- 1 Departamento de Salud Mental, Facultad de Medicina, Universidad Nacional Autónoma de México, Distrito Federal, Mexico
- 2 Instituto Nacional de Psiquiatría “Ramón de la Fuente Muñíz,”, Distrito Federal, Mexico
- 3 Department of Psychiatry, Yale University School of Medicine, New Haven, CT, USA
- 4 Yale Child Study Center, Yale University School of Medicine, New Haven, CT, USA
School dropout has significant consequences for both individuals and societies. Only 21% of adults in Mexico achieve the equivalent of a high school education. We examined the relationship between school dropout and self-reported psychiatric symptoms in a middle school in a suburb of Mexico City. We used binomial logistic regression to examine the odds ratio (OR) of school dropout associated with students’ self-reported psychopathology. Two-hundred thirty-seven students participated in the study. Psychosis [OR = 8.0 (95% confidence interval, CI: 1.7–37.2)], depression [OR = 4.7 (95% CI: 2.2–9.7)], tic disorders [OR = 3.7 (95% CI: 1.4–9.5)], ADHD [OR = 3.2 (95% CI: 1.5–6.4)], and social phobia [OR = 2.6 (95% CI: 1.2–5.8)] were associated with increased risk of school dropout after controlling for age and gender as covariates. Our study suggested that students’ self-reported psychopathology is associated with increased school dropout in Mexico. ADHD and depression may be particularly useful childhood psychiatric disorders to target with public health interventions because they explain the greatest amount of the variance in school dropout of child psychiatric disorders.
Introduction
School dropout has significant consequences for both individuals and societies. Little has been written about the impact of school dropouts in Mexico. According to published data from the United States, high school dropouts are twice as likely to be unemployed as high school graduates (KewalRamani et al., 2007). For those high school dropouts fortunate enough to work, pay is considerably lower. The average high school dropout in the United States earns just 37 cents for every dollar that is earned by a high school graduate (Rumberger and Thomas, 2000). Eighty-eight percent of adults in the United States of America have achieved at least a secondary level of education (OECD, 2003). However, graduation rates among underrepresented minority students, particularly Latinos and African Americans, are even lower (KewalRamani et al., 2007). Only slightly more than half of these student populations graduate from high school on time. U.S. Latinos have the highest dropout rate of all the major racial/ethnic groups, and youths of Mexican descent are especially susceptible to not completing school (Valencia, 2002; Calderón et al., 2009). Because the lack of information on this subject from Mexico, it is difficult to draw conclusions from this last statement.
In Mexico, much less is known about school dropouts, but it is clear the problem is quite dire. More than half of the adults in Mexico have at most a primary level education (equivalent to grade school education in the USA). Only 21% of adults in Mexico have a secondary level of education (equivalent to a high school education in the USA; OECD, 2010). Increased drug use has been associated with poor school attendance and dropout rates (Tavares et al., 2001). Among Mexican middle school students, poor academic performance was associated with increased depressive symptomatology (de la Peña et al., 1999). Roughly one in five Mexican children experiences a significant child psychiatric illness in his lifetime (Sauceda, 1994). In both the United States and Mexico, improving high school graduation rates continues to be a formidable educational and public health challenge (Ream and Rumberger, 2008). Childhood psychopathology represents both a possible predictor of future school dropout and a potential area for intervention.
The purpose of this study is to examine the association between self-reported childhood psychopathology and school dropout by the end of the school year in a cohort of Mexican middle school students. Our goals are to determine the child symptoms suggestive of a psychiatric disorder that seem to be most strongly associated with future school dropout and to determine which child symptoms suggestive of a psychiatric disorder accounted for the greatest number of school dropouts.
Materials and Methods
Selection
Subjects were recruited from the Technical Middle – High School Num. One hundred sixteen “Netzahualpilli” in the town of Texcoco, Mexico, located in the metropolitan area of Mexico City. The school was chosen by convenience because the school administrative authorities were enthusiastic about the research study and shared valuable information regarding grades, academic history of the subjects, all this information could be accessed after the proper parent consent and student ascent. The school population is generally lower middle-class, with no significant racial-ethnic diversity. All children between the ages of 12–15 years enrolled at this school were eligible. In order to participate, subjects, and their parents were required to read and sign an informed consent form.
All subjects were evaluated with the following set of scales.
