The Predictive Value of Integrated Pulmonary Index after Off-Pump Coronary Artery Bypass Grafting: A Prospective Observational Study
- Department of Anesthesiology and Intensive Care Medicine, Northern State Medical University, Arkhangelsk, Russia
Background: The early warning scores may increase the safety of perioperative period. The objective of this study was to assess the diagnostic and predictive role of Integrated Pulmonary Index (IPI) after off-pump coronary artery bypass grafting (OPCAB).
Materials and Methods: Forty adult patients undergoing elective OPCAB were enrolled into a single-center prospective observational study. We assessed respiratory function using IPI that includes oxygen saturation, end-tidal CO2, respiratory rate, and pulse rate. In addition, we evaluated blood gas analyses and hemodynamics, including ECG, invasive arterial pressure, and cardiac index. The measurements were performed after transfer to the intensive care unit, after spontaneous breathing trial and at 2, 6, 12, and 18 h after extubation.
Results and Discussion: The value of IPI registered during respiratory support correlated weakly with cardiac index (rho = 0.4; p = 0.04) and ScvO2 (rho = 0.4, p = 0.02). After extubation, IPI values decreased significantly, achieving a minimum by 18 h. The IPI value ≤9 at 6 h after extubation was a predictor of complicated early postoperative period (AUC = 0.71; p = 0.04) observed in 13 patients.
Conclusion: In off-pump coronary surgery, the IPI decreases significantly after tracheal extubation and may predict postoperative complications.
Introduction
Cardiac surgery can be complicated by respiratory failure that may contribute to increased morbidity and additional health-care costs (1, 2). The outcome of coronary artery bypass grafting can be significantly influenced by decompensation caused by chronic pulmonary diseases and other complications (atelectases, pleuritis, etc.) (3–5). Therefore, the thorough postoperative monitoring of pulmonary function during both mechanical ventilation and spontaneous breathing may be of a great value. Notably, the modern monitoring devices should be accurate and non- or minimally invasive with measurements that are continuous and results easily interpreted (6).
To maintain respiratory function, the cardiosurgical patients are monitored using pulse oximetry, capnography, respiratory rate, and discrete blood gas analysis (7–9). Although blood gas analyses are the gold standard for early detection of different types of respiratory failure, they are invasive, cannot be measured continuously, and frequently impose a delay between sampling and availability of results (10). Thus, the early warning systems allowing early recognition of critical respiratory events might be of value when patient is monitored both in the intensive care unit (ICU), postoperative ward, and high dependency unit. This approach can be particularly useful with a limited number of medical staff. Several observational studies indicate that early warning systems improve detection of complications (11), and their use is recommended by the World Federation of Societies of Anesthesiologists to facilitate the work of nurses and physicians in the ICU (12, 13).
The Integrated Pulmonary Index (IPI) is an automated value calculated by one monitor (Capnostream-20, Medtronic, Israel) and can be considered as an automated early warning system. The IPI algorithm utilizes the real time measures and interactions of four parameters—end-tidal CO2 (PetCO2), respiration rate, pulse rate, and oxygen saturation (SpO2) to provide an assessment of the patient’s respiratory status. The calculation of the IPI is based on the fuzzy logic principle, a mathematical model, which mimics human logic thinking; detailed description of the algorithm was provided by Ronen et al. (14) The values of IPI below 7 have been suggested to be an indicator for respiratory deterioration (14).
Currently, only few investigations of IPI were performed during non-cardiosurgical procedures (14–18) In these studies, IPI algorithm correlated with the respiratory status and has demonstrated the ability for promoting early awareness to changes in a patient’s respiratory system.
The aim of our study was to assess the diagnostic and predictive role of IPI during the discontinuation from mechanical ventilation and in the early postextubation period after off-pump coronary artery bypass grafting (OPCAB).
Materials and Methods
The study was performed in a 900-bed university hospital (City Hospital #1 of Arkhangelsk, Russia). During 2015, 40 adult patients undergoing elective OPCAB were enrolled into an observational prospective study. The study design and the informed consent form were approved by the Ethical Committee of Northern State Medical University (Arkhangelsk, Russian Federation) and registered with http://ClinicalTrials.gov (ref: NCT02524522). Written informed consent was obtained from every patient. Exclusion criteria were age <18 and >80 years, morbid obesity with body mass index >40 kg/m2, and constant atrial fibrillation.
