- 1 “Vincent P. Dole” Dual Diagnosis Unit, Santa Chiara University Hospital, Department of Psychiatry, NPB, University of Pisa, Pisa, Italy
- 2 Association for the Application of Neuroscientific Knowledge to Social Aims, Lucca, Italy
- 3 “G. De Lisio,” Institute of Behavioral Sciences Pisa, Pisa, Italy
In this study we evaluated, by means of the “cocaine rush visual analog scale,” the impact of ropinirole on the expected rush induced by cocaine in a group of heroin addicts abusing cocaine; the self-reported reaction to the rush blockade (if any) on cocaine consumption, and the correlations between this self-reported reaction and individual, clinical, and therapeutic parameters. Nineteen cocaine abuser heroin-dependent patients entered the study. Their experienced cocaine rush was 61.31 ± 32.1% of the maximum effect previously experienced. Compared with their previous rush intensity 16 patients experienced significantly lower intensity, 3 the same intensity, and none a higher intensity. In particular, two patients experienced a complete blockade of rush and reported a reduced use of cocaine. Fourteen patients experienced a partial blockade of cocaine rush; of these, nine reported they had reduced their use of cocaine. Ropinirole does diminish the subjective intensity of an expected cocaine rush, so interfering with the dynamics of reward, while supporting its possible use in the treatment of cocaine dependence.
Introduction
To date, cocaine addiction is a poorly treatable disease that brings with it major trouble in terms of mortality, morbidity, and social life disruption (Dackis and O’Brien, 2001). In line with the paradigm of opiate addiction treatment, attempts have been made to ascertain the therapeutic potential of a variety of medications which have been tested for anti-craving and blocking properties (McCance, 1997; Grabowski et al., 2000; Sofuoglu and Kosten, 2005). On biochemical grounds, the mesolimbic dopaminergic pathway was regarded as the biological target in a majority of trials, so that a large variety of dopaminergic agents have been studied in cocaine addicts (Dackis and O’Brien, 2001; de Lima et al., 2002; Kosten et al., 2002; Soares et al., 2003; Sofuoglu and Kosten, 2005).
In rats, D2-selective dopamine antagonists increased cocaine self-administration (Caine et al., 2002). Dopamine antagonism alone, such as that provided by risperidone, or haloperidol and fluphenazine, does not seem to limit cocaine abuse, and may exacerbate it in former cocaine abusers who are being treated for psychoses (Ohuoha et al., 1997) or non-psychotic cocaine abusers (Grabowski et al., 2000). Moreover, the blockade of cocaine-induced subjective effects provided by D2-selective dopamine antagonists is incomplete, even though it may render cocaine less rewarding and more anxiogenic (Ohuoha et al., 1997). Disulfiram too has been employed in attempts to change the quality of cocaine consumption from pleasant and rewarding to aversive with contrasting results (George et al., 2000; Petrakis et al., 2000; Mutschler et al., 2009; Oliveto et al., 2011). The shifting of dopamine from blocked D2 receptors to other subtypes, or the engagement of dopamine excess on synaptic receptors may be responsible for the aversive reactions related to D2 blockade. On the other hand, partial antagonism may grant some benefits, by combining an anti-craving property with an at least partial cocaine blockade.
Unfortunately, current evidence does not support the clinical use of dopamine agonists such as amantadine, bromocriptine, and pergolide in the treatment of cocaine dependence (Soares et al., 2003). Amantadine, however, does not seem to act at a receptorial level and displayed no blockade property against cocaine-induced subjective effects (Collins et al., 2003).
Aripiprazole (APZ) is an atypical antipsychotic, with peculiar pharmacologic properties compared with the other second-generation antipsychotics. APZ is the first partial dopamine agonist antipsychotic to reach clinical practice. The peculiar partial-agonist activity at dopamine D2 receptors has stimulated researchers to test APZ in the treatment of cocaine abuse/addiction, but its efficacy is still controversial (Janiri et al., 2007; Cassano et al., 2009; Martinotti et al., 2009; Haney et al., 2011; Meini et al., 2011).
