- 1Department of Health Promotion and Community Health Sciences, Texas A&M Health Science Center School of Public Health, College Station, TX, USA
- 2Department of Health Promotion and Behavior, The University of Georgia College of Public Health, Athens, GA, USA
- 3National Center for Injury Prevention and Control, Centers for Disease Control and Prevention, Atlanta, GA, USA
- 4Department of Epidemiology and Biostatistics, Texas A&M Health Science Center School of Public Health, College Station, TX, USA
- 5Department of Statistics, Texas A&M University, College Station, TX, USA
Tai Chi: Moving for Better Balance (TCMBB) is an evidence-based fall prevention exercise program being disseminated in selected communities through state injury prevention programs. This study: (1) describes the personal characteristics of TCMBB participants; (2) quantifies participants’ functional and self-reported health status at enrollment; and (3) measures changes in participants’ functional and self-reported health status post-intervention. There were 421 participants enrolled in 36 TCMBB programs delivered in Colorado, New York, and Oregon. Of the 209 participants who completed both baseline enrollment and post-intervention surveys, the average age of participants was 75.3 (SD ± 8.2) years. Most participants were female (81.3%), non-Hispanic (96.1%), White (94.1%), and described themselves as in excellent or very good health (52.2%). Paired t-test and general estimating equation models assessed changes over the 3-month program period. Pre- and post-assessment self-reported surveys and objective functional data [Timed Up and Go (TUG) test] were collected. On average, TUG test scores decreased (p < 0.001) for all participants; however, the decrease was most noticeable among high-risk participants (mean decreased from 18.5 to 15.7 s). The adjusted odds ratio of reporting feeling confident that a participant could keep themselves from falling was five times greater after completing the program. TCMBB, which addresses gait and balance problems, can be an effective way to reduce falls among the older adult population. By helping older adults maintain their functional abilities, TCMBB can help community-dwelling older adults continue to live independently.
Introduction
Tai Chi is a Chinese form of exercise that uses slow, flowing body movements. It had been practiced for centuries in Asia before being introduced to the United States in the early twentieth century (1). The physical and mental health benefits of Tai Chi are well documented (2–4), and in the 1990s, Tai Chi was rigorously tested by the National Institute on Aging as a fall prevention intervention (5, 6). A Cochrane review and meta-analysis concluded that Tai Chi reduced the risk of falling 28%, with greater effectiveness among those with lower initial fall risk (7). Today Tai Chi is widely recognized as an effective fall intervention (8–10).
The Tai Chi: Moving for Better Balance (TCMBB) program is an evidence-based fall prevention exercise program that was developed by researchers at the Oregon Research Institute with partial funding from the Centers for Disease Control and Prevention (CDC). The original 26-week intervention used 24 Tai Chi forms or sequences of controlled movements, and it was shown in a randomized controlled trial to be effective in reducing falls (11, 12). TCMBB consists of eight forms that progress from easy to difficult to improve older adults’ postural stability, balance, and coordination (13). Classes consist of 10–15 participants led by a trained instructor. One-hour classes are held twice a week for 12 weeks (24 total classes) (13). Feasibility testing has demonstrated that this program is well accepted by older adults and can be implemented with fidelity in community settings (14, 15).
In 2011, the CDC launched a 5-year project to implement TCMBB in selected communities in Oregon, Colorado, and New York. This was part of a larger project to reduce falls and fall-related injuries by engaging fall prevention coalitions, healthcare organizations, and other partners to integrate clinical and evidence-based community fall prevention programs in selected communities (16). TCMBB is intended for relatively healthy older adults with few functional limitations.
This study describes the results of implementing TCMBB during the first 2 years of the project. The purposes of the study were to: (1) describe the personal characteristics of TCMBB participants; (2) quantify participants’ functional and self-reported health status at enrollment; and (3) measure changes in participants’ functional and self-reported health status after completing the program.
Materials and Methods
TCMBB Implementation
The three states offered TCMBB in a variety of settings including YMCAs, healthcare organizations, residential facilities, faith-based organizations, recreational facilities, and senior centers. State grantees hosted 30 TCMBB trainings from 2011 to 2013 at which Master Trainers from the Oregon Research Institute trained 400 instructors. In addition, the YMCA of the USA (Y-USA) engaged the Oregon Research Institute to train 10 YMCA faculty trainers to be TCMBB instructors.
