Treatment of fistula-in-ano with fistula plug – a review under special consideration of the technique
- 1Department of Surgery and Center for Minimally Invasive Surgery, Academic Teaching Hospital of Charité Medical School, Vivantes Hospital, Berlin, Germany
- 2Exeter Surgical Health Services Research Unit (HeSRU), Royal and Exeter Hospital, Exeter, UK
Introduction: In a recent Cochrane review, the authors concluded that there is an urgent need for well-powered, well-conducted randomized controlled trials comparing various modes of treatment of fistula-in-ano. Ten randomized controlled trials were available for analyses: There were no significant differences in recurrence rates or incontinence rates in any of the studied comparisons. The following article reviews the studies available for treatment of fistula-in-ano with a fistula plug with special attention paid to the technique.
Material and Methods: PubMed, Medline, Embase, and the Cochrane medical database were searched up to July 2015. Sixty-four articles were relevant for this review.
Results: Healing rates of 50–60% can be expected for treatment of complex anal fistula with a fistula plug, with a plug-extrusion rate of 10–20%. Such results can be achieved not only with plugs made of porcine intestinal submucosa but also those made of other biological or synthetic bioabsorbable mesh materials. Important technical steps are firm suturing of the head of the plug in the primary opening and wide drainage of the secondary opening.
Discussion: Treatment of a complex fistula-in-ano with a fistula plug is an option with a success rate of 50–60% with low complication rate. Further improvements in technique and better studies are needed.
Introduction
Fistula-in-ano is a difficult problem that physicians have struggled with since the time of Hippocrates (1). Despite the long-standing history of fistula-in-ano and the multiple approaches that are utilized, there is a paucity of high quality data to guide decision (1). In a recent Cochrane review, the authors concluded that there is an urgent need for well-powered, well-conducted randomized controlled trials comparing various modes of treatment of fistula-in-ano (2).Ten randomized controlled trials were available for analyses: there were no significant differences in recurrence rates or incontinence rates in any of the studied comparisons. The American Gastroenterological Association divides the fistula-in-ano into simple and complex (1). Simple fistulas are low – i.e., they involve a small or no portion of the sphincter complex. These fistulas include superficial, low intersphincteric, or low transsphincteric fistula. In addition, communication between the anal canal end skin is only via one tract and is not associated with inflammatory bowel disease, radiation or involve any other organ (1). Complex fistulas are anatomically higher: they involve a significant portion of the sphincter musculature, may have multiple tracts, involve other organs (i.e., vagina) and may be associated with radiation or inflammatory bowel disease. Recurrent fistulas are usually included in this category as well (1).
Fistulotomy, although extremely effective in treating low anal fistulas, is not a feasible option when the fistula tract incorporates a significant amount of the internal and external anal sphincter, as is the case for many high transsphincteric fistulas (3). It is also frequently contraindicated for anterior transsphincteric fistulas in women, for most fistulas in patients with Crohn’s disease, and for fistulas in patients who have diminished continence (3).
The alternative treatment option of a transanal mucosal advancement flap for patients with high transsphincteric fistulas has reported success rates ranging from 59 to 98%. However, these procedures are technically challenging and some authors report incontinence rates of up to 20% (3).
In Crohn’s disease-related high perianal fistulas, the mucosa advancement flap was combined with platelet-rich plasma (4).
Fibrin glue has also been used as treatment option, but with modest or poor success rates of between 0 and 74% (3–8).
Cutting seton procedures result in low recurrence rates, but can cause incontinence in up to 12–25% of patients (3, 9).
Ligation of the intersphincteric tract (LIFT) is a further alternative technique and has been associated with fistula closure rates of between 57 and 94% (3, 9). In a recent systematic review of 26 studies, including only 1 randomized controlled trial and 24 case series, 7 technical variations were used. Primary healing rates ranged from 47 to 95% (10).
Johnson et al. (11) first described the anal fistula plug, a bioabsorbable xenograft made of lyophilized porcine intestinal submucosa.
The following article reviews the studies available on treatment of fistula-in-ano with a fistula plug and calculates the success rates, while paying special attention to the fistula closure rate and the techniques used. The literature reports a success rate ranging from 24 to 88% with the mean follow up of 8 months. A possible explanation for this discrepancy could be differences in patient selection and variation of the technique (5). In a Consensus Conference, it was stated that a frequent issue affecting the plug procedure is a failure in the plug placement technique (5, 12). Therefore, each publication was carefully reviewed to identify the surgical technique employed. This sets this systematic review apart from those published hitherto.
Materials and Methods
PubMed, Medline, Embase, and the Cochrane medical databases were searched up to December 2014 using the key words: “Anal fistula” AND “Plug,” “Fistula-in-ano” AND “Plug,” “Anal fistula” AND “Fistula plug.” In addition, the references of articles retrieved were searched for relevant articles not previously identified. Sixty-four articles were relevant for this review.
Results
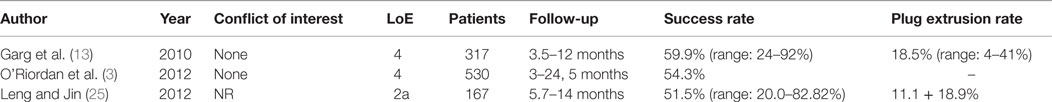
The first systematic review of the efficacy of a SIS-anal-fistula plug was published in 2010 (13). All randomized/non-randomized, controlled/non-controlled clinical trials, which studied SIS-anal-fistula plug or compared SIS-anal-fistula plug with other treatment methods for anal fistula and which reported clinical healing of the fistula as the outcome, were included. Studies on patients with rectovaginal fistula who were treated by SIS-anal-fistula plug and patients undergoing additional procedure (advancement flap or fibrin glue) along with SIS-anal-fistula plug were excluded from the review. One study reporting the usage of an acellular extracellular matrix was not included because the material used was different.
Twelve studies were analyzed in the systematic review (Table 1). These consisted of one RCT (11), seven prospective case series (14–20), and four retrospective case series (21–24). Since the majority of studies analyzed in the systematic review are prospective or retrospective case series, the level of evidence is only 4. Table 2 gives details of the surgical technique used in the studies included in the review.