Ropinirole is a D2-selective dopaminergic full agonist (Hoefer et al., 2006) which does not show any significant affinity for the D1 receptor subtype, while it binds weakly to the μ-opioid receptor (Tulloch, 1997). It has proved useful and safe in the treatment of Parkinson’s disease (Lam, 2000; Matheson and Spencer, 2000; Jost, 2004) and Bipolar Depression (Perugi et al., 2001). A pilot open-label trial of ropinirole for cocaine dependence has shown promising results (Meini et al., 2008).
By applying this rationale, we formed the hypothesis that ropinirole might display blocking properties against cocaine by acting as a competitive agonist. In this case it would be a candidate for the treatment of cocaine addiction. Our view would be strengthened if ropinirole proved to be able to curtail the reinforcement of cocaine’s subjective effects on humans.
The aims of the present study are: (1) to verify the impact of ropinirole on the expected rush induced by cocaine in a group of stabilized heroin addicts with concurrent abuse of cocaine, (2) to evaluate the self-reported reaction to rush blockade, if any, on cocaine consumption and, lastly, (3) to assess the correlations between this self-reported reaction and individual, clinical and therapeutic parameters.
Materials and methods
Study Design
A naturalistic study was designed in order to assess, in a sample of heroin-dependent patients with concurrent abuse of cocaine and receiving treatment with opioid agonists, the impact of ropinirole on the expected rush induced by cocaine. All the patients included came from the PISA-methadone program. For the program’s setting and characteristics, please refer to our previous papers (Maremmani et al., 2007, 2008). We selected patients who had requested medication to limit their craving for cocaine. We studied patients who had taken prescribed ropinirole for almost 1 month and had used cocaine, at least once, during the ropinirole intake period. Patients were evaluated twice: at the beginning of the ropinirole treatment we recorded the prescribed dose of ropinirole and collected information in constructing a sociodemographic profile, clinical history, and cocaine involvement for each participant; at the end of the treatment period (lasting at least 1 month) we went on to record the intensity of the rush blockade and the self-reported reaction to it (whether the cocaine dose was being increased or decreased, or was held at its usual level).
All subjects gave their oral informed consent to the anonymous use of the questionnaires for research purposes. The study procedures were in accordance with the Helsinki Declaration of 1975.
Sample
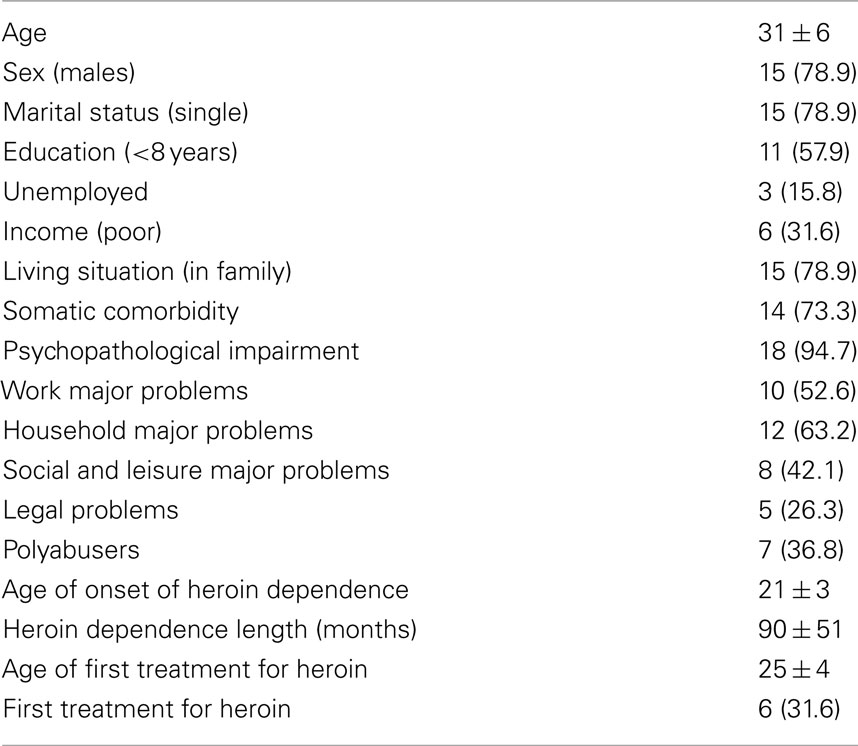
The sample consisted of 19 heroin-dependent patients. Table 1 reports main demographic and clinical characteristics of our patients.