The target audience for TCMBB is community-dwelling older adults aged 60 and older who can walk easily with or without assistive devices. In each state, participants were recruited by staff at member organizations, through family and friends, and through advertisements aimed at older adults. Methods of recruitment and referral varied across states and were based on existing partnerships. For example, Colorado and New York were most likely to recruit at YMCAs whereas Oregon recruited through senior centers and health care organizations since there were no YMCAs in their service delivery areas. As a program implemented through existing traditional community settings, there were limited exclusionary criteria and medical clearance was not required for participation. While no age restrictions were placed on enrollment, our analyses were restricted to people aged 60 years and older to reflect the study target population.
Data Collection
Data for this project were collected from multiple sources. Attendance was obtained from attendance logs collected at each class. A 20-question self-administered survey was used to collect pre- and post-TCMBB program data. The first was administered at the initial TCMBB class (enrollment or baseline survey) and the second at the final class (course completion or post-intervention survey). The surveys took approximately 15 minutes to complete and assistance was provided to participants who needed help filling out the forms. Questions included socio-demographic characteristics (e.g., age, sex, race, and ethnicity), whether the participant had been referred to the program by a healthcare provider, self-reported health status (excellent, very good, good, fair, or poor), satisfaction with their current activity levels (very, mostly, somewhat, or not at all satisfied), and confidence in their ability to keep themselves from falling (four-point scale ranging from strongly agree to strongly disagree). Self-reported functional ability was assessed by the reported level of difficulty in performing various activities (e.g., climbing one flight of stairs) on a four-point scale ranging from no difficulty (scored 1) to unable to do (scored 4) (17). Class completion was defined as attending at least 70% of the classes (i.e., 17 out of 24 classes).
The Timed Up and Go (TUG) test was used to measure functional status at enrollment and completion. This test has been widely used to assess functional mobility and predict fall risk and has been validated among community-dwelling older adults (18–20). The test measures the time in seconds required for participants to “rise from a standard arm chair, walk at [their] typical or normal pace to a line on the floor 3 meters away, turn, return, and sit down again” (21). Participants who completed the TUG in <12 seconds were classified as low risk and those who took 12 or more seconds were classified as high risk (22).
Statistical Analyses