The dimensional scale of psychopathology in adolescence (EDPA)
It consists of 66 items in a Likert type scale. Validation studies show an internal consistency set of a Cronbach alpha of 0.92, differentiation of externalized and internalized symptoms the Cronbach alpha values were of 0.89 and 0.85 respectively. Test–retest on both versions was of r = 0.87 (Suarez, 1999).
The scale for the evaluation of externalized problems in kids, adolescents, and young adults (EPE-AA)
Validation of this scale reported by the factor analisys of clinical population show the following data: five factors with a cumulative variance of 40.7%. Inattention factor explained the 9.9% of variance, oppositional factor 8.8%, hyperactive–impulsive factor 7.7%, dissocial–predatory 7.5%, and dissocial non-predatory 6.8%. The Cronbach value pretest was 0.9114 and posttest 0.9224. Confiability test–retest was made by Pearsons’ r for each factor and showed: inattention factor (r = 0.77 vs 0.79), oppositional defiant factor (r = 0.64 vs 0.74), hyperactive-inattention factor (r = 0.76 vs 0.77; Palacios, 2003).
The screen for child anxiety related emotional disorders
Internal consistency was measured with Cronbach alpha with an internal consistency for children of 0.87 and parents of 0.85. The factorial analysis by Cronbach alpha for panic-somatization was 0.71, generalized anxiety of 0.63, social fobia of 0.25, and school fobia of 0.65. There were not significative differences between sex and age (Birmaher et al., 1997).
The depression self rating scale
The internal consistency with a Cronbach alpha in clinical population was of 0.85 and 0.77 for open population. The cutoff of 14 obtains the most stability between sensitivity and specificity of 87 and 74 respectively (de la Peña et al., 1996).
ADHD rating scale-IV
Questionnaire that includes 18 articles referred to the symptoms DSM-IV. It can be administered by a clinician or be self-reported by the patient or with a direct relative (DuPaul et al., 1998).
Each student had 30–60 min of class time to answer the self-reports; this was done with previous authorization of the class teacher. At the end of the academic year, the school officials provided us with information regarding school year completion success and overall grade point averages for each subject. All the information respecting psychopathology was self-reported, we did not retrieved parents reports.
Subjects
A total of 237 subjects (91 males and 146 females) out of 526 eligible students participated in the study, with the average age being 13.4 ± 0.9 years old. The participation rate was 31% (23% for males and 39% for females). Participants were more likely to be female (χ2 = 23.2, df = 1, p < 0.001) and have better grades than non-participants (t = 19.1, df = 759, p < 0.001). During the year this study was conducted the school dropout rate in this particular school was 15.7% and males dropped out more frequently than females.
Data Analysis
Likely presence of child symptoms suggestive of a psychiatric disorder were determined based on the self-report rating scale score. Their cutoff points are as follows: DRSR (depression) >15, SCARED subscales: panic >7, general anxiety >9, separation anxiety >5, social phobia >8, school phobia >3, ADHD >18, EDPA subscales: psychotic symptoms >12, obsessive–compulsive symptoms >8, Substance use (alcohol, drugs, or tobacco) >1, eating disorder >8, elimination disorder >2. Finally, for the EPE-AA, the sum of the total scores on the predatory conduct disorder, non-predatory conduct disorder and oppositional defiant disorder subscales. These cutoff points are not validated cutoffs for each scale, but rather were determined prior to data analysis by noting where the natural splits in the data occurred.
To determine the association between school dropout and child symptoms suggestive of a psychiatric disorder, we conducted binomial logistic regression analysis, with dropout status as the dependent variable and child symptoms suggestive of a psychiatric disorder as the independent variable. We conducted this analysis with and without age and gender as covariates in our model as a way to determine the odds ratio (OR) for children who dropped out of school who had symptoms suggestive of a psychiatric disorder compared to those who did not have symptoms. In order to determine how much of the overall dropout rate could be explained by child symptoms suggestive of a psychiatric disorder, we conducted an exploratory forward stepwise binomial logistic regression model with school dropout as the dependent variable and rating scale scores and gender, when appropriate, as the potential variables of interest. Terms were entered into the regression model for p < 0.05 and discarded for p > 0.1. We ran exploratory models for all the children and then again for boys and girls separately.
