Enrollment, Childbearing Motivations, and Intentions of Couples in the Creighton Model Effectiveness, Intentions, and Behaviors Assessment (CEIBA) Study
- Department of Family and Preventive Medicine, University of Utah, Salt Lake City, UT, United States
Context: The Creighton Model FertilityCareTM System (CrM) is a standardized approach for educating women about the biomarkers of their fertility. Couples can use this information for timing intercourse during “fertile” or “infertile” days in order to try to conceive or to avoid pregnancy.
Objectives: The study of Creighton Model Effectiveness, Intentions, and Behaviors Assessment (CEIBA) was conducted to assess fertility motivations, intentions, fertility-related sexual behaviors, and their impact on effectiveness to avoid and to conceive among new users of the CrM. This paper reports enrollment baseline characteristics.
Settings and design: We conducted this prospective cohort study at 17 CrM FertilityCareTM Centers; 16 in the USA and one in Toronto, Canada.
Materials and methods: Couples who were new or returning users of the CrM were eligible. Couples who were initially trying to conceive or had a history of subfertility were excluded. Couples were enrolled and followed prospectively by their CrM instructors and also by CEIBA study staff. They completed baseline questionnaires.
Results: 1,132 new couples were assessed; 1,090 (96%) couples were screened; 429 (39%) couples were eligible; 305 women (71%) and 290 (95%) male partners were enrolled. The majority of women was engaged (39%) or married (51%), college graduates (77%), Caucasian non-Hispanic (80%), and Roman Catholic (80%). The most common reasons for learning CrM (women) were to use a natural method for family planning (91%), for moral/ethical/religious reasons (70%), the lack of side effects (71%), or insight into the menstrual cycle and fertility (62%). Women and men intended to have a mean of three and two additional children, respectively. Of women, 21% intended to have a child within a year and 60% between 1 and 3 years. The mean positive childbearing motivation score was 3.3 for both women and men (range 1–4, with 4 being most positive).
Conclusion: Couples beginning use of the CrM to avoid pregnancy have high levels of motivation, desire, and intention for future childbearing. The CEIBA study has prospective measures of desires, intentions, and sexual/fertility behaviors for up to 1 year. We will assess the impact of desires, intentions, and behaviors on the pregnancy rates among these couples.
Introduction
Methods of family planning based upon identifying the days of potential fertility in women, known as natural family planning (NFP) or fertility awareness-based methods (FABMs), are an important option for family planning (1–4). These methods use various biomarkers to identify days in the menstrual cycle when intercourse is likely to result in pregnancy. Among their advantages are low cost, lack of side effects, and the education they can provide users about their own reproductive physiology and health (5–7). By definition, NFP refers to avoiding pregnancy through abstinence from genital contact (8, 9), while FABM allows for the use of barriers or withdrawal on fertile days—as well as abstinence—when pregnancy avoidance is intended (10, 11).
In addition to their use in avoiding pregnancy, FABM or NFP methods are unique among family planning methods in their additional ability to help couples try to time pregnancy (12–14). Indeed, in population-based studies, potential interest in these methods has been greater for the purpose of conceiving than of avoiding conception (15, 16). Many, perhaps most, long-term users of FABM or NFP methods will at different times use the method both to avoid pregnancy and to conceive, transitioning between these intentions (17–19).
The Creighton Model FertilityCareTM System (CrM), a NFP method based on initial research at St. Louis University, was further developed and implemented by Dr. Hilgers and colleagues at the Creighton University Medical Center and the Pope Paul VI Institute for the Study of Human Reproduction, Omaha, Nebraska (20, 21). It is based on standardized observation and recording of vaginal discharge (especially from cervical mucus) and vaginal bleeding, interpretation of these biomarkers for fertility and health status, and teaching using a case management approach (22). The CrM instructors are called Creighton Model FertilityCareTM Practitioners (CrM FCPs). CrM instruction is provided through Creighton FertilityCareTM Centers; in the United States and Canada, these are registered through FertilityCareTM Centers of America, while in other parts of the world they are registered through FertilityCareTM Centers International (www.fertilitycare.org). Additionally, a system of medical protocols called natural procreative technology (NaProTechnology) has been developed for supporting women with gynecologic problems and couples with infertility and integrated with the CrM (23). Integral to the teaching of the CrM is emphasizing to the couples that they have radical autonomy to choose to have intercourse or not on any given day with full knowledge of the possibility of pregnancy on that day (“selective intercourse”) and that there is no requirement for what they “should” do with regard to possible pregnancy outcomes (22).