Baseline characteristics (demographic characteristics, class attendance, and TUG results) were compared for those who completed both the baseline and post-intervention questionnaires to those who completed only the baseline questionnaire using chi-square tests to identify potential biases from loss to follow-up. Changes in TUG test times between baseline and post-intervention were compared using two-tailed paired t-tests; results were examined for all participants combined and stratified by baseline risk level. General estimating equations (GEE) models using a logit link function were used to compare differences in self-reported functional and health status at baseline and post-intervention; models were run using SAS version 9.3 GENMOD procedure (SAS Institute Inc., Cary, NC, USA) and adjusted for gender, age, race, and state. GEE models are longitudinal data models that use all available data in model estimation (i.e., do not require paired data) and can account for the correlation among repeated measures from the same participant (23).
The Texas A&M University Institutional Review Board granted approval to analyze data on program participants and outcomes collected using survey instruments and functional assessments.
Results
Participant Characteristics and Course Attendance
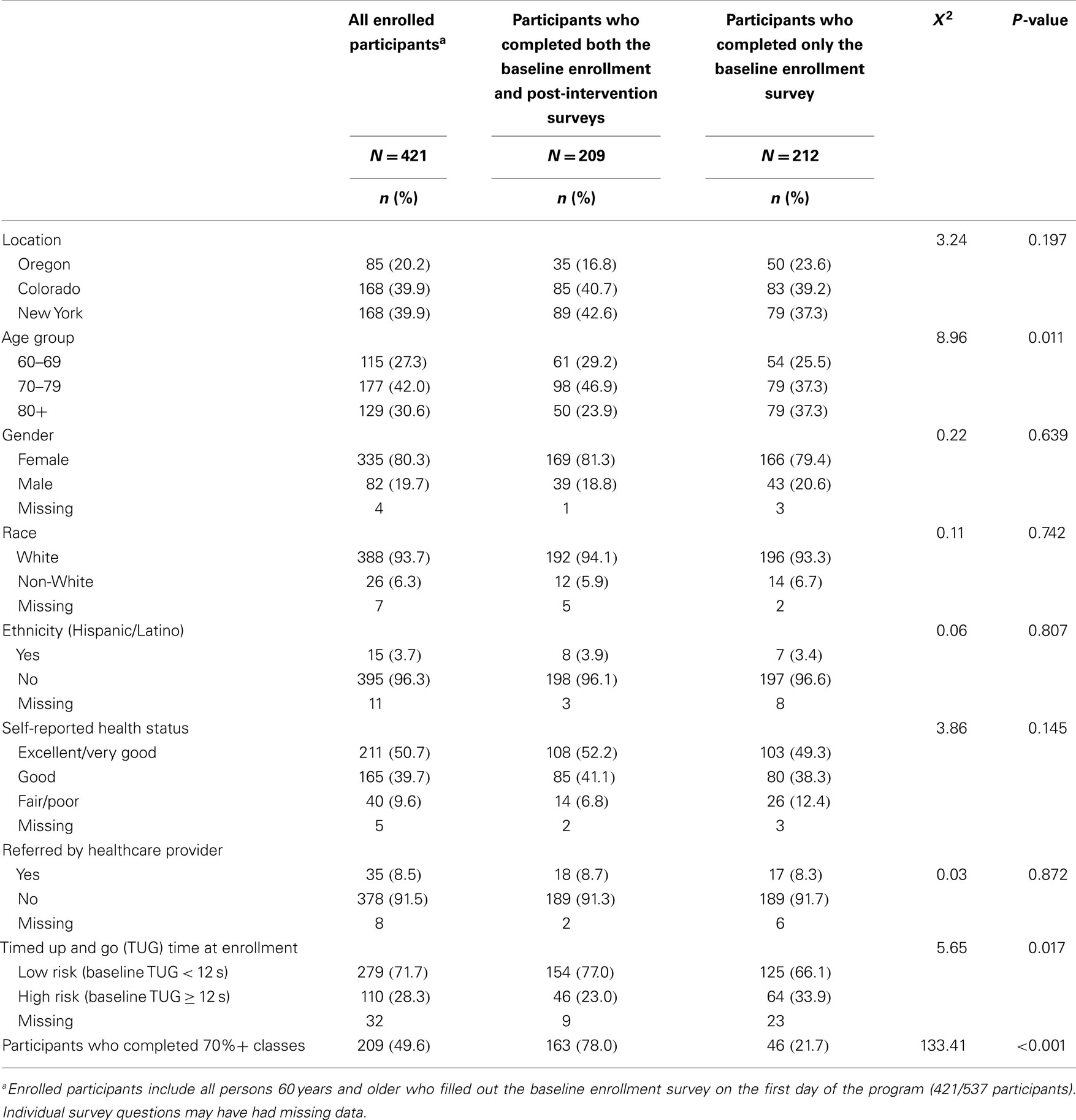
Between September 1, 2011 and December 31, 2013, the three states offered 36 TCMBB programs and enrolled 537 people aged 60 and older. Of these enrollees, baseline data were collected from 421 (78.4%); 20.2% of participants were in Oregon, 39.9% in Colorado, and 39.9% in New York (Table 1). Of the 421 participants who provided a baseline questionnaire, 209 also completed a post-intervention questionnaire (Table 1).
The average age of participants was 75.3 (SD ± 8.2) years. Most participants were female, non-Hispanic, and White. About half of the participants attended at least 70% of classes (17 out of 24), with participants attending on average 13.6 (SD ± 8.0) of the 24 possible classes. Only 16 participants (8.5%) reported they were referred to TCMBB by a healthcare provider.
The 212 participants who “dropped out” or were lost to follow-up were not significantly different from those who completed the program in terms of gender, race, ethnicity, self-reported health status, or provider referral to class. However, dropouts were significantly older (average age 76.1 vs. 74.1) and more likely to have been classified as high risk based their TUG time at baseline.
Participant Functional Performance
Of 421 participants with baseline data, 199 (47.3%) completed the TUG test at both baseline and post-intervention (Table 2). Of these, 45 (22.6%) were categorized as high risk. After completing TCMBB, the proportion of participants categorized as high risk decreased significantly to 14% (n = 28; data not shown). On average, TUG test scores decreased significantly for all participants but the change was most evident among high risk participants where the average TUG time decreased from 18.5 to 15.7 seconds.