Results
Association between Child Psychopathology and Dropout
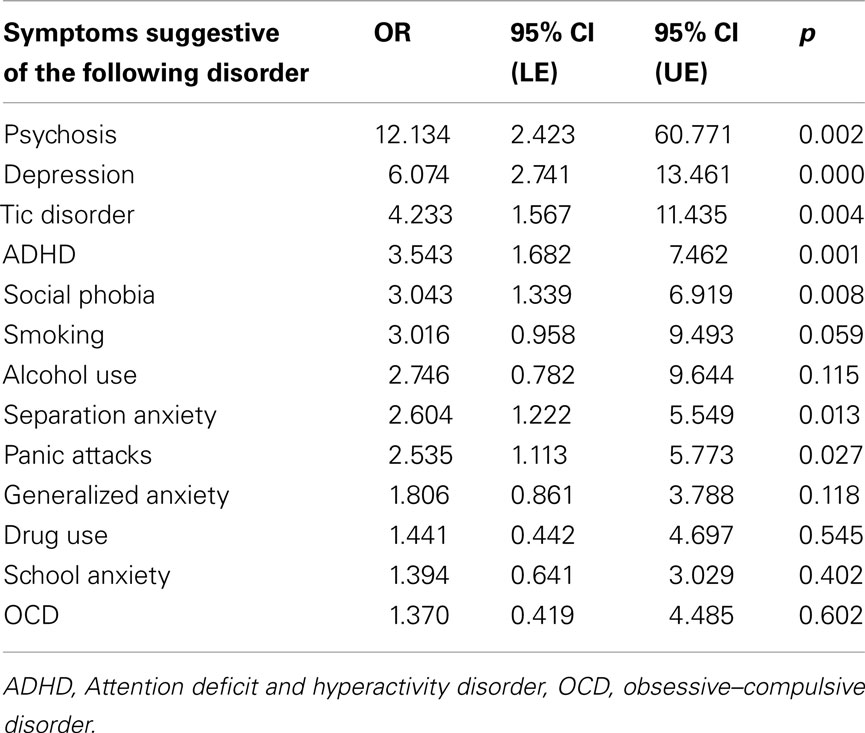
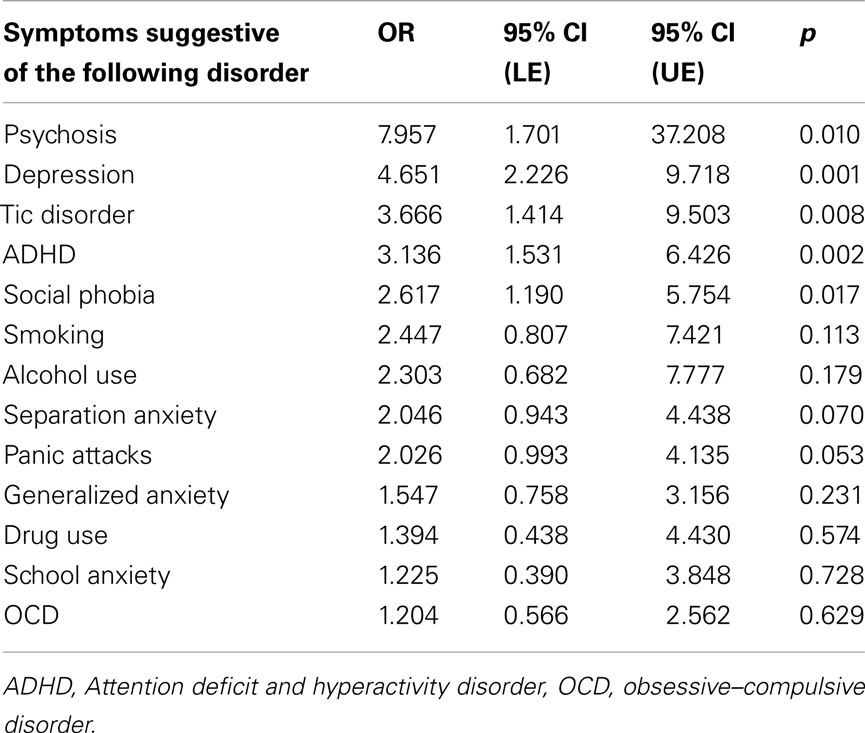
Table 1 depicts the association between dropout and the child symptoms suggestive of a psychiatric disorder adjusting for age and gender as covariates and Table 2 depicts the association between dropout and the child symptoms suggestive of a psychiatric disorder without adjusting for age and gender as covariates. There was a significant association between school dropout and the number of child symptoms suggestive of a psychiatric disorder, including psychosis, depression, tics, ADHD, and social anxiety. Additionally, separation anxiety and panic attacks were associated with school dropout after controlling for age and gender as covariates.