Several previous studies have been published regarding the CrM’s effectiveness in both promoting or preventing pregnancy (24–30). These studies were based on assessments of the couples’ behavior and knowledge; they made very limited assessment of the relationships between intentions, behaviors, and pregnancy rates. The study of Creighton Model Effectiveness, Intentions, and Behaviors Assessment (CEIBA) was conducted to assess the spectrum of fertility motivations, intentions, and fertility-related sexual behaviors and quantify their impact on effectiveness in avoiding or achieving pregnancy among new users of the CrM with initial pregnancy avoidance intentions. In this paper, we report on the recruitment for CEIBA, baseline demographic characteristics, and the childbearing motivations and intentions of women and men (heterosexual couples) who started use of the CrM with the initial intention of avoiding pregnancy. We also describe the protocol for assessing follow-up intentions, behaviors, and pregnancy.
Materials and Methods
Design, Setting, Timeline, and Approval
The CEIBA study was a prospective cohort study implemented in 17 different CrM FertilityCareTM Centers throughout the United States and Canada. Of the participating CrM centers, eight were directly connected to a Catholic institution, while the other nine were independent organizations, most with strong networking connections to local Catholic communities. Participating CrM FertilityCareTM Centers and CrM FCPs are listed in the acknowledgments. All new or returning couples seeking instruction in the CrM were screened for study eligibility with a screening questionnaire. The study began enrollment in September 2009 and closed enrollment in December 2011. Some of the participating CrM FertilityCareTM centers joined the study later, after September 2009; all finished enrollment by December 2011. The study was reviewed and approved by the University of Utah Institutional Review Board (IRB) number 00034487. All local participating sites either had local IRB approval or an authorization agreement relying upon the University of Utah IRB.
Recruitment
Couples were recruited from among those normally presenting to the participating centers to learn the CrM. Participating CrM FertilityCareTM Centers used posters and brochures to inform their clients and potential clients about the study. In addition, we recruited online through blog posts, websites, and a Facebook page. Inquiries from the online recruiting were referred to a participating CrM FertilityCareTM Center for CrM instruction and study screening.
Eligibility and Consent
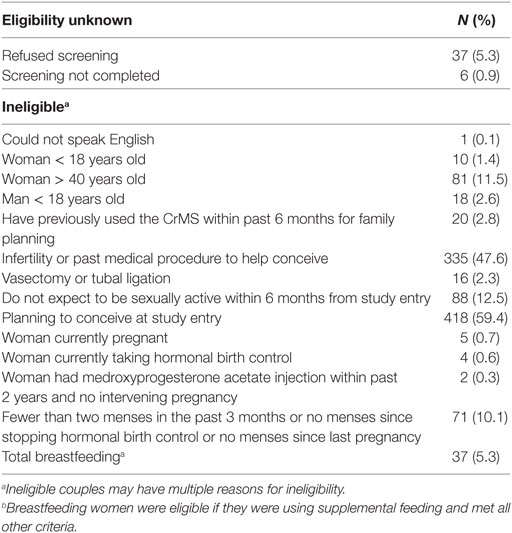
We attempted to screen all couples presenting to the participating FCPs for eligibility. Initially, couples were eligible for this study if they were learning CrM for the first time with the stated intention of avoiding pregnancy. Screening for eligibility was performed by the CrM FCPs, using a screening questionnaire. Specific exclusion criteria are listed in Table 1. These were designed to exclude couples who had possible reduced fecundity, had previously used the CrM, were not planning to be sexually active within 6 months, could not communicate adequately to complete study procedures, or were under 18 years of age.
In August 2010, after the study had been enrolling for 1 year and about 100 couples had been enrolled, eligibility criteria were expanded to include couples who were returning to CrM use after 6 months or more without using CrM (for example, after a pregnancy). This change was made to maximize recruitment, while still maintaining a focus on couples who were beginning use of the CrM to avoid pregnancy.
