- 1Clinical Psychology and Psychosomatics Service, University Hospital San Luigi Gonzaga, University of Turin, Orbassano, Italy
- 2Clinical and Biological Sciences Department, University Hospital San Luigi Gonzaga, University of Turin, Orbassano, Italy
- 3Neurologia 2 – Centro di Riferimento Regionale Sclerosi Multipla, Azienda Ospedaliero-Universitaria San Luigi Gonzaga, Orbassano, Italy
- 4eCampus University, Novedrate (CO), Italy
- 5Department of Mental Health, Azienda Sanitaria Locale Torino 3, Turin, Italy
- 6Facharzt für Psychosomatische und Innere Medizin, Eye Movement Desensitization and Reprocessing Institut Deutschland, Bergisch Gladbach, Germany
- 7Department of Psychology, University of Turin, Turin, Italy
Objective: Multiple Sclerosis (MS) is a demyelinating autoimmune disease that imposes a significant emotional burden with heavy psychosocial consequences. Several studies have investigated the association between MS and mental disorders such as depression and anxiety, and recently researchers have focused also on Post-traumatic Stress Disorder (PTSD). This is the first study that investigates the usefulness of proposing a treatment for PTSD to patients with MS.
Methods: A randomized controlled trial with patients with MS diagnosed with PTSD comparing Eye Movement Desensitization and Reprocessing (EMDR; n = 20) and Relaxation Therapy (RT; n = 22). The primary outcome measure was the proportion of participants that no longer meet PTSD diagnosis as measured with Clinician Administered PTSD Scale 6-months after the treatment.
Results: The majority of patients were able to overcome their PTSD diagnosis after only 10 therapy sessions. EMDR treatment appears to be more effective than RT in reducing the proportion of patients with MS suffering from PTSD. Both treatments are effective in reducing PTSD severity, anxiety and depression symptoms, and to improve Quality of Life.
Conclusion: Although our results can only be considered preliminary, this study suggests that it is essential that PTSD symptoms are detected and that brief and cost-effective interventions to reduce PTSD and associated psychological symptoms are offered to patients, in order to help them to reduce the psychological burden associated with their neurological condition.
Trial registration: NCT01743664, https://clinicaltrials.gov/ct2/show/NCT01743664
Introduction
Multiple Sclerosis (MS) is a demyelinating autoimmune disease of the central nervous system that affects both the brain and the spinal cord by destroying the myelin sheath that protects the nerve fibers, leaving plaques or scars on the damaged sites. MS typically onsets during young age, and thus it poses a significant emotional burden with heavy psychosocial consequences. The disease substantially interferes with daily activities and family, social and working life, disturbs emotional well-being, and reduces Quality of Life (QoL) (Janssens et al., 2003).
Several studies have focused on the association between MS and psychiatric illnesses, such as depression (Siegert and Abernethy, 2005; Wallin et al., 2006; Beiske et al., 2008; Feinstein, 2011; Moore et al., 2012) and anxiety (Zorzon et al., 2001; José Sá, 2008), but only recently have researchers focused on Post-traumatic Stress Disorder (PTSD) associated to MS.
Relation between stress and MS relapses is complex and reciprocal. An increasing amount of research (Mohr et al., 2004; Mohr, 2007; Mitsonis et al., 2009) points toward an association between stressful life events and relapse of MS, proposing that stress may enhance the risk of exacerbation (Nisipeanu and Korczyn, 1993; Brown et al., 2006). Moreover recent studies focusing on psychoneuroimmunology are gaining importance, proposing that stress may influence immune function via the autonomic nervous system and the hypothalamus-pituitary adrenal axis (Kern and Ziemssen, 2008; Karagkouni et al., 2013).
Since chronic and potentially life-threatening illness was explicitly included as a stressor that could precipitate PTSD in DSM-IV (American Psychiatric Association, 1994), it was therefore possible for individuals who suffer from MS to receive a PTSD diagnosis related to their illness. From then on there was a spread of empirical studies on Post-traumatic symptoms in patients with different medical illnesses (Smith et al., 1999; Kangas et al., 2002; Tedstone and Tarrier, 2003; Einsle et al., 2012). As pointed out by some studies (Tedstone and Tarrier, 2003; Jackson et al., 2007), despite the fact that experience of a serious medical illness can be undoubtedly stressful, some aspects of this experience differ from what is traditionally defined and widely studied as a trauma, such as serious car accidents, sexual assaults, earthquakes or exposures to combat. At the same time stressful experiences such as the communication of the diagnosis, the information provided on the prognosis, some debilitating treatments or disabling symptoms seem to be potential traumatic events such as those already considered in the PTSD literature (Tedstone and Tarrier, 2003). The existential threat due to a life-threatening illness may be more comparable to long-term trauma, such as that experienced in abusive relationships. As in those cases, the traumatic experience that promotes PTSD does not derive from a single event (Tedstone and Tarrier, 2003; Chalfant et al., 2004), but from the cumulative effect of these negative experiences (Turner and Lloyd, 1995; Alonzo, 2000).
To date, only three studies have evaluated the prevalence and the characteristics of PTSD secondary to MS (Chalfant et al., 2004; Counsell et al., 2013; Ostacoli et al., 2013). All these studies included different clinical types of MS (Relapsing-Remitting, Primary Progressive and Secondary Progressive). The first study evaluated a small sample of MS patients and found a relatively high prevalence of PTSD (n = 9/58, i.e., 15.5%), similar to that found in studies on cancer patients (Andrykowski and Cordova, 1998; Jacobsen et al., 1998). Counsell et al. (2013) conducted an Internet survey and found that almost 55.1% of their sample indicated that having MS was at least somewhat traumatic. Ostacoli et al. (2013) found a significant lower prevalence (12/232; 5.2%) than previous studies, probably due to different tools being used for PTSD diagnosis.
Moreover, none of these studies found an association between PTSD and clinical indices of MS, such as duration, severity, clinical type of MS and degree of disability, confirming that PTSD is more related to individual factors than to the precipitating event (Brewin et al., 2000).
Several studies have highlight that PTSD, if not treated, is long-lasting (Van Etten and Taylor, 1998; Andrykowski et al., 2000; Peris et al., 2011) and it may be a highly debilitating and impairing condition with also huge societal costs (Kessler, 2000; Galatzer-Levy et al., 2013; Tuerk et al., 2013).
Although there is extensive evidence on the effectiveness of treatments for PTSD, to date no study has been conducted to investigate the usefulness of proposing a treatment for this disorder to patients with MS. Effective treatments for PTSD include individual Trauma Focused CBT (TF-CBT), Eye Movement Desensitization and Reprocessing (EMDR), and stress management/relaxation training (Silver et al., 1995; Taylor et al., 2003; Bisson and Andrew, 2007; Tol et al., 2013), but clinical guidelines indicate that trauma-focused therapies, such as EMDR and TF-CBT are more effective than non trauma-focused intervention (National Collaborating Centre for Mental Health (UK), 2005).
