281, 20932–20939. doi: 10.1074/jbc.M601147200
Bourguignon, L. Y. W., Wong, G., Earle, C. A., and Xia, W. (2011). Interaction of low molecular weight hyaluronan with CD44 and toll-like receptors promotes the actin filament-associated protein 110-actin binding and MyD88-NFκB signaling leading to proinflammatory cytokine/chemokine production and breast tumor invasion. Cytoskeleton (Hoboken) 68, 671–693. doi: 10.1002/cm.20544
Brassart-Pasco, S., Sénéchal, K., Thevenard, J., Ramont, L., Devy, J., Di Stefano, L., et al. (2012). Tetrastatin, the NC1 domain of the α4(IV) collagen chain: a novel potent anti-tumor matrikine. PLoS ONE 7:e29587. doi: 10.1371/journal.pone.0029587
Brooks, P. C., Silletti, S., von Schalscha, T. L., Friedlander, M., and Cheresh, D. A. (1998). Disruption of angiogenesis by PEX, a noncatalytic metalloproteinase fragment with integrin binding activity. Cell 92, 391–400. doi: 10.1016/S0092-8674(00)80931-9
Carulli, S., Beck, K., Dayan, G., Boulesteix, S., Lortat-Jacob, H., and Rousselle, P. (2012). Cell surface proteoglycans syndecan-1 and -4 bind overlapping but distinct sites in laminin α3 LG45 protein domain. J. Biol. Chem. 287, 12204–12216. doi: 10.1074/jbc.M111.300061
Celik, I., Sürücü, O., Dietz, C., Heymach, J. V., Force, J., Höschele, I., et al. (2005). Therapeutic efficacy of endostatin exhibits a biphasic dose-response curve. Cancer Res. 65, 11044–11050. doi: 10.1158/0008-5472.CAN-05-2617
Chen, Y., Du, Y., Li, P., Wu, F., Fu, Y., Li, Z., et al. (2014). Phase I trial of M2ES, a novel polyethylene glycosylated recombinant human endostatin, plus gemcitabine in advanced pancreatic cancer. Mol. Clin. Oncol. 2, 586–590. doi: 10.3892/mco.2014.271
Chura-Chambi, R. M., Bellini, M. H., Jacysyn, J. F., Andrade, L. N., Medina, L. P., Prieto-da-Silva, A. R. B., et al. (2014). Improving the therapeutic potential of endostatin by fusing it with the BAX BH3 death domain. Cell Death Dis. 5, e1371. doi: 10.1038/cddis.2014.309
Couchman, J. R., Gopal, S., Lim, H. C., Nørgaard, S., and Multhaupt, H. A. B. (2015). Syndecans: from peripheral coreceptors to mainstream regulators of cell behaviour. Int. J. Exp. Pathol. 96, 1–10. doi: 10.1111/iep.12112
Cyphert, J. M., Trempus, C. S., and Garantziotis, S. (2015). Size Matters: molecular weight specificity of hyaluronan effects in cell biology. Int. J. Cell Biol. 2015:563818. doi: 10.1155/2015/563818
Davis, G. E., Bayless, K. J., Davis, M. J., and Meininger, G. A. (2000). Regulation of tissue injury responses by the exposure of matricryptic sites within extracellular matrix molecules. Am. J. Pathol. 156, 1489–1498. doi: 10.1016/S0002-9440(10)65020-1
De Rossi, G., and Whiteford, J. R. (2014). Syndecans in angiogenesis and endothelial cell biology. Biochem. Soc. Trans. 42, 1643–1646. doi: 10.1042/BST20140232
Donet, M., Brassart-Pasco, S., Salesse, S., Maquart, F.-X., and Brassart, B. (2014). Elastin peptides regulate HT-1080 fibrosarcoma cell migration and invasion through an Hsp90-dependent mechanism. Br. J. Cancer 111, 139–148. doi: 10.1038/bjc.2014.239
Duca, L., Blanchevoye, C., Cantarelli, B., Ghoneim, C., Dedieu, S., Delacoux, F., et al. (2007). The elastin receptor complex transduces signals through the catalytic activity of its Neu-1 subunit. J. Biol. Chem. 282, 12484–12491. doi: 10.1074/jbc.M609505200
Duca, L., Lambert, E., Debret, R., Rothhut, B., Blanchevoye, C., Delacoux, F., et al. (2005). Elastin peptides activate extracellular signal-regulated kinase 1/2 via a Ras-independent mechanism requiring both p110gamma/Raf-1 and protein kinase A/B-Raf signaling in human skin fibroblasts. Mol. Pharmacol. 67, 1315–1324. doi: 10.1124/mol.104.002725
Ezhilarasan, R., Jadhav, U., Mohanam, I., Rao, J. S., Gujrati, M., and Mohanam, S. (2009). The hemopexin domain of MMP-9 inhibits angiogenesis and retards the growth of intracranial glioblastoma xenograft in nude mice. Int. J. Cancer 124, 306–315. doi: 10.1002/ijc.23951
Faye, C., Chautard, E., Olsen, B. R., and Ricard-Blum, S. (2009a). The first draft of the endostatin interaction network. J. Biol. Chem. 284, 22041–22047. doi: 10.1074/jbc.M109.002964
Faye, C., Moreau, C., Chautard, E., Jetne, R., Fukai, N., Ruggiero, F., et al. (2009b). Molecular interplay between endostatin, integrins, and heparan sulfate. J. Biol. Chem. 284, 22029–22040. doi: 10.1074/jbc.M109.002840
Fernando, N. T., Koch, M., Rothrock, C., Gollogly, L. K., D'Amore, P. A., Ryeom, S., et al. (2008). Tumor escape from endogenous, extracellular matrix-associated angiogenesis inhibitors by up-regulation of multiple proangiogenic factors. Clin. Cancer Res. 14, 1529–1539. doi: 10.1158/1078-0432.CCR-07-4126
Filmus, J., Capurro, M., and Rast, J. (2008). Glypicans. Genome Biol. 9:224. doi: 10.1186/gb-2008-9-5-224
Folkman, J. (1971). Tumor angiogenesis: therapeutic implications. N. Engl. J. Med. 285, 1182–1186. doi: 10.1056/NEJM197111182852108
Folkman, J. (2006). Tumor suppression by p53 is mediated in part by the antiangiogenic activity of endostatin and tumstatin. Sci. STKE 2006:pe35. doi: 10.1126/stke.3542006pe35
Fridolfsson, H. N., Roth, D. M., Insel, P. A., and Patel, H. H. (2014). Regulation of intracellular signaling and function by caveolin. FASEB J. 28, 3823–3831. doi: 10.1096/fj.14-252320
Gao, F., Yang, C. X., Mo, W., Liu, Y. W., and He, Y. Q. (2008). Hyaluronan oligosaccharides are potential stimulators to angiogenesis via RHAMM mediated signal pathway in wound healing. Clin. Investig. Med. 31, E106–E116.