All patients were intubated using the standard induction technique with sodium thiopental (4 mg/kg), fentanyl (2.5–3.0 μg/kg) and pipecuronium bromide (0.1 mg/kg). Anesthesia was maintained using sevoflurane (0.5–3.0 vol.% at the end of expiration) and fentanyl (2.0–4.0 μg/kg/h). Depth of anesthesia was adjusted to maintain BIS values between 40 and 60 (LifeScope, Nihon Kohden, Japan).
In all cases, preoxygenation with 80% O2 was provided during 3–5 min before anesthesia. After tracheal intubation, patients were ventilated using a protective volume-controlled mode (Dräger Primus, Germany) with tidal volume of 6–8 mL/kg of predicted body weight, flow of 1 L/min and positive end-expiratory pressure (PEEP) of 5 cm H2O. FiO2 was set to at least 50% or higher to achieve intraoperative SpO2 above 95%. The respiratory rate was adjusted to maintain PetCO2 value within 30–35 mmHg.
After surgery, all patients were transferred to the postoperative cardiac ICU and shortly sedated with continuous infusion of propofol (2–4 μg/kg/h) to maintain BIS values within 60–70. Respiratory support in ICU was provided by a G5 ventilator (Hamilton Medical, Switzerland) using pressure controlled ventilation mode with parameters of intraoperative ventilation. Additionally, all patients received recruitment maneuver by raising the PEEP to 20 cm H2O for 5 min.
After the initial measurements, sedation was stopped, and the weaning from respiratory support was initiated. The weaning protocol included gradual reduction of inspiratory pressure and mandatory respiratory rate, as well as spontaneous breathing trial. After passing the 30-min spontaneous breathing trial, all the patients were immediately extubated. After extubation, the patients received a supplementary oxygen flow of 4 L/min via a nasal catheter. During the weaning process and in the early postextubation period, all the patients received continuous infusion of fentanyl and discrete administration of paracetamol for multimodal analgesia. In addition, the postoperative therapy included aspirin, low-molecular weight heparins, and bisoprolol.
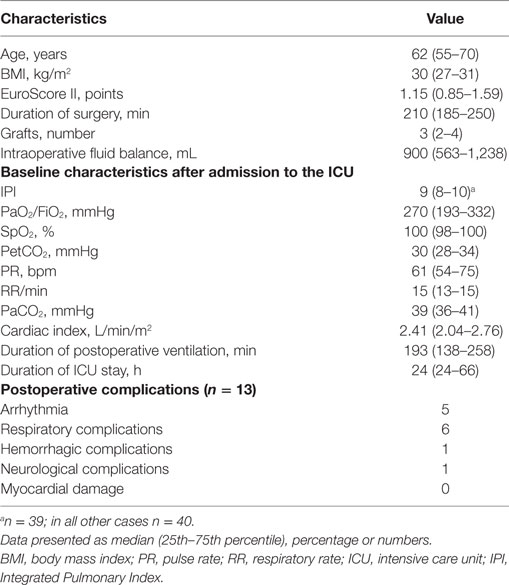
The measurements included ventilator parameters, blood gas analyses (ABL800Flex, Radiometer, Denmark), PetCO2, SpO2, respiratory rate, pulse rate, and IPI (Capnostream-20, Medtronic). The IPI measurement is based on continuous transformation of SpO2, PetCO2, pulse rate, and respiratory rate values into a single index from 1 to 10, where “10” indicates a normal respiratory status, and “1” indicates that patient requires immediate intervention. We distributed patients into two subgroups: with optimal (IPI 9–10) and suboptimal (IPI ≤ 8) IPI values (Table 1). After tracheal extubation, for a more accurate assessment of the IPI, all the values were measured following breathing during 5 min without supplemental oxygen (FiO2 0.21), avoiding the reduction of SpO2 less than 88%. Continuous hemodynamic measurements included ECG monitoring, invasive arterial pressure and cardiac output measured with pulse wave transit time (esCCO, Nihon Kohden, Japan).