Both EMDR and Relaxation Therapy (RT) were effectively used with patients suffering from other medical diseases such as chronic pain (Grant and Threlfo, 2002; Schneider et al., 2008; Chang et al., 2015), fibromyalgia (Friedberg, 2004; Theadom et al., 2015), myocardial infarction (Arabia et al., 2011; Whalley et al., 2014) and cancer (Yoo et al., 2005; Capezzani et al., 2013).
The main purpose of this study was to investigate the efficacy of EMDR in treating MS-related PTSD as compared to RT, in order to prove the role of EMDR as an elective intervention also in this specific population. Furthermore, as a secondary aim, we evaluated the efficacy of EMDR and RT on Post-traumatic Stress-associated symptoms (i.e., anxiety and depression), and on QoL and fatigue.
Lastly, we aimed to detect possible differences between these two treatments (EMDR vs. RT) at the follow-up evaluation for Post-traumatic Stress-associated symptoms and QoL.
Materials and Methods
This was a randomized controlled clinical trial where two active treatments (EMDR and RT) were compared with a restricted randomization in a 1:1 ratio, conducted in Italy. The trial registration number is NCT01743664.
Participants
Patients with MS were consecutively recruited from 2010 to 2013 from the Regional Reference Centre for Multiple Sclerosis (CReSM) affiliated with the University Hospital San Luigi Gonzaga of Orbassano, Turin, Italy. This study was approved by the Research Ethics Committee of the University Hospital San Luigi Gonzaga. Informed consent was obtained from all the participants.
Inclusion criteria were as follows: (1) definite diagnosis of a relapsing-remitting and primary or secondary progressive MS disease (McDonald Criteria) (Polman et al., 2011); (2) age between 18 and 65 years; (3) clinically inactive phase of the disease; (4) fluent Italian speaker; (5) legal capacity to consent to the treatment; (6) diagnosis of PTSD; (7) Post-traumatic symptoms present for at least 3 months; (8) willingness to suspend all concomitant psychological treatment; (9) suspension of all psychotropic medications at least 1 month before the treatment or maintenance at baseline level throughout the study.
Exclusion criteria were as follows: (1) presence of severe psychiatric disorders such as psychosis or bipolar disorder; (2) presence of severe medical conditions other than MS, such as diabetes, strokes or traumatic brain injuries; (3) drug or alcohol abuse; (4) suicide attempts; (5) overt dementia; (6) corticosteroid treatment during the previous 30 days.
Recruitment and Measures
Participants were recruited with a two-step screening: the Impact of Event Scale-Revised (IES-R) was administered to all patients corresponding to the neurological inclusion and exclusion criteria, specifying in the instructions that they consider only the illness as the traumatic event. The IES-R (Horowitz et al., 1979; Weiss and Marmar, 1997) is a 22- item self-report questionnaire consisting of three subscales (eight items relate to intrusions, eight items evaluate avoidance, and six items assess hyperarousal). The scale assesses subjective distress caused by traumatic events. A cut-off equal to or above 33, which is the cut-off most widely recognized in the literature (Creamer et al., 2003), is considered indicative of Post-traumatic stress symptoms.
Patients with scores equal to or above the cut-off of 33 were assessed with the PTSD module of Structured Clinical Interview for DSM-IV (SCID) (First, 1997) in order to confirm diagnosis of PTSD. Only PTSD primarily related to MS was considered. We also assessed the presence of previous trauma other than that related to MS, but they were not relevant to diagnose PTSD in this study.
Then patients with a confirmed diagnosis of PTSD were assessed with the Clinician-Administered PTSD Scale (CAPS) (Blake et al., 1995), a clinical semi-structured interview based on the DSM-IV-TR with B (intrusion), C (avoidance), and D (hyperarousal); to determine the presence of a symptom, we utilized the rule “1,2”: a frequency score of 1 (scale 0 = “none of the time” to 4 = “most or all of the time”) and an intensity score of 2 (scale 0 = “none” to 4 = “extreme”) is required for a particular symptom to meet criterion (Weathers et al., 2001). A severity score is calculated by adding together the frequency and intensity scores of subscales. Additional questions assess Criteria A, E, and F. CAPS is considered the gold standard in assessing PTSD (Foa and Tolin, 2000; Weathers et al., 2001).
The following psychological questionnaires were also administered:
- Hospital Anxiety and Depression Scale (HADS) was developed to identify caseness (possible and probable) of anxiety disorders and depression among patients in non-psychiatric hospital clinics. It is divided into an Anxiety subscale (HADS-A) and a Depression subscale (HADS-D) (Zigmond and Snaith, 1983; Bjelland et al., 2002). Each subscale contains seven items, which are evaluated by the patient on a four-point Likert scale (0–3), so that the possible scores range from 0 to 21 for both anxiety and depression. For each subscale, a result of 0–7 represents the normal condition; 8–10 identify mild cases; 11–15 moderate cases; and 16 or above indicates the presence of severe cases (Crawford et al., 2001; Quelhas and Costa, 2009). The tool has also been validated for use with patients with MS (Honarmand and Feinstein, 2009).
- Chicago Multiscale Depression Inventory (CMDI) is a 42-item, self-report questionnaire which was developed to assess depression in MS and other chronic diseases. The subscales assess mood (dysphoria), vegetative symptoms (physical malfunctioning) and evaluative symptoms (self-criticism). The mood subscale alone provides a more conservative indication of depression than total CMDI score (Solari et al., 2004).
- Functional Assessment of QoL in MS (FAMS) is a factorially derived self-report scale designed to assess six primary aspects of QOL of patients with MS: Mobility, Symptoms, Emotional Well-Being, General Contentment Thinking and Fatigue, and Family/Social Well- Being (Cella et al., 1996; Patti et al., 2007).
- Trauma Antecedent Questionnaire (TAQ) is a questionnaire to assess the trauma load due to previous traumas. The TAQ asks for the frequency (never, rarely, commonly) of experiences assigned to 11 domains (ranging from positive experiences such as competence and safety to negative experiences such as neglect, physical, emotional, sexual abuse, and witnessing trauma), separately assesses four developmental periods including early childhood (0–6), middle childhood, (7–12), adolescence (13–18), and adulthood (19+) (Garieballa et al., 2006).
- Fatigue Severity Scale (FSS) is a nine item one-dimensional questionnaire assessing the severity, frequency and impact of fatigue on daily life (Krupp et al., 1989). The cut-off of 36 is indicative of a severe fatigue (Flachenecker et al., 2002).
Lastly, patients received a score on the Expanded Disability Status Scale (EDSS) (Kurtzke, 1983, 2015) from their neurologist, to assess the level of disability.
Assessment Points and Randomization
The psychological assessments were administered at pre-intervention (T0), at post-intervention (T1) that was about 12–15 weeks later, and at follow-up (T2) 6 months after the end of the treatment. T2 was considered as the main assessment point throughout all the analyses. Assessments were independent and blind to treatment.