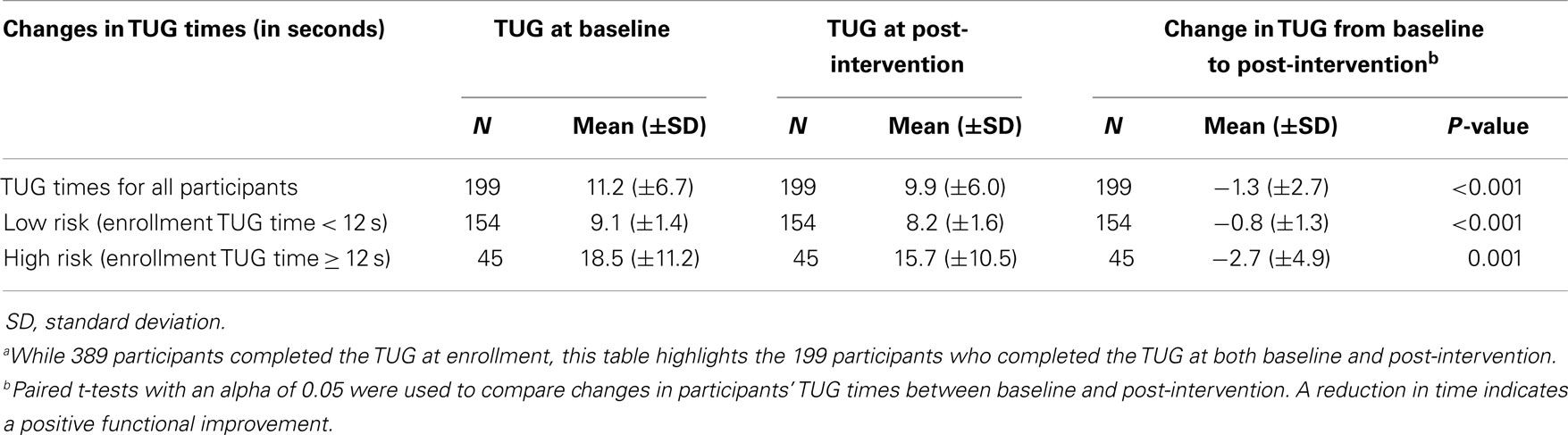
Table 2. Changes in Tai Chi: Moving for Better Balance (TCMBB) participants’ timed up and go (TUG) times from baseline enrollment to post-interventiona.
Self-Reported Outcome Improvements
Table 3 compares self-reported outcome measures at baseline and post-intervention. Results are presented as percentages and as odds ratios adjusted for gender, age, race, and state. Significant improvements from baseline to post-intervention were observed for all outcomes except self-reported difficulty in walking across the room.
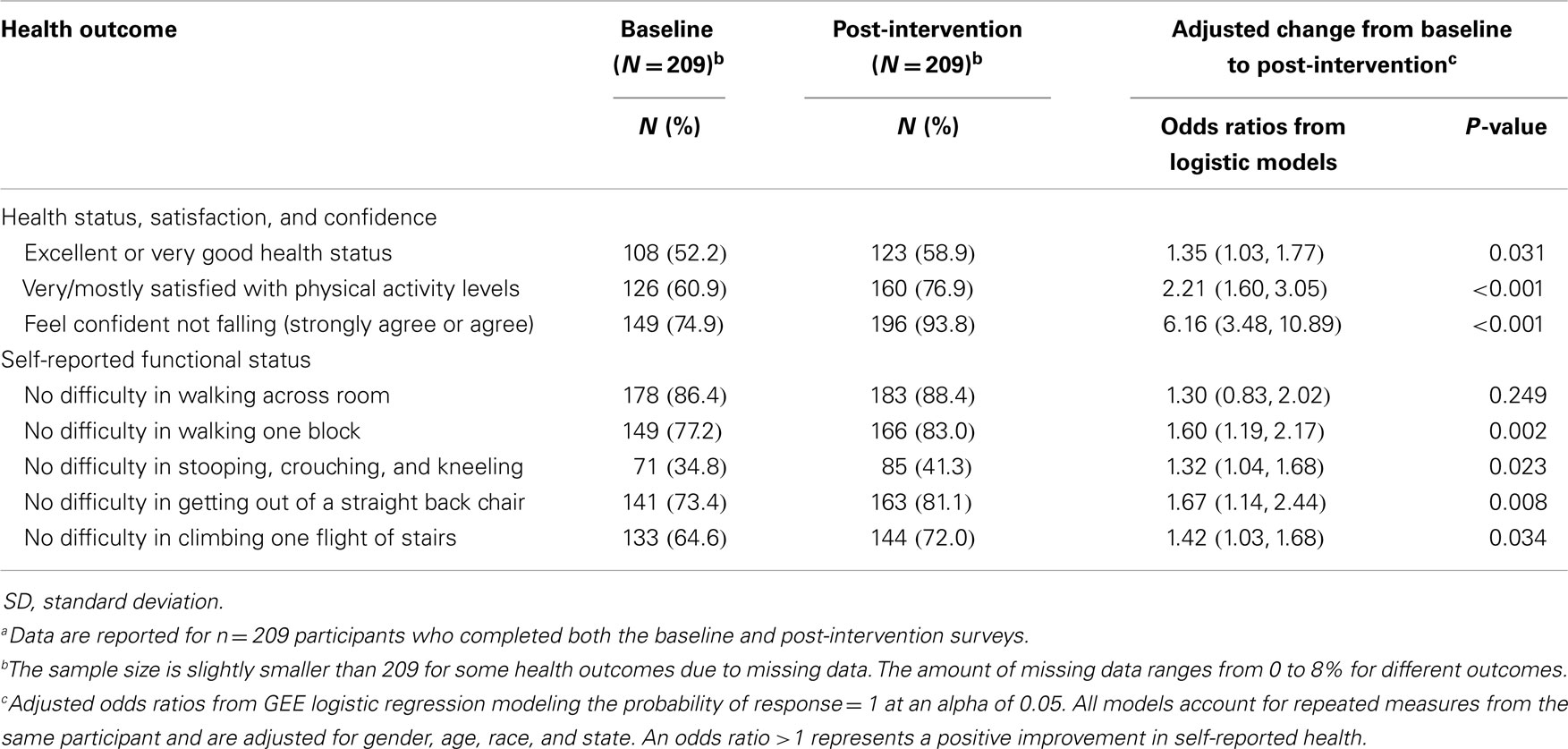
Table 3. Changes in Tai Chi: Moving for Better Balance (TCMBB) participants’ self-reported health and functional outcomes from baseline to post-interventiona.
The GEE model results showed that the adjusted odds ratio (aOR) of reporting excellent or very good health status increased by 35% (aOR = 1.35, 95% CI 1.03–1.77). The odds of being very or mostly satisfied with physical activity levels also increased significantly (aOR = 2.21, 95% CI 1.60–3.05). The odds of feeling confident that a participant could keep themselves from falling was five times greater after completing TCMBB (aOR = 6.16 95% CI 3.48–10.89).
Among the five items assessing functional status, the aORs for participants who reported “no difficulty” significantly increased for walking one block (aOR = 1.60, 95% CI 1.19–2.17); stooping, crouching, kneeling (aOR = 1.32, 95% CI 1.04–1.68); getting out of a straight back chair (aOR = 1.67, 95% CI 1.14–2.44); and climbing one flight of stairs (aOR = 1.42, 95% CI 1.03–1.68). About 86% of participants reported no difficulty walking across the room at baseline, and this proportion did not increase significantly at post-intervention.
Discussion
This study examined 2 years of evaluation data collected from older adults age 60+ who participated in TCMBB programs offered in selected communities across three states. Comparing data collected at enrollment and course completion, TCMBB was associated with significant improvements in self-reported health status, satisfaction with physical activity levels, fall-related confidence, ability to perform basic functional tasks (e.g., walking one block, climbing a flight of stairs), and in the TUG test. Similar positive results have been seen in earlier studies of Tai Chi (14, 24), and provide additional evidence that Tai Chi is a useful fall prevention program for older adults.
Recruitment of participants is a concern for most fall prevention programs. While the distribution of TCMBB participants’ race and ethnicity was similar to the populations from which they were recruited, the percentage of male participants was low. Retaining TCMBB participants was also challenging. Participants attended on average 57% of the 24 classes. While it was not possible in this study to monitor falls, those who did not attend regularly may not have received an adequate intervention dose for reducing their fall risk. The reasons for low attendance are unknown. However, anecdotal reports from the state health departments implementing TCMBB suggest that some older adults may have considered the Tai Chi program a “drop-in” activity instead of an ongoing program. Those who did not complete the course were somewhat older and took longer to complete the TUG at enrollment, which suggests that health issues may have contributed to their not finishing the program.