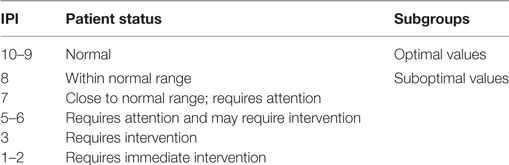
Table 1. The clinical interpretation of Integrated Pulmonary Index (IPI) (14).
All these parameters were registered after transfer to the ICU, as well as after spontaneous breathing trial and at 2, 6, 12, and 18 h after extubation. In addition, we recorded the preoperative EuroScore II, perioperative fluid balance, left ventricle ejection fraction assessed by transthoracic echocardiography before and 24 h after surgery, duration of postoperative mechanical ventilation and ICU stay, as well as early postoperative complications and hospitalization time. Postoperative complications were assessed according to the categories as predefined the study protocol: arrhythmias, hemorrhage, respiratory complications, neurological complications, and postoperative myocardial damage. Arrhythmic complications were comprised of any episode of atrial fibrillation, ventricular arrhythmia, or fibrillation requiring therapeutic intervention. Hemorrhagic complications were defined as drainage blood loss of more than 200 mL/h for three consecutive hours or re-sternotomy. Respiratory complications were reintubation, need for prolonged oxygen therapy, pneumothorax, hydrothorax, chylothorax, or pneumonia. Patients were considered as requiring prolonged oxygen therapy after extubation in case if needed oxygen insufflation more than 12 h to maintain SpO2 > 93%. Neurological complications were defined as postoperative delirium or stroke. The postoperative myocardial damage was defined as an increase in the plasma concentration of creatine kinase-MB > 50 pg/mL.
Statistical Analysis
For data collection and analysis, we used SPSS software (version 17.0; SPSS Inc., USA) and MedCalc software (version 12.3, MedCalc Software, Belgium). Due to pilot design of the study, the sample size was limited by 40 patients. All the variables were expressed as median (25th–75th interquartile interval). The groups were compared using Mann–Whitney test. The intragroup comparisons were performed by Friedman and post hoc Wilcoxon tests with Bonferroni correction. For correlation analysis, we used Spearman test. Nominal data were compared using χ2 test and expressed as patient number. To evaluate the ability of IPI and PetCO2 to predict cardiac index <2.5 L/min/m2 during mechanical ventilation, we performed ROC-curve analysis and calculated area under the ROC curve (AUC). The ROC analysis was also used to assess the capability of IPI and PaO2/FiO2 measured at 6 h after extubation for prediction of postoperative complications during 24 h. The optimal cutoff point for IPI was determined by maximum value of the Youden Index (maximizing sensitivity and specificity). For post hoc intragroup comparisons, p value < 0.013 was considered as statistically significant. In all other cases, p value < 0.05 was regarded as statistically significant.
Results
We enrolled 30 males and 10 females. Demographic and baseline characteristics of the patients, as well as postoperative complications are shown in Table 2.
After admission to the ICU, we had difficulties in registration of the IPI value only in one patient. Notably, 10 min later IPI was registered in 100% of patients. After admission to the ICU, 5% of patients required attention according to their respiratory status and had IPI < 7. Simultaneously, 63% of patients had PaO2/FiO2 < 300 mmHg. The IPI values, measured after ICU admission, weakly correlated with cardiac index (rho = 0.4, p = 0.04) and ScvO2 (rho = 0.4, p = 0.02). The decreased values of IPI and PetCO2 during controlled mechanical ventilation were associated with CI < 2.5 L/min/m2 (cutoff point for IPI ≤ 8, sensitivity 84%, specificity 53%, positive predictive value 64%, negative predictive value 75%, AUC = 0.72, p = 0.02; cutoff point for PetCO2 ≤ 30 mmHg, sensitivity 78%, specificity 68%, positive predictive value 70%, negative predictive value 76%, AUC = 0.73, p = 0.02, Figure 1).