The research protocol was then proposed to patients with PTSD who met the inclusion/exclusion criteria, with an explanation of the aims of the study, its relevance for MS patients and the possibility that they may be included, by random assignment, in the treatment or control group for the period of the study, with the same timing and assessment tools. If they agreed, they signed the informed consent and they were randomized to the experimental group (EMDR) or to the control group (RT), using a block-wise randomization sequence (block size of 10). The sequence was determined by an independent statistical consultant using the “Random Number Generators” function in SPSS version 14.0.
Interventions
Treatments were independent and blinded to the clinical psychologists conducting the clinical assessments. All the participants, regardless of the type of treatment, received 10 individual 60-min-long treatment sessions conducted over 12–15 weeks, preceded by two sessions for history taking with particular attention to any stressful episodes in their life histories.
Eye Movement Desensitization and Reprocessing treatment was administered in accordance with Shapiro’s protocol for traumatic events (Shapiro, 2001). In the first session the patient is trained to stabilization techniques, such as the Safe Place. These imaginary exercises are used as a coping strategy to reduce distress, and the patient can also practice them at home as homework, or wherever and whenever they are needed. In the successive sessions the patient is induced to recall the traumatic images related to the illness, focusing on his/her worst negative thoughts, images or body sensations, thus provoking emotional disturbance, while the therapist uses external stimuli (usually eye movements, or tapping). Between each set of stimulation the patient reports thoughts, feelings or images that become the focus of the ongoing reprocessing. The residual distress becomes the focus of the next session of EMDR and the process continues until the distress evoked by the traumatic events, both past and future-oriented, is reduced, and negative cognitions are replaced by positive ones.
The three clinicians in the EMDR condition had more than 6 years’ experience in the liaison setting, working at the Clinical Psychology and Psychosomatics Service, Mental Health Department of the University Hospital San Luigi Gonzaga, with Level II EMDR training and a minimum of 3 years of experience in treating patients with PTSD. They received extensive training and supervision in the manualized protocol established for the study from a certified senior EMDR instructor.
Relaxation therapy included a series of relaxation techniques, including diaphragmatic breathing, progressive muscle relaxation, visualization, cue-controlled relaxation, and rapid relaxation (van Kessel et al., 2008). Relaxation treatment was performed by two psychotherapists working in the same facility of the EMDR intervention. The two clinicians in the Relaxation condition were at MSc level or higher, with a certified training in relaxation techniques and they had a minimum of 3 years’ experience treating patients with PTSD.
Statistical Analysis
Data were processed and analyzed using IBM SPSS (Statistical Package for Social Sciences) version 19.0.
Both parametric and non-parametric tests were used, in accordance with Shapiro–Wilk as a test for normality. Baseline group differences were assessed using Student’s t-test or Mann–Whitney U test to compare the two groups for continuous measures and Fisher’s Exact Test for categorical measures.
Fisher’s Exact Test was used to evaluate the association between the treatment group (EMDR vs. RT) and the PTSD diagnosis at T1 and at T2. Cramer’s V was used to calculate the effect size for the primary outcome (proportion of participants that no longer meet PTSD diagnosis as measured with CAPS at T2).
GLM repeated measures multivariate ANOVA (RM-MANOVA) was used to analyze the main pre- and post-intervention effects and interactions both between and within EMDR and RT groups. Pairwise comparison between groups were made by simple contrast and are reported as means difference with the Sidak correction 95% Confidence Interval (95%CI) for multiple comparisons.
An intention to treat analysis was not possible due to patients’ refusal of following evaluations.
All tests were two-sided and a p < 0.05 was considered statistically significant throughout all analyses.
Results
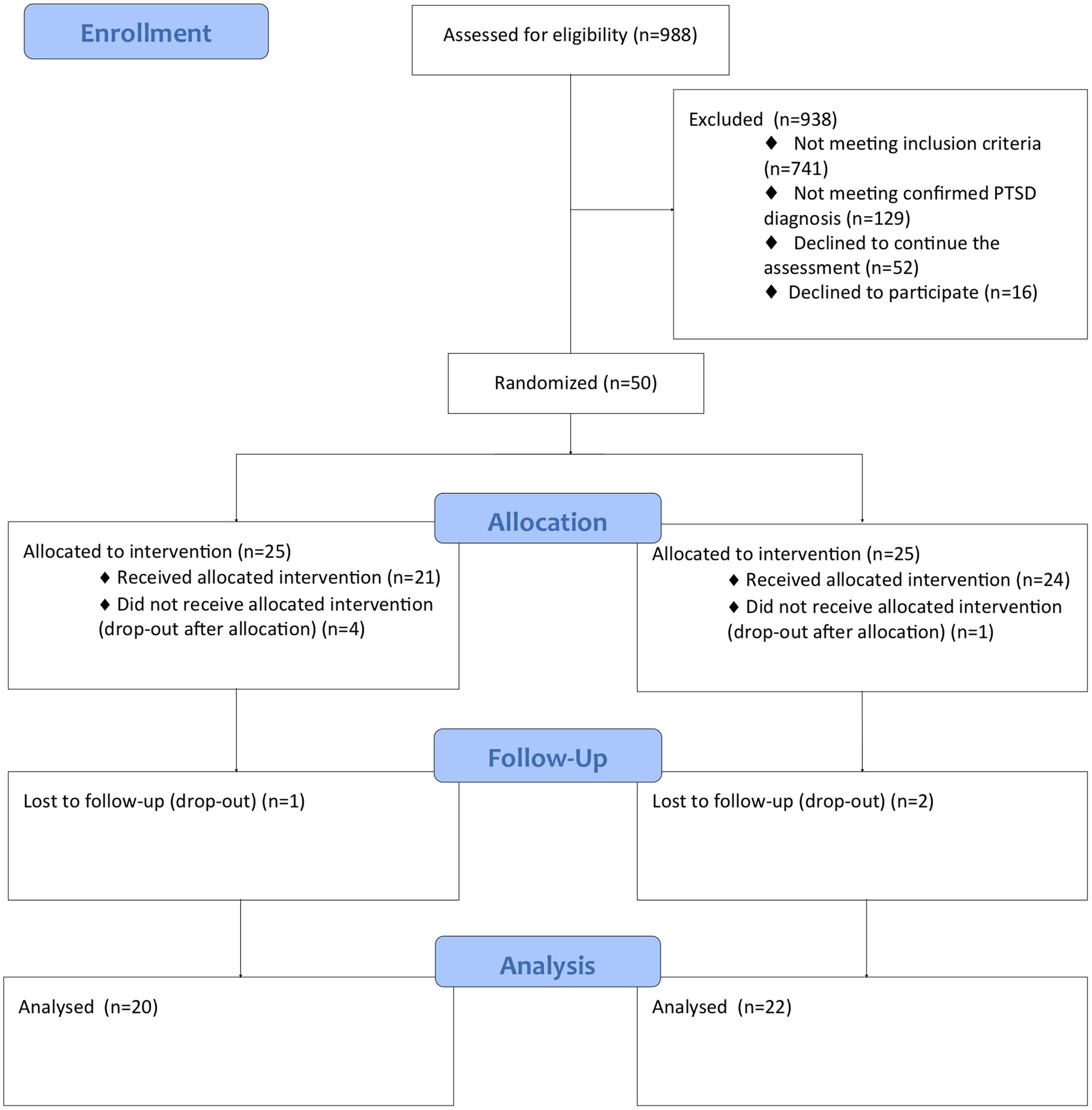
Figure 1 shows the flow diagram with number of participants at each assessment stage.