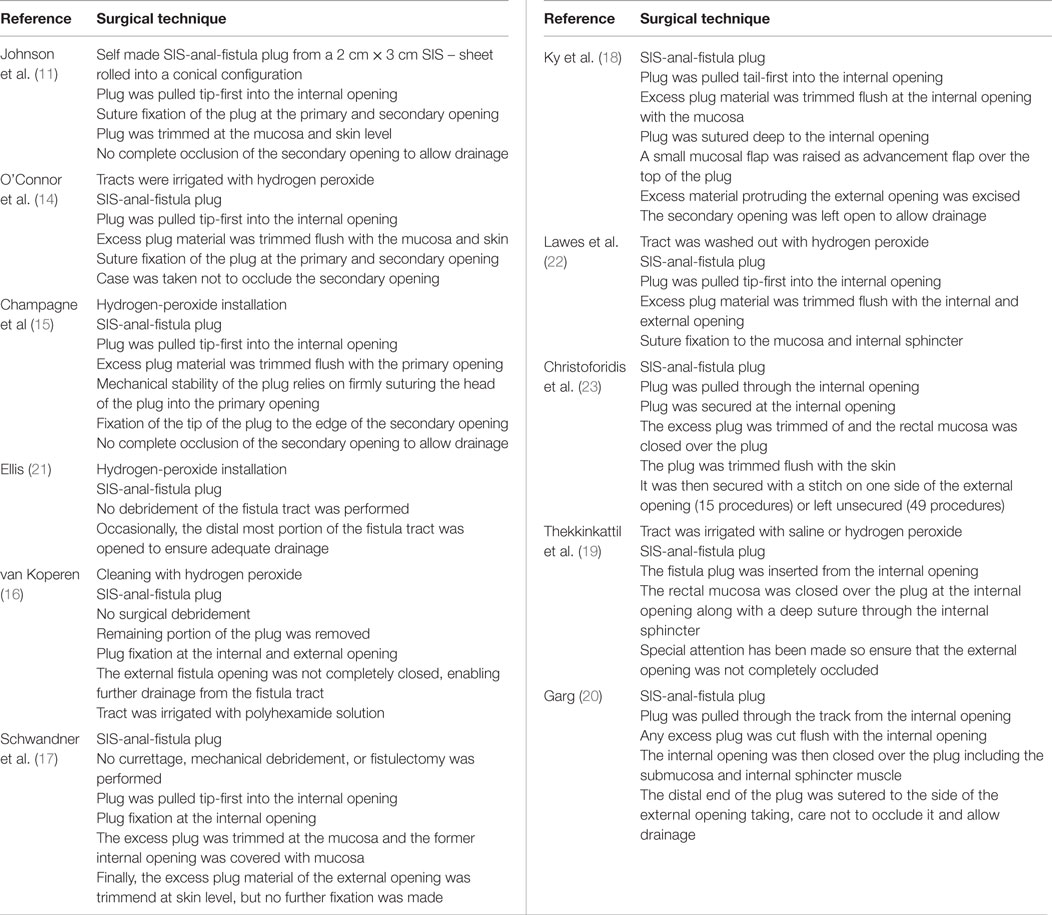
Table 2. Surgical techniques used in the studies included in the systematic review of Garg et al. (13).
A total of 317 patients were analyzed in the review by Garg (13) with a follow-up of range 3.5–12 months (Table 1). The SIS-anal-fistula plug procedure had a success rate of n = 180/317 (59.9%) ranging from 24 to 92%. The number of complex fistulae reported in 8 out of 12 studies was 186 with a success rate of n = 119/186 (64.0%) ranging from 35–87%. In patients with recurrent fistula, the success rate was n = 16/34 (47.1%) ranging from 13 to 71%. The success rate in patients with Crohn’s disease was n = 26/41 (63.4%) ranging from 29 to 86%. The success rate in patients with single tracts (n = 123/184; 66.8%, range 44–93%) seemed better than for patients with multiple tracts (n = 21/43; 48.8% range 20–71%). If the patients with plug extrusion were excluded from the analysis, the success rate was n = 121/189 (64.0%), ranging from 40 to 90%.The plug extrusion rate was n = 43/232 (18.5%), ranging from 4 to 41%.