Goyal, A., Pal, N., Concannon, M., Paul, M., Doran, M., Poluzzi, C., et al. (2011). Endorepellin, the angiostatic module of perlecan, interacts with both the α2β1 integrin and vascular endothelial growth factor receptor 2 (VEGFR2): a dual receptor antagonism. J. Biol. Chem. 286, 25947–25962. doi: 10.1074/jbc.M111.243626
Goyal, A., Poluzzi, C., Willis, C. D., Smythies, J., Shellard, A., Neill, T., et al. (2012). Endorepellin affects angiogenesis by antagonizing diverse vascular endothelial growth factor receptor 2 (VEGFR2)-evoked signaling pathways: transcriptional repression of hypoxia-inducible factor 1α and VEGFA and concurrent inhibition of nuclear factor of activated T cell 1 (NFAT1) activation. J. Biol. Chem. 287, 43543–43556. doi: 10.1074/jbc.M112.401786
Green, P. M., Ludbrook, S. B., Miller, D. D., Horgan, C. M., and Barry, S. T. (2001). Structural elements of the osteopontin SVVYGLR motif important for the interaction with alpha(4) integrins. FEBS Lett. 503, 75–79. doi: 10.1016/S0014-5793(01)02690-4
Grünewald, F. S., Prota, A. E., Giese, A., and Ballmer-Hofer, K. (2010). Structure-function analysis of VEGF receptor activation and the role of coreceptors in angiogenic signaling. Biochim. Biophys. Acta 1804, 567–580. doi: 10.1016/j.bbapap.2009.09.002
Gu, Q., Sun, C., Luo, J., Zhang, T., and Wang, L. (2014). Inhibition of angiogenesis by a synthetic fusion protein VTF derived from vasostatin and tumstatin. Anticancer. Drugs 25, 1044–1051. doi: 10.1097/CAD.0000000000000134
Gunda, V., and Sudhakar, Y. A. (2013). Regulation of tumor angiogenesis and choroidal neovascularization by endogenous angioinhibitors. J. Cancer Sci. Ther. 5, 417–426. doi: 10.4172/1948-5956.1000235
Guo, L., Geng, X., Chen, Y., Qi, F., Liu, L., Miao, Y., et al. (2014). Pre-clinical toxicokinetics and safety study of M2ES, a PEGylated recombinant human endostatin, in rhesus monkeys. Regul. Toxicol. Pharmacol. 69, 512–523. doi: 10.1016/j.yrtph.2014.05.019
Guo, L., Song, N., He, T., Qi, F., Zheng, S., Xu, X.-G., et al. (2015). Endostatin inhibits the tumorigenesis of hemangioendothelioma via downregulation of CXCL1. Mol. Carcinog. 54, 1340–1353. doi: 10.1002/mc.22210
Hahn, C. S., Scott, D. W., Xu, X., Roda, M. A., Payne, G. A., Wells, J. M., et al. (2015). The matrikine N-α-PGP couples extracellular matrix fragmentation to endothelial permeability. Sci. Adv. 1:e1500175. doi: 10.1126/sciadv.1500175
Han, K.-Y., Azar, D. T., Sabri, A., Lee, H., Jain, S., Lee, B.-S., et al. (2012). Characterization of the interaction between endostatin short peptide and VEGF receptor 3. Protein Pept. Lett. 19, 969–974. doi: 10.2174/092986612802084465
Han, K.-Y., Chang, M., Ying, H.-Y., Lee, H., Huang, Y.-H., Chang, J.-H., et al. (2015). Selective binding of endostatin peptide 4 to recombinant VEGF receptor 3 in vitro. Protein Pept. Lett. 22, 1025–1030. doi: 10.2174/0929866522666150907111953
Hanai, J., Dhanabal, M., Karumanchi, S. A., Albanese, C., Waterman, M., Chan, B., et al. (2002). Endostatin causes G1 arrest of endothelial cells through inhibition of cyclin D1. J. Biol. Chem. 277, 16464–16469. doi: 10.1074/jbc.M112274200
Hayashi, S., Wang, Z., Bryan, J., Kobayashi, C., Faccio, R., and Sandell, L. J. (2011). The type II collagen N-propeptide, PIIBNP, inhibits cell survival and bone resorption of osteoclasts via integrin-mediated signaling. Bone 49, 644–652. doi: 10.1016/j.bone.2011.06.011
He, X., Hao, Y., Long, W., Song, N., Fan, S., and Meng, A. (2015). Exploration of peptide T7 and its derivative as integrin αvβ3-targeted imaging agents. OncoTargets Ther. 8, 1483–1491. doi: 10.2147/OTT.S82095
He, Y., Jiang, Y., Li, Y.-J., Liu, X.-H., Zhang, L., Liu, L.-J., et al. (2010). 19-peptide, a fragment of tumstatin, inhibits the growth of poorly differentiated gastric carcinoma cells in vitro and in vivo. J. Gastroenterol. Hepatol. 25, 935–941. doi: 10.1111/j.1440-1746.2009.06209.x
Heinz, A., Jung, M. C., Duca, L., Sippl, W., Taddese, S., Ihling, C., et al. (2010). Degradation of tropoelastin by matrix metalloproteinases–cleavage site specificities and release of matrikines. FEBS J. 277, 1939–1956. doi: 10.1111/j.1742-4658.2010.07616.x
Ho, D. N., Kohler, N., Sigdel, A., Kalluri, R., Morgan, J. R., Xu, C., et al. (2012). Penetration of endothelial cell coated multicellular tumor spheroids by iron oxide nanoparticles. Theranostics 2, 66–75. doi: 10.7150/thno.3568
Hu, S., and Zhang, Y. (2010). Endostar-loaded PEG-PLGA nanoparticles: in vitro and in vivo evaluation. Int. J. Nanomed. 5, 1039–1048. doi: 10.2147/IJN.S14753
Huang, D., Lan, H., Liu, F., Wang, S., Chen, X., Jin, K., et al. (2015). Anti-angiogenesis or pro-angiogenesis for cancer treatment: focus on drug distribution. Int. J. Clin. Exp. Med. 8, 8369–8376.