A total of 988 patients with MS were screened with the IES-R; only 247 of these patients presented IES-R score above the cut-off (25%). Fifty-two patients (5.3%) refused to continue the evaluation (refusal rate: 21.1%). Of the other 195 patients, 66 meet the criteria of PTSD diagnosis (6.7%). Fourteen patients refused to participate (the reasons were mainly the distance of the place of residence from the place of treatment and the inability to independently reach the place of treatment) and two patients were excluded because they had a bipolar disorder.
Fifty patients were randomized: 25 were assigned to the EMDR intervention and 25 were assigned to the RT intervention.
Five patients did not begin the treatment (four in the EMDR group and one in the RT group) and three patients (one in the EMDR group and two in the RT group) attended only the first two sessions. These patients refused to continue with the assessment at T1 and T2 and therefore it was not possible to include them in the statistical analysis. Therefore a total of 42 patients (20 in the EMDR group and 22 in the RT group) completed the treatment and were assessed at the post-intervention (T1 and T2).
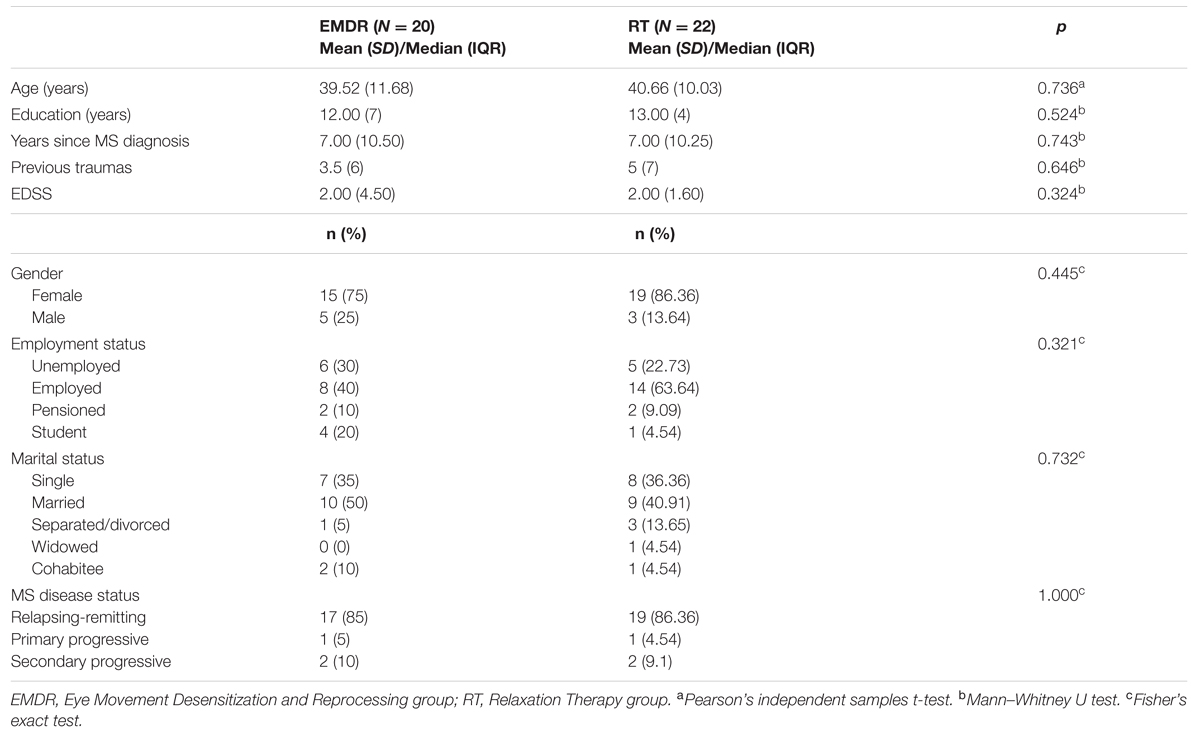
Table 1 presents socio-demographic characteristics of these patients at baseline. There were no significant differences in demographics and in clinical characteristics between the two groups at baseline (T0).
Firstly, we evaluated the proportion of patients that no longer meet PTSD diagnostic criteria at the end of the treatment (T1) and at follow-up assessment (T2). At T1 we found that 17 out of 20 patients in the EMDR group (85%) and 16 out of 22 patients (72.7%) in the RT group did not meet PTSD diagnosis criteria any longer. At T2, that is considered the primary outcome of our study, we found that all the patients in the EMDR group (20 out of 20, 100%) and 17 out of 22 patients (77.3%) in the RT group did not meet PTSD diagnosis criteria, with a statistically significant difference (χ2 = 5.160, p = 0.049; Cramer’s V = 0.350) in favor of EMDR.
Then we evaluated whether the different psychotherapy treatments (EMDR or RT) had a different impact on the psychological variables of interests. A Repeated-Measures MANOVA was performed on the pre- (T0) and post-intervention (T2) clinical scores (CAPS-Total, HADS-Anxiety, HADS-Depression, IES-R, FSS, CMDI-Mood, FAMS-Total), comparing group and time effects and interactions between group and time.
The RM-MANOVA yielded a significant pre-post main effect [F(7,34) = 45.244, p < 0.001; = 0.903], while no significant interaction was found between the pre-post measures and the treatment condition [F(7,34) = 0.631, p = 0.727; = 0.115]. Significant time effects were found across both groups on all variables, indicating that the mean participant scores improved from time 0 (pre-intervention) to time 1 (T2) in both groups without significant differences (Table 2).