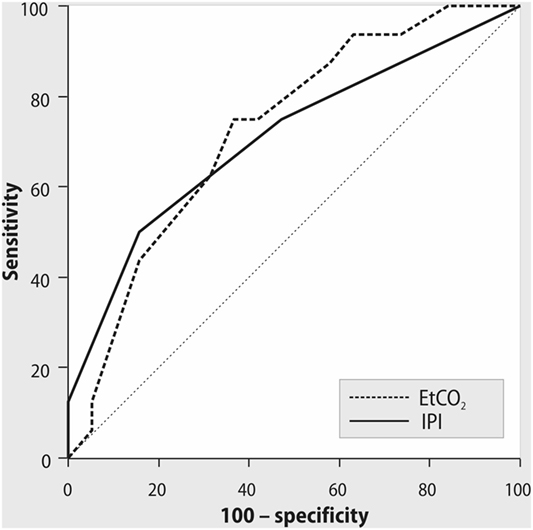
Figure 1. ROC curves for Integrated Pulmonary Index (IPI), end-tidal CO2, and cardiac index < 2.5 L/min/m2 during mechanical ventilation. AUC = 0.72, p = 0.02; cutoff point of IPI ≤ 8, with sensitivity 84%, specificity 53%, positive predictive value 64%, negative predictive value 75%. AUC = 0.73, p = 0.02; cutoff point of PetCO2 ≤ 30 mmHg, with sensitivity 78%, specificity 68%, positive predictive value 70%, negative predictive value 76%.
All patients were successfully weaned from mechanical ventilation. PaO2/FiO2 ratio was stable both during the spontaneous breathing trial and after tracheal extubation. In contrast, IPI decreased significantly after OPCAB with a minimal value at 18 h after extubation (Figure 2). As shown in Figure 3, in patients with PaO2/FiO2 < 200 mmHg on ICU admission, the IPI values at 2, 6, 12, and 18 h after extubation did not exceed suboptimal range (≤8) (p < 0.05 as compared to IPI values of the subgroup with PaO2/FiO2 > 200 mmHg).
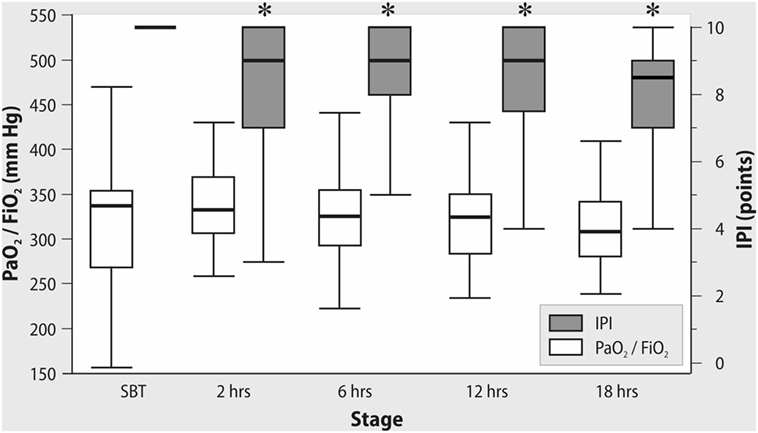
Figure 2. Changes in PaO2/FiO2 and Integrated Pulmonary Index (IPI) after tracheal extubation. *Wilcoxon test, p < 0.01.
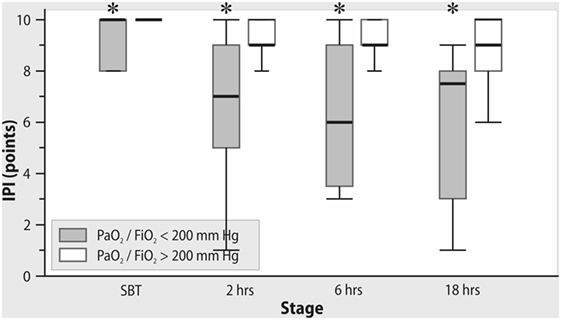
Figure 3. The changes in Integrated Pulmonary Index (IPI) after extubation in subgroups with PaO2/FiO2 <200 mmHg and >200 mmHg on admission to the intensive care unit. *Mann–Whitney test, p < 0.05.