Barriers to the success of TCMBB, as for other community-based fall prevention programs, include maintaining regular attendance and encouraging participants to continue activities after the program ends. Although the participants in this study demonstrated positive outcomes, one 12-week program is unlikely to provide long-term benefits without booster classes. Tai Chi, like other strength and balance exercises, is most effective when it is practiced for 50 hours or more (11). Therefore, older adults would benefit from having an ongoing Tai Chi program in their community, if they attended regularly. Some participating sites are now offering an introductory 12-week TCMBB followed by an ongoing program.
Another challenge has been the limited availability of community Tai Chi classes. State health departments have been able to address this by developing public–private partnerships with organizations that have existing infrastructure to offer classes to older adults. For example, the Y-USA now endorses a modified version of TCMBB called Y-Moving for Better Balance (Y-MFBB) that is being offered in local YMCAs (25). State health departments are also beginning to implement and support other Tai Chi programs (e.g., Tai Chi for Arthritis) that have been shown to be effective for fall prevention (26).
Ideally all older adults would have access to a wide range of evidence-based fall prevention programs that could meet their varied needs. Thus, in the larger fall prevention project, TCMBB was offered along with Stepping On (27) and Otago (28), which are designed for older adults with some functional limitations who are at moderate and high fall risk, respectively. As the availability of Tai Chi and other fall prevention programs expands, it will be important to ensure that fidelity to the key elements of the original interventions is maintained so that the programs remain effective in preventing falls.
Limitations
This study has number of limitations. First, sampling and dropout issues limit the generalizability of the results. Participants were self-selected from participating communities and may not be representative of the older adult population either in those communities or in the participating states. Program effectiveness was based on comparing assessments from participants who attended both the first and last class. These participants were slightly younger and had fewer functional limitations, as measured by better TUG times at baseline, compared to participants who were not available for the post-intervention assessment. However, because the results are for those who provided both baseline enrollment and post-intervention assessments, we can be confident we are comparing the same population before and after the intervention. We did not take into account differences in total attendance among people who provided baseline and post-intervention assessments, so the effectiveness of the full intervention may be underestimated.
Second, the program was delivered in a multitude of settings, and outcomes may have been influenced by variability in instructor and site. Although all instructors were certified trained instructors, we recommend more attention be given to treatment fidelity monitoring in future research and practice. The CDC Guide for Program Implementation (13) has examples of a class observation form for monitoring instructor adherence to core program elements.
Third, in order to limit the reporting burden on the program delivery personnel, we used a limited number of self-reported outcomes and one timed functional assessment (i.e., the TUG). Although there was training provided for conducting the TUG, including available step-by-step online videos, this training was limited. Therefore, results may not be comparable to standardized TUG tests administered by trained professionals. Finally, while TCMBB participants reported improved functional status and demonstrated better TUG scores, we do not know if this led to a reduction in falls, since falls were not monitored during or after the program.
Conclusion
Tai Chi: Moving for Better Balance, which addresses gait and balance problems, can be an effective way to reduce falls among the older adult population. Various forms of Tai Chi have been shown to be most appropriate for younger and healthier older adults who are at relatively low risk of falling. By helping older adults maintain their functional abilities, TCMBB can help community-dwelling older adults continue to live independently.
In this study, TCMBB participants reported positive effects on their functional and health status. However, the high dropout rates among program participants highlight a major challenge to implementing effective community-based fall prevention programs. Community-based programs are a promising approach for older adult fall prevention, but there are ongoing challenges to ensuring that high quality programs are available for – and attended by – older adults who can benefit from such programs.
Conflict of Interest Statement
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
This paper is included in the Research Topic, “Evidence-Based Programming for Older Adults.” This Research Topic received partial funding from multiple government and private organizations/agencies; however, the views, findings, and conclusions in these articles are those of the authors and do not necessarily represent the official position of these organizations/agencies. All papers published in the Research Topic received peer review from members of the Frontiers in Public Health (Public Health Education and Promotion section) panel of Review Editors. Because this Research Topic represents work closely associated with a nationwide evidence-based movement in the US, many of the authors and/or Review Editors may have worked together previously in some fashion. Review Editors were purposively selected based on their expertise with evaluation and/or evidence-based programming for older adults. Review Editors were independent of named authors on any given article published in this volume.