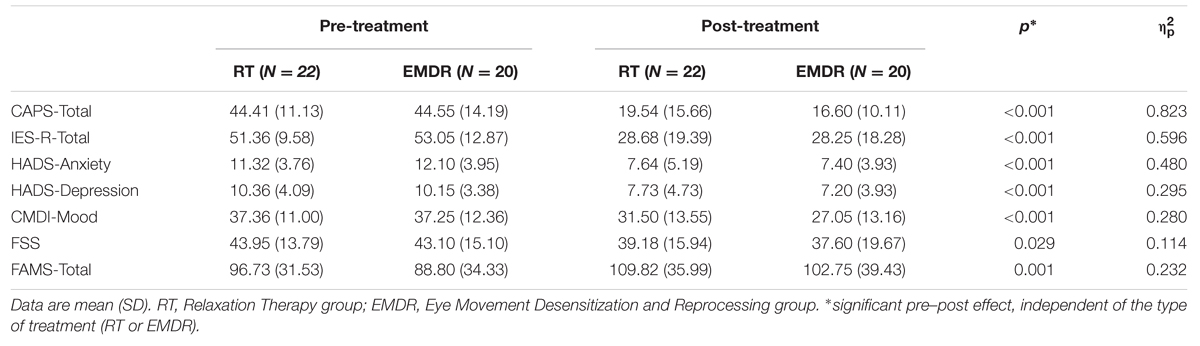
TABLE 2. Comparison of clinical variables between pre- (T0) and post-treatment (T2) for the two groups (EMDR and RT).
Discussion
The present study is the first that evaluates the efficacy of two different types of psychological treatment for PTSD in patients with MS.
The most significant result emerging from this study is that the majority of patients were able to overcome their PTSD diagnosis after only 10 therapy sessions.
As expected, EMDR treatment appears to be more effective than RT in reducing the proportion of patients with MS suffering from PTSD. This is in accordance with guidelines that indicate that trauma-focused therapies, such as EMDR and TF-CBT, are more effective than non-trauma focused intervention, also having a more stable effect (National Collaborating Centre for Mental Health (UK), 2005; Bisson and Andrew, 2007; Bisson et al., 2013).
Both treatments were able to significantly reduce levels of PTSD symptoms and PTSD severity, showing that a non-trauma focused intervention such as RT could be as efficacious as EMDR in this specific population. As this is the first study aiming to investigate this important issue, it is possible that our sample does not allow possible differences between the two treatments to be revealed; future studies are needed to confirm these results.
Furthermore, both treatments are effective in reducing anxiety and depression symptoms even in a limited number of sessions, with an effect that lasts at least 6 months after the end of the psychological treatment. Both treatments worked on emotional stabilization and containment and maybe these components, that are present in both EMDR and RT, are the effective elements causing an improvement of anxiety and depression secondary to MS.
In line with previous studies focusing on EMDR and RT efficacy on QoL and fatigue related to other physical illness such as cancer or fibromyalgia (Friedberg, 2004; Yoo et al., 2005; Capezzani et al., 2013; Theadom et al., 2015), our study also showed QoL and fatigue improving significantly after both treatments. This result suggests that treatments that focus on Post-traumatic symptoms could also be useful to target lifestyle components, which are of great importance for patients who have to deal with a chronic disabling disease such as MS.
The results of this study could be interpreted also taking into account the recent changes in DSM-5, which states that medical disease per se can no longer be considered as a stressor event to qualify for a criterion A for PTSD diagnosis (American Psychiatric Association, 2013). DSM-5 also states that Adjustment Disorders are common accompaniments of medical illness and may be the major psychological response to a medical disorder (American Psychiatric Association, 2013). According to Kangas (2013), the stress reaction to a medical disease can include not only symptoms closely associated with PTSD but also a number of other symptoms that can be better understood by other diagnostic categories such as Adjustment Disorder. In fact, in this specific population the traumatic components seem to be part of a more complex adaptation process to the illness and the assessment of stress response symptoms may be complicated by the multiplicity and indeterminate nature of the stressor events and by the confounding effect of symptoms related to the illness or treatment (Kwakkenbos et al., 2014). Consistent with Kangas (2013), the results of this study suggest that EMDR could be a promising effective treatment also for Adjustment Disorder with Post-traumatic symptoms, in addition to PTSD.
Moreover, the majority of patients in our study reported previous traumas (e.g., sexual abuse, physical and psychological violence, complicated bereavement). This finding is in line with the accumulated burden of adversity model (Alonzo, 2000), according to which MS-related traumatic experiences (e.g., communication of the diagnosis, disabling treatments, possible exacerbation and/or recurrence of disease, functional impairment, fear of being confined to a wheelchair), when added to previous adverse experiences in life, may act as a trigger for developing PTSD or other trauma- and stressor-related disorders. Future studies should keep in mind these considerations and try to adapt already available treatments to the complex psychological and medical condition of these patients.
This study has also some strengths. It is the first ever study to evaluate the efficacy of psychological interventions for PTSD and associated symptoms in patients with MS.
The present study has some limitations. The number of included patients treated with EMDR and RT is not large, despite the very large group of patients screened. Another limitation is that there was no placebo or waiting list group, in order to control for the effect of time. This limit has an ethical implication, taking into account that PTSD symptom resolution does not occur with the passage of time, as shown in studies with cancer patients (Gonçalves et al., 2011). Also, depression in MS is largely chronic (Koch et al., 2015); therefore it’s extremely likely that untreated PTSD related to MS would not improve without any treatment.
Although our results can only be considered preliminary, this study suggests that EMDR is more effective than RT in reducing the proportion of patients with MS suffering from PTSD. Both EMDR and RT are effective for reducing Post-traumatic Stress symptoms and associated symptoms, also within a limited number of sessions.
These encouraging results suggest that it is essential that PTSD symptoms are detected and that brief and cost-effective interventions to reduce PTSD and associated psychological symptoms are offered to patients, in order to help them to reduce the psychological burden associated with their neurological condition.
Author Contributions
LO, AZ, and AH were responsible for the conception and the design of the study. SC, MB, GB, FO, MC, and SM were responsible for data collection and analysis. SC wrote the article, which was critically revised by MB, GB, FO, MC, AH, AZ, SM, and LO. All authors read and approved the final version of the manuscript.
Funding
This work was supported by FISM—Fondazione Italiana Sclerosi Multipla [2009/R/11].
Conflict of Interest Statement
AH is the president of EMDR Germany Institute. The other authors declare that there is no conflict of interest.
Acknowledgments
We would like to thank the participants involved in the study for their time and effort. We are very grateful to Debora Boni, Massimo Castaldo, Luana Marnetto, Manuela Negro, and Clarisse Zaccarino for their contribution to this study. We want also to thank Roberto D’Amico for statistical suggestions.
References
Alonzo, A. A. (2000). The experience of chronic illness and post-traumatic stress disorder: the consequences ofcumulative adversity. Soc. Sci. Med. 198250, 1475–1484. doi: 10.1016/S0277-9536(99)00399-8
American Psychiatric Association (1994). Diagnostic and Statistical Manual of Mental Disorders, 4th Edn. Washington DC: American Psychiatric Pub.
American Psychiatric Association (2013). Diagnostic and Statistical Manual of Mental Disorders: DSM-5. Washington, DC: American Psychiatric Publishing, Inc.