In addition, the suboptimal IPI values at 2 h after tracheal extubation were associated with higher preoperative EuroScore and decreased left ventricular ejection fraction before and after OPCAB (Table 3). In the subgroup with IPI ≤ 8, we observed decreased SpO2 and etCO2, as well as increased pulse rate. Higher IPI values were associated with positive fluid balance and decreased rate of diuretic administration at the first day of ICU stay.
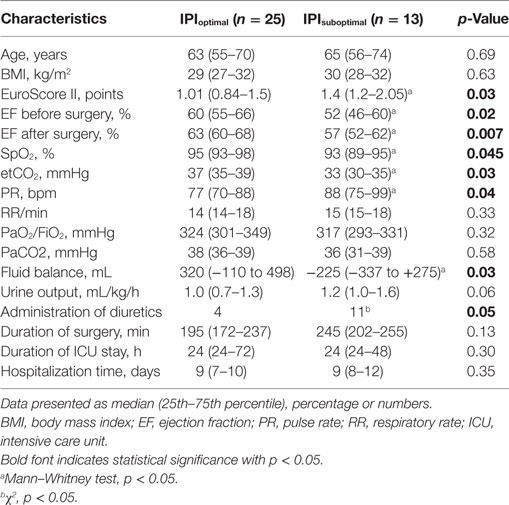
Table 3. Comparative characteristics in subgroups of patients with optimal (>8) and suboptimal (≤8) IPI values at 2 h after extubation.
The length of ICU and hospital stay did not differ between the patients with optimal and suboptimal IPI values. We did not find any associations between PaO2/FiO2 ratio and the length of ICU stay either. However, IPI value ≤9 at 6 h after extubation demonstrated moderate predictive ability for early postoperative complications (AUC = 0.707; p = 0.04, with sensitivity 92% and specificity 48%, positive predictive value 57%, negative predictive value 89%, Figure 4). PaO2/FiO2 ratio at 6 h after extubation did not demonstrate any predictive ability for postoperative complications (AUC = 0.543; p = 0.67).
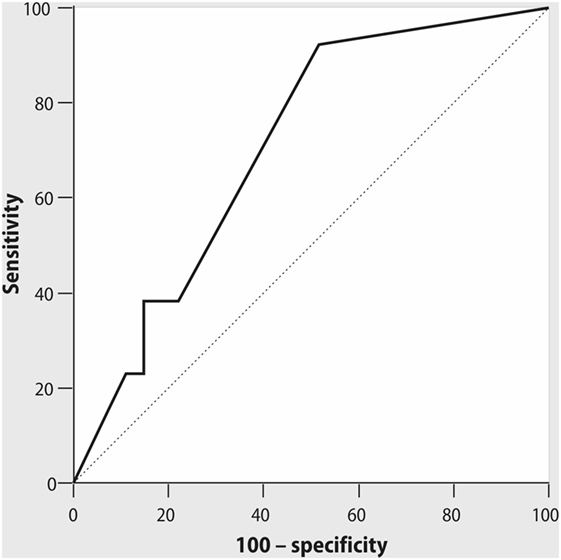
Figure 4. ROC curve for Integrated Pulmonary Index (IPI), measured at 6 h after tracheal extubation, and early postoperative complications. AUC = 0.71; p = 0.04, cutoff point of IPI ≤ 9 with sensitivity 92% and specificity 48%, positive predictive value 57%, negative predictive value 89%.
Discussion
Our study has shown that IPI can provide important information about respiratory and hemodynamic status of the cardiosurgical patient, especially during the postextubation period.
In our study, we observed difficulties in registration of the IPI value after admission to the ICU in one patient from 40 enrolled into the study; this problem can be explained by decreased perfusion, leading to low SpO2 signal. Low perfusion as well as motion artifacts are the well-known limitations of pulse oximetry observed in the early postoperative period after cardiac surgery (19).