Exploratory Best-Fit Model for Explaining Dropout and Child Psychopathology
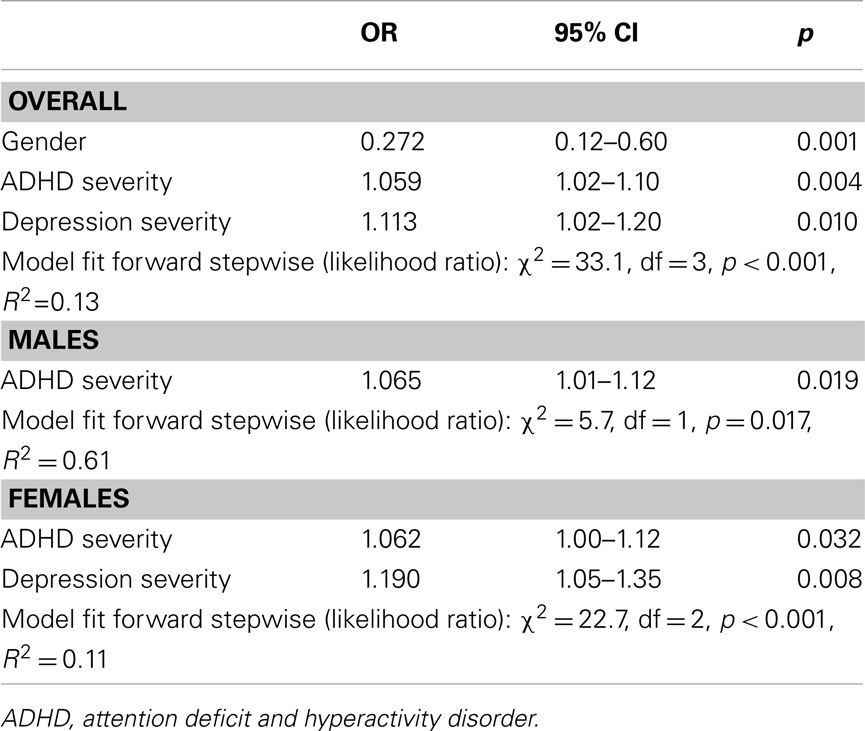
Table 3 depicts the best-fit model for explaining school dropout based on child symptoms suggestive of a psychiatric disorder. Among all children, increased school dropout was associated with male gender and severity of self-reported ADHD and depression symptoms. These variables explained only 13% of the variance in overall dropout rates. We also found that among females, increased ADHD and depression symptoms were significantly associated with increased dropout and among males ADHD symptoms were associated with dropout.
Discussion
Epidemiological studies suggest that approximately 15% of children in Mexico have a significant mental illness by age 14 (SSA, 2001). In our study we found that the presence of self-reported psychiatric symptoms is associated with increased risk for school dropout. Self-reported symptoms of psychosis, depression, ADHD, tics, social phobia, and other anxiety disorders were specifically associated with future school dropout. School dropout has profound negative consequences in Mexico and worldwide. Failure to graduate is associated with greater lifetime unemployment and lower anticipated wages. The natural history of many of these child psychiatric disorders (particularly depression, ADHD, and social phobia), can be altered dramatically with proper treatment (March et al., 2004, 2009; Kratochvil et al., 2009; Molina et al., 2009; Reinecke et al., 2009). With early intervention, the developmental impact of all of these disorders can be minimized (Birmaher et al., 1996; Graham et al., 2006). Thus, our data suggests that in many cases the self-reported screening strategies may be able to identify individuals with high likelihood of having child mental issues that are associated with school dropout and that children appear willing to endorse symptoms on self-report measures. This data also suggests that not only educational interventions but interventions designed to improve overall childhood mental health in Mexico may decrease school dropout rates. Of course, these hypotheses need to be analyzed in larger, multi-school studies that use structured assessment for clinical psychiatric diagnoses and measure important covariates like intelligence, parental education, and socio-economic status.