Humphries, J. D., Paul, N. R., Humphries, M. J., and Morgan, M. R. (2015). Emerging properties of adhesion complexes: what are they and what do they do? Trends Cell Biol. 25, 388–397. doi: 10.1016/j.tcb.2015.02.008
Iozzo, R. V., and Schaefer, L. (2015). Proteoglycan form and function: A comprehensive nomenclature of proteoglycans. Matrix Biol. J. 42, 11–55. doi: 10.1016/j.matbio.2015.02.003
Jain, K., and Jain, N. K. (2014). Surface engineered dendrimers as antiangiogenic agent and carrier for anticancer drug: dual attack on cancer. J. Nanosci. Nanotechnol. 14, 5075–5087. doi: 10.1166/jnn.2014.8677
Jain, R. K. (2005). Normalization of tumor vasculature: an emerging concept in antiangiogenic therapy. Science 307, 58–62. doi: 10.1126/science.1104819
Javaherian, K., Lee, T.-Y., Tjin Tham Sjin, R. M., Parris, G. E., and Hlatky, L. (2011). Two Endogenous antiangiogenic inhibitors, endostatin and angiostatin, demonstrate biphasic curves in their antitumor profiles. Dose Response. 9, 369–376. doi: 10.2203/dose-response.10-020.Javaherian
Jiang, L.-P., Zou, C., Yuan, X., Luo, W., Wen, Y., and Chen, Y. (2009). N-terminal modification increases the stability of the recombinant human endostatin in vitro. Biotechnol. Appl. Biochem. 54, 113–120. doi: 10.1042/BA20090063
Jing, Y., Lu, H., Wu, K., Subramanian, I. V., and Ramakrishnan, S. (2011). Inhibition of ovarian cancer by RGD-P125A-endostatin-Fc fusion proteins. Int. J. Cancer 129, 751–761. doi: 10.1002/ijc.25932
Jordan, A. R., Racine, R. R., Hennig, M. J. P., and Lokeshwar, V. B. (2015). The Role of CD44 in Disease Pathophysiology and Targeted Treatment. Front. Immunol. 6:182. doi: 10.3389/fimmu.2015.00182
Karumanchi, S. A., Jha, V., Ramchandran, R., Karihaloo, A., Tsiokas, L., Chan, B., et al. (2001). Cell surface glypicans are low-affinity endostatin receptors. Mol. Cell 7, 811–822. doi: 10.1016/S1097-2765(01)00225-8
Katagiri, Y. U., Sleeman, J., Fujii, H., Herrlich, P., Hotta, H., Tanaka, K., et al. (1999). CD44 variants but not CD44s cooperate with beta1-containing integrins to permit cells to bind to osteopontin independently of arginine-glycine-aspartic acid, thereby stimulating cell motility and chemotaxis. Cancer Res. 59, 219–226.
Kawaguchi, T., Yamashita, Y., Kanamori, M., Endersby, R., Bankiewicz, K. S., Baker, S. J., et al. (2006). The PTEN/Akt pathway dictates the direct alphaVbeta3-dependent growth-inhibitory action of an active fragment of tumstatin in glioma cells in vitro and in vivo. Cancer Res. 66, 11331–11340. doi: 10.1158/0008-5472.CAN-06-1540
Kikkawa, Y., Hozumi, K., Katagiri, F., Nomizu, M., Kleinman, H. K., and Koblinski, J. E. (2013). Laminin-111-derived peptides and cancer. Cell Adhes. Migr. 7, 150–256. doi: 10.4161/cam.22827
Kim, Y.-M., Hwang, S., Kim, Y.-M., Pyun, B.-J., Kim, T.-Y., Lee, S.-T., et al. (2002). Endostatin blocks vascular endothelial growth factor-mediated signaling via direct interaction with KDR/Flk-1. J. Biol. Chem. 277, 27872–27879. doi: 10.1074/jbc.M202771200
Lee, B., Clarke, D., Al Ahmad, A., Kahle, M., Parham, C., Auckland, L., et al. (2011). Perlecan domain V is neuroprotective and proangiogenic following ischemic stroke in rodents. J. Clin. Invest. 121, 3005–3023. doi: 10.1172/JCI46358
Lee, S.-H., Jeung, I. C., Park, T. W., Lee, K., Lee, D. G., Cho, Y.-L., et al. (2015). Extension of the in vivo half-life of endostatin and its improved anti-tumor activities upon fusion to a humanized antibody against tumor-associated glycoprotein 72 in a mouse model of human colorectal carcinoma. Oncotarget 6, 7182–7194. doi: 10.18632/oncotarget.3121
Lee, T.-Y., Tjin Tham Sjin, R. M., Movahedi, S., Ahmed, B., Pravda, E. A., Lo, K.-M., et al. (2008). Linking antibody Fc domain to endostatin significantly improves endostatin half-life and efficacy. Clin. Cancer Res. 14, 1487–1493. doi: 10.1158/1078-0432.CCR-07-1530
Lemmon, M. A., Schlessinger, J., and Ferguson, K. M. (2014). The EGFR family: not so prototypical receptor tyrosine kinases. Cold Spring Harb. Perspect. Biol. 6:a020768. doi: 10.1101/cshperspect.a020768
Leung, K. (2004). “(99m)Tc-Ethylenedicysteine-endostatin,” in Molecular Imaging and Contrast Agent Database (MICAD). (Bethesda, MD: National Center for Biotechnology Information (US)). Available online at: http://www.ncbi.nlm.nih.gov/books/NBK23681/ (Accessed November 16, 2015).