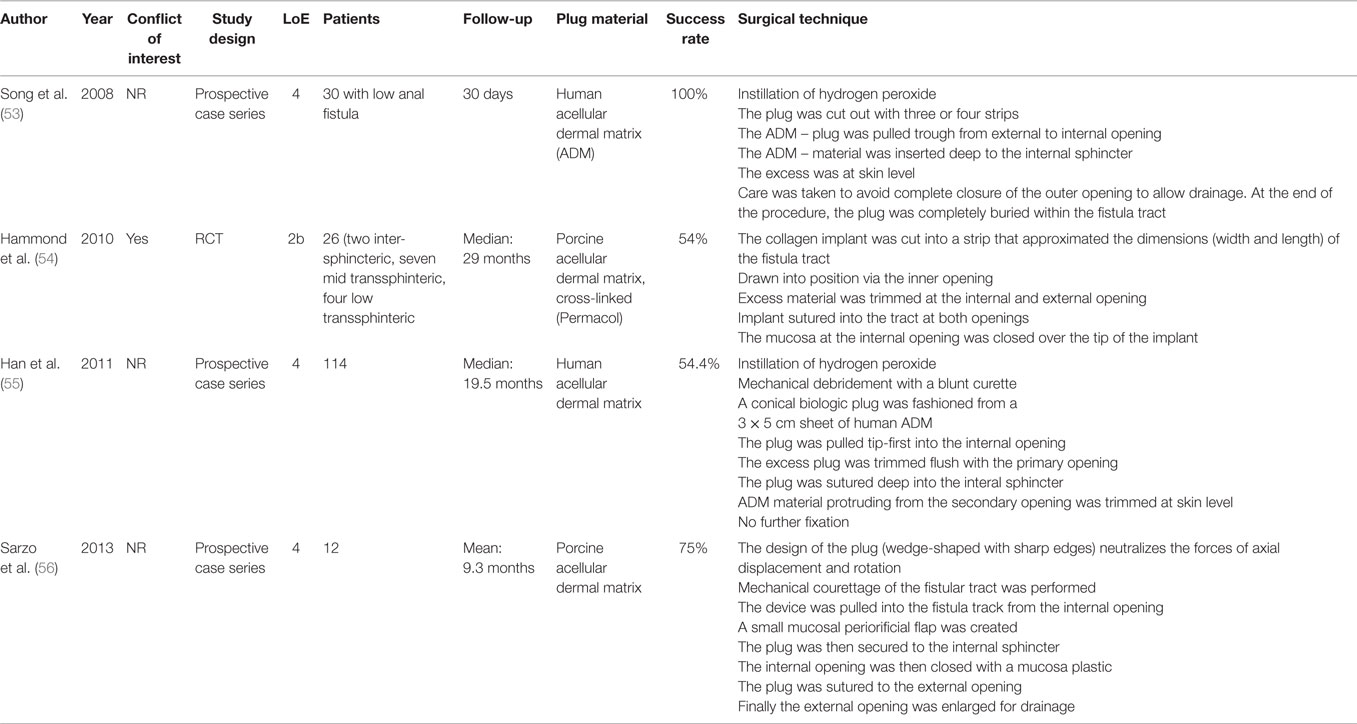
In 2012, another systematic review was published (3). This systematic review included studies whose results for patients with and without Crohn’s disease could be differentiated. Patients with rectovaginal, anovaginal, rectouretral, or ileal-pouch vaginal fistulas were excluded as were studies where the mean or median follow-up was <3 months.
The systematic review contained 20 studies, consisting of 18 articles and 2 abstracts (26, 27). Among the 20 studies included are two RCTs (28, 29), 10 prospective case series (15, 16, 20, 26, 30–35), and 8 retrospective case series (22, 24, 27, 36–40). Only 5 out of 20 of the publications listed were also included in the review by Garg (13, 15, 16, 20, 22, 24). This systematic review, too, was supported only by level of evidence 4 in view of the predominant number of prospective and retrospective case series.
Table 3 lists the exact surgical technique employed in the studies that were included in the review by O’Riordan (3) and not already analyzed in the Garg (13) review in Ref. (15, 16, 22, 24). Details of the surgical technique are not given for studies for which only an abstract is available (26, 27).
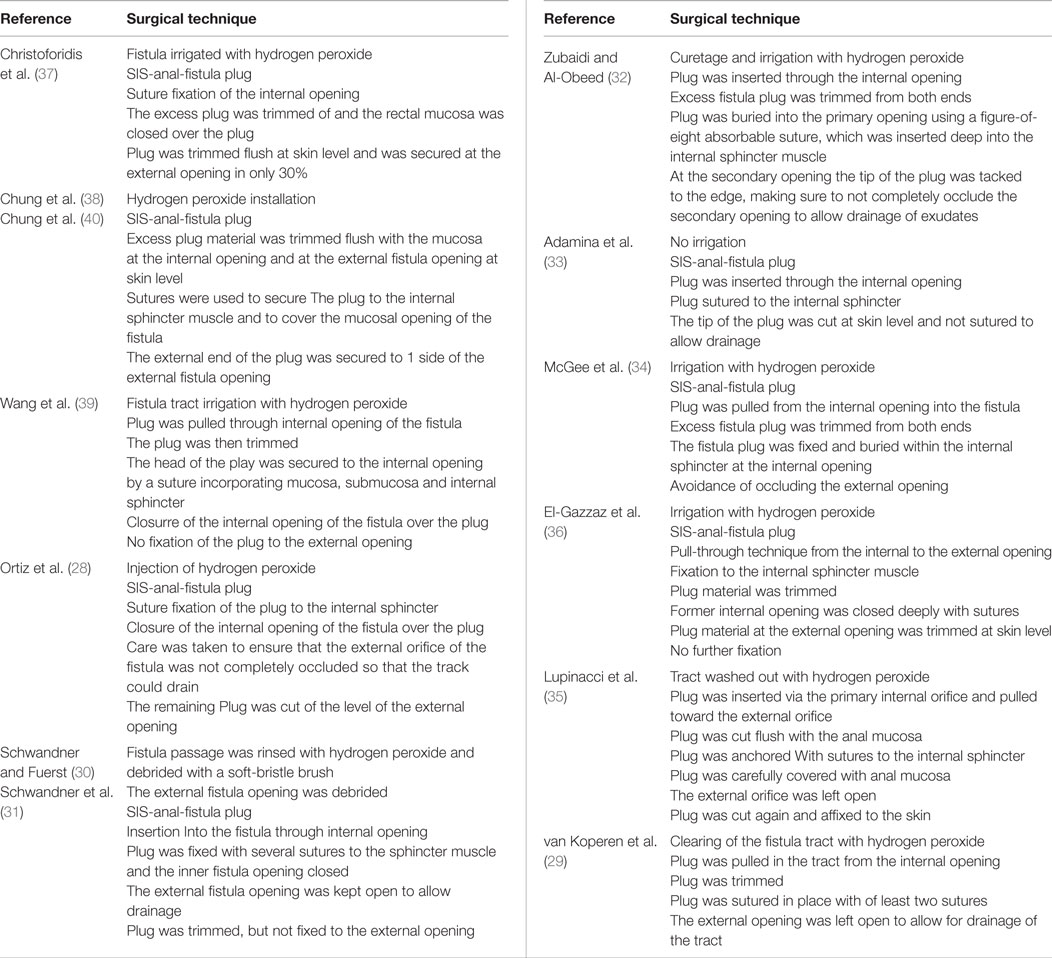
Table 3. Surgical techniques used in the studies included in the systematic review of O’Riordan et al. (3) minus abstracts and studies already analyzed in the review of Garg et al. (13).