An informed consent document was completed by participants, either on paper or online, and was signed by both partners. If completed on paper, it was signed by the FCP instructing the couple; if completed online, a study staff member called each partner to verify their consent and answer any questions. If the woman did not complete the consent form within 6 weeks of the first CrM follow-up visit or within 6 weeks of the first menstrual flow for postpartum women, they were not enrolled in the study.
Standard Creighton Model Procedures and Instruments
Couples were instructed in the CrM according to standard procedures. Briefly, couples attended an introductory session (usually in a small group setting), where the scientific underpinnings of the CrM were presented, reading materials were given, and instructions were given for the woman to begin making and interpreting daily vulvar observations. Follow-up sessions were always conducted individually with the couple and a CrM FCP and were recommended to occur about every 2 weeks for the first four follow-ups; subsequent follow-ups were scheduled at longer intervals, for up to eight follow-ups over 1 year. Standard CrM records included the following (22).
• the general intake form, filled out by the couple at entry and containing demographic and reproductive history;
• the CrM user chart (daily diary record) kept by the couple to document vulvar observations, the designation of a day as “fertile” or “infertile” (by use of interpretive stamps), as well as acts of sexual intercourse;
• the CrM follow-up form, a standardized teaching and assessment record used by the CrM FCP during the follow-up sessions;
• an assessment of dimensions of sexual intimacy filled out during two different follow-ups by the couple; and
• CrM pregnancy evaluation forms, described further below under Outcome.
Copies of each of these records were obtained and entered into an electronic study database.
Procedures and Instruments Unique to This Study
• For all new or returning couples for CrM instruction, CrM FCPs filled out a study screening questionnaire, which was used to determine eligibility, as described above (see also Table 1).
• An informed consent document was completed as described above.
• After consent, an entrance questionnaire was completed online, with a separate questionnaire for the woman and the man. This questionnaire contained additional information about demographics and medical history, and questions about childbearing motivations, desires, and behaviors. These include a series of questions which are averaged to form two scaled measures for positive childbearing motivation and negative childbearing motivation. There are also a series of questions about childbearing desires and childbearing intentions. These scales and associated questions have been previously used and validated in other studies (31–34).
• At or near the beginning of each menstrual cycle, a brief cycle questionnaire was completed online, with a separate questionnaire for the woman and the man. This questionnaire assessed intention regarding pregnancy for the coming cycle, and use of any other family planning or fertility tracking methods in the prior cycle, including condoms, withdrawal, urine LH kits, or basal body temperature.
• Upon exit from the study, the couple completed an online exit questionnaire. There were four versions of this questionnaire: for pregnancy or no pregnancy during the study, each separately for the woman and the man. This questionnaire included items about factors around the use of CrM during the study, including repeating questions about use of other family planning or fertility tracking methods. For couples with a pregnancy, it had questions about the pregnancy.
Outcome
The primary outcome for this study was a clinical pregnancy, as identified by the woman or man. There was active surveillance for pregnancy throughout the study follow-up in three ways: (1) the CrM user chart documented the onset of each menstrual flow and the length of each postovulatory phase (i.e., luteal phase) throughout the study and through the first menstrual flow beyond 1 year whenever possible; (2) the beginning of cycle questionnaire documented the date of the onset of each menstrual flow, independently of the CrM user chart; and (3) the couples attended periodic follow-up sessions with the FCPs. For each identified pregnancy, we reminded and encouraged study participants to contact the CrM FCPs to complete a standard CrM pregnancy evaluation, documented using the CrM pregnancy evaluation form (35). Where circumstances did not allow the original CrM FCP to complete the pregnancy evaluation, we arranged for the study participant to receive a pregnancy evaluation with a different CrM FCP. The CrM pregnancy evaluation form is designed to be completed for every CrM pregnancy. It records dates and results of pregnancy tests, physician encounters, pregnancy symptoms, the couple’s opinion of which day of intercourse resulted in pregnancy and other circumstances of the pregnancy. There is a “long form” and a “short form” version of the pregnancy evaluation form; for the CEIBA study, we requested that the “long form” version should be used. It is a standard CrM procedure for some pregnancies to receive a second pregnancy evaluation by a different CrM FCP (35); in these cases, we collected both pregnancy evaluation forms.
Independently of the pregnancy evaluation form, when pregnancies occurred we sent an online pregnancy version of the study exit questionnaire to both the woman and the man, who completed it directly online, as described above.