Li, S., Qi, Z., Li, H., Hu, J., Wang, D., Wang, X., et al. (2015a). Conditionally replicating oncolytic adenoviral vector expressing arresten and tumor necrosis factor-related apoptosis-inducing ligand experimentally suppresses lung carcinoma progression. Mol. Med. Rep. 12, 2068–2074. doi: 10.3892/mmr.2015.3624
Li, Z.-N., Yuan, Z.-F., Mu, G.-Y., Hu, M., Cao, L.-J., Zhang, Y.-L., et al. (2015b). Inhibitory effect of polysulfated heparin endostatin on alkali burn induced corneal neovascularization in rabbits. Int. J. Ophthalmol. 8, 234–238. doi: 10.3980/j.issn.2222-3959.2015.02.04
Lin, X., Huang, H., Li, S., Li, H., Li, Y., Cao, Y., et al. (2007). A phase I clinical trial of an adenovirus-mediated endostatin gene (E10A) in patients with solid tumors. Cancer Biol. Ther. 6, 648–653. doi: 10.4161/cbt.6.5.4004
Lu, S., Li, L., Luo, Y., Zhang, L., Wu, G., Chen, Z., et al. (2015). A multicenter, open-label, randomized phase II controlled study of rh-endostatin (Endostar) in combination with chemotherapy in previously untreated extensive-stage small-cell lung cancer. J. Thorac. Oncol. 10, 206–211. doi: 10.1097/JTO.0000000000000343
Lund, S. A., Giachelli, C. M., and Scatena, M. (2009). The role of osteopontin in inflammatory processes. J. Cell Commun. Signal. 3, 311–322. doi: 10.1007/s12079-009-0068-0
Luo, H., Xu, M., Zhu, X., Zhao, J., Man, S., and Zhang, H. (2015). Lung cancer cellular apoptosis induced by recombinant human endostatin gold nanoshell-mediated near-infrared thermal therapy. Int. J. Clin. Exp. Med. 8, 8758–8766.
Luo, Y.-Q., Wang, L.-H., Ma, X.-L., Kong, J.-X., and Jiao, B.-H. (2006). Construction, expression, and characterization of a new targeted bifunctional fusion protein: tumstatin45-132-TNF. IUBMB Life 58, 647–653. doi: 10.1080/15216540600981743
Ma, Y., Jin, X.-B., Chu, F.-J., Bao, D.-M., and Zhu, J.-Y. (2014). Expression of liver-targeting peptide modified recombinant human endostatin and preliminary study of its biological activities. Appl. Microbiol. Biotechnol. 98, 7923–7933. doi: 10.1007/s00253-014-5818-0
Maeda, I., Mizoiri, N., Briones, M. P. P., and Okamoto, K. (2007). Induction of macrophage migration through lactose-insensitive receptor by elastin-derived nonapeptides and their analog. J. Pept. Sci. 13, 263–268. doi: 10.1002/psc.845
Maeshima, Y., Colorado, P. C., and Kalluri, R. (2000). Two RGD-independent alpha vbeta 3 integrin binding sites on tumstatin regulate distinct anti-tumor properties. J. Biol. Chem. 275, 23745–23750. doi: 10.1074/jbc.C000186200
Maeshima, Y., Sudhakar, A., Lively, J. C., Ueki, K., Kharbanda, S., Kahn, C. R., et al. (2002). Tumstatin, an endothelial cell-specific inhibitor of protein synthesis. Science 295, 140–143. doi: 10.1126/science.1065298
Magnon, C., Galaup, A., Mullan, B., Rouffiac, V., Bouquet, C., Bidart, J.-M., et al. (2005). Canstatin acts on endothelial and tumor cells via mitochondrial damage initiated through interaction with alphavbeta3 and alphavbeta5 integrins. Cancer Res. 65, 4353–4361. doi: 10.1158/0008-5472.CAN-04-3536
Manon-Jensen, T., Itoh, Y., and Couchman, J. R. (2010). Proteoglycans in health and disease: the multiple roles of syndecan shedding. FEBS J. 277, 3876–3889. doi: 10.1111/j.1742-4658.2010.07798.x
Matou-Nasri, S., Gaffney, J., Kumar, S., and Slevin, M. (2009). Oligosaccharides of hyaluronan induce angiogenesis through distinct CD44 and RHAMM-mediated signalling pathways involving Cdc2 and gamma-adducin. Int. J. Oncol. 35, 761–773. doi: 10.3892/ijo_00000389
McDonell, L. M., Kernohan, K. D., Boycott, K. M., and Sawyer, S. L. (2015). Receptor tyrosine kinase mutations in developmental syndromes and cancer: two sides of the same coin. Hum. Mol. Genet. 24, R60–R66. doi: 10.1093/hmg/ddv254
Mercurius, K. O., and Morla, A. O. (2001). Cell adhesion and signaling on the fibronectin 1st type III repeat; requisite roles for cell surface proteoglycans and integrins. BMC Cell Biol. 2, 18. doi: 10.1186/1471-2121-2-18
Min, C., Kirsch, K. H., Zhao, Y., Jeay, S., Palamakumbura, A. H., Trackman, P. C., et al. (2007). The tumor suppressor activity of the lysyl oxidase propeptide reverses the invasive phenotype of Her-2/neu-driven breast cancer. Cancer Res. 67, 1105–1112. doi: 10.1158/0008-5472.CAN-06-3867
Misra, S., Hascall, V. C., Markwald, R. R., and Ghatak, S. (2015). Interactions between hyaluronan and its receptors (CD44, RHAMM) regulate the activities of inflammation and cancer. Front. Immunol. 6:201. doi: 10.3389/fimmu.2015.00201
Missan, D. S., and DiPersio, M. (2012). Integrin control of tumor invasion. Crit. Rev. Eukaryot. Gene Expr. 22, 309–324. doi: 10.1615/CritRevEukarGeneExpr.v22.i4.50
Monboisse, J. C., Oudart, J. B., Ramont, L., Brassart-Pasco, S., and Maquart, F. X. (2014). Matrikines from basement membrane collagens: a new anti-cancer strategy. Biochim. Biophys. Acta 1840, 2589–2598. doi: 10.1016/j.bbagen.2013.12.029
Monslow, J., Govindaraju, P., and Puré, E. (2015). Hyaluronan - a functional and structural sweet spot in the tissue microenvironment. Front. Immunol. 6:231. doi: 10.3389/fimmu.2015.00231
Morbidelli, L., Donnini, S., Chillemi, F., Giachetti, A., and Ziche, M. (2003). Angiosuppressive and angiostimulatory effects exerted by synthetic partial sequences of endostatin. Clin. Cancer Res. 9, 5358–5369.
