Efficiency of the Lausanne clinical pathway for proximal femoral fractures
- Centre Hospitalier Universitaire Vaudois (CHUV) and University of Lausanne, Lausanne, Switzerland
Purpose/Introduction: The number of hip fractures is rising, due to increases in life expectancy. In such cases, patients are at risk from post-operative complications and subsequently the average length of hospitalization may be extended. In 2011, we established a clinical pathway (CP), a specific model of care for patient-care management, to improve the clinical and economic outcomes of proximal femoral fracture management in elderly patients. The goal was to evaluate the CP using clinical, process, and financial indicators.
Methods: We included all surgical patients aged 65 and over, admitted to the emergency department with a fracture of the proximal femur following a fall. Assessment parameters included three performance indicators: clinical, process, and financial. The clinical indicators were the presence or absence of acute delirium on the third post-operative day, diagnosis of nosocomial pneumonia, and the number of patients fulfilling at least 75% of their nutritional requirements at the end of the hospitalization period. The process indicator was the time interval between arrival at the emergency department and surgery. The financial indicator was based on the number of days spent in hospital.
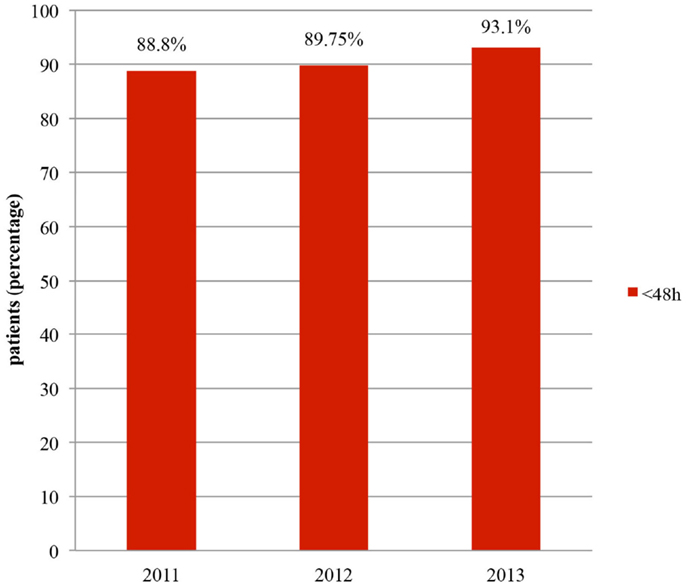
Results: From 2011 to 2013, 669 patients were included in the CP. We observed that the average length of stay in hospital decreased as soon as the CP was implemented and stabilized afterwards. The goal of 90% of patients undergoing surgery within 48 h of arrival in the emergency department was surpassed in 2013 (93.1%). Furthermore, we observed an improvement in the clinical indicators.
Conclusion: The application of a CP allowed an improvement in the qualitative and quantitative efficiency of proximal femoral fracture management in elderly patients, in terms of clinical, process, and financial factors.
Introduction
Due to the increase in life expectancy, and the rise in the average age of the population, the number of hip fractures is still growing. According to Gullberg, the projected annual incidence of hip fractures, world-wide, will rise from 1.26 million in 1990 to 2.6 million by the year 2025 and to 4.5 million by 2050 (1). In our university hospital, over 200 patients annually, present with fractures of the proximal part of the femur, which require extended mean periods of hospitalization, subsequently resulting in elevated medical costs. Many of these patients suffer from undernutrition (2) and post-operative delirium (3), which can lead to post-operative complications, institutionalization, or death. Also, it was found that an operative delay of 2 days and more, after hospital admission, was associated with increased mortality (4). With early detection and treatment, post-operative morbidity and mortality rates could be reduced. Traditionally, clinicians looking after patients work individually, and not necessarily in a coordinated manner. Taking into consideration these different points, a clinical pathway (CP) was established in 2011, to improve the qualitative and quantitative efficiency of proximal femoral fracture management in elderly patients (5). Some publications (6–8) show encouraging results using various CP programs. This CP, founded on evidence-based medicine guidelines, proposed to establish a system of patient-care management, for a specific patient population, involving a multidisciplinary team (9).This created interdisciplinary associations between emergency physicians, surgeons, nurses, unit management, responsible for the flow of patients through the system, physiotherapists, geriatricians, specialists in osteoporosis, and nutritionists. We evaluated this proximal femoral fracture CP, using clinical, process, and financial indicators.