Acknowledgments
We thank the Colorado, New York, and Oregon State Injury Prevention Centers for coordinating Tai Chi: Moving for Better Balance, a Community-Based Older Adult Fall Prevention Program and collecting the study data and Margaret Kaniewski with the Centers for Disease Control and Prevention for her programmatic support and critical review of the manuscript. Funding Source: This research was supported in part by the Centers for Disease Control and Prevention, Prevention Research Centers Special Initiative Project funding for the State Fall Prevention Program under 5U48DP001924, and the Research Participation Program at the Centers for Disease Control and Prevention administered by the Oak Ridge Institute for Science and Education through an interagency agreement between the U.S. Department of Energy and CDC.
References
1. National Center for Complementary and Alternative Medicine (NCCAM). Tai Chi: An Introduction. National Institute of Health (2010) [cited 2014 Aug 11]. Available from: http://nccam.nih.gov/health/taichi/introduction.htm#overview
2. Leung DP, Chan CK, Tsang HW, Tsang WW, Jones AY. Tai chi as an intervention to improve balance and reduce falls in older adults: a systematic and meta-analytical review. Altern Ther Health Med (2011) 17(1):40–8.
3. Lee MS, Ernst E. Systematic reviews of t’ai chi: an overview. Br J Sports Med (2012) 46(10):713–8. doi: 10.1136/bjsm.2010.080622
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
5. Ory MG, Schechtman KB, Miller JP, Hadley EC, Fiatarone MA, Province MA, et al. Frailty and injuries in later life: the FICSIT trials. J Am Geriatr Soc (1993) 41(3):283–96.
6. Province MA, Hadley EC, Hornbrook MC, Lipsitz LA, Miller JP, Mulrow CD, et al. The effects of exercise on falls in elderly patients. A preplanned meta-analysis of the FICSIT trials. Frailty and injuries: cooperative studies of intervention techniques. JAMA (1995) 273(17):1341–7. doi:10.1001/jama.273.17.1341
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
7. Cameron ID, Murray GR, Gillespie LD, Robertson MC, Hill KD, Cumming RG, et al. Interventions for preventing falls in older people in nursing care facilities and hospitals. Cochrane Database Syst Rev (2010) 20(1):CD005465. doi:10.1002/14651858.CD005465.pub2
8. Michael YL, Whitlock EP, Lin JS, Fu R, O’Connor EA, Gold R, et al. Primary care-relevant interventions to prevent falling in older adults: a systematic evidence review for the U.S. preventive services task force. Ann Intern Med (2010) 153(12):815–25. doi:10.7326/0003-4819-153-12-201012210-00008
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
9. Stevens JA. A CDC Compendium of Effective Fall Interventions: What Works for Community-Dwelling Older Adults. Atlanta, GA: Centers for Disease Control and Prevention. National Center for Injury Prevention and Control. Division of Unintentional Injury Prevention (2010).
10. National Council on Aging. Falls Free: Promoting a National Falls Preventions Action Plan (2005) [cited 2014 Aug 11]:[1-51 p.]. Available from: http://www.ncoa.org/improve-health/center-for-healthy-aging/content-library/FallsFree_NationalActionPlan_Final.pdf
11. Sherrington C, Tiedemann A, Fairhall N, Close JCT, Lord S. Exercise to prevent falls in older adults: an updated meta-analysis and best practice recommendations. N S W Public Health Bull (2011) 22(3–4):78–83. doi:10.1071/NB10056
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
12. Li F, Harmer P, McAuley E, Duncan TE, Duncan SC, Chaumeton N, et al. An evaluation of the effects of Tai Chi exercise on physical function among older persons: a randomized controlled trial. Ann Behav Med (2001) 23(2):139–46. doi:10.1207/S15324796ABM2302_9
13. National Center for Injury Prevention and Control. Tai chi: Moving for Better Balance A guide for program Implementation (2011) [cited 2014 Aug 6]:[1-146 p.]. Available from: http://api.ning.com/files/lpWX79eu*NgqhrxYqum3lrPOm6Dp4GRQCK9J1qwtJylSBPaJ2W38NVNJNcBqszLkRplWB9ee-lwV4PIN-hUoPujtn*zU9vRw/TCManual_Compiled__v19.pdf
14. Li F, Harmer P, Glasgow R, Mack KA, Sleet D, Fisher KJ, et al. Translation of an effective tai chi intervention into a community-based falls-prevention program. Am J Public Health (2008) 98(7):1195–8. doi:10.2105/AJPH.2007.120402
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
15. Li F, Harmer P, Mack KA, Sleet D, Fisher KJ, Kohn MA, et al. Tai Chi: moving for better balance – development of a community-based falls prevention program. J Phys Act Health (2008) 5(3):445–55.