Morgan, M. R., Humphries, M. J., and Bass, M. D. (2007). Synergistic control of cell adhesion by integrins and syndecans. Nat. Rev. Mol. Cell Biol. 8, 957–969. doi: 10.1038/nrm2289
Neskey, D. M., Ambesi, A., Pumiglia, K. M., and McKeown-Longo, P. J. (2008). Endostatin and anastellin inhibit distinct aspects of the angiogenic process. J. Exp. Clin. Cancer Res. 27:61. doi: 10.1186/1756-9966-27-61
Nguyen, T. M. B., Subramanian, I. V., Xiao, X., Ghosh, G., Nguyen, P., Kelekar, A., et al. (2009). Endostatin induces autophagy in endothelial cells by modulating Beclin 1 and beta-catenin levels. J. Cell. Mol. Med. 13, 3687–3698. doi: 10.1111/j.1582-4934.2009.00722.x
Nie, Y., Zhang, X., Wang, X., and Chen, J. (2006). Preparation and stability of N-terminal mono-PEGylated recombinant human endostatin. Bioconjug. Chem. 17, 995–999. doi: 10.1021/bc050355d
Nikitovic, D., Tzardi, M., Berdiaki, A., Tsatsakis, A., and Tzanakakis, G. N. (2015). Cancer microenvironment and inflammation: role of hyaluronan. Front. Immunol. 6:169. doi: 10.3389/fimmu.2015.00169
Ning, T., Jiang, M., Peng, Q., Yan, X., Lu, Z.-J., Peng, Y.-L., et al. (2012). Low-dose endostatin normalizes the structure and function of tumor vasculature and improves the delivery and anti-tumor efficacy of cytotoxic drugs in a lung cancer xenograft murine model. Thorac. Cancer 3, 229–238. doi: 10.1111/j.1759-7714.2012.00111.x
Nishimoto, T., Mlakar, L., Takihara, T., and Feghali-Bostwick, C. (2015). An endostatin-derived peptide orally exerts anti-fibrotic activity in a murine pulmonary fibrosis model. Int. Immunopharmacol. 28, 1102–1105. doi: 10.1016/j.intimp.2015.07.039
Nyström, A., Shaik, Z. P., Gullberg, D., Krieg, T., Eckes, B., Zent, R., et al. (2009). Role of tyrosine phosphatase SHP-1 in the mechanism of endorepellin angiostatic activity. Blood 114, 4897–4906. doi: 10.1182/blood-2009-02-207134
Ozdener, G. B., Bais, M. V., and Trackman, P. C. (2015). Determination of cell uptake pathways for tumor inhibitor lysyl oxidase propeptide. Mol. Oncol. 10, 1–23. doi: 10.1016/j.molonc.2015.07.005
Pasco, S., Monboisse, J. C., and Kieffer, N. (2000). The alpha 3(IV)185-206 peptide from noncollagenous domain 1 of type IV collagen interacts with a novel binding site on the beta 3 subunit of integrin alpha Vbeta 3 and stimulates focal adhesion kinase and phosphatidylinositol 3-kinase phosphorylation. J. Biol. Chem. 275, 32999–33007. doi: 10.1074/jbc.M005235200
Pedchenko, V., Zent, R., and Hudson, B. G. (2004). Alpha(v)beta3 and alpha(v)beta5 integrins bind both the proximal RGD site and non-RGD motifs within noncollagenous (NC1) domain of the alpha3 chain of type IV collagen: implication for the mechanism of endothelia cell adhesion. J. Biol. Chem. 279, 2772–2780. doi: 10.1074/jbc.M311901200
Petitclerc, E., Boutaud, A., Prestayko, A., Xu, J., Sado, Y., Ninomiya, Y., et al. (2000). New functions for non-collagenous domains of human collagen type IV. Novel integrin ligands inhibiting angiogenesis and tumor growth in vivo. J. Biol. Chem. 275, 8051–8061. doi: 10.1074/jbc.275.11.8051
Pocza, P., Süli-Vargha, H., Darvas, Z., and Falus, A. (2008). Locally generated VGVAPG and VAPG elastin-derived peptides amplify melanoma invasion via the galectin-3 receptor. Int. J. Cancer 122, 1972–1980. doi: 10.1002/ijc.23296
Poluzzi, C., Casulli, J., Goyal, A., Mercer, T. J., Neill, T., and Iozzo, R. V. (2014). Endorepellin evokes autophagy in endothelial cells. J. Biol. Chem. 289, 16114–16128. doi: 10.1074/jbc.M114.556530
Qiu, Z., Hu, J., Xu, H., Wang, W., Nie, C., and Wang, X. (2013). Generation of antitumor peptides by connection of matrix metalloproteinase-9 peptide inhibitor to an endostatin fragment. Anticancer Drugs 24, 677–689. doi: 10.1097/CAD.0b013e328361b7ad
Rakoff-Nahoum, S., and Medzhitov, R. (2009). Toll-like receptors and cancer. Nat. Rev. Cancer 9, 57–63. doi: 10.1038/nrc2541
Rehn, M., Veikkola, T., Kukk-Valdre, E., Nakamura, H., Ilmonen, M., Lombardo, C., et al. (2001). Interaction of endostatin with integrins implicated in angiogenesis. Proc. Natl. Acad. Sci. U.S.A. 98, 1024–1029. doi: 10.1073/pnas.98.3.1024
Ricard-Blum, S., and Ballut, L. (2011). Matricryptins derived from collagens and proteoglycans. Front. Biosci. (Landmark Ed.) 16, 674–697. doi: 10.2741/3712
Ricard-Blum, S., Féraud, O., Lortat-Jacob, H., Rencurosi, A., Fukai, N., Dkhissi, F., et al. (2004). Characterization of endostatin binding to heparin and heparan sulfate by surface plasmon resonance and molecular modeling: role of divalent cations. J. Biol. Chem. 279, 2927–2936. doi: 10.1074/jbc.M309868200
Ricard-Blum, S., and Salza, R. (2014). Matricryptins and matrikines: biologically active fragments of the extracellular matrix. Exp. Dermatol. 23, 457–463. doi: 10.1111/exd.12435
Ricard-Blum, S., and Vallet, S. D. (2015). Proteases decode the extracellular matrix cryptome. Biochimie. doi: 10.1016/j.biochi.2015.09.016. [Epub ahead of print].