After admission to the ICU, the number of patients with compromised respiratory function according to their PaO2/FiO2 values (63%) was higher than the number of patients requiring attention according to the IPI values (5%). During controlled mechanical ventilation, several components of IPI like respiratory rate, SpO2, and PetCO2, are determined mainly by the operator-depending settings of the ventilator that may not reflect the complex respiratory status. The association of IPI, measured after admission to the ICU, with cardiac index and ScvO2, observed in our study can be explained by the relationship between cardiac output, PetCO2, and oxygen transport (20). Although the described correlations were weak that can be caused by dependence of end-tidal CO2 not only from cardiac output but also from ventilation, metabolism, and other factors, our findings are consistent with other investigations in this field. In several studies, authors demonstrated that PetCO2 and cardiac output had a positive association in different categories of patients (21–23). Thus, Baraka and colleagues have shown that cardiac output correlated with PetCO2 during partial cardiopulmonary bypass and following weaning from bypass (22). In this study, PetCO2 > 30 mmHg during partial bypass predicted an adequate cardiac output after perfusion. At the same time, PetCO2 < 30 mmHg may correctly denote a low cardiac output only in combination with low ScvO2 (22). This relationship between PetCO2 and cardiac function can be relevant not only for cardiac surgery; thus, Dunham and colleagues have found that a decline in PetCO2 correlates with decrease in non-invasive cardiac output in emergently intubated trauma patients (23). Notably, the addition of pulse rate into the algorithm for calculation of IPI could improve the ability of this parameter to predict decreased cardiac output compared with PetCO2 alone. However, our ROC analysis has shown equal AUC to predict CI < 2.5 L/min/m2 both for IPI < 8 and for PetCO2 < 30 mmHg. The possible explanation for this finding could be that the heart rate is just one of the determinants of cardiac output, thus PetCO2 alone may have similar accuracy with IPI in predicting cardiac output after OPCAB.
Notably, reduced IPI values during controlled mechanical ventilation observed in our study can be explained by decreased PetCO2 levels. During spontaneous breathing with ambient air (FiO2 21%), suboptimal IPI was also associated with decreased SpO2 values and increased pulse rate, aiming to maintain adequate cardiac output and oxygen delivery. We suppose that, summarizing the key cardiovascular and respiratory parameters, IPI can be a useful tool for postoperative assessment of patient in addition to PaO2/FiO2 ratio, which has a limited value due to dependence on FiO2 (24) This can explain the stable values of PaO2/FiO2 with simultaneous reduction of SpO2 and IPI after extubation while breathing with ambient air. It is important to mention that the measurement of IPI does not replace postoperative blood gases but it can potentially reduce the number of blood gas samples, is continuous as compared to discrete blood gases and can serve as a “monitoring bridge” after discontinuation of mechanical ventilation and invasive monitoring.
The association of suboptimal IPI values with preoperative EuroScore and ejection fraction before and after intervention demonstrates the relationship of IPI and severity of cardiac comorbidities. Several studies have shown that decreased ejection fraction after cardiac surgery may be associated with risk of sepsis, postoperative respiratory failure and prolonged mechanical ventilation (25, 26). Thus, the reduction of IPI after cardiac surgery can detect patients who require more complex hemodynamic monitoring and optimization including fluids, diuretics, inotrope/vasopressor support, and other therapies.
Association between IPI value ≤9, recorded at 6 h after extubation and the incidence of early complications after OPCAB seems to be relevant for prediction of the course of postoperative period. We did not find in other studies the data about the opportunity of IPI to predict the course of postoperative period, although IPI was effective in detection of clinically significant events, such as hypoxia or bradypnea, during the intraoperative period (16, 17). The complications observed during our study (predominantly, atrial fibrillation and respiratory failure) are accompanied by changes in respiratory and hemodynamic status of the patient. The patients after cardiac surgery can have a higher alert threshold of IPI as compared to other settings where the attention is required when IPI is ≤7. The diagnostic capabilities of IPI need further validation and studies including the assessment of IPI as a marker for the safe transfer from ICU.
Study Limitations
Our findings have a limitation due to relatively small sample size. In addition, all the patients from our study received bisoprolol postoperatively that may influence the heart rate, as well as the IPI value.
Conclusion
Integrated pulmonary index is associated with changes in cardiac output and may predict the postoperative complications during the discontinuation from mechanical ventilation and in the early postextubation period after OPCAB. This index may be a valuable adjunct to the routine monitoring during spontaneous breathing, but not during controlled mechanical ventilation.