Materials and Methods
Patients Demographics
In the first instance, we included all surgical patients aged 65 and over, admitted to the emergency department with a fracture of the proximal femur following a fall. From 01.03.2011 to 31.12.2013, 669 patients were included. The men age of the cohort was 83.8 years in 2011, 83.7 years in 2012, and 82.9 years in 2013, of which 148 were men (22.1%) and 521 were women (77.9%).
Inclusion and Exclusion Criteria
We excluded patients with periprosthetic fractures and pathological fractures and all polytrauma cases. Any patient that remained in the intensive care unit post-inclusion in the CP or was transferred to another unit for more than 2 days was excluded.
Flowchart
Initially, anterior–posterior pelvic and axial view radiographs of the proximal femoral fractures were performed, and were followed, when necessary, by a CT scan. MRI was only used in cases without a definitive diagnosis (Figure 1). Patients had a complete blood count, and TP, PTT, Na+, K+, glycemia, creatinine, eGFR, CK, albumin, blood group, phosphorus, magnesium, and corrected calcium blood tests, followed by a geriatric consultation in order to detect, treat, or prevent delirium incidences, where necessary. A second geriatric consultation, intended to identify and prevent various accident risk factors, was organized, to assess cognitive impairment, review medication in particular psychotropic drugs, advise on the use of walking aids, and make recommendations for the general practitioner.
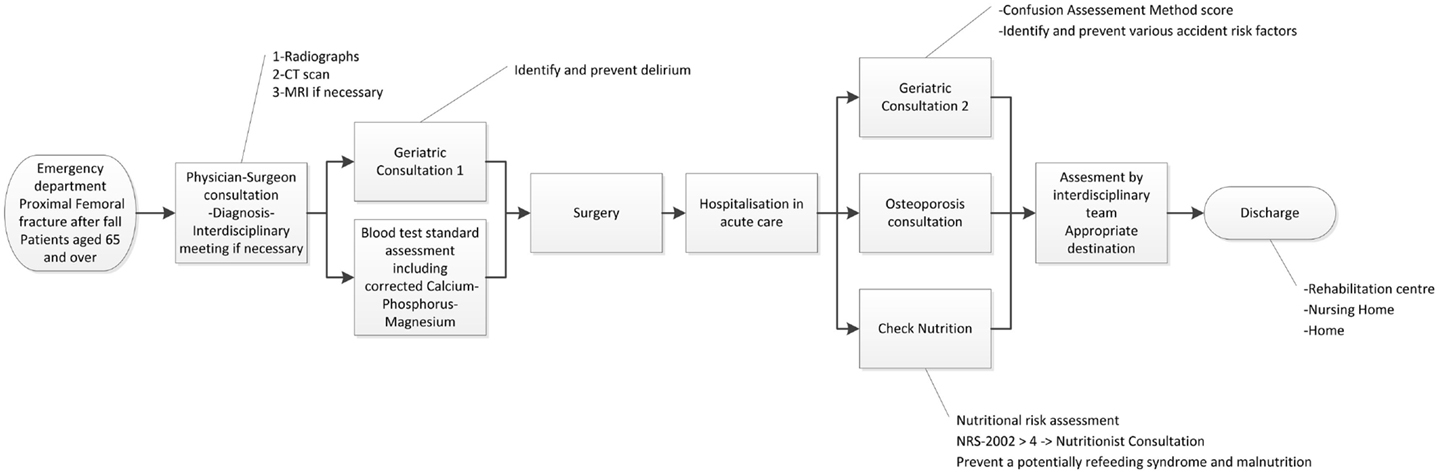
Figure 1. Flowchart: clinical pathway for surgical patients aged 65 and over with a proximal femoral fracture following a fall.
The patient was transferred directly to the operating room or to the orthopedic unit pending an intervention. After surgery, each patient was monitored daily, to identify, treat, and prevent any incidences of delirium. Nutritional risk assessments were performed using the NRS-2002 method (10) on the first post-operative day and repeated weekly. Patients with an NRS-2002 ≥4 were assessed by a nutritionist in order to define nutritional requirements, to treat malnutrition, and to prevent a potentially refeeding syndrome (2).