Population based surveys of physicians who treat children and adolescents reveal that the rate and proportion of office visits associated with ADHD are high, and have increased during the past decade. They also show that until recent years clinical guidelines were not available for country-specific populations (Ulloa et al., 2005). According to the Pan-American Health Organization, Latin America’s and the Caribbean’s access to health services is restricted to less than 30% of the general population, with access to mental health services being even worse, and potentially generating severe stigma, and economic and social problems (Acuña and Bolis, 2005). Our logistic regression model suggests that ADHD and depression may be particularly useful childhood psychiatric disorders to target with public health interventions because they (1) explain the greatest amount of the variance in school dropout of child psychiatric disorders and (2) they respond well to treatment.
In light of our findings, this study has several limitations. We relied on childrens’ self-reported measures of psychiatric illness, without using formal structured clinical assessments to confirm these diagnoses. Our screening tools involved the use of many rating scales that have not been validated in the Spanish language and our analysis relied on un-validated cutoff points in many of the scales. Thus, we can only conclude from our data that specific self-reported psychiatric symptoms are associated with dropout, not necessarily the disorders themselves. Another limitation of this study is that our data came exclusively from one middle school in Mexico. This school was chosen by convenience and because we thought it would be likely to be representative of urban education in Mexico. We do not know how well the results from this school can be generalized to the rest of Mexico or the developing world. Further studies need to examine the generalizability of our results. Additionally, we did not measure potentially important confounders in the study population including intelligence, reading level, socioeconomical status, and parental education. Finally, only 31% of students completed self-report measures. Students who participated in this study were more likely to be female and have better academic performance than those who chose not to participate. Thus, we cannot say that these populations did not differ in additional unmeasured variables
Despite the limitations our study suggested that several different types of child symptoms suggestive of a psychiatric disorder (ADHD, depression, psychosis, tics, and social phobia) are associated with increased rate of school dropout in Mexico. We also found that children are willing to self-report most psychiatric symptoms. This is a very significant finding, as these self-report screening strategies may be very useful in helping decrease the number of school dropouts. There are already certain teen screening programs designed to target adolescent suicide in the US, and these programs have been highly successful at screening for depression using self-report measures (Shaffer et al., 1998; Aseltine and DeMartino, 2004; Levitt et al., 2004; Gould et al., 2005). Improvements in screening and treatment of these childhood mental disorders in Mexico may lead, not only to improved overall mental well-being in children, but also to decreased academic failure. Future studies exploring the feasibility, possible methodologies, and potential impact of child mental health screening in Mexico are needed. By enhancing child mental health education, screening, and treatment, we will very likely see an improved quality of life and mental health for these individuals, as well as the overall health, education, and economy of the Mexican society.
Finally, it is important for parents and school authorities to be aware and in constant communication about the issues of mental health of children and adolescents, since early detection of child psychiatric disorders has the potential to lead to better overall child mental health, academic performance and future quality of life (Kessler et al., 1995).
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors acknowledge the National Institute of Mental Health support of the Yale Child Study Center Research Training Program (MHB), the National Institutes of Health Loan Repayment Program (MHB), the support of the Tourette’s Syndrome Association Inc. (MHB), the APIRE/Eli Lilly Psychiatric Research Fellowship (MHB), the AACAP/Eli Lilly Pilot Research Award (MHB), the Trichotillomania Learning Center (MHB) and NARSAD (MHB). Academic Committee, Scholarship Committee and Education Department at the National Institute of Psychiatry “Ramón de la Fuente Muñíz”, México, DF. Thanks to Prof. Gerardo Gallardo, Alicia Chalita and Fernanda Perez Tagle for their administrative support.
References
Acuña, C., and Bolis, M. (2005). La estigmatización y el acceso a la atención de salud en América Latina: Amenazas y perspectivas. Available at: http://www.paho.org/Project.asp?SEL=TP&LNG=ENG&ID=216
Aseltine, R. H., and DeMartino, R. (2004). An outcome evaluation of the SOS Suicide Prevention Program. Am. J. Public Health 94, 446–451.
Birmaher, B., Khetarpal, S., Brent, D., Cully, M., Balach, L., Kaufman, J., and Neer, S. M. (1997). The Screen for Child Anxiety Related Emotional Disorders (SCARED): scale construction and psychometric characteristics. J. Am. Acad. Child Adolesc. Psychiatry 36, 545–553.