Robinet, A., Fahem, A., Cauchard, J.-H., Huet, E., Vincent, L., Lorimier, S., et al. (2005). Elastin-derived peptides enhance angiogenesis by promoting endothelial cell migration and tubulogenesis through upregulation of MT1-MMP. J. Cell Sci. 118, 343–356. doi: 10.1242/jcs.01613
Roper, J. A., Williamson, R. C., and Bass, M. D. (2012). Syndecan and integrin interactomes: large complexes in small spaces. Curr. Opin. Struct. Biol. 22, 583–590. doi: 10.1016/j.sbi.2012.07.003
Rosca, E. V., Koskimaki, J. E., Rivera, C. G., Pandey, N. B., Tamiz, A. P., and Popel, A. S. (2011). Anti-angiogenic peptides for cancer therapeutics. Curr. Pharm. Biotechnol. 12, 1101–1116. doi: 10.2174/138920111796117300
Roskoski, R. (2008). VEGF receptor protein-tyrosine kinases: structure and regulation. Biochem. Biophys. Res. Commun. 375, 287–291. doi: 10.1016/j.bbrc.2008.07.121
Salza, R., Oudart, J.-B., Ramont, L., Maquart, F.-X., Bakchine, S., Thoannès, H., et al. (2015). Endostatin level in cerebrospinal fluid of patients with Alzheimer's disease. J. Alzheimers Dis. 44, 1253–1261. doi: 10.3233/JAD-142544
Salza, R., Peysselon, F., Chautard, E., Faye, C., Moschcovich, L., Weiss, T., et al. (2014). Extended interaction network of procollagen C-proteinase enhancer-1 in the extracellular matrix. Biochem. J. 457, 137–149. doi: 10.1042/BJ20130295
Schenk, S., Hintermann, E., Bilban, M., Koshikawa, N., Hojilla, C., Khokha, R., et al. (2003). Binding to EGF receptor of a laminin-5 EGF-like fragment liberated during MMP-dependent mammary gland involution. J. Cell Biol. 161, 197–209. doi: 10.1083/jcb.200208145
Shi, H., Huang, Y., Zhou, H., Song, X., Yuan, S., Fu, Y., et al. (2007). Nucleolin is a receptor that mediates antiangiogenic and antitumor activity of endostatin. Blood 110, 2899–2906. doi: 10.1182/blood-2007-01-064428
Shin, S.-U., Cho, H.-M., Merchan, J., Zhang, J., Kovacs, K., Jing, Y., et al. (2011). Targeted delivery of an antibody-mutant human endostatin fusion protein results in enhanced antitumor efficacy. Mol. Cancer Ther. 10, 603–614. doi: 10.1158/1535-7163.MCT-10-0804
Simons, M. (2012). An inside view: VEGF receptor trafficking and signaling. Physiology (Bethesda) 27, 213–222. doi: 10.1152/physiol.00016.2012
Soares, M. A., Teixeira, F. C. O. B., Fontes, M., Arêas, A. L., Leal, M. G., Pavão, M. S. G., et al. (2015). Heparan sulfate proteoglycans may promote or inhibit cancer progression by interacting with integrins and affecting cell migration. Biomed Res. Int. 2015:453801. doi: 10.1155/2015/453801
Song, N., Ding, Y., Zhuo, W., He, T., Fu, Z., Chen, Y., et al. (2012). The nuclear translocation of endostatin is mediated by its receptor nucleolin in endothelial cells. Angiogenesis 15, 697–711. doi: 10.1007/s10456-012-9284-y
Stadtmann, A., and Zarbock, A. (2012). CXCR2: from bench to bedside. Front. Immunol. 3:263. doi: 10.3389/fimmu.2012.00263
Su, J., Stenbjorn, R. S., Gorse, K., Su, K., Hauser, K. F., Ricard-Blum, S., et al. (2012). Target-derived matricryptins organize cerebellar synapse formation through α3β1 integrins. Cell Rep. 2, 223–230. doi: 10.1016/j.celrep.2012.07.001
Sudhakar, A., Nyberg, P., Keshamouni, V. G., Mannam, A. P., Li, J., Sugimoto, H., et al. (2005). Human alpha1 type IV collagen NC1 domain exhibits distinct antiangiogenic activity mediated by alpha1beta1 integrin. J. Clin. Invest. 115, 2801–2810. doi: 10.1172/JCI24813
Sudhakar, A., Sugimoto, H., Yang, C., Lively, J., Zeisberg, M., and Kalluri, R. (2003). Human tumstatin and human endostatin exhibit distinct antiangiogenic activities mediated by alpha v beta 3 and alpha 5 beta 1 integrins. Proc. Natl. Acad. Sci. U.S.A. 100, 4766–4771. doi: 10.1073/pnas.0730882100
Sund, M., Nyberg, P., and Eikesdal, H. P. (2010). Endogenous matrix-derived inhibitors of angiogenesis. Pharmaceuticals 3, 3021–3039. doi: 10.3390/ph3103021
Swindle, C. S., Tran, K. T., Johnson, T. D., Banerjee, P., Mayes, A. M., Griffith, L., et al. (2001). Epidermal growth factor (EGF)-like repeats of human tenascin-C as ligands for EGF receptor. J. Cell Biol. 154, 459–468. doi: 10.1083/jcb.200103103
Takafuji, V., Forgues, M., Unsworth, E., Goldsmith, P., and Wang, X. W. (2007). An osteopontin fragment is essential for tumor cell invasion in hepatocellular carcinoma. Oncogene 26, 6361–6371. doi: 10.1038/sj.onc.1210463
Tan, H., Yang, S., Liu, C., Cao, J., Mu, G., and Wang, F. (2012). Enhanced anti-angiogenesis and anti-tumor activity of endostatin by chemical modification with polyethylene glycol and low molecular weight heparin. Biomed. Pharmacother. 66, 648–654. doi: 10.1016/j.biopha.2011.04.007
Taylor, K. R., Trowbridge, J. M., Rudisill, J. A., Termeer, C. C., Simon, J. C., and Gallo, R. L. (2004). Hyaluronan fragments stimulate endothelial recognition of injury through TLR4. J. Biol. Chem. 279, 17079–17084. doi: 10.1074/jbc.M310859200
Teodoro, J. G., Parker, A. E., Zhu, X., and Green, M. R. (2006). p53-mediated inhibition of angiogenesis through up-regulation of a collagen prolyl hydroxylase. Science 313, 968–971. doi: 10.1126/science.1126391
Thevenard, J., Ramont, L., Mir, L. M., Dupont-Deshorgue, A., Maquart, F.-X., Monboisse, J.-C., et al. (2013). A new anti-tumor strategy based on in vivo tumstatin overexpression after plasmid electrotransfer in muscle. Biochem. Biophys. Res. Commun. 432, 549–552. doi: 10.1016/j.bbrc.2013.02.074