Follow-up and Exit
Couples began to contribute time into the study during the cycle in which they first recorded any sexual intercourse. Some engaged couples were not sexually active at the time they attended the introductory session; they were entered into the active follow-up of the study when they became sexually active, if occurring within 6 months. Couples were followed until 1 year from the first sexual intercourse, voluntary withdrawal from the study, withdrawal by investigators because the couple did not provide data for the study, or pregnancy. Couples were not eligible to enter the study again after pregnancy, regardless of the outcome of the pregnancy.
Statistical Analysis
We used descriptive statistics to summarize characteristics and reproductive history of study participants at the entrance to the study (and start of CrM use), as well as measures of their childbearing motivations, desires, and intentions; similar methods were used to examine reasons for exclusion from the study for those not eligible. Using the chi-square statistic, we compared demographic and reproductive characteristics of both women and men who were consented versus not consented for the study. We constructed multivariate linear regression models to examine predictors of number of future children desired and number of future children intended, for both women and men. We initially included all variables measured to assess to pregnancy and childbearing motivations; in the final models we only included those variables that were significant to at least P = 0.10 in at least one of the final models.
Results
A total of 1,132 new or returning couples were seen across all centers: 1,090 (96%) were screened, and of those screened, 429 (39%) were eligible couples of which 305 women (71%) consented to the study, along with 290 of their male partners (95%). The number of couples enrolled per month ranged from 0 to 30, with a median of 10 enrollments per month. The 305 women were enrolled across all 17 sites. The minimum number enrolled per sites was 2, the maximum was 60, and the median enrollment per site was 16. Table 1 lists reasons for the 704 women excluded from the study (43 who did not complete screening and 661 who were not eligible), including the reasons for not completing screening or for ineligibility.