According to Cocaine Problem Severity Index (CPSI-RS) criteria, 1 patient showed a recreational use of cocaine, 10 reported a non-addictive form of abuse (moderate severity), and 8 reported a markedly severe form of addiction that they judged to be treatable in an outpatient setting.
The ropinirole dosages prescribed were 1.23 ± 0.4 mg/daily.
Instruments
Sociodemographic and clinical features were recorded using the Drug Addiction History Rating Scale (DAH-RS; Maremmani and Castrogiovanni, 1989), an instrument which is tailored to the purpose of collecting clinical information in cases of heroin ab(use) and dependence.
The DAH-RS is a multi-scale questionnaire assessing the following issues: somatic health, mental health, typology of abused substances, current and lifetime features of opiate use, treatment history, social adjustment, and environmental factors. Nine factor scores are distinguished: physical problems, mental problems, polysubstance abuse, previous treatment, combined treatments, occupational level, family situation, sexual problems, socialization and leisure time, and drug-related legal problems.
The dysfunctional uses of cocaine were evaluated by the CPSI-RS (Rawson et al., 1989), in its Italian version. The CPSI-RS consists of 18 items, each with 4 possible answers. Its total score ranges from 0 to 84. The items investigate the degree of involvement with cocaine, the pattern of consumption, drug-related environmental features, and drug-induced somatic, mental and social impairment. Four categories of cocaine use status are distinguished, as follows: total score < 12 = recreational use; total score in the 13–25 range = non-addictive abuse or moderate severity; total score in the 26–55 range = addiction treatable in an outpatient setting or marked severity; total score in the 56–100 range = addiction requiring hospitalization or extreme severity). Non-users fall into a fifth, zero-score, category.
The impact of ropinirole on the expected rush induced by cocaine was evaluated by means of the “cocaine rush visual analog scale” (CRVAS). The CRVAS consisted of two parallel columns, representing the baseline expected intensity of cocaine rush (control column) and the level actually experienced while on ropinirole, in that order. The first, control column corresponded to a subjective 100%, and subjects were asked to mark how intense their cocaine rush had been, on average, while they were on ropinirole, in the second column. The CRAV was administered to obtain a retrospective assessment. Subjects had not been warned in advance of a possible cocaine blockade.
The following additional parameters were recorded for each patient: ropinirole dose, severity of cocaine use, intensity of rush blockage, self-reported reaction to possible blockade during the observation period.
Statistical analysis
We used a descriptive approach. Correlation between the percentage of maximum pre-ropinirole cocaine rush experienced and sociodemographic and clinical variables were tested by multiple regression analysis. Comparisons between time periods (intensity of cocaine rush pre-ropinirole over a patient’s lifetime vs. intensity during ropinirole treatment) were carried out using Wilcoxon matched-pairs signed ranks test.
We used the statistical routines of SPSS package.