Tolg, C., McCarthy, J. B., Yazdani, A., and Turley, E. A. (2014). Hyaluronan and RHAMM in wound repair and the “cancerization” of stromal tissues. Biomed Res. Int. 2014:103923. doi: 10.1155/2014/103923
Tong, Y., Zhong, K., Tian, H., Gao, X., Xu, X., Yin, X., et al. (2010). Characterization of a monoPEG20000-Endostar. Int. J. Biol. Macromol. 46, 331–336. doi: 10.1016/j.ijbiomac.2010.01.017
Toole, B. P. (2009). Hyaluronan-CD44 interactions in cancer: paradoxes and possibilities. Clin. Cancer Res. 15, 7462–7468. doi: 10.1158/1078-0432.CCR-09-0479
Toupance, S., Brassart, B., Rabenoelina, F., Ghoneim, C., Vallar, L., Polette, M., et al. (2012). Elastin-derived peptides increase invasive capacities of lung cancer cells by post-transcriptional regulation of MMP-2 and uPA. Clin. Exp. Metastasis 29, 511–522. doi: 10.1007/s10585-012-9467-3
Tran, M., Rousselle, P., Nokelainen, P., Tallapragada, S., Nguyen, N. T., Fincher, E. F., et al. (2008). Targeting a tumor-specific laminin domain critical for human carcinogenesis. Cancer Res. 68, 2885–2894. doi: 10.1158/0008-5472.CAN-07-6160
Ugarte-Berzal, E., Bailón, E., Amigo-Jiménez, I., Albar, J. P., García-Marco, J. A., and García-Pardo, A. (2014). A novel CD44-binding peptide from the pro-matrix metalloproteinase-9 hemopexin domain impairs adhesion and migration of chronic lymphocytic leukemia (CLL) cells. J. Biol. Chem. 289, 15340–15349. doi: 10.1074/jbc.M114.559187
Ugarte-Berzal, E., Bailón, E., Amigo-Jiménez, I., Vituri, C. L., del Cerro, M. H., Terol, M. J., et al. (2012). A 17-residue sequence from the matrix metalloproteinase-9 (MMP-9) hemopexin domain binds α4β1 integrin and inhibits MMP-9-induced functions in chronic lymphocytic leukemia B cells. J. Biol. Chem. 287, 27601–27613. doi: 10.1074/jbc.M112.354670
Veenstra, M., and Ransohoff, R. M. (2012). Chemokine receptor CXCR2: physiology regulator and neuroinflammation controller? J. Neuroimmunol. 246, 1–9. doi: 10.1016/j.jneuroim.2012.02.016
Verma, R. K., Gunda, V., Pawar, S. C., and Sudhakar, Y. A. (2013). Extra cellular matrix derived metabolite regulates angiogenesis by FasL mediated apoptosis. PLoS ONE 8:e80555. doi: 10.1371/journal.pone.0080555
Walia, A., Yang, J. F., Huang, Y.-H., Rosenblatt, M. I., Chang, J.-H., and Azar, D. T. (2015). Endostatin's emerging roles in angiogenesis, lymphangiogenesis, disease, and clinical applications. Biochim. Biophys. Acta 1850, 2422–2438. doi: 10.1016/j.bbagen.2015.09.007
Wan, Y.-Y., Tian, G.-Y., Guo, H.-S., Kang, Y.-M., Yao, Z.-H., Li, X.-L., et al. (2013). Endostatin, an angiogenesis inhibitor, ameliorates bleomycin-induced pulmonary fibrosis in rats. Respir. Res. 14:56. doi: 10.1186/1465-9921-14-56
Wang, F., Dong, X., Xiu, P., Zhong, J., Wei, H., Xu, Z., et al. (2015a). T7 peptide inhibits angiogenesis via downregulation of angiopoietin-2 and autophagy. Oncol. Rep. 33, 675–684. doi: 10.3892/or.2014.3653
Wang, J., Sun, Y., Liu, Y., Yu, Q., Zhang, Y., Li, K., et al. (2005). Results of randomized, multicenter, double-blind phase III trial of rh-endostatin (YH-16) in treatment of advanced non-small cell lung cancer patients. J. Lung Cancer 8, 283–290. doi: 10.3779/j.issn.1009-3419.2005.04.07
Wang, S., Lu, X.-A., Liu, P., Fu, Y., Jia, L., Zhan, S., et al. (2015b). Endostatin has ATPase activity, which mediates its antiangiogenic and antitumor activities. Mol. Cancer Ther. 14, 1192–1201. doi: 10.1158/1535-7163.MCT-14-0836
Wang, W., Chen, P., Tang, M., Li, J., Pei, Y., Cai, S., et al. (2015c). Tumstatin 185-191 increases the sensitivity of non-small cell lung carcinoma cells to cisplatin by blocking proliferation, promoting apoptosis and inhibiting Akt activation. Am. J. Transl. Res. 7, 1332–1344.
Wang, Z., Bryan, J., Franz, C., Havlioglu, N., and Sandell, L. J. (2010). Type IIB procollagen NH(2)-propeptide induces death of tumor cells via interaction with integrins alpha(V)beta(3) and alpha(V)beta(5). J. Biol. Chem. 285, 20806–20817. doi: 10.1074/jbc.M110.118521
Wang, Z., Li, Z., Wang, Y., Cao, D., Wang, X., Jiang, M., et al. (2015d). Versican silencing improves the antitumor efficacy of endostatin by alleviating its induced inflammatory and immunosuppressive changes in the tumor microenvironment. Oncol. Rep. 33, 2981–2991. doi: 10.3892/or.2015.3903
Wei, C., Xun, A. Y., Wei, X. X., Yao, J., Wang, J. Y., Shi, R. Y., et al. (2015). Bifidobacteria expressing tumstatin protein for antitumor therapy in tumor-bearing mice. Technol. Cancer Res. Treat. doi: 10.1177/1533034615581977. [Epub ahead of print].
Wells, J. M., Gaggar, A., and Blalock, J. E. (2015). MMP generated matrikines. Matrix Biol. 44–46, 122–129. doi: 10.1016/j.matbio.2015.01.016
Welti, J., Loges, S., Dimmeler, S., and Carmeliet, P. (2013). Recent molecular discoveries in angiogenesis and antiangiogenic therapies in cancer. J. Clin. Invest. 123, 3190–3200. doi: 10.1172/JCI70212
Wen, Q.-L., Meng, M.-B., Yang, B., Tu, L.-L., Jia, L., Zhou, L., et al. (2009). Endostar, a recombined humanized endostatin, enhances the radioresponse for human nasopharyngeal carcinoma and human lung adenocarcinoma xenografts in mice. Cancer Sci. 100, 1510–1519. doi: 10.1111/j.1349-7006.2009.01193.x
Weston, S. A., Hulmes, D. J., Mould, A. P., Watson, R. B., and Humphries, M. J. (1994). Identification of integrin alpha 2 beta 1 as cell surface receptor for the carboxyl-terminal propeptide of type I procollagen. J. Biol. Chem. 269, 20982–20986.