Most participants were engaged (39%) or married (51%), college graduates (77% of women), Caucasian non-Hispanic (80% of women), and Catholic (80% of women). There were demographic differences between couples who enrolled in the CEIBA study, and couples seen during the same time who were not enrolled. Women who enrolled were more likely to be of age 20–29 years, to be engaged (versus married or single), to have a college-level education, to have lower household income, to be Catholic, and to have no prior pregnancy or live birth (Table 2). Similar patterns were found for men’s age, marital status, education, and religion. There was a high level of religious involvement: 79% of women and 67% of men reported attending religious or worship service at least once per week. The mean age of women enrolled was 27.8 years.
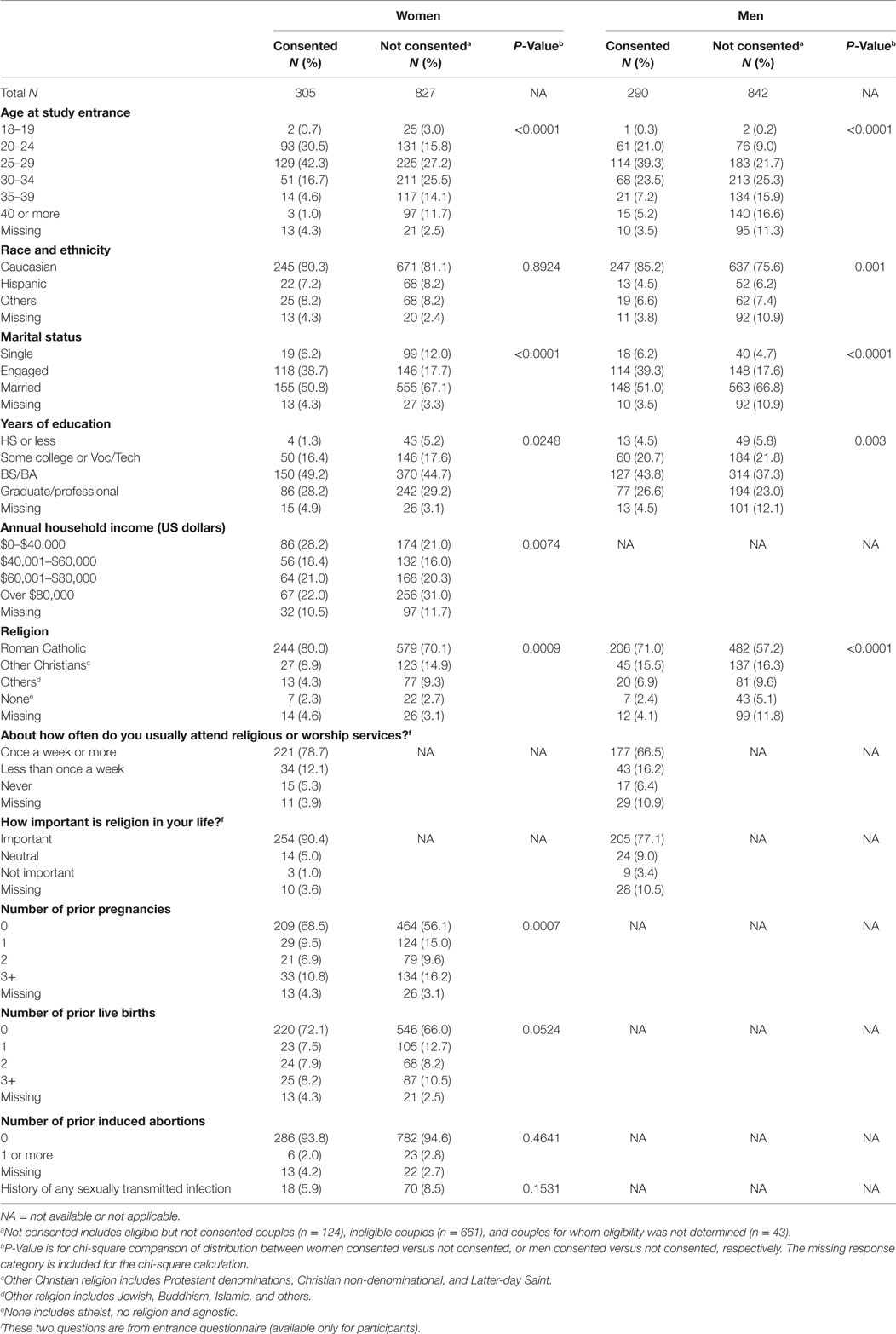
Table 2. Demographic and reproductive characteristics of women and men consented and not consented for the CEIBA study.
The most common previously used family planning methods were the oral contraceptive pill (60%) and the male condom (57%) (Table 3). Twenty-two women had previously used the CrM to avoid pregnancy, and 11 women had previously used the CrM to conceive. Overall, there were 27 of all consented women who had previously used the CrM in either way, representing 8.9% of all women enrolled. These women were eligible and enrolled under the expanded criteria (described above) because they were returning to use of the CrM after a pregnancy or other time period of not using the CrM.
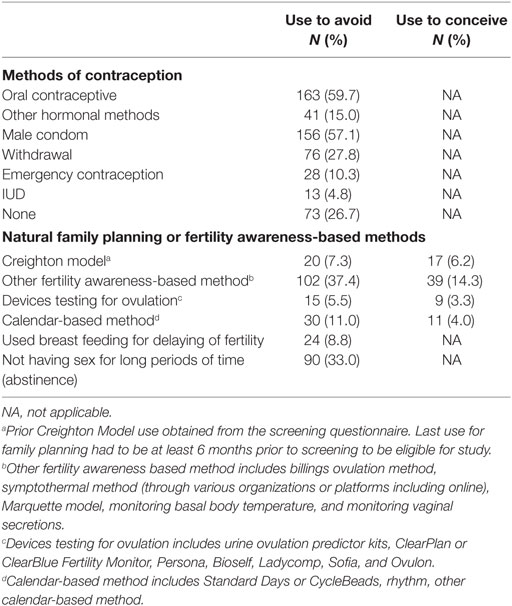
Table 3. Prior use of family planning methods, reported on the entrance questionnaire (N = 273 women).
Reasons reported for starting (or resuming) the use of the CrM are indicated in Table 4. For women, the most common reasons were to use a natural method (91%), for moral/ethical/religious reasons (70%), the lack of side effects (71%), or insight into the menstrual cycle and fertility (62%). For men, the most common reasons were to use a natural method (76%), moral/ethical/religious reasons (70%), for wife/partner’s choice (62%), and lack of side effects (61%).