Andrykowski, M. A., and Cordova, M. J. (1998). Factors associated with PTSD symptoms following treatment for breast cancer: test of the andersen model. J. Trauma. Stress 11, 189–203. doi: 10.1023/A:1024490718043
Andrykowski, M. A., Cordova, M. J., McGrath, P. C., Sloan, D. A., and Kenady, D. E. (2000). Stability and change in posttraumatic stress disorder symptoms following breast cancer treatment: a 1-year follow-up. Psychooncology 9, 69–78. doi: 10.1002/(SICI)1099-1611(200001/02)9:1<69::AID-PON439>3.3.CO;2-I
Arabia, E., Manca, M. L., and Solomon, R. M. (2011). EMDR for survivors of life-threatening cardiac events: results of a pilot study. J. EMDR Pract. Res. 5, 2–13. doi: 10.1891/1933-3196.5.1.2
Beiske, A. G., Svensson, E., Sandanger, I., Czujko, B., Pedersen, E. D., Aarseth, J. H., et al. (2008). Depression and anxiety amongst multiple sclerosis patients. Eur. J. Neurol. 15, 239–245. doi: 10.1111/j.1468-1331.2007.02041.x
Bisson, J., and Andrew, M. (2007). Psychological treatment of post-traumatic stress disorder (PTSD). Cochrane Database Syst. Rev. 18:CD003388. doi: 10.1002/14651858.CD003388.pub3
Bisson, J., Roberts, N. P., Andrew, M., Cooper, R., and Lewis, C. (2013). Psychological therapies for chronic post-traumatic stress disorder (PTSD) in adults. Cochrane Database Syst. Rev. 12:CD003388. doi: 10.1002/14651858.CD003388.pub4
Bjelland, I., Dahl, A. A., Haug, T. T., and Neckelmann, D. (2002). The validity of the hospital anxiety and depression scale. An updated literature review. J. Psychosom. Res. 52, 69–77. doi: 10.1016/S0022-3999(01)00296-3
Blake, D. D., Weathers, F. W., Nagy, L. M., Kaloupek, D. G., Gusman, F. D., Charney, D. S., et al. (1995). The development of a clinician-administered PTSD scale. J. Trauma. Stress 8, 75–90. doi: 10.1002/jts.2490080106
Brewin, C. R., Andrews, B., and Valentine, J. D. (2000). Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. J. Consult. Clin. Psychol. 68, 748–766. doi: 10.1037/0022-006X.68.5.748
Brown, R. F., Tennant, C. C., Sharrock, M., Hodgkinson, S., Dunn, S. M., and Pollard, J. D. (2006). Relationship between stress and relapse in multiple sclerosis: part II. Direct and indirect relationships. Mult. Scler. 12, 465–475. doi: 10.1191/1352458506ms1296oa
Capezzani, L., Ostacoli, L., Cavallo, M., Carletto, S., Fernandez, I., Solomon, R., et al. (2013). EMDR and CBT for cancer patients: comparative study of effects on PTSD, anxiety, and depression. J. EMDR Pract. Res. 7, 134–143. doi: 10.1891/1933-3196.7.3.134
Cella, D. F., Dineen, K., Arnason, B., Reder, A., Webster, K. A., Karabatsos, G., et al. (1996). Validation of the functional assessment of multiple sclerosis quality of life instrument. Neurology 47, 129–139. doi: 10.1212/WNL.47.1.129
Chalfant, A. M., Bryant, R. A., and Fulcher, G. (2004). Posttraumatic stress disorder following diagnosis of multiple sclerosis. J. Trauma. Stress 17, 423–428. doi: 10.1023/B:JOTS.0000048955.65891.4c
Chang, K.-L., Fillingim, R., Hurley, R. W., and Schmidt, S. (2015). Chronic pain management: nonpharmacological therapies for chronic pain. FP Essent. 432, 21–26.
Counsell, A., Hadjistavropoulos, H. D., Kehler, M. D., and Asmundson, G. J. G. (2013). Posttraumatic stress disorder symptoms in individuals with multiple sclerosis. Psychol. Trauma Theor. Res. Pract. Policy 5, 448–452. doi: 10.1037/a0029338
Crawford, J. R., Henry, J. D., Crombie, C., and Taylor, E. P. (2001). Normative data for the HADS from a large non-clinical sample. Br. J. Clin. Psychol. Br. Psychol. Soc. 40, 429–434. doi: 10.1348/014466501163904
Creamer, M., Bell, R., and Failla, S. (2003). Psychometric properties of the impact of event scale—revised. Behav. Res. Ther. 41, 1489–1496. doi: 10.1016/j.brat.2003.07.010
Einsle, F., Kraft, D., and Köllner, V. (2012). Post-traumatic stress disorder (PTSD) in cardiology and oncology–which diagnostic tools should be used? J. Psychosom. Res. 72, 434–438. doi: 10.1016/j.jpsychores.2012.02.008
Feinstein, A. (2011). Multiple sclerosis and depression. Mult. Scler. 17, 1276–1281. doi: 10.1177/1352458511417835
First, M. B. (1997). User’s Guide for the Structured Clinical Interview for DSM-IV axis I Disorders SCID-I: Clinician Version. Washington, DC: American Psychiatric Press.