Within 24–48 h after surgery, patients had a bedside osteoporosis consultation, in order to identify cases of osteoporotic disease and develop appropriate treatments.
During hospitalization, depending on the functional, medical, and social statuses of each patient, the appropriate destination after acute care was assessed by the interdisciplinary team. Patients could be directed to a rehabilitation center, their own homes, or a nursing home following a few days of acute rehabilitation.
Indicators
In terms of assessment parameters, the first clinical indicator chosen was a positive delirium diagnosis on the third post-operative day (yes/no) based on the confusion assessment method score (CAM) (11). The presence of a nosocomial pneumonia (yes/no), the second clinical indicator, was defined by a positive AP chest radiograph or CT and antibiotherapy. The third clinical indicator was the rate of patients fulfilling at least 75% of their nutritional requirements at the end of the stay, which was calculated by monitoring food intake and oral nutritional supplement consumption. The process indicator chosen was the time interval between hospital admission and surgery (hours) and the financial indicator was based on the costs related to the number of days spent in hospital (days).
Statistical Analysis
Parametric tests and non-parametric tests were used for comparison of length of stay (LOS) (Student, Wilcoxon, Trend tests). The chi-squared test was used for dichotomous variables. Descriptive analysis was completed when data were not available before the onset of the CP.
Results
Patients
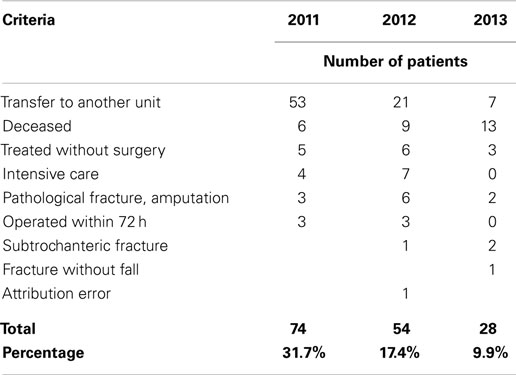
From March to December 2011, 233 patients were considered suitable for initial inclusion in this CP. One hundred fifty-nine patients completed their entire hospital stay within the CP. The main reasons for exclusion were a transfer to another department where the CP was not implemented, death, conservative treatments, pathological fractures, and cases where the time interval between emergency admission and surgery exceeded 72 h (details in Table 1). In 2011, the rate of exclusion was 31.7%. In view of these figures, it was decided to open the CP across more units (01.05.2012) and to include cases with hospital admission to surgery time intervals of more than 72 h. The exclusion rate dropped to 17.4% in 2012. In 2012, 310 patients were initially included in this CP after emergency unit admission, 256 of whom remained in the CP for their entire hospital stay. In 2013, we definitively included 254 patients in this CP with a lower exclusion rate of 9.9%. From 01.03.11 to 31.12.13, the application of these criteria yielded an ultimate total of 669 patients who had followed this CP.
Clinical Indicators
The first clinical indicator was the prevalence of delirium on the third post-operative day (D3). In 2012, 83.6% of patients were evaluated, 16.3% of whom were found to have a positive CAM at D3. In 2013, 56% of patients were evaluated at D3 and 12.7% of these patients had delirium. The second clinical indicator, the rate of occurrence of pneumonia remained stable at 3.14 and 3.12% for the first 2 years and then decreased to 2.75% in 2013.The third clinical indicator, the proportion of patients fulfilling at least 75% of their nutritional needs at the end of the hospitalization period, increased from 37 to 60% between 2011 and 2013.