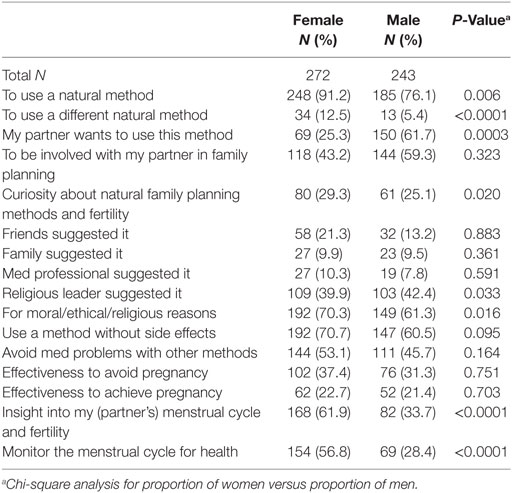
Table 4. Women’s and men’s reasons for choosing to learn the Creighton Model FertilityCareTM System.
Desires, intentions, and motivations for future childbearing are presented in Table 5. At the median, women intended to have three additional children (range 0–11); while men intended to have two additional children (range −2 to 10). About one in five women (21%) intended to have a child within a year, and 60% between 1 and 3 years. The majority of women reported that their closest family members (55%) and closest friends (57%) would be in favor of them having a child at the present time. The mean positive childbearing motivation score for both women and men was 3.3 (range 1–4, with 4 being most positive).
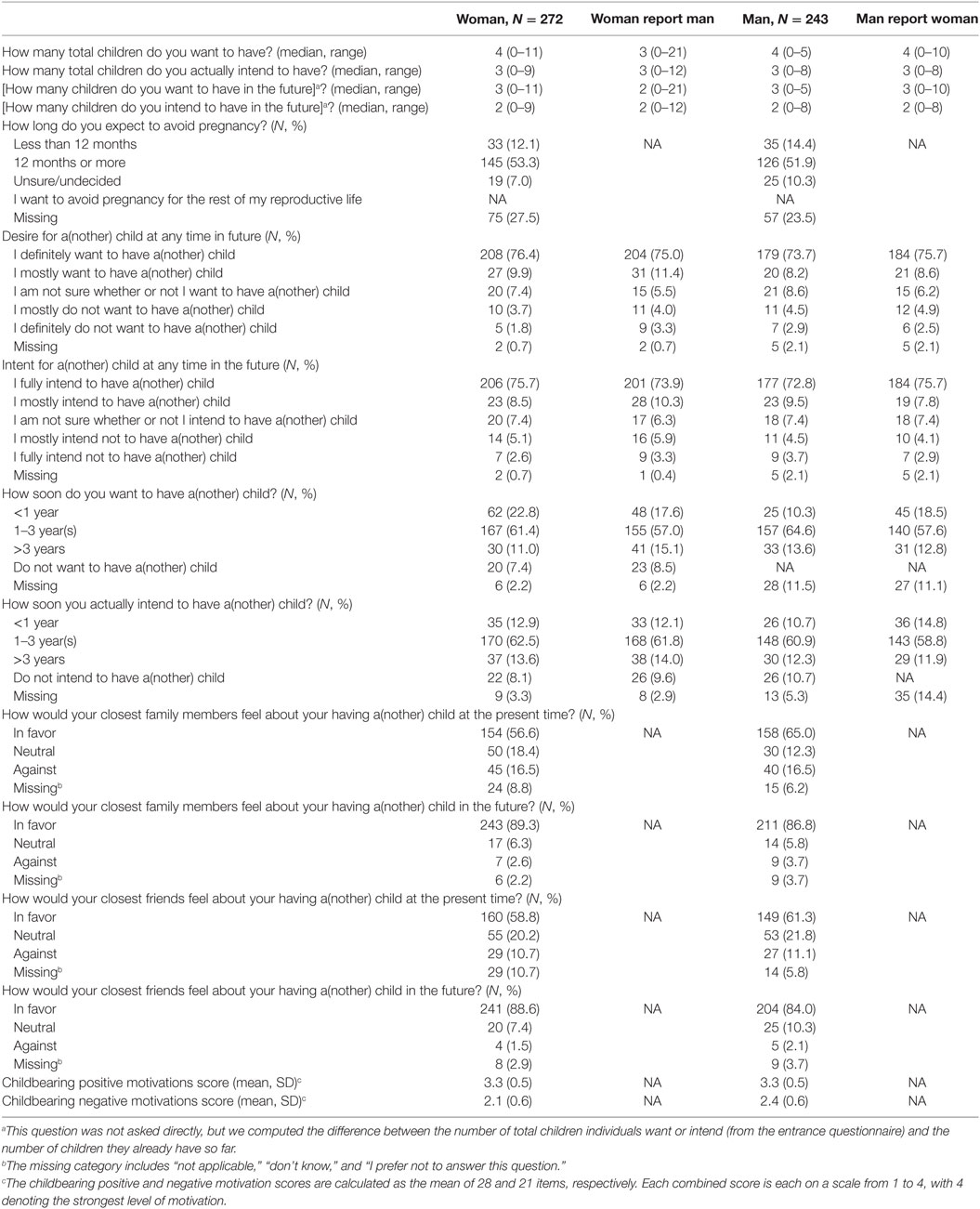
Table 5. Women and men’s pregnancy and childbearing motivations and intentions at entry to the CEIBA study.