Results
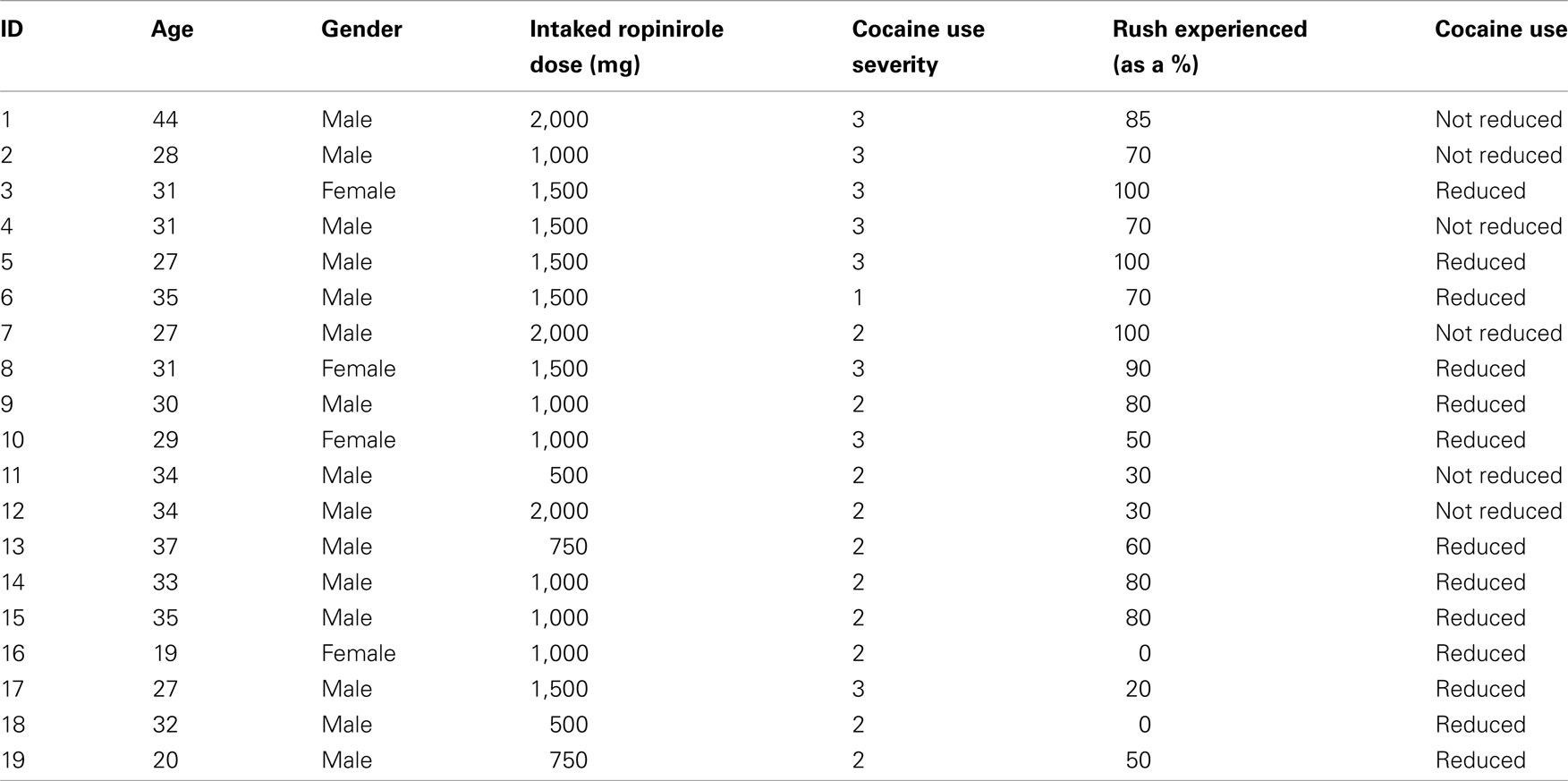
Table 2 shows various different features of the 19 patients belonging to the sample. We reported age, gender, prescribed ropinirole dose, severity of cocaine use, subjectively experienced cocaine rush as a percentage of the pre-ropinirole effect, and the self-reported post-ropinirole intake use of cocaine. Two patients (10.5%) experienced a complete blockade of cocaine rush and reported that, during the observation period, they had reduced their use of cocaine. Three patients (15.8%) felt cocaine as intensely as they expected, with no blockade at all; of these, two reported that they had reduced cocaine use during the observation period. Fourteen patients (73.7%) experienced a partial blockade of cocaine rush; of these, nine reported that they had reduced cocaine use during the observation period.