Flachenecker, P., Kümpfel, T., Kallmann, B., Gottschalk, M., Grauer, O., Rieckmann, P., et al. (2002). Fatigue in multiple sclerosis: a comparison of different rating scales and correlation to clinical parameters. Mult. Scler. 8, 523–526. doi: 10.1191/1352458502ms839oa
Foa, E. B., and Tolin, D. F. (2000). Comparison of the PTSD symptom scale-interview version and the clinician-administered PTSD scale. J. Trauma. Stress 13, 181–191. doi: 10.1023/A:1007781909213
Friedberg, F. (2004). Eye movement desensitization in fibromyalgia: apilot study. Complement. Ther. Nurs. Midwifery 10, 245–249. doi: 10.1016/j.ctnm.2004.06.006
Galatzer-Levy, I. R., Ankri, Y., Freedman, S., Israeli-Shalev, Y., Roitman, P., Gilad, M., et al. (2013). Early PTSD symptom trajectories: persistence, recovery, and response to treatment: results from the jerusalem trauma outreach and prevention study (J-TOPS). PLoS ONE 8:e70084. doi: 10.1371/journal.pone.0070084
Garieballa, S. S., Schauer, M., Neuner, F., Saleptsi, E., Kluttig, T., Elbert, T., et al. (2006). Traumatic events, PTSD, and psychiatric comorbidity in forensic patients–assessed by questionnaires and diagnostic interview. Clin. Pract. Epidemiol. Ment. Health 2:7. doi: 10.1186/1745-0179-2-7
Gonçalves, V., Jayson, G., and Tarrier, N. (2011). A longitudinal investigation of posttraumatic stress disorder in patients with ovarian cancer. J. Psychosom. Res. 70, 422–431. doi: 10.1016/j.jpsychores.2010.09.017
Grant, M., and Threlfo, C. (2002). EMDR in the treatment of chronic pain. J. Clin. Psychol. 58, 1505–1520. doi: 10.1002/jclp.10101
Honarmand, K., and Feinstein, A. (2009). Validation of the hospital anxiety and depression scale for use with multiple sclerosis patients. Mult. Scler. 15, 1518–1524. doi: 10.1177/1352458509347150
Horowitz, M., Wilner, N., and Alvarez, W. (1979). Impact of event scale: a measure of subjective stress. Psychosom. Med. 41, 209–218. doi: 10.1097/00006842-197905000-00004
Jackson, J. C., Hart, R. P., Gordon, S. M., Hopkins, R. O., Girard, T. D., and Ely, E. W. (2007). Post-traumatic stress disorder and post-traumatic stress symptoms following critical illness in medical intensive care unit patients: assessing the magnitude of the problem. Crit. Care 11:R27. doi: 10.1186/cc5707
Jacobsen, P. B., Widows, M. R., Hann, D. M., Andrykowski, M. A., Kronish, L. E., and Fields, K. K. (1998). Posttraumatic stress disorder symptoms after bone marrow transplantation for breast cancer. Psychosom. Med. 60, 366–371. doi: 10.1097/00006842-199805000-00026
Janssens, A. C. J. W., van Doorn, P. A., de Boer, J. B., van der Meché, F. G. A., Passchier, J., and Hintzen, R. Q. (2003). Impact of recently diagnosed multiple sclerosis on quality of life, anxiety, depression and distress of patients and partners. Acta Neurol. Scand. 108, 389–395. doi: 10.1034/j.1600-0404.2003.00166.x
José Sá, M. (2008). Psychological aspects of multiple sclerosis. Clin. Neurol. Neurosurg. 110, 868–877. doi: 10.1016/j.clineuro.2007.10.001
Kangas, M. (2013). DSM-5 trauma and stress-related disorders: implications for screening for cancer-related stress. Front. Psychiatry 4:122. doi: 10.3389/fpsyt.2013.00122
Kangas, M., Henry, J. L., and Bryant, R. A. (2002). Posttraumatic stress disorder following cancer. Clin. Psychol. Rev. 22, 499–524. doi: 10.1016/S0272-7358(01)00118-0
Karagkouni, A., Alevizos, M., and Theoharides, T. C. (2013). Effect of stress on brain inflammation and multiple sclerosis. Autoimmun. Rev. 12, 947–953. doi: 10.1016/j.autrev.2013.02.006
Kern, S., and Ziemssen, T. (2008). Brain-immune communication psychoneuroimmunology of multiple sclerosis. Mult. Scler. 14, 6–21. doi: 10.1177/1352458507079657
Kessler, R. C. (2000). Posttraumatic stress disorder: the burden to the individual and to society. J. Clin. Psychiatry 61(Suppl. 5), 4–12, discussion 13–14.
Koch, M. W., Patten, S., Berzins, S., Zhornitsky, S., Greenfield, J., Wall, W., et al. (2015). Depression in multiple sclerosis: along-term longitudinal study. Mult. Scler. 21, 76–82. doi: 10.1177/1352458514536086
Krupp, L. B., LaRocca, N. G., Muir-Nash, J., and Steinberg, A. D. (1989). The fatigue severity scale. Application to patients with multiple sclerosis and systemic lupus erythematosus. Arch. Neurol. 46, 1121–1123. doi: 10.1001/archneur.1989.00520460115022
Kurtzke, J. F. (1983). Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS). Neurology 33, 1444–1452. doi: 10.1212/WNL.33.11.1444
Kurtzke, J. F. (2015). On the origin of EDSS. Mult. Scler. Relat. Disord. 4, 95–103. doi: 10.1016/j.msard.2015.02.003
Kwakkenbos, L., Coyne, J. C., and Thombs, B. D. (2014). Prevalence of posttraumatic stress disorder (PTSD) in women with breast cancer. J. Psychosom. Res. 76, 485–486. doi: 10.1016/j.jpsychores.2014.03.103
Mitsonis, C. I., Potagas, C., Zervas, I., and Sfagos, K. (2009). The effects of stressful life events on the course of multiple sclerosis: areview. Int. J. Neurosci. 119, 315–335. doi: 10.1080/00207450802480192
Mohr, D. C. (2007). Stress and multiple sclerosis. J. Neurol. 254(Suppl. 2), II65–II68. doi: 10.1007/s00415-007-2015-4
Mohr, D. C., Hart, S. L., Julian, L., Cox, D., and Pelletier, D. (2004). Association between stressful life events and exacerbation in multiple sclerosis: ameta-analysis. BMJ 328:731. doi: 10.1136/bmj.38041.724421.55
Moore, P., Hirst, C., Harding, K. E., Clarkson, H., Pickersgill, T. P., and Robertson, N. P. (2012). Multiple sclerosis relapses and depression. J. Psychosom. Res. 73, 272–276. doi: 10.1016/j.jpsychores.2012.08.004
National Collaborating Centre for Mental Health (UK) (2005). Post-Traumatic Stress Disorder: The Management of PTSD in Adults and Children in Primary and Secondary Care. Leicester: Gaskell Available at: http://www.ncbi.nlm.nih.gov/books/NBK56494/ [accessed June 24, 2015].
Nisipeanu, P., and Korczyn, A. D. (1993). Psychological stress as risk factor for exacerbations in multiple sclerosis. Neurology 43, 1311–1312. doi: 10.1212/WNL.43.7.1311
Ostacoli, L., Carletto, S., Borghi, M., Cavallo, M., Rocci, E., Zuffranieri, M., et al. (2013). Prevalence and significant determinants of post-traumatic stress disorder in a large sample of patients with multiple sclerosis. J. Clin. Psychol. Med. Settings 20, 240–246. doi: 10.1007/s10880-012-9323-2
Patti, F., Russo, P., Pappalardo, A., Macchia, F., Civalleri, L., Paolillo, A., et al. (2007). Predictors of quality of life among patients with multiple sclerosis: an Italian cross-sectional study. J. Neurol. Sci. 252, 121–129. doi: 10.1016/j.jns.2006.10.017
Peris, A., Bonizzoli, M., Iozzelli, D., Migliaccio, M. L., Zagli, G., Bacchereti, A., et al. (2011). Early intra-intensive care unit psychological intervention promotes recovery from post traumaticstress disorders, anxiety and depression symptoms in critically ill patients. Crit. Care Lond. Engl. 15, R41. doi: 10.1186/cc10003
Polman, C. H., Reingold, S. C., Banwell, B., Clanet, M., Cohen, J. A., Filippi, M., et al. (2011). Diagnostic criteria for multiple sclerosis: 2010 revisions to the McDonald criteria. Ann. Neurol. 69, 292–302. doi: 10.1002/ana.22366
Quelhas, R., and Costa, M. (2009). Anxiety, depression, and quality of life in Parkinson’s disease. J. Neuropsychiatry Clin. Neurosci. 21, 413–419. doi: 10.1176/appi.neuropsych.21.4.413
Schneider, J., Hofmann, A., Rost, C., and Shapiro, F. (2008). EMDR in the treatment of chronic phantom limb pain. Pain Med. Malden Mass 9, 76–82. doi: 10.1111/j.1526-4637.2007.00299.x
Shapiro, F. (2001). Eye Movement Desensitization and Reprocessing (EMDR): Basic Principles, Protocols, and Procedures, 2nd Edn. New York, NY: Guilford Press.