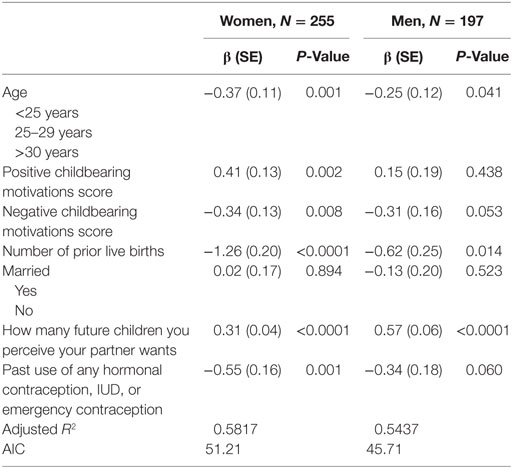
We examined factors related to desire for children, with results presented in Table 6. In the each of the models for Tables 6 and 7, we included all variables that were significant in any one of the models. For both women and men, the number of future children desired was positively correlated with positive childbearing motivation scores and perception of spouse or partner’s desired number of future children. Number of future children desired was negatively correlated with age, negative childbearing motivations, number of prior live births, and past use of any hormonal contraception, IUD, or emergency contraception. Marital status was not correlated. Altogether, these variables accounted for over half of the variance (adjusted R2) for number of future children wanted for both women and men.
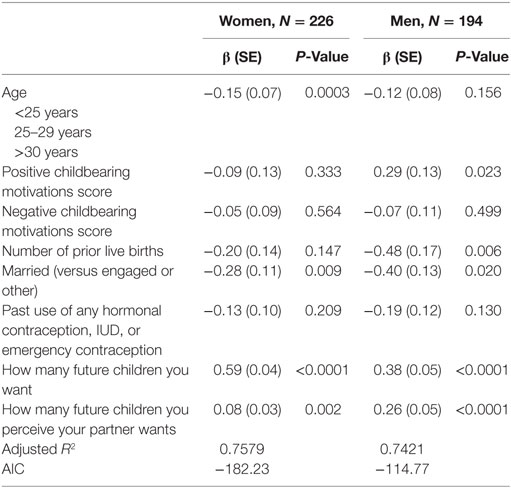
We also examined factors related to intention for children, with results presented in Table 7. As expected, the number of future children intended was most strongly correlated with number of future children wanted. Positive correlations were also present with perception of number of future children wanted by the spouse or partner, especially for men. There was a negative association for being married (in comparison with mostly engaged couples), and number of prior live births (for men only). For men, there was a positive association with positive childbearing motivations, but no other association with childbearing motivations score for women and men. Altogether, these variables accounted for about 75% of the variance (adjusted R2) for number of future children intended for both women and men.
Discussion
We recruited 305 couples to a prospective study of the CrM for family planning. The majority was engaged or married, college graduates, and Catholic. All CrM centers serve women and couples of any faith (or no faith), but the association with Catholic institutions means that the exposure and accessibility to the CrM is greater for Catholic couples. In addition, the majority of women (70%) and men (61%) cited moral/ethical/religious reasons as a motivator for learning the CrM, and many women (40%) and men (42%) indicated that they were motivated by the method being suggested by a religious leader. This is consistent with a study in Germany and Poland which found that, while interest in NFP was not associated with religious motivation, the actual use of NFP was associated with Catholic affiliation (17).