Process Indicators
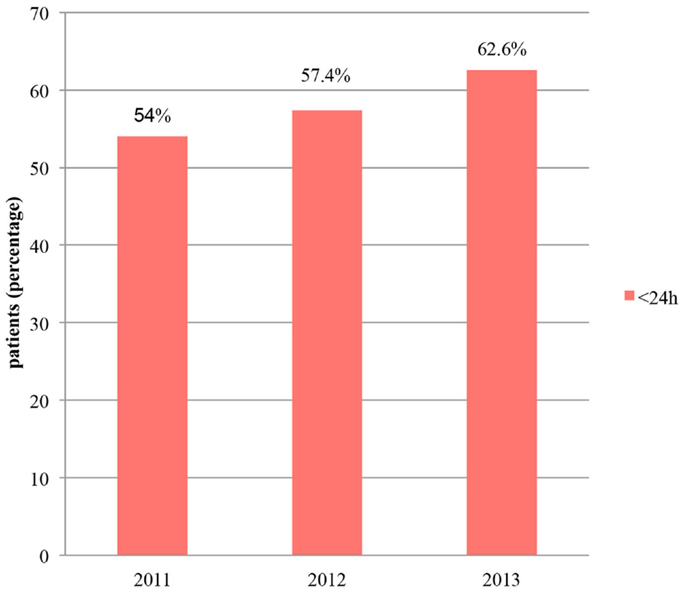
In terms of the time interval between emergency admission and surgery, the goal of the CP was to ensure that at least 90% of patients underwent surgery within 48 h. At the end of 2011, 88.8% of patients were treated within 48 h (Figure 2). In 2012, this figure dropped to 85.5%, due, in part, to the inclusion of patients who had an extended pre-operative period of longer than 72 h. However, if we excluded the patients who waited for medical reasons (cardiac or neurologic investigations, etc.), and therefore non-structural reasons (evaluated in 12 patients), this rate was then better than 2011, with a value of 89.75%. In 2013, with the same approach, 93.1% of patients underwent surgery within 48 h and 62.6% within 24 h (Figure 3).
Financial Indicators
The financial indicator chosen was the average LOS in hospital. As shown in Figure 4, fractures of the proximal femur, without major complications, accounted for 16 days in 2010 before the introduction of the CP. After initiation of the CP, this figure dropped to 11 days and remained constant thereafter (p Student <0.001, p Wilcoxon <0.001, p Trend test <0.001) (Figure 4).
We noted that in 2012, 52% of the patients went to a rehabilitation center at the end of their stay in acute care hospital, 32% to a nursing home, and <10% went directly home. In 2013, these figures were 55.1, 26.8, and 10.2%, respectively. In 2013, 35.4% of these patients were transferred to their previous living place. We observed an increase of patients going back home with a trend test almost significant (p = 0.57) and a chi-squared test that is statistically significant between 2010 and 2012 (p = 0.002).
Discussion
With this femoral fracture CP, we targeted a model of care, which focused on the patients’ needs, through a multidisciplinary approach. The aim was to combine a better quality of care for the patient, with a reduction in hospitalization costs. This CP was made possible with the concerted efforts of emergency physicians, orthopedic surgeons, nurses, unit management, responsible for the flow of patients through the system, physiotherapists, geriatricians, specialists in osteoporosis, and nutritionists. The osteoporosis specific treatment, which is given after the fracture for these patients, was not evaluated here as it is part of another CP (osteoporosis CP). After 3 years, we noted significant improvements in terms of the number of patients included in the CP (almost 90%).
Concerning the first clinical indicator, the prevalence of delirium, evaluations showed a decrease in the rate of positive delirium diagnosis in 2 years. This emphasized the importance of sharing knowledge between geriatricians and other medical personnel. This was particularly important in terms of necessity of frequent CAM assessments: this allowed to identify, treat, and prevent incidences of delirium. Within this program, in 3 years, we noted a clinically significant improvement in the rates of positive delirium detection by the nursing staff. However, this did not negate the essential role of geriatricians in the pre-operative and post-operative care of these patients (12). As a comparison in Brisbane (13), 54% of the patients with hip fractures experienced post-operative delirium. A rate of 12.7% was observed here after the implementation of the CP.
The meta-analysis of CPs for hip fracture cases of Neuman (8) found no significant differences in the proportion of post-operative pneumonia diagnoses, between pathway patients who underwent surgery within 36 h of hospital admission, and those receiving usual care. In our hospital, no statistical difference in this rate after 3 years of the CP was also found. However, early surgery, within 48 h of hospitalization, should reduce the risk of pneumonia among patients according to the systematic review and meta-analysis of Simunovic (14).