The study sample sizes ranged from 4 to 60 patients with a pooled total of 530 patients for this review. Forty-two of these patients had Crohn’s disease, whereas 488 patients did not have Crohn’s disease. The shortest mean or median follow-up in the 20 studies was 3 months, and the longest follow-up was 24.5 months.
Closure of the fistula was successful in 288 of the 530 patients with fistula-in-ano (54.3%; 95% CI 0.50–0.59). The overall success rate for patients with Crohn’s disease was 23 of 42 patients (54.8%), whereas for patients without Crohn’s disease it was 265 of 488 patients (54.3%).
A total of 46 patients experienced plug extrusion (8.7%). Eight of the 20 included articles reported continence levels pre- and post-insertion of the SIS-anal-fistula plug (20, 23, 24, 29, 31, 34, 40). There were no reported cases of any significant change in continence after insertion of the SIS-anal-fistula plug in any of the patients in these studies (n = 196 patients).
Leng et al. (25) then published a meta-analysis comparing anal fistula plug vs. mucosa advancement flap in complex fistula-in-ano. The studies included were three RCTs (28, 29, 41), one prospective cohort study (33) and two retrospective case series (37, 38). Hence the level of evidence is 2a. Apart from the RCT by A ba-bai-Ke-re et al. (41), the other studies had also been taken into account in the systematic review by O’Riordan et al. (3) and Garg et al. (13).
The six studies encompassed 408 patients with 167 cases of SIS-anal-fistula plug treatment and 241 with mucosa advancement flap. The difference in the overall success rates and incidence of fistula recurrence was not statistically significant between SIS-anal-fistula plug and mucosa advancement flap in complex fistula-in-ano treatment (risk difference = −0.12. 95% CI: −0.39–0.14; risk difference = 0.13; 95% CI: −0.18–0.43, respectively). However, for the SIS-anal-fistula plug, the risk of postoperative impaired continence was lower (risk difference = −0.08. 95% CI: −0.15–0.02) as was the incidence of other complications (risk difference = −0.06. 95% CI: −0.11 to 0.00). Patients treated with the SIS-anal-fistula plug had less persistent pain of a shorter duration and the healing time of the fistula and hospital stay were also reduced. Another comparative study identified similar results for treatment, in addition to cost savings for the plug-in technique because of the shorter hospital stay (42).
Other studies (43–51), which had not been included in the systematic reviews and the meta-analysis (Table 4) do not have any implications for the results of the systematic reviews.
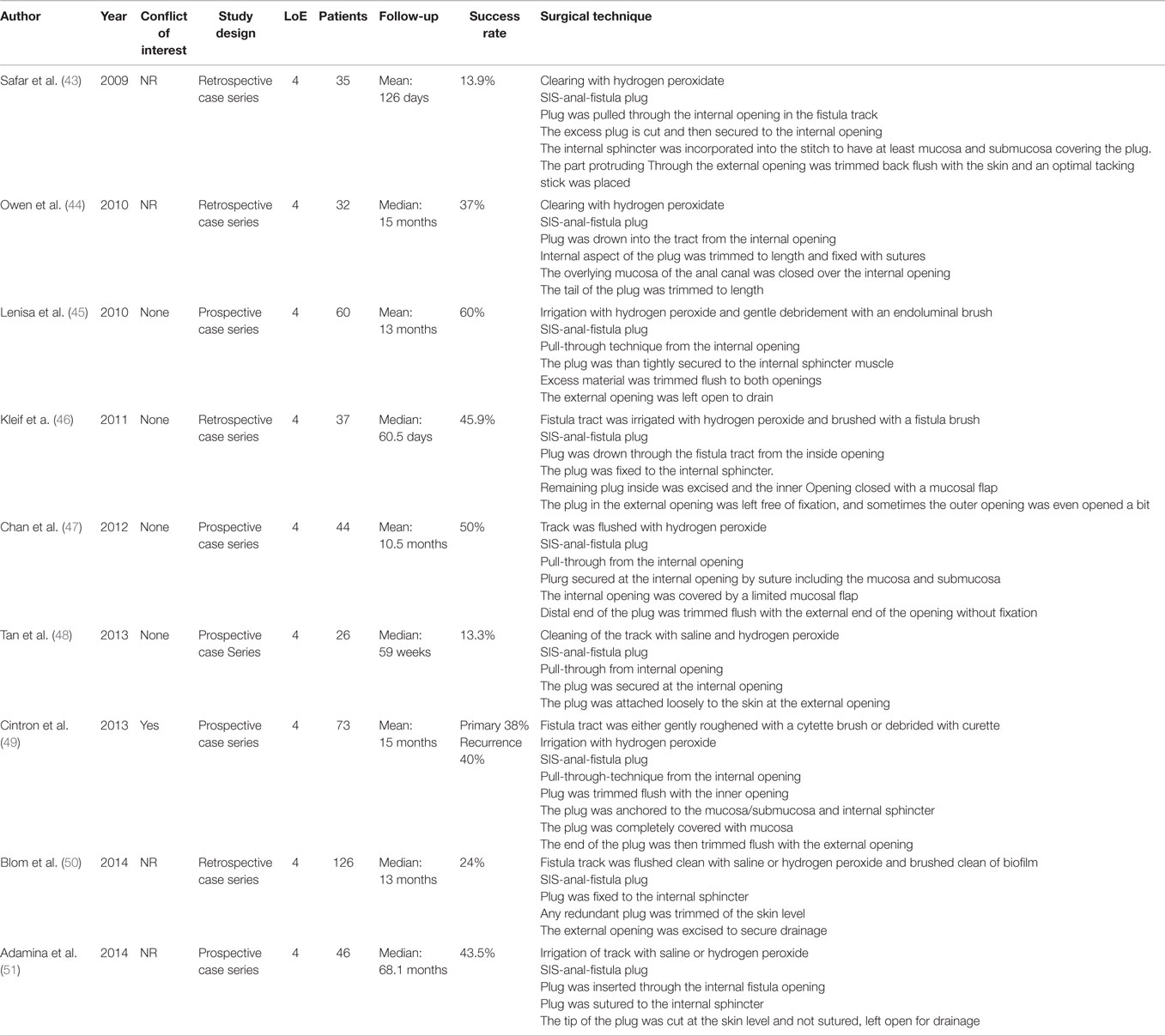
Table 4. Case series of SIS-anal-fistula plug treatment not included in the systematic reviews and meta-analyses.