Wickström, S. A., Alitalo, K., and Keski-Oja, J. (2002). Endostatin associates with integrin alpha5beta1 and caveolin-1, and activates Src via a tyrosyl phosphatase-dependent pathway in human endothelial cells. Cancer Res. 62, 5580–5589.
Wickström, S. A., Alitalo, K., and Keski-Oja, J. (2003). Endostatin associates with lipid rafts and induces reorganization of the actin cytoskeleton via down-regulation of RhoA activity. J. Biol. Chem. 278, 37895–37901. doi: 10.1074/jbc.M303569200
Willis, C. D., Poluzzi, C., Mongiat, M., and Iozzo, R. V. (2013). Endorepellin laminin-like globular 1/2 domains bind Ig3-5 of vascular endothelial growth factor (VEGF) receptor 2 and block pro-angiogenic signaling by VEGFA in endothelial cells. FEBS J. 280, 2271–2284. doi: 10.1111/febs.12164
Wu, G., Zhang, R., Ren, J., and Sun, Y. (2008). Autophagic cell death of human hepatoma cells induced by endostar, a recombinant human endostatin. Cancer Biother. Radiopharm. 23, 735–740. doi: 10.1089/cbr.2008.0518
Wu, M., Du, Y., Liu, Y., He, Y., Yang, C., Wang, W., et al. (2014). Low molecular weight hyaluronan induces lymphangiogenesis through LYVE-1-mediated signaling pathways. PLoS ONE 9:e92857. doi: 10.1371/journal.pone.0092857
Xiong, J., Balcioglu, H. E., and Danen, E. H. J. (2013). Integrin signaling in control of tumor growth and progression. Int. J. Biochem. Cell Biol. 45, 1012–1015. doi: 10.1016/j.biocel.2013.02.005
Xu, F., Ma, Q., and Sha, H. (2007). Optimizing drug delivery for enhancing therapeutic efficacy of recombinant human endostatin in cancer treatment. Crit. Rev. Ther. Drug Carrier Syst. 24, 445–492. doi: 10.1615/CritRevTherDrugCarrierSyst.v24.i5.20
Yamaguchi, Y., Takihara, T., Chambers, R. A., Veraldi, K. L., Larregina, A. T., and Feghali-Bostwick, C. A. (2012). A peptide derived from endostatin ameliorates organ fibrosis. Sci. Transl. Med. 4, 136ra71. doi: 10.1126/scitranslmed.3003421
Yang, C., Cao, M., Liu, H., He, Y., Xu, J., Du, Y., et al. (2012). The high and low molecular weight forms of hyaluronan have distinct effects on CD44 clustering. J. Biol. Chem. 287, 43094–43107. doi: 10.1074/jbc.M112.349209
Yokosaki, Y., Tanaka, K., Higashikawa, F., Yamashita, K., and Eboshida, A. (2005). Distinct structural requirements for binding of the integrins alphavbeta6, alphavbeta3, alphavbeta5, alpha5beta1 and alpha9beta1 to osteopontin. Matrix Biol. 24, 418–427. doi: 10.1016/j.matbio.2005.05.005
Zhang, X., Li, Y., Cheng, Y., Tan, H., Li, Z., Qu, Y., et al. (2015). Tat PTD-endostatin: a novel anti-angiogenesis protein with ocular barrier permeability via eye-drops. Biochim. Biophys. Acta 1850, 1140–1149. doi: 10.1016/j.bbagen.2015.01.019
Zhang, X., Yang, G., Zhang, Y., Huang, P., Qiu, J., Sun, Y., et al. (2014). An experimental research into endostatin microbubble combined with focused ultrasound for anti-tumor angiogenesis in colon cancer. Gastroenterol. Rep. 2, 44–53. doi: 10.1093/gastro/got038
Zhang, Y., Zhang, J., Jiang, D., Zhang, D., Qian, Z., Liu, C., et al. (2012). Inhibition of T-type Ca2+ channels by endostatin attenuates human glioblastoma cell proliferation and migration. Br. J. Pharmacol. 166, 1247–1260. doi: 10.1111/j.1476-5381.2012.01852.x
Zhao, J., Chen, X., Zhang, A., Xu, F., Hu, M., Xie, C., et al. (2014). A pilot study of combination intraperitoneal recombinant human endostatin and chemotherapy for refractory malignant ascites secondary to ovarian cancer. Med. Oncol. 31, 930. doi: 10.1007/s12032-014-0930-7
Zheng, M. (2009). Endostatin derivative angiogenesis inhibitors. Chin. Med. J. (Engl.) 122, 1947–1951. doi: 10.3760/cma.j.issn.0366-6999.2009.16.02
Zheng, Y., Chen, H., Zeng, X., Liu, Z., Xiao, X., Zhu, Y., et al. (2013). Surface modification of TPGS-b-(PCL-ran-PGA) nanoparticles with polyethyleneimine as a co-delivery system of TRAIL and endostatin for cervical cancer gene therapy. Nanoscale Res. Lett. 8:161. doi: 10.1186/1556-276X-8-161
Keywords: matricryptins, endostatin, matricellular receptors, interaction networks, anticancer drugs
Citation: Ricard-Blum S and Vallet SD (2016) Matricryptins Network with Matricellular Receptors at the Surface of Endothelial and Tumor Cells. Front. Pharmacol. 7:11. doi: 10.3389/fphar.2016.00011
Received: 20 November 2015; Accepted: 12 January 2016;
Published: 04 February 2016.
Edited by:
Hervé Emonard, Université de Reims Champagne-Ardenne, FranceReviewed by:
Jean Claude Monboisse, University of Reims Champagne-Ardenne, FranceMarie-Paule Jacob, Institut National de la Santé Et de la Recherche Médicale, France
Copyright © 2016 Ricard-Blum and Vallet. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sylvie Ricard-Blum, sylvie.ricard-blum@univ-lyon1.fr
 Sylvie Ricard-Blum
Sylvie Ricard-Blum Sylvain D. Vallet
Sylvain D. Vallet