One of the goals of the CP was to have 100% of patients fulfilling at least 75% of their nutritional needs at the end of hospitalization. Three years after CP implementation the results had improved but, it still remains a weak point of this program. Indeed, two main barriers were observed. The first was missing or incomplete data on caloric intake. Subsequently, joint efforts by the Clinical Nutrition Team and the Orthopedic unit sought to increase the number of regular assessments. The second barrier was the loss of patients appetite and the difficulty of increasing food intake at mealtimes, despite support from the medical team. A strategy to encourage the consumption of snacks between meals has been proposed to overcome this issue. Though, this will require re-organization of the nursing day care. A recent study has shown that patients with higher caloric intake have lower complication rates and a shorter hospital stay on average (15).
An important clinical improvement after the implementation of the CP was the increase in the number of patients undergoing surgery within 48 h of admission. This rate was 88.8% after the first year of CP in 2011 and had increased to 93.1% by 2013. Particular efforts by surgeons to reduce the pre-operative period contributed massively to these excellent results. In comparison, the United Kingdom National Hip Fracture Database (UKD) (7) reported that the percentage of patients, with complete data, treated within 48 h of admission and within normal working hours had risen from 80% in 2010 to 87% in 2011, 83% in 2012, and 86% in 2013 (all patients who were medically unfit on admission were excluded). Similar results were found in 2009 in Hong-Kong, with 68% of the patients with hip fractures who underwent surgery within 48 h of hospital admission; in the hospital where a CP had been implemented since 2007, this rate was 86% (16).
The average LOS in our hospital for proximal femur fracture patients, without major complications, decreased from 16 days in 2010 to 11 days in 2012 and 2013. In UK (7), the national reports showed a mean length of acute stay of 16.4 days in 2011 and 15.7 days in 2013, which compare favorably with the average of 19.7 days observed in 2010. Another experience in Hong-Kong (16) showed that, after CP implementation the LOS in acute hospital reduced from 12.07 days in 2006 to 8.27 days in 2007, 7.67 days in 2008, and 6.66 days in 2009. However, some units provide both acute and rehabilitation services while other units favor quick discharge. Therefore, though we observed a decrease in the LOS in each hospital, which had a CP in operation, the LOS itself was dependent of individual hospital policy.
Finally, the communication between numerous clinicians has increased and is now perpetuated through regular CP review meetings. The successful deployment of a CP demanded concerted action and effective cooperation between different health professionals. We deem it essential that, as we did from initiation, a project manager is in place to ensure adequate data collection, provide training for the various care teams and oversee meeting coordination and communication between various disciplines. This is to safeguard the efficiency of the CP, and reassess aspects of the CP, with all partners, if required. Where necessary, responsibilities may also extend to the issuing of warnings when deficiencies in the process are identified. According to the Hong-Kong CP study also, an orthopedic nurse was engaged as project manager, and was responsible for data collection and auditing, and was considered to be a key element in the successful execution of the scheme (16).
Conclusion
Implementation of a CP for proximal femoral fractures had a positive impact. This CP facilitated an improvement in the qualitative and quantitative efficiency of proximal femoral fracture management in elderly patients particularly in terms of clinical, process, and financial factors. These good results should allow people to extend the concept of CP to patients with other common musculoskeletal pathologies.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors would like to thank Ariane Seuret, Duong Hong Dung for their assistance in data collection and Estelle Lecureux for help with statistical analysis.
References
1. Gullberg B, Johnell O, Kanis JA. World-wide projections for hip fracture. Osteoporos Int (1997) 7(5):407–13. doi: 10.1007/PL00004148
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
2. Berset DG, Dehlavi MA, Borens O, Bertrand PC. Traumatologie de la personne âgée: une urgence nutritionnelle ? Nutr Clinique et Métabolisme (2009) 23(3):129–32. doi:10.1016/j.nupar.2009.05.003
3. Bruce AJ, Ritchie CW, Blizard R, Lai R, Raven P. The incidence of delirium associated with orthopedic surgery: a meta-analytic review. Int Psychogeriatr (2007) 19(2):197–214. doi:10.1017/S104161020600425X
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
4. Shiga T, Wajima Z, Ohe Y. Is operative delay associated with increased mortality of hip fracture patients? Systematic review, meta-analysis, and meta-regression. Can J Anaesth (2008) 55(3):146–54. doi:10.1007/BF03016088
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
5. Mouhsine E, Wettstein M, Echenmoser G, Barres AM, Nicolas F, Gandibleux N. [Clinical pathway in traumatology, a fashion or need?]. Rev Med Suisse (2010) 6(276):2438–42.