It can thus be stated that treatment of complex anal fistula with SIS-anal-fistula plug is likely to be associated with a failure rate of about 50%. This result is not worse than that obtained for the mucosa advancement flap. However, the plug technique has the advantage of a lower postoperative complication rate and no negative impact on continence. More studies and technical modifications are needed to further improve the plug technique.
For example, Köckerling et al. (52) reported on a modified plug technique in which the extra-sphincteric portion of the complex anal fistula was removed by means of a limited fistulectomy and the remaining section of the fistula in the sphincter muscle was repaired using the fistula plug with fixing button. After a mean of 19.32 ± 6.9 months with a follow-up rate of 77% the success rate was 90%.
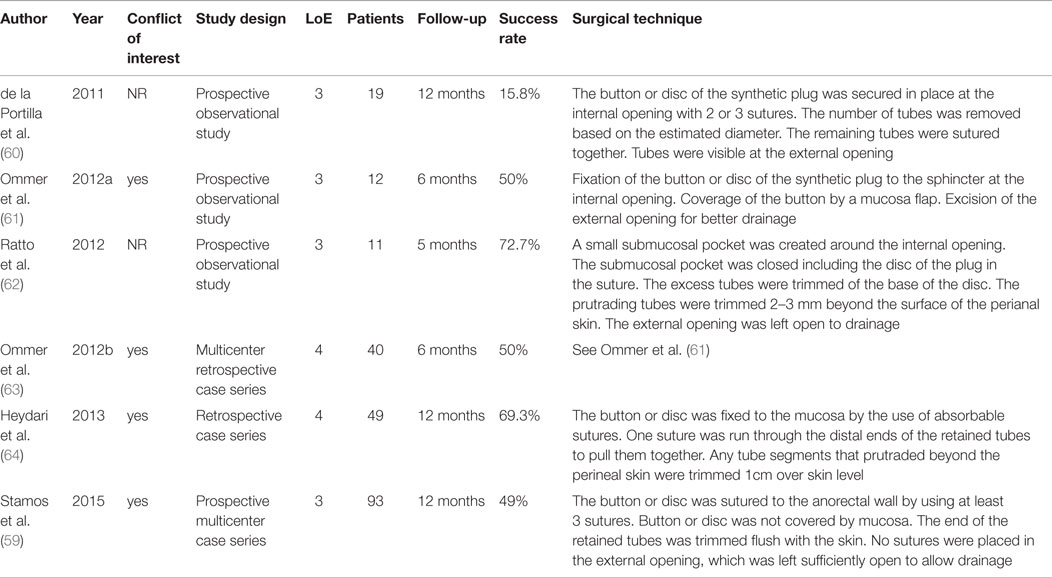
Another modification entails the use of plugs made of acellular dermal matrix instead of intestine submucosa (53–56). These are not preconfigured as a plug but are cut out from flat biological meshes. Details of the technique as well as the results are given in Table 5. The studies available show that success rates similar to those achieved with the SIS-anal-fistula plug can also be obtained with plugs made from acellular dermal matrix under similar technical conditions. In comparison to traditional surgical treatment, the fistula recurrence rate was significantly lower in the group treated with acellular dermal matrix (57).
In a pilot study, 10 patients with a median of 3 previous fistula operations were successfully operated on with an autologous cartilage plug from the nose or the ear. The treatment was initially successful in 90% of the patients, but two patients later developed a recurrence (58).
A relative new product for treatment of anal fistulas consists of a synthetic bioabsorbable anal fistula plug composed of a copolymer, from polyglycolic acid trimethylene carbonate, which is gradually absorbed by the body. This plug consists of a button or disc, with numerous tubes attached to it. Depending on the diameter of the fistula canal, several tubes are trimmed. The bioabsorption process is supposed to have been completed after 6–7 months (59). To date, there are only six prospective and retrospective cases series that report on treatment of anal fistulas with this synthetic bioabsorbable anal fistula plug (59–64). The results are illustrated in Table 6. The results obtained for the bioabsorbable fistula plug, too, are very variable, ranging from 15.8–72.7%. As in the case of the biological plug, that may be due to differences in the technical conduct of the operation (Tab. 6) or to differences in patient selection. Otherwise, the results obtained for the synthetic bioabsorbable anal fistula plug are comparable with those obtained for the plug made of biological material.
Discussion
In summary, healing rates of 50–60% can be expected for treatment of complex anal fistula with a fistula plug, with a plug extrusion rate of 10–20%. That result is not worse than that achieved for the mucosa advancement flap, fibrin glue treatment or ligation of the intersphincteric tract.
The anal fistula plug poses a lower risk of postoperative impairment of sphincter muscle function and other postoperative complications than the transanal mucosal advancement flap. Such results can be achieved not only with plugs made of porcine intestinal submucosa, but also those made of other biological mesh materials, such as acellular dermal matrix, and synthetic bioabsorbable material.
It is possible that additional modifications to the technique, e.g., limited fistulectomy of the extrasphincter portion of the anal fistula, will further improve the outcome. Important technical steps in the successful performance of a complex anal fistula plug repair are a mechanical debridement of the fistula tract or partial removal of the extra sphincteric portion of the tract, pulling the plug tip-first in the internal opening, trimming excess plug material flush with the primary opening, suturing firmly the head of the plug into the primary opening, fixation of the tip of the plug to the edge of the secondary opening and no complete occlusion, but wide secondary opening to allow drainage.