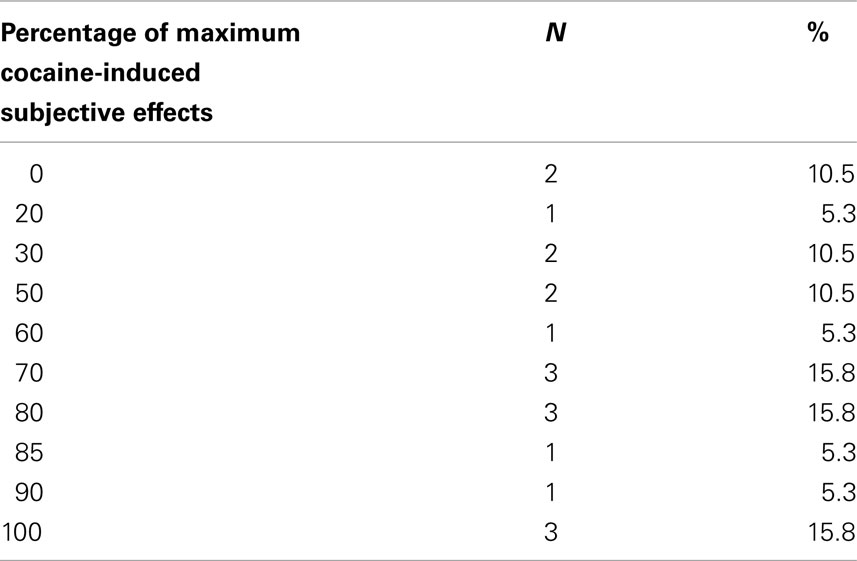
Compared with their previous rush intensity 16 patients experienced lower intensity, 3 the same intensity, and none a higher intensity (Wilcoxon pair test: z = −3.51; two-tailed P = 0.0004). For details, see Table 3.
Overall, patients experienced 61.31 ± 32.1% of the maximum intensity of the cocaine rush effect experienced in the past.
Using stepwise multiple regression analysis (criterion = percentage of maximum pre-ropinirole cocaine rush experienced), no correlations were found between criterion and age, gender, ropinirole dose, severity of cocaine use; no variables were entered/removed during the analysis.
Discussion
In a sample of stabilized heroin addicts with concurrent (ab)use of cocaine, ropinirole proved to have a partial (in 73.7% of participating subjects) or complete (in 10.5% of these subjects) blockade effect on the expected rush induced by cocaine. All the patients who experienced a complete blockade effect (n = 2) reported that their use of cocaine had fallen during the observation period. Of the patients who experienced a partial blockade effect (n = 14) a clear majority (n = 9) reported that their use of cocaine had been reduced during the observation period. Lastly, two of the three patients who felt cocaine to the same degree of intensity as they had expected reported a reduction in cocaine use during the observation period.
All the patients (except one) who requested cocaine anti-craving therapy scored above the CPSI threshold for cocaine abuse, so that the subjective judgment that they were in need of help turned out to be consistent with an objective measurement of the severity of their engagement with substance abuse.
Ropinirole does diminish the subjective intensity of the previously experienced cocaine rush, thus interfering with the dynamics of reward. This mechanism was probably fundamental in the two patients who experienced a complete blockade of their cocaine rush, by determining the subsequent self-reported reduction in their cocaine use. Looking at this question from another angle, it may be hypothesized that ropinirole’s dopamine-stimulating action reasonably provides a certain degree of support to the dopamine-mediated functions with a related anti-craving effects. This second mechanism could come into play, together with the first one, in the patients who experienced a partial blockade effect of their cocaine rush and reported that, during the observation period, they had reduced their use of cocaine. Lastly, the hypothesized anti-craving effect of ropinirole could at least partly explain the self-reported reduction in cocaine use in two patients who did not experience any blockade at all of cocaine rush. It should be added that this study does not support the hypothesis that the success or failure of an anti-reward approach depends on the severity of cocaine abuse.
To the best of our knowledge the role of ropinirole in cocaine dependence treatment has been the subject of very few investigations. In particular, only one pilot open-label trial has considered the administration of ropinirole in cocaine-dependent patients (Meini et al., 2008, 2011).
The modulation of reinforcing subjective cocaine effects, as reported by our patients, is consistent with the study just cited and supports several papers suggesting that psychostimulants may play a role in the pharmacotherapy of cocaine dependence (Castells et al., 2010). Other agents that support the dopaminergic system, such as disulfiram, have been tested in cocaine dependence treatment (Pani et al., 2010). In addition, ropinirole has been proposed as a possible therapeutic strategy for the treatment of methamphetamine abuse (Hoefer et al., 2006).