Birmaher, B., Ryan, N. D., Williamson, D. E., Brent, D. A., Kaufman, J., Dahl, R. E., Perel, J., and Nelson, B. (1996). Childhood and adolescent depression: a review of the past 10 years. Part I. J. Am. Acad. Child Adolesc. Psychiatry 35, 1427–1439.
Calderón, J. M., Robles, R. R., Reyes, J. C., Matos, T. D., Negrón, J. L., and Cruz, M. A. (2009). Predictors of school dropout among adolescents in Puerto Rico. P. R. Health Sci. J. 28, 307–312.
de la Peña, F., Estrada, A., Almeida, L., and Páez, F. (1999). Prevalence of depressive disorders and low academic achievement in junior high school students. Salud Ment. 22, 9–13.
de la Peña, F., Lara, M. C., and Cortes, J. (1996). Traducción al español y validez de la escala de Birleson (DSRS) para el trastorno depresivo mayor en la adolescencia. Salud Ment. 3, 17–23.
DuPaul, G. J., Power, T. J., Anastopoulos, A. D., and Reid, R. (1998). ADHD Rating Scale – IV: Checklists, Norms, and Clinical Interpretation. New York, NY: Guilford Press.
Gould, M. S., Marrocco, F. A., Kleinman, M., Thomas, J. G., Mostkoff, K., Cote, J., and Davies, M. (2005). Evaluating iatrogenic risk of youth suicide screening programs: a randomized controlled trial. JAMA 293, 1635–1643.
Graham, E., Kratochvil, C., Vitiello, B., Silva, S., Mayes, T., McNulty, S., Weller, E., Waslick, B., Casat, C., Walkup, J., Pathak, S., Rohde, P., Posner, K., March, J., and Columbia Suicidality Classification Group; TADS Team. (2006). Treatment for Adolescents with Depression Study (TADS): safety results. J. Am. Acad. Child Adolesc. Psychiatry 45, 1440–1455.
Kessler, R. C., Foster, C. L., Saunders, W. B., and Stang, P. E. (1995). Social consequences of psychiatric disorders, I: educational attainment. Am. J. Psychiatry 152, 1026–1032.
KewalRamani, A., Gilbertson, L., Fox, M. A., and Provasnik, S. (2007). Status and trends in the education of racial and ethnic minorities. NCES 2007-039. Available at: http://nces.ed.gov/pubs2007/minoritytrends/ind_4_17.asp.
Kratochvil, C. J., May, D. E., Silva, S. G., Madaan, V., Puumala, S. E., Curry, J. F., Walkup, J., Kepley, H., Vitiello, B., and March, J. S. (2009). Treatment response in depressed adolescents with and without co-morbid attention-deficit/hyperactivity disorder in the Treatment for Adolescents with Depression Study. J. Child Adolesc. Psychopharmacol. 19, 519–527.
Levitt, J. M., WonPat-Borja, A., Buffered, S., and Jensen, P. (2004). Implementing Evidence-Based Assessment Strategies in Schools. Honolulu, HI: American Psychological Association.
March, J., Silva, S., Curry, J., Wells, K., Fairbank, J., Burns, B., Domino, M., Vitiello, B., Severe, J., Riedal, K., Goldman, M., Feeny, N., Findling, R., Stull, S., Baab, S., Weller, E. B., Robbins, M., Weller, R. A., Jessani, N., Waslick, B., Sweeney, M., Dublin, R., Walkup, J., Ginsburg, G., Kastelic, E., Koo, H., Kratochvil, C., May, D., LaGrone, R., Vaughan, B., Albano, A. M., Hirsch, G. S., Podniesinki, E., Chu, A., Reincecke, M., Leventhal, B., Rogers, G., Jacobs, R., Pathak, S., Wells, J., Lavanier, S. A., Danielyan, A., Rohde, P., Simons, A., Grimm, J., Frank, S., Emslie, G., Kennard, B., Hughes, C., Mayes, T. L., Rosenberg, D., Benazon, N., Butkus, M., and Bartoi, M. (2009). The Treatment for Adolescents With Depression Study (TADS): outcomes over 1 year of naturalistic follow-up. Am. J. Psychiatry 166, 1141–1149.