There is a need for more high-quality prospective comparative studies which, in addition to the anal fistula diagnosis, give precise technical details of the operation technique, design and biological or synthetic material of the plugs employed as well as their fixation. Both RCTs and registries lend themselves to that effect.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at https://www.frontiersin.org/article/10.3389/fsurg.2015.00055
References
1. Bleier JIS, Moloo H. Current management of cryptoglandular fistula-in-ano. World J Gastroenterol (2011) 17(28):3286–91. doi: 10.3748/wjg.v17.i28.3286
2. Jacob TJ, Perakath B, Keighley MR. Surgical intervention for anorectal fistula. Cochrane Database Syst Rev (2010) 12(5):CD006319. doi:10.1002/14651858.CD006319.pub2
3. O’Riordan JM, Datta I, Johnston C, Baxter NN. A systematic review of the anal fistula plug for patients with Crohn’s and non-Crohn’s related fistula-in-ano. Dis Colon Rectum (2012) 55:351–8. doi:10.1097/DCR.0b013e318239dle4
4. Göttgens KWA, Smeets RR, Stassen LPS, Beets GL, Pierik M, Breukink SO. Treatment of Crohn’s disease-related high perianal fistulas combining the mucosa. advancement flap with platelet-rich plasma: a pilot study. Tech Coloproctol (2015) 19:455–9. doi:10.1007/s10151-015-1311-8
5. Limura E, Giordano P. Modern management of anal fistula. World J Gastroenterol (2015) 21(1):12–20. doi:10.3748/wjg.v21.i1.12
6. Zmora O, Neufeld D, Ziv Y, Tulchinsky H, Scott D, Khaikin M, et al. Prospective, multicenter evaluation of highly concentrated fibrin glue in the treatment of complex cryptogenic perianal fistulas. Dis Colon Rectum (2005) 48:2167–72. doi:10.1007/s10350-005-0199-1
7. Hammond TM, Grahn MF, Lunniss PJ. Fibrin glue in the management of anal fistulae. Colorectal Dis (2004) 6:308–19. doi:10.1111/j.1463-1318.2004.00676.x
8. Swinscoe MT, Ventakasubramaniam AK, Jayne DG. Fibrin glue for fistula-in-ano: the evidence reviewed. Tech Coloproctol (2005) 9(2):89–94. doi:10.1007/s10151-005-0204-7
9. Shawki S, Wexner SD. Idiopathic fistula-in-ano. World J Gastroenterol (2011) 17(28):3277–85. doi:10.3748/wjg.v17.i28.3277
10. Sirany AME, Nygaard RM, Morken JJ. The ligation of the intersphinctereic fistula tract procedure for anal fistula: a mixed bag of results. Dis Colon Rectum (2015) 58:604–12. doi:10.1097/DCR.0000000000000374
11. Johnson EK, Gaw JU, Armstrong DN. Efficacy of anal fistula plug vs fibrin glue in closure of anorectal fistulas. Dis Colon Rectum (2006) 49:371–6. doi:10.1007/s10350-005-0288-1
12. The surgisis® AFP™ anal fistula plug: report of a consensus conference. Colorectal Dis (2007) 10:17–20. doi:10.1111/j.1463-1318.2007.01423.x
13. Garg P, Song J, Bhatia A, Kalia H, Menon GR. The efficacy of anal fistula plug in fistula-in-ano: a systematic review. Colorectal Dis (2010) 12:965–70. doi:10.1111/j.1463-1318.2009.01933.x
14. O’Connor L, Champagne BJ, Ferguson MA, Orangio GR, Schertzer ME, Armstrong DN. Efficacy of anal fistula plug in closure of Crohn’s anorectal fistulas. Dis Colon Rectum (2006) 49:1569–73. doi:10.1007/s10350-006-0695-y
15. Champagne BJ, O’Connor LM, Ferguson M, Orangio GR, Schertzer ME, Armstrong DN. Efficacy of anal fistula plug in closure of cryptoglandular fistulas: long-term follow-up. Dis Colon Rectum (2006) 49:1817–21. doi:10.1007/s10350-006-0755-3
16. van Koperen PJ, Hoore A, Wolthuis AM, Bemelman WA, Slores JFM. Anal fistula plug for closure of difficult anorectal fistula: a prospective study. Dis Colon Rectum (2007) 50:2168–72. doi:10.1007/s10350-007-0298-2
17. Schwandner O, Stadler F, Dietle O, Wirsching RP, Fuerst A. Initial experience on efficacy in closure of cryptoglandular and Crohn’s transsphincteric fistulas by the use of the anal fistula plug. Int J Colorectal Dis (2008) 23:319–24. doi:10.1007/s00384-007-0398-4
18. Ky AJ, Sylla P, Steinhagen R, Steinhagen E, Khaitov S, Ly EK. Collagen fistula plug for the treatment of anal fistulas. Dis Colon Rectum (2008) 51:838–43. doi:10.1007/s10350-007-9191-2
19. Thekkinkattil DK, Botterill I, Ambrose NS, Lundby L, Sagar PM, Buntzen S, et al. Efficacy of the anal fistula plug in complex anorectal fistulae. Colorectal Dis (2009) 11:584–7. doi:10.1111/j.1463-1318.2008.01627.x
20. Garg P. To determine the efficacy of anal fistula plug in the treatment of high fistula-in-ano: an initial experience. Colorectal Dis (2009) 11:588–91. doi:10.1111/j.1463-1318.2008.01632.x
21. Ellis CN. Bioprosthetic plugs for complex anal fistulas: an early experience. J Surg Educ (2007) 64(1):36–40. doi:10.1016/j.cursur.2006.07.005
22. Lawes DA, Efron JE, Abbas M, Heppell J, Young-Fadok TM. Early experience with the bioabsorbale anal fistula plug. World J Surg (2008) 32:1157–9. doi:10.1007/s00268-008-9504-1
23. Christoforidis D, Etzioni DA, Goldberg SM, Madoff RD, Mellgren A. Treatment of complex anal fistulas with the fistula plug. Dis Colon Rectum (2008) 51:1482–7. doi:10.1007/s10350-008-9374-5
24. Echenique I, Mella JR, Rosado F, Echenique IA, Mella MT, Quevedo G. Puerto Rico experience with plugs in the treatment of anal fistulas. Bol Asoc Med P R (2008) 100:8–12.