Ethics Statement
This study was carried out in accordance with the recommendations of the ethics committee of the Northern State Medical University (Arkhangelsk, Russian Federation). All subjects gave written informed consent in accordance with the Declaration of Helsinki. The protocol was approved by the ethics committee of the Northern State Medical University (Arkhangelsk, Russian Federation).
Author Contributions
All authors had contributed equally.
Conflict of Interest Statement
The study has received the research grant from Medtronic (Boulder, CO, USA). The authors declare that the research was conducted in the absence of any other commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors thank the personnel of the cardiosurgical ICU, City Hospital #1 of Arkhangelsk, for their kind assistance during the conduct of the investigation.
Funding
The study has received the research grant from Medtronic (Boulder, CO, USA).
References
1. Ng CS, Wan S, Yim AP, Arifi AA. Pulmonary dysfunction after cardiac surgery. Chest (2002) 4:1269–77. doi:10.1378/chest.121.4.1269
2. Weissman C. Pulmonary complications after cardiac surgery. Semin Cardiothorac Vasc Anesth (2004) 8:185–211. doi:10.1177/108925320400800303
3. Forouzannia SK, Abdollahi MH, Mirhosseini SJ, Hadadzadeh M, Hosseini H, Moshtaghion SH, et al. Perioperative predictors and clinical outcome in early and late ICU discharge after off-pump coronary artery bypass surgery. Acta Med Iran (2011) 49:307–9.
4. Ho CH, Chen YC, Chu CC, Wang JJ, Liao KM. Postoperative complications after coronary artery bypass grafting in patients with chronic obstructive pulmonary disease. Medicine (Baltimore) (2016) 95:1–5. doi:10.1097/MD.0000000000002926
5. Vakili M, Shirani S, Paknejad O, Yousefshahi F. Acute respiratory distress syndrome diagnosis after coronary artery bypass: comparison between diagnostic criteria and clinical picture. Acta Med Iran (2015) 53:51–6.
6. Vincent JL, Rhodes A, Perel A, Martin GS, Della Roca G, Vallet B, et al. Clinical review: update on hemodynamic monitoring-a consensus of 16. Crit Care (2011) 15:1–8. doi:10.1186/cc10291
7. Brochard L, Martin GS, Blanch L, Pelosi P, Belda FJ, Jubran A, et al. Clinical review: respiratory monitoring in the ICU – a consensus of 16. Crit Care (2012) 16:1–14. doi:10.1186/cc11146
8. Heinze H, Sedemund-Adib B, Heringlake M, Meier T, Eichler W. Relationship between functional residual capacity, respiratory compliance, and oxygenation in patients ventilated after cardiac surgery. Respir Care (2010) 55:589–94.
9. MacNaughton PD. Assessement of lung function in the ventilated patients. Intensive Care Med (1997) 8:810–8. doi:10.1007/s001340050417
10. Technology Subcommittee of the Working Group on Critical Care, Ontario Ministry of Health. Noninvasive blood gas monitoring: a review for use in the adult critical care unit. CMAJ (1992) 146:703–12.