March, J., Silva, S., Petrycki, S., Curry, J., Wells, K., Fairbank, J., Burns, B., Domino, M., McNulty, S., Vitiello, B., Severe, J., and Treatment for Adolescents with Depression Study (TADS) Team. (2004). Fluoxetine, cognitive-behavioral therapy, and their combination for adolescents with depression: Treatment for Adolescents with Depression Study (TADS) randomized controlled trial. JAMA 292, 807–820.
Molina, B. S., Hinshaw, S. P., Swanson, J. M., Arnold, L. E., Vitiello, B., Jensen, P. S., Epstein, J. N., Hoza, B., Hechtman, L., Abikoff, H. B., Elliott, G. R., Greenhill, L. L., Newcorn, J. H., Wells, K. C., Wigal, T., Gibbons, R. D., Hur, K., Houck, P. R., and MTA Cooperative Group. (2009). The MTA at 8 years: prospective follow-up of children treated for combined-type ADHD in a multisite study. J. Am. Acad. Child Adolesc. Psychiatry 48, 484–500.
OECD. (2003). Online Education Database (Internet; cited 2010). Available at: http://www.oecd.org/document/54/0,3343,en_2649_39263238_38082166_1_1_1_37455,00.html#9
OECD. (2010). StatExtracts. Available at: http://stats.oecd.org/Index.aspx?DatasetCode=RPOP.
Palacios, L. (2003). Escala de evaluacion de problemas externalizados para adolescentes y adultos jovenes (EPE-AA). M. S. Thesis, UNAM, Mexico.
Ream, R. K., and Rumberger, R. W. (2008). Student Engagement, Peer Social Capital, and School Dropout Among Mexican American and Non-Latino White Students. Sociol. Educ. 81, 109–139.
Reinecke, M. A., Curry, J. F., and March, J. S. (2009). Findings from the Treatment for Adolescents with Depression Study (TADS): what have we learned? What do we need to know? J. Clin. Child Adolesc. Psychol. 53, 761–767.
Rumberger, R. W., and Thomas, S. L. (2000). The distribution of dropout and turnover rates among urban and suburban high schools. Sociol. Educ. 73, 39–67.
Sauceda, J. M. (1994). Normalidad y psicopatología en la adolescencia. Rev. Mex. Pediatría 61, 153–157.
Shaffer, D., Restifo, K., Garfinkel, R., Wilcox, H., Ehrensaft, M., and Munfakh, J. (1998). Screening for Young-Adult Suicidality and Mood Disorders in High School. Anaheim, CA: AACAP.
SSA. (2001). “Programa de accion en salud mental,” in Diagnostico Epidemiologico, ed. Secretaria de Salud Mexico (Mexico), 29–51.
Suarez, A. (1999). Diseño y determinacion de la estructura factorial de la Escala Dimensional de Psicopatología para Adolescentes (EDPA). UNAM: Mexico.
Tavares, B. F., Béria, J. U., and Silva de Lima, M. (2001). Drug use prevalence and school performance among adolescents. Rev. Saúde Pública 35, 150–158.
Keywords: student dropout, child psychiatry, Mexico
Citation: Chalita PJ, Palacios L, Cortes JF, Landeros-Weisenberger A, Panza KE and Bloch MH (2012) Relationship of dropout and psychopathology in a high school sample in Mexico. Front. Psychiatry 3:20. doi: 10.3389/fpsyt.2012.00020
Received: 27 September 2011; Accepted: 25 February 2012;
Published online: 13 March 2012.
Edited by:
Boris Lorberg, University of Massachusetts School of Medicine, USAReviewed by:
Lynsay Ayer, University of Vermont, USAConstance Moore, University of Massachusetts Medical School, USA
Copyright: © 2012 Chalita, Palacios, Cortes, Landeros-Weisenberger, Panza and Bloch. This is an open-access article distributed under the terms of the Creative Commons Attribution Non Commercial License, which permits non-commercial use, distribution, and reproduction in other forums, provided the original authors and source are credited.
*Correspondence: Pablo J. Chalita, Instituto Nacional de Psiquiatría “Ramón de la Fuente Muñíz”, Calzada México Xochimilco Num. 101, Col. San Lorenzo Huipulco, Tlalpan, C.P. 14370 Distrito Federal, Mexico. e-mail: pchalita@gmail.com