25. Leng QL, Jin HY. Anal fistula plug vs mucosa advancement flap in complex fistula-in-ano: a meta-analysis. World J Gastrointest Surg (2012) 4(11):256–61. doi:10.4240/wjgs.v4.i11.256
26. Starck M, Bohe M, Zawadzki A. Success rate of closure of high transsphincteric fistulas using anal fistula plug. Dis Colon Rectum (2008) 51:692.
27. Anyadike C, Attuwaybi B, Visco J, Butler B, Barrios G. The anal fistula plug in simple and complex fistula-in-ano: a western New York expience. Dis Colon Rectum (2010) 53:575.
28. Ortiz H, Marzo J, Ciga MA, Oteiza F, Armendáriz P, Miguel de M. Randomized clinical trial of anal fistula plug versus endorectal advancement flap for the treatment of high cryptoglandular fistula in ano. Br J Surg (2009) 96:608–12. doi:10.1002/bjs.6613
29. van Koperen PJ, Bemelman WA, Gerhards MF, Janssen LWM, Tets van WF, Dalsen van AD, et al. The anal fistula plug treatment compared with the mucosal advancement flap for cryptoglandular high transsphincteric perianal fistula: a double-blinded multicenter randomized trial. Dis Colon Rectum (2011) 54:387–93. doi:10.1007/DCR0b013e318206043e
30. Schwandner O, Fuerst A. Preliminary results on efficacy in closure of transsphincteric and rectovaginal fistulas associated with Crohn’s disease using new biomaterials. Surg Innov (2009) 16(2):162–8. doi:10.1177/1553350609338041
31. Schwandner T, Roblick MH, Kierer W, Brom A, Padberg W, Hirschburger M. Surgical treatment of complex anal fistulas with the anal fistula plug: a prospective, multicenter study. Dis Colon Rectum (2009) 52:1578–83. doi:10.1007/DCR0b013e3181a8fbb7
32. Zubaidi A, Al-Obeed O. Anal fistula plug in high fistula-in-ano: an early Saudi experience. Dis Colon Rectum (2009) 52:1584–8. doi:10.1007/DCR.0b013e3181a90b65
33. Adamina M, Hoch JS, Burnstein MJ. To plug or not to plug: a cost-effectiveness analysis for complex anal fistula. Surgery (2010) 147(1):72–8. doi:10.1016/j.surg.2009.05.018
34. McGee MF, Champagne BJ, Stulberg JJ, Reynolds H, Marderstein E, Delaney CP. Tract length predicts sucessful closure with anal fistula plug in cryptoglandular fistulas. Dis Colon Rectum (2010) 53:1116–20. doi:10.1007/DCR.0b013e3181d972a9
35. Lupinacci RM, Vallet C, Parc Y, Chafai N, Tiret E. Treatment of fistula-in-ano with the surgisis® AFP™ anal fistula plug. Gastroenterol Clin Biol (2010) 34:549–53. doi:10.1016/j.gcb.2009.06.021
36. El-Gazzaz G, Zutshi M, Hull T. A retrospective review of chronic anal fistulae treated by anal fistulae plug. Colorectal Dis (2010) 12:442–7. doi:10.1111/j.1463-1318.2009.01802.x
37. Christoforidis D, Pieh MC, Madoff RD, Mellgren AF. Treatment of transsphincteric anal fistulas by endorectal advancement flap or collagen fistula plug: a comparative study. Dis Colon Rectum (2009) 52:18–22. doi:10.1007/DCR.0b013e31819756ac
38. Chung W, Kazemi P, Ko D, Sun C, Brown CJ, Raval M, et al. Anal fistula plug and fibrin glue versus conventional treatment in repair of complex anal fistulas. Am J Surg (2009) 197:604–8. doi:10.1016/j.amjsurg.2008.12.013
39. Wang JY, Garcia-Aguilar J, Sternberg JA, Abel ME, Varma MG. Treatment of transsphincteric anal fistulas: are fistula plugs an acceptable alternative? Dis Colon Rectum (2009) 52:692–7. doi:10.1007/DCR.0b013e31819d473f
40. Chung W, Ko D, Sun C, Raval MJ, Brown CL, Phang PT. Outcomes of anal fistula surgery in patients with inflammatory bowel disease. Am J Surg (2010) 199(5):609–13. doi:10.1016/j.amjsurg.2010.01.007
41. A ba-bai-ke-re MM, When H, Huang HG, Chu H, Lu M, Chang ZS, et al. Randomized controlled trial of minimally invasive surgery using acellular dermal matrix for complex anorectal fistula. World J Gastroenterol (2010) 16:3279–86. doi:10.3748/wjg.v16.i26.3279
42. Fisher OM, Raptis DA, Vetter D, Novak A, Dindo D, Hahnloser D, et al. An outcome and cost analysis of anal fistula plug insertion vs endorectal advancement flap for complex anal fistulae. Colorectal Dis (2014) 17:619–26. doi:10.1111/codi.12888
43. Safar B, Jobanputra S, Sands D, Weiss EG, Nogueras JJ, Wexner SD. Anal fistula plug: initial experience and outcomes. Dis Colon Rectum (2009) 52:248–52. doi:10.1007/DCT.0b013e31819c96ac
44. Owen G, Keshava A, Stewart P, Patterson J, Chapuis P, Bokey E, et al. Plugs unplugged. Anal fistula plug: the Concord experience*. ANZ J Surg (2010) 80:341–3. doi:10.111/j.1445-2197.2010.05278.x
45. Lenisa L, Espin-Basany E, Rusconi A, Mascheroni L, Escoll-Rufino J, Lozoya-Trujillo R, et al. Anal fistula plug is a valid alternative option for the treatment of complex anal fistula in the long term. Int J Colorectal Dis (2010) 25:1487–93. doi:10.1007/s00384-010-0957-y
46. Kleif J, Hagen K, Wille-Jørgensen P. Acceptable results using plug for the treatment of complex anal fistulas. Dan Med Bull (2011) 58(3):A4254.