11. Alam N, Hobbelink EL, Tienhoven AJ. The impact of the use of the early warning score (EARLY WARNING SYSTEMS) on patient outcomes: a systematic review. Resuscitation (2014) 85:587–94. doi:10.1016/j.resuscitation.2014.01.013
12. Dawes TR, Cheek E, Bewick V, Dennis M, Duckitt RW, Walker J, et al. Introduction of an electronic physiological early warning system: effects on mortality and length of stay. Br J Anaesth (2014) 4:603–9. doi:10.1093/bja/aeu107
13. Kyriacos U, Jelsma J, James M, Jordan S. Early warning scoring systems versus standard observations charts for wards in South Africa: a cluster randomized controlled trial. Trials (2015) 16:103–18. doi:10.1186/s13063-015-0624-2
14. Ronen M, Weissbrod R, Overdyk FJ, Ajizian S. Smart respiratory monitoring: clinical development and validation of the IPI™ (integrated pulmonary index) algorithm. J Clin Monit Comput (2017) 31:435–42. doi:10.1007/s10877-016-9851-7
15. Berkenstadt H, Ben-Menachem E, Herman A, Dach R. An evaluation of the integrated pulmonary index (IPI) for the detection of respiratory events in sedated patients undergoing colonoscopy. J Clin Monit Comput (2012) 26:177–81. doi:10.1007/s10877-012-9357-x
16. Garah J, Adiv OE, Rosen I, Shaoul R. The value of integrated pulmonary index (IPI) monitoring during endoscopies in children. J Clin Monit Comput (2015) 29:773–8. doi:10.1007/s10877-015-9665-z
17. Sabbatani P, Mantovan R. Electrical cardioversion of atrial fibrillation: evaluation of sedation safety with midazolam by means of EtCO2 and IPI algorithm analysis. Int J Cardiol (2013) 169:430–2. doi:10.1016/j.ijcard.2013.10.015
18. Karbing DS, Rees SE, Jaffe MB. Journal of clinical monitoring and computing 2015 end of year summary: respiration. J Clin Monit Comput (2016) 30:7–12. doi:10.1007/s10877-015-9820-6
19. Nitzan M, Romem A, Koppel R. Pulse oximetry: fundamentals and technology update. Med Devices (Auckl) (2014) 7:231–9. doi:10.2147/MDER.S47319
20. Isserles SA, Breen PH. Can changes in end-tidal PCO2 measure changes in cardiac output? Anesth Analg (1991) 6:808–14.
21. Whitaker DK, Benson JP. Capnography standards for outside the operating room. Curr Opin Anaesthesiol (2016) 29(4):485–92. doi:10.1097/ACO.0000000000000355
22. Baraka AS, Aouad MT, Jalbout MI, Kaddoum RN, Khatib MF, Haroun-Bizri ST. End-tidal CO2 for prediction of cardiac output following weaning from cardiopulmonary bypass. J Extra Corpor Technol (2004) 36:255–7.
23. Dunham CM, Chirichella TJ, Gruber BS, Ferrari JP, Martin JA, Luchs BA, et al. In emergently ventilated trauma patients, low end-tidal CO2 and low cardiac output are associated and correlate with hemodynamic instability, hemorrhage, abnormal pupils, and death. BMC Anesthesiol (2013) 13:20–8. doi:10.1186/1471-2253-13-20
24. Karbing DS, Kjaergaard S, Smith BW, Espersen K, Allerød C, Andreassen S, et al. Variation in the PaO2/FiO2 ratio with FiO2: mathematical and experimental description, and clinical relevance. Crit Care (2007) 11:R118. doi:10.1186/cc5697
25. Cohen AJ, Katz MG, Frenkel G, Medalion B, Geva D, Schachner A. Morbid results of prolonged intubation after coronary artery bypass surgery. Chest (2000) 6:1724–31. doi:10.1378/chest.118.6.1724
Keywords: postoperative respiratory failure, coronary artery bypass grafting, monitoring, microstream capnography, integrated pulmonary index
Citation: Fot EV, Izotova NN, Yudina AS, Smetkin AA, Kuzkov VV and Kirov MY (2017) The Predictive Value of Integrated Pulmonary Index after Off-Pump Coronary Artery Bypass Grafting: A Prospective Observational Study. Front. Med. 4:132. doi: 10.3389/fmed.2017.00132
Received: 14 June 2017; Accepted: 25 July 2017;
Published: 09 August 2017
Edited by:
Bernd Saugel, University Medical Center Hamburg-Eppendorf, GermanyReviewed by:
Agnes S. Meidert, Ludwig-Maximilians-Universität München, GermanyDaniel Lahner, Institute for Experimental and Clinical Traumatology (LBG), Austria
Copyright: © 2017 Fot, Izotova, Yudina, Smetkin, Kuzkov and Kirov. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Evgenia V. Fot, ev_fot@mail.ru
 Evgenia V. Fot
Evgenia V. Fot Natalia N. Izotova
Natalia N. Izotova
 Vsevolod V. Kuzkov
Vsevolod V. Kuzkov Mikhail Y. Kirov
Mikhail Y. Kirov