Nevertheless, it must be stressed that, on the therapeutic level, the reported partial capacity of ropinirole to block cocaine sensitivity proved to be insufficient, in our patients, to achieve their detachment from cocaine to any great degree. In fact, the “partial” anti-reward effect seems to be only partly mirrored by the therapeutic response, as far as reduction in cocaine use is concerned. In addition, the partial anti-reward coverage was unable to prevent the exacerbation of cocaine use to overcome the ropinirole-induced blockade. In other words, this anti-reward effect may promote ropinirole treatment discontinuation, presumably in order to restore patients’ sensitivity to cocaine.
This phenomenon resembles that of the effects of buprenorphine on the mu-opioidergic system. On the other hand, in a way similar to that found with buprenorphine, the low degree of agonist action coupled with a significant level of blockade may turn out to be critical in patients whose metabolic system has undergone major conditioning by substance intoxication (Dum and Herz, 1981; Budd, 1983; Bickel et al., 1988; Walsh et al., 1995; Barnett et al., 2001; Zuurmond et al., 2002; Virk et al., 2009).
Limitations
As limitations we must consider the low number of subjects and the naturalistic design of the study. Besides, another limitation is that the subjects included in the study were methadone treated heroin addicts and not pure cocaine users. The presence of multiple substance abuse is a common and peculiar condition that can alter the interpretation of data.
Conclusion
In conclusion, this study, which suggests that ropinirole may exert a partial blocking effect on cocaine rush, supports the view that this medication could play a positive role in the pharmacotherapy of cocaine dependence.
Randomized controlled trials are now needed to verify this hypothesis.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
Barnett, P. G., Rodgers, J. H., and Bloch, D. A. (2001). A meta-analysis comparing buprenorphine to methadone for treatment of opiate dependence. Addiction 96, 683–690.
Bickel, W. K., Stitzer, M. L., Begelow, G. E., Liebson, I. A., Jasinski, D. R., and Johnson, R. E. (1988). Buprenorphine: dose-related blockade of opioid challenge in opioid dependent humans. J. Pharmacol. Exp. Ther. 247, 47–53.
Caine, S. B., Negus, S. S., Mello, N. K., Patel, S., Bristow, L., Kulagowski, J., Vallone, D., Saiardi, A., and Borrelli, E. (2002). Role of dopamine D2-like receptors in cocaine self-administration: studies with D2 receptor mutant mice and novel D2 receptor antagonists. J. Neurosci. 22, 2977–2988.
Cassano, G. B., Lattanzi, L., Litta, A., Lombardi, V., Tatulli, A., Benedetti, A., Longobardi, A., and Maremmani, I. (2009). Is aripripazole useful to refrain from cocaine use after detoxification (avoiding relapses)? Addict. Disord. Their Treat. 8, 161–166.
Castells, X., Casas, M., Perez-Mana, C., Roncero, C., Vidal, X., and Capella, D. (2010). Efficacy of psychostimulant drugs for cocaine dependence. Cochrane Database Syst. Rev. CD007380. doi: 10.1002/14651858.CD007380.pub3.
Collins, E. D., Vosburg, S. K., Hart, C. L., Haney, M., and Foltin, R. W. (2003). Amantadine does not modulate reinforcing, subjective, or cardiovascular effects of cocaine in humans. Pharmacol. Biochem. Behav. 76, 401–407.
Dackis, C. A., and O’Brien, C. P. (2001). Cocaine dependence: a disease of the brain’s reward centers. J. Subst. Abuse Treat. 21, 111–117.
de Lima, M. S., de Oliveira Soares, B. G., Reisser, A. A., and Farrell, M. (2002). Pharmacological treatment of cocaine dependence: a systematic review. Addiction 97, 931–949.
Dum, J. E., and Herz, A. (1981). In vivo receptor binding of the opiate partial agonist, buprenorphine, correlated with its agonistic and antagonistic actions. Br. J. Pharmacol. 74, 627–633.