6. Rotter T, Kinsman L, James E, Machotta A, Willis J, Snow P, et al. The effects of clinical pathways on professional practice, patient outcomes, length of stay, and hospital costs: cochrane systematic review and meta-analysis. Eval Health Prof (2012) 35(1):3–27. doi:10.1177/0163278711407313
7. Johansen A, Wakeman R, Boulton C, Plant F, Roberts J, Williams A. National Hip Fracture Database: National Report 2013. London: NHFD, Falls and Fragility Fracture Audit Programme, Royal College of Physicians (2013).
8. Neuman MD, Archan S, Karlawish JH, Schwartz JS, Fleisher LA. The relationship between short-term mortality and quality of care for hip fracture: a meta-analysis of clinical pathways for hip fracture. J Am Geriatr Soc (2009) 57(11):2046–54. doi:10.1111/j.1532-5415.2009.02492.x
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
9. De Bleser L, Depreitere R, De Waele K, Vanhaecht K, Vlayen J, Sermeus W. Defining pathways. J Nurs Manag (2006) 14(7):553–63. doi:10.1111/j.1365-2934.2006.00702.x
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
10. Kondrup J, Rasmussen HH, Hamberg O, Stanga Z, Ad hoc EWG. Nutritional risk screening (NRS 2002): a new method based on an analysis of controlled clinical trials. Clin Nutr (2003) 22(3):321–36. doi:10.1016/S0261-5614(02)00214-5
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
11. Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med (1990) 113(12):941–8. doi:10.7326/0003-4819-113-12-941
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
12. Coutaz M, Morisod J. [Orthogeriatric unit: a marriage of convenience between orthopedic surgeon and geriatrician?]. Rev Med Suisse (2010) 6(269):2094, 6–9.
13. Sivakumar BS, McDermott LM, Bell JJ, Pulle CR, Jayamaha S, Ottley MC. Dedicated hip fracture service: implementing a novel model of care. ANZ J Surg (2013) 83(7–8):559–63. doi:10.1111/j.1445-2197.2012.06201.x
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
14. Simunovic N, Devereaux PJ, Sprague S, Guyatt GH, Schemitsch E, Debeer J, et al. Effect of early surgery after hip fracture on mortality and complications: systematic review and meta-analysis. Can Med Assoc J (2010) 182(15):1609–16. doi:10.1503/cmaj.092220
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
15. Anbar R, Beloosesky Y, Cohen J, Madar Z, Weiss A, Theilla M, et al. Tight Calorie Control in geriatric patients following hip fracture decreases complications: a randomized, controlled study. Clin Nutr (2014) 33(1):23–8. doi:10.1016/j.clnu.2013.03.005
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
16. Lau TW, Leung F, Siu D, Wong G, Luk KD. Geriatric hip fracture clinical pathway: the Hong Kong experience. Osteoporos Int (2010) 21(Suppl 4):S627–36. doi:10.1007/s00198-010-1387-y
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
Keywords: clinical pathway, hip fractures, surgery efficiency, proximal femoral fracture, elderly patients
Citation: Fleury N, Chevalley F, Rubli E, Coti P, Farron A and Jolles BM (2015) Efficiency of the Lausanne clinical pathway for proximal femoral fractures. Front. Surg. 2:5. doi: 10.3389/fsurg.2015.00005
Received: 24 November 2014; Accepted: 01 February 2015;
Published online: 19 February 2015.
Edited by:
William Robert Walsh, UNSW Australia, AustraliaReviewed by:
Konstantinos Markatos, University of Athens, GreeceVedran Lovric, UNSW Australia, Australia
Copyright: © 2015 Fleury, Chevalley, Rubli, Coti, Farron and Jolles. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Brigitte M. Jolles, Hôpital Orthopédique, Avenue Pierre Decker 4, Ch-1011 Lausanne, Switzerland e-mail: brigitte.jolles-haeberli@chuv.ch
 Nicole Fleury
Nicole Fleury François Chevalley
François Chevalley Eve Rubli
Eve Rubli Pauline Coti
Pauline Coti
 Alain Farron
Alain Farron Brigitte M. Jolles
Brigitte M. Jolles