16. Kaniewski M, Stevens JA, Parker EM, Lee R. An introduction to the Centers for Disease Control and Prevention’s efforts to prevent older adult falls. Front Public Health (2015) 2:119. doi:10.3389/fpubh.2014.00119
17. Wallace RB, Herzog AR. Overview of the health measures in the health and retirement study. J Hum Resour (1995) 30:S84–107. doi:10.2307/146279
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
18. Bohannon RW. Reference values for the timed up and go test: a descriptive meta-analysis. J Geriatr Phys Ther (2006) 29(2):64–8. doi:10.1519/00139143-200608000-00004
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
19. Hutton I, Gamble G, McLean G, Butcher H, Gow P, Dalbeth N. Obstacles to action in arthritis: a community case-control study. Int J Rheum Dis (2009) 12(2):107–17. doi:10.1111/j.1756-185X.2009.01392.x
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
20. Shumway-Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community-dwelling older adults using the timed up & go test. Phys Ther (2000) 80(9):896–903.
21. Podsiadlo D, Richardson S. The timed “up & go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc (1991) 39(2):142–8.
22. Bischoff HA, Stahelin HB, Monsch AU, Iversen MD, Weyh A, von Dechend M, et al. Identifying a cut-off point for normal mobility: a comparison of the timed ‘up and go’ test in community-dwelling and institutionalised elderly women. Age Ageing (2003) 32(3):315–20. doi:10.1093/ageing/32.3.315
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
23. Hardin JW. Generalized Estimating Equations (GEE). Encyclopedia of Statistics in Behavioral Science. Hoboken, NJ: John Wiley & Sons, Ltd. (2005). doi:10.1002/0470013192.bsa250
24. Rogers CE, Larkey LK, Keller C. A review of clinical trials of tai chi and qigong in older adults. West J Nurs Res (2009) 31(2):245–79. doi:10.1177/0193945908327529
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
25. Ehrenreich H, Pike M, Hohman K, Kaniewski M, Longjohn M, Myers G, et al. CDC and YMCA: a promising partnership for delivering fall prevention programming. Front Public Health (2015) 2:235. doi:10.3389/fpubh.2014.00235
26. Stevens JA, Voukelatos A, Ehrenreich H. Preventing falls with Tai Ji Quan: a public health perspective. J Sport Health Sci (2014) 3(1):21–6. doi:10.1016/j.jshs.2013.10.002
27. Ory MG, Smith ML, Jiang L, Lee R, Chen S, Wilson AD, et al. Fall prevention in community settings: results from implementing Stepping On in three states. Front Public Health (2015) 2:232. doi:10.3389/fpubh.2014.00232
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
Keywords: Tai Chi: Moving for Better Balance, fall prevention, fall prevention program, community setting, older adults
Citation: Ory MG, Smith ML, Parker EM, Jiang L, Chen S, Wilson AD, Stevens JA, Ehrenreich H and Lee R (2015) Fall prevention in community settings: results from implementing Tai Chi: Moving for Better Balance in three states. Front. Public Health 2:258. doi: 10.3389/fpubh.2014.00258
Received: 27 August 2014; Paper pending published: 19 October 2014;
Accepted: 10 November 2014; Published online: 27 April 2015.
Edited by:
Michal Grivna, United Arab Emirates University, United Arab EmiratesReviewed by:
Milka Dančević-Gojković, Public Health Institute of Federation of Bosnia and Herzegovina, Bosnia and HerzegovinaPankaja Desai, University of Illinois at Chicago, USA
Copyright: © 2015 Ory, Smith, Parker, Jiang, Chen, Wilson, Stevens, Ehrenreich and Lee. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Marcia G. Ory, Department of Health Promotion and Community Health Sciences, Texas A&M Health Science Center, 1266, College Station, TX 77843–1266, USA e-mail: mory@srph.tamhsc.edu
 Marcia G. Ory
Marcia G. Ory Matthew Lee Smith
Matthew Lee Smith Erin M. Parker
Erin M. Parker Luohua Jiang
Luohua Jiang Shuai Chen
Shuai Chen Ashley D. Wilson1
Ashley D. Wilson1 Judy A. Stevens
Judy A. Stevens Heidi Ehrenreich
Heidi Ehrenreich Robin Lee
Robin Lee