George, T. P., Chawarski, M. C., Pakes, J., Carroll, K. M., Kosten, T. R., and Schottenfeld, R. S. (2000). Disulfiram versus placebo for cocaine dependence in buprenorphine-maintained subjects: a preliminary trial. Biol. Psychiatry 47, 1080–1086.
Grabowski, J., Rhoades, H., Silverman, P., Schmitz, J. M., Stotts, A., Creson, D., and Bailey, R. (2000). Risperidone for the treatment of cocaine dependence: randomized, double-blind trial. J. Clin. Psychopharmacol. 20, 305–310.
Haney, M., Rubin, E., and Foltin, R. W. (2011). Aripiprazole maintenance increases smoked cocaine self-administration in humans. Psychopharmacology (Berl.) 216, 379–387.
Hoefer, M. E., Voskanian, S. J., Koob, G. F., and Pulvirenti, L. (2006). Effects of terguride, ropinirole, and acetyl-L-carnitine on methamphetamine withdrawal in the rat. Pharmacol. Biochem. Behav. 83, 403–409.
Janiri, L., Martinotti, G., and Di Nicola, M. (2007). Aripiprazole for relapse prevention and craving in alcohol-dependent subjects: results from a pilot study. J. Clin. Psychopharmacol. 27, 519–520.
Jost, W. H. (2004). Ropinirole: current status of the studies. J. Neurol. 251(Suppl. 6), VI/13–VI/18.
Kosten, T. R., George, T. P., and Kosten, T. A. (2002). The potential of dopamine agonists in drug addiction. Expert Opin. Investig. Drugs 11, 491–499.
Maremmani, I., and Castrogiovanni, P. (1989). DAH-RS: Drug Addiction History Rating Scale. Pisa: University Press.
Maremmani, I., Pacini, M., Lubrano, S., Perugi, G., Tagliamonte, A., Pani, P. P., Gerra, G., and Shinderman, M. (2008). Long-term outcomes of treatment-resistant heroin addicts with and without DSM-IV axis I psychiatric comorbidity (dual diagnosis). Eur. Addict. Res. 14, 134–142.
Maremmani, I., Pani, P. P., Mellini, A., Pacini, M., Marini, G., Lovrecic, M., Perugi, G., and Shinderman, M. (2007). Alcohol and cocaine use and abuse among opioid addicts engaged in a methadone maintenance treatment program. J. Addict. Dis. 26, 61–70.
Martinotti, G., Di Nicola, M., Di Giannantonio, M., and Janiri, L. (2009). Aripiprazole in the treatment of patients with alcohol dependence: a double-blind, comparison trial vs. naltrexone. J. Psychopharmacol. 23, 123–129.
Matheson, A. J., and Spencer, C. M. (2000). Ropinirole: a review of its use in the management of Parkinson’s disease. Drugs 60, 115–137.
McCance, E. F. (1997). Overview of potential treatment medications for cocaine dependence. NIDA Res. Monogr. 175, 36–72.
Meini, M., Capovani, B., Sbrana, A., Massei, G. J., Ravani, L., Massimetti, G., Daini, L., Scaramelli, D., and Moncini, M. (2008). A pilot open-label trial of ropinirole for cocaine dependence. Am. J. Addict. 17, 165–166.
Meini, M., Moncini, M., Cecconi, D., Cellesi, V., Biasci, L., Simoni, G., Ameglio, M., Pellegrini, M., Forgione, R. N., and Rucci, P. (2011). Aripiprazole and ropinirole treatment for cocaine dependence: evidence from a pilot study. Curr. Pharm. Des. 17, 1376–1383.
Mutschler, J., Diehl, A., and Kiefer, F. (2009). Pronounced paranoia as a result of cocaine-disulfiram interaction: case report and mode of action. J. Clin. Psychopharmacol. 29, 99–101.
Ohuoha, D. C., Maxwell, J. A., Thomson, L. E. III, Cadet, J. L., and Rothman, R. B. (1997). Effect of dopamine receptor antagonists on cocaine subjective effects: a naturalistic case study. J. Subst. Abuse Treat. 14, 249–258.