Siegert, R. J., and Abernethy, D. A. (2005). Depression in multiple sclerosis: areview. J. Neurol. Neurosurg. Psychiatry 76, 469–475. doi: 10.1136/jnnp.2004.054635
Silver, S. M., Brooks, A., and Obenchain, J. (1995). Treatment of Vietnam War veterans with PTSD: acomparison of eye movement desensitization and reprocessing, biofeedback, and relaxation training. J. Trauma. Stress 8, 337–342. doi: 10.1002/jts.2490080212
Smith, M. Y., Redd, W. H., Peyser, C., and Vogl, D. (1999). Post-traumatic stress disorder in cancer: areview. Psychooncology 8, 521–537. doi: 10.1002/(SICI)1099-1611(199911/12)8:6<521::AID-PON423>3.0.CO;2-X
Solari, A., Motta, A., Mendozzi, L., Aridon, P., Bergamaschi, R., Ghezzi, A., et al. (2004). Italian version of the Chicago multiscale depression inventory: translation, adaptation and testing in people with multiple sclerosis. Neurol. Sci. 24, 375–383. doi: 10.1007/s10072-003-0192-1
Taylor, S., Thordarson, D. S., Maxfield, L., Fedoroff, I. C., Lovell, K., and Ogrodniczuk, J. (2003). Comparative efficacy, speed, and adverse effects of three PTSD treatments: exposure therapy, EMDR, and relaxation training. J. Consult. Clin. Psychol. 71, 330–338. doi: 10.1037/0022-006X.71.2.330
Tedstone, J. E., and Tarrier, N. (2003). Posttraumatic stress disorder following medical illness and treatment. Clin. Psychol. Rev. 23, 409–448. doi: 10.1016/S0272-7358(03)00031-X
Theadom, A., Cropley, M., Smith, H. E., Feigin, V. L., and McPherson, K. (2015). Mind and body therapy for fibromyalgia. Cochrane Database Syst. Rev. 4, CD001980. doi: 10.1002/14651858.CD001980.pub3
Tol, W. A., Barbui, C., and van Ommeren, M. (2013). Management of acute stress, PTSD, and bereavement: WHO recommendations. JAMA 310, 477–478. doi: 10.1001/jama.2013.166723
Tuerk, P. W., Wangelin, B., Rauch, S. A. M., Dismuke, C. E., Yoder, M., Myrick, H., et al. (2013). Health service utilization before and after evidence-based treatment for PTSD. Psychol. Serv. 10, 401–409. doi: 10.1037/a0030549
Turner, R. J., and Lloyd, D. A. (1995). Lifetime traumas and mental health: the significance of cumulative adversity. J. Health Soc. Behav. 36, 360–376. doi: 10.2307/2137325
Van Etten, M. L., and Taylor, S. (1998). Comparative efficacy of treatments for post-traumatic stress disorder: ameta-analysis. Clin. Psychol. Psychother. 5, 126–144. doi: 10.1002/(SICI)1099-0879(199809)5:3<126::AID-CPP153>3.0.CO;2-H
van Kessel, K., Moss-Morris, R., Willoughby, E., Chalder, T., Johnson, M. H., and Robinson, E. (2008). A randomized controlled trial of cognitive behavior therapy for multiple sclerosis fatigue. Psychosom. Med. 70, 205–213. doi: 10.1097/PSY.0b013e3181643065
Wallin, M. T., Wilken, J. A., Turner, A. P., Williams, R. M., and Kane, R. (2006). Depression and multiple sclerosis: review of a lethal combination. J. Rehabil. Res. Dev. 43, 45–62. doi: 10.1682/JRRD.2004.09.0117
Weathers, F. W., Keane, T. M., and Davidson, J. R. (2001). Clinician-administered PTSD scale: areview of the first ten years of research. Depress. Anxiety 13, 132–156. doi: 10.1002/da.1029
Weiss, D. S., and Marmar, C. R. (1997). “The impact of event scale-revised,” in Assessing Psychological Trauma and PTSD, eds J. P. Wilson and T. M. Keane (New York, NY: Guilford Press), 399–411.
Whalley, B., Thompson, D. R., and Taylor, R. S. (2014). Psychological interventions for coronary heart disease: cochrane systematic review and meta-analysis. Int. J. Behav. Med. 21, 109–121. doi: 10.1007/s12529-012-9282-x
Yoo, H. J., Ahn, S. H., Kim, S. B., Kim, W. K., and Han, O. S. (2005). Efficacy of progressive muscle relaxation training and guided imagery in reducing chemotherapy side effects in patients with breast cancer and in improving their quality of life. Support. Care Cancer 13, 826–833. doi: 10.1007/s00520-005-0806-7
Zigmond, A. S., and Snaith, R. P. (1983). The hospital anxiety and depression scale. Acta Psychiatr. Scand. 67, 361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x
Keywords: multiple sclerosis, PTSD, EMDR, relaxation therapy, stress
Citation: Carletto S, Borghi M, Bertino G, Oliva F, Cavallo M, Hofmann A, Zennaro A, Malucchi S and Ostacoli L (2016) Treating Post-traumatic Stress Disorder in Patients with Multiple Sclerosis: A Randomized Controlled Trial Comparing the Efficacy of Eye Movement Desensitization and Reprocessing and Relaxation Therapy. Front. Psychol. 7:526. doi: 10.3389/fpsyg.2016.00526
Received: 17 February 2016; Accepted: 29 March 2016;
Published: 21 April 2016.
Edited by:
Francesco Pagnini, Catholic University of Milan, ItalyReviewed by:
Marcelo Fernandes Costa, Universidade de São Paulo, BrazilDeborah Phillips, Harvard University, USA
Copyright © 2016 Carletto, Borghi, Bertino, Oliva, Cavallo, Hofmann, Zennaro, Malucchi and Ostacoli. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sara Carletto, sara.carletto@unito.it
 Sara Carletto
Sara Carletto Martina Borghi
Martina Borghi Gabriella Bertino
Gabriella Bertino Francesco Oliva
Francesco Oliva Marco Cavallo
Marco Cavallo Arne Hofmann
Arne Hofmann Alessandro Zennaro
Alessandro Zennaro Simona Malucchi
Simona Malucchi Luca Ostacoli
Luca Ostacoli