47. Chan S, McCullough J, Schizas A, Vasas P, Engledow A, Windsor A, et al. Initial experience of treating anal fistula with the surgisis anal fistula plug. Tech Coloproctol (2012) 16:201–6. doi:10.1007/s10151-012-0810-0
48. Tan KK, Kaur G, Byrne CM, Young CJ, Wright C, Solomon MJ. Long-term outcome of the anal fistula plug for anal fistula of cryptoglandular origin. Colorectal Dis (2013) 15:1510–4. doi:10.1111/codi.12391
49. Cintron JR, Abcarian H, Chaudhry V, Singer M, Hunt S, Birnbaum E, et al. Treatment of fistula-in-ano using a porcine small intestinal submucosa anal fistula plug. Tech Coloproctol (2013) 17:187–91. doi:10.1007/s10151-012-0897-3
50. Blom J, Husberg-Sellberg B, Lindelius A, Gustafsson UM, Carlens S, Oppelstrup H, et al. Results of collagen plug occlusion of anal fistula: a multicenter study of 126 patients. Colorectal Dis (2014) 16:626–30. doi:10.1111/codi.12585
51. Adamina M, Ross T, Guenin MO, Warschkow R, Rodger C, Cohen Z, et al. Anal fistula plug: a prospective evaluation of success, continence and quality of life in the treatment of complex fistulae. Colorectal Dis (2014) 16:547–54. doi:10.1111/codi.12594
52. Köckerling F, Rosen von T, Jacob D. Modified plug repair with limited sphincter sparing fistulectomy in the treatment of complex anal fistulas. Front Surg (2014) 1:17. doi:10.3389/fsurg.2014.00017
53. Song WL, Wang ZJ, Zheng Y, Yang XQ, Peng YP. A anorectal fistula treatment with acellular extracellular matrix: a new technique. World J Gastroenterol (2008) 14(30):4791–4. doi:10.3748/wjg.14.4791
54. Hammond TM, Porrett TR, Scott SM, Williams NS, Lunniss PJ. Management of idiopathic and fistula using cross-linked collagen: a prospective phase 1 study. Colorectal Dis (2010) 13:94–104. doi:10.1111/j.1463-1318.2009.02087.x
55. Han JG, Wang ZJ, Zhao C, Zheng Y, Zhao B, Yi BQ, et al. Long-term outcomes of human acellular dermal matrix plug in closure of complex anal fistulas with a single tract. Dis Colon Rectum (2011) 54:1412–8. doi:10.1097/DCR.0b013e31822c5398
56. Sarzo G, Finco C, Mungo B, Gruppo M, Cadrobbi R, Polese L, et al. Anal fistula repair with acellular dermal matrix plug: description of a novel technique and early results. J Surg (2013) 1(1):1–6 and non-Crohn’s related fistula-in-ano. Dis Colon Rectum 55:351–58. doi:10.1097/DCR.0b013e318239dle4
57. Cirocchi R, Trastulli S, Morelli U, Desiderio J, Boselli C, Parisi A, et al. The treatment of anal fistulas with biologically derived products: is innovation better than convertional surgical treatment? An update. Tech Coloproctol (2013) 17:259–73. doi:10.1007/s10151-012-0948-9
58. Ozturk E. Treatment of recurrent anal fistula using an autologous cartilage plug: a pilot study. Tech Coloproctol (2015) 19:301–7. doi:10.1007/s10151-015-1299-0
59. Stamos MJ, Snyder M, Robb BW, Ky A, Singer M, Stewart DB, et al. Prospective multicenter study of a synthetic bioabsorbable anal fistula plug to treat cryptoglandular transsphincteric anal fistulas. Dis Colon Rectum (2015) 58:344–51. doi:10.1097/DCR0000000000000288
60. de la Portilla F, Rada R, Jiménez-Rodriguez R, Diaz-Pavon JM, Sanchez-Gil JM. Evaluation of a new synthetic plug in the treatment of anal fistulas: results of a pilot study. Dis Colon Rectum (2011) 54:1419–22. doi:10.1097/DCR.0b013e31822c4d59
61. Ommer A, Schmidt C, Rolfs T, Walz MK. Gore Bio-A Fistelplug zur Behandlung hoher Analfisteln. Coloproctology (2012) 34:24–30. doi:10.1007/s00053-011-0245-5
62. Ratto C, Litta F, Parello A, Donisi L, Zaccone G, De Simone V. Gore Bio-A® fistula Plug: a new sphincter-sparing procedure for complex anal fistula. Colorectal Dis (2012) 14:e264–9. doi:10.1111/j.1463-1318.2012.02964.x
63. Ommer A, Herold A, Joos A, Schmidt C, Weyand G, Bussen D. Gore BioA fistula plug in the treatment of high anal fistulas – initial results from a German multicenter-study. Ger Med Sci (2012) 10:Doc13. doi:10.3205/000164
Keywords: complex anal fistula, fistula plug, biological mesh, fistula closure rate, incontinence
Citation: Köckerling F, Alam NN, Narang SK, Daniels IR and Smart NJ (2015) Treatment of fistula-in-ano with fistula plug – a review under special consideration of the technique. Front. Surg. 2:55. doi: 10.3389/fsurg.2015.00055
Received: 22 July 2015; Accepted: 30 September 2015;
Published: 16 October 2015
Edited by:
Sanoop Koshy Zachariah, MOSC Medical College, IndiaReviewed by:
Jose M. Ramia, Regional Public Health System of Castilla La Mancha, SpainBoris Eugeniev Sakakushev, University Hospital St George Plovdiv, Bulgaria
Tzu-An Chen, Taiwan Landseed Hospital, Taiwan
Copyright: © 2015 Köckerling, Alam, Narang, Daniels and Smart. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ferdinand Köckerling, ferdinand.koeckerling@vivantes.de
 Ferdinand Köckerling
Ferdinand Köckerling Nasra N. Alam
Nasra N. Alam Sunil K. Narang
Sunil K. Narang Ian R. Daniels
Ian R. Daniels Neil J. Smart
Neil J. Smart