Oliveto, A., Poling, J., Mancino, M. J., Feldman, Z., Cubells, J. F., Pruzinsky, R., Gonsai, K., Cargile, C., Sofuoglu, M., Chopra, M. P., Gonzalez-Haddad, G., Carroll, K. M., and Kosten, T. R. (2011). Randomized, double blind, placebo-controlled trial of disulfiram for the treatment of cocaine dependence in methadone-stabilized patients. Drug Alcohol Depend. 113, 184–191.
Pani, P. P., Trogu, E., Vacca, R., Amato, L., Vecchi, S., and Davoli, M. (2010). Disulfiram for the treatment of cocaine dependence. Cochrane Database Syst. Rev. 1, CD007024.
Perugi, G., Toni, C., Ruffolo, G., Frare, F., and Akiskal, H. (2001). Adjunctive dopamine agonists in treatment-resistant bipolar II depression: an open case series. Pharmacopsychiatry 34, 137–141.
Petrakis, I. L., Carroll, K. M., Nich, C., Gordon, L. T., McCance-Katz, E. F., Frankforter, T., and Rounsaville, B. J. (2000). Disulfiram treatment for cocaine dependence in methadone-maintained opioid addicts. Addiction 95, 219–228.
Rawson, R. A., Obert, J. L., McCann, D. P., Smith, D. P., and Scheffey, E. H. (1989). The Neurobehavioural Treatment Manual: A Therapist Manual for Outpatient Cocaine Addiction Treatment. Bevery Hills, CA: Matrix Center.
Soares, B. G., Lima, M. S., Reisser, A. A., and Farrell, M. (2003). Dopamine agonists for cocaine dependence. Cochrane Database Syst. Rev. CD003352. doi: 10.1002/14651858.CD003352.pub2.
Sofuoglu, M., and Kosten, T. R. (2005). Novel approaches to the treatment of cocaine addiction. CNS Drugs 19, 13–25.
Tulloch, I. F. (1997). Pharmacologic profile of ropinirole: a nonergoline dopamine agonist. Neurology 49(1 Suppl. 1), S58–S62.
Virk, M. S., Arttamangkul, S., Birdsong, W. T., and Williams, J. T. (2009). Buprenorphine is a weak partial agonist that inhibits opioid receptor desensitization. J. Neurosci. 29, 7341–7348.
Walsh, S. L., Preston, K. L., Bigelow, G. E., and Stitzer, M. L. (1995). Acute administration of buprenorphine in humans: partial agonist and blockade effects. J. Pharmacol. Exp. Ther. 274, 361–372.
Keywords: ropinirole, cocaine abuse, blockade effect, anti-craving effect
Citation: Maremmani AGI, Pacini M, Rovai L, Rugani F, Dell’Osso L and Maremmani I (2011) Can ropinirole modulate reinforcing subjective effects of cocaine in humans? Front. Psychiatry 2:50. doi: 10.3389/fpsyt.2011.00050
Received: 08 April 2011;
Accepted: 23 July 2011;
Published online: 02 August 2011.
Edited by:
Marco Diana, University of Sassari, ItalyReviewed by:
Giovanni Martinotti, Catholic University of Rome, ItalyDiana Martinez, Columbia University, USA
Lorenzo Somaini, Addiction Treatment Centre Local Health Unit Biella, Italy
Copyright: © 2011 Maremmani, Pacini, Rovai, Rugani, Dell’Osso and Maremmani. This is an open-access article subject to a non-exclusive license between the authors and Frontiers Media SA, which permits use, distribution and reproduction in other forums, provided the original authors and source are credited and other Frontiers conditions are complied with.
*Correspondence: Icro Maremmani, “Vincent P. Dole” Dual Diagnosis Unit, Santa Chiara University Hospital, Department of Psychiatry, University of Pisa, Via Roma, 67 56100 Pisa, Italy. e-mail: maremman@med.unipi.it
 Angelo Giovanni Icro Maremmani1,2
Angelo Giovanni Icro Maremmani1,2