Consistent with eligibility criteria for the study, all couples were originally planning to avoid (or space) pregnancy, but the vast majority had high levels of childbearing motivation, desire, and childbearing intention for the near future. Among women, 69% wanted a child within 3 years, while 71% of men wanted a child within 3 years. It is instructive to compare the positive and negative childbearing motivation scores of the CEIBA couples with those of 401 couples in California in a 1995 study (33). In the California study, all the couples were married: half had no children and had been married for a mean of 3.1 years, and half had one child and had been married for a mean of 4.7 years; also they were somewhat older and wealthier than the couples in the CEIBA study. The mean positive childbearing motivation score in the California study was 2.9 and 2.8 for women and men, respectively. The mean negative childbearing motivation score was 2.2 and 2.4, respectively. The mean total number of children desired was 2.5 for both women and men. In comparison, our sample had higher positive childbearing motivation scores (mean 3.3 for both women and men), lower negative childbearing motivation scores (mean 2.1 and 2.4 for women and men, respectively), and a much higher total number of children wanted (median of 4 for women and 3 for men). This high level of childbearing motivations, desires, and intentions may represent a strong proceptive influence from high levels of involvement in Catholicism and perhaps other religions (36, 37). In addition, CEIBA participants reported that friends and family members were highly supportive of childbearing.
A minority (39%) of screened new users at the participating centers was eligible for the study. Among those who were ineligible, 59% were learning the CrM to try to conceive and 48% had a medical history of infertility. This represents a significant shift from a study conducted more than 10 years ago across eight CrM centers in the United States, which enrolled new CrM users from 1996 to 2000 (38). In that study, only 19% of new users were trying to conceive at study entry. This shift may also be consistent with current trends for the use of fertility apps for smart phones and other personal mobile computing devices, most of which seem to emphasize seeking pregnancy rather than avoiding pregnancy (1).
Because NFP methods can be used either to avoid pregnancy or to conceive, assessing users’ intentions is essential to assessing any NFP method’s effectiveness (12, 13, 18, 39). The CrM educational materials and interactions emphasize radical autonomy for the couple, who decides whether to use it to avoid pregnancy or to conceive (28, 40). Consistent with this philosophy, past evaluations of pregnancy rates with the CrM have been based on behavioral evaluation, rather than stated intentions (25, 28, 29). This contrasts with contraceptive methods that have only the purpose of avoiding pregnancy, and in which prospectively stated intentions have been standard for assessing pregnancy rates (41). One of the purposes of the CEIBA study is to compare intention-based measures of pregnancy rates with behaviorally based measures.
According to the well-established Theory of Reasoned Action and similar theories, intentions are largely driven by desires, and are also influenced by social norms. In turn, desires are largely formed by motivations, as well as other factors (42, 43). Our findings for number of pregnancies wanted and intended by women and men are consistent with this framework. In future analyses, we will assess quantitatively the relationships between desires, intentions, behaviors, and fertility outcomes (i.e., pregnancy) in this study population.
Conclusion
Women/couples beginning use of the CrM to avoid pregnancy within the United States and Toronto, Canada are mostly young, religious, engaged or newly married, Roman Catholic, and have high levels of motivation, desire, and intention for future childbearing, with the large majority of both women and men wanting a child within 3 years. The CEIBA study assessed these factors at baseline and implemented prospective measures of each of desires, intentions, and sexual/fertility behaviors for up to 1 year after beginning sexual activity. These data will allow us to assess the impact of desires, intentions, and behaviors on the incidence of pregnancy among these couples.
Ethics Statement
The study was reviewed and approved by the University of Utah Institutional Review Board, IRB number 00034487. All local participating sites either had local IRB approval or an authorization agreement relying upon the University of Utah IRB.
Author Contributions
JS was the principal investigator for designing and implementing the CEIBA study, directed the data analysis, and wrote the manuscript. CP served as coinvestigator to conduct the study, provided guidance for the analysis, and helped revise the manuscript.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We thank the following Creighton Model FertilityCareTM Centers and Creighton Model FertilityCareTM Practitioners for participating in this study: Marguerite d’Youville FertilityCareTM Services (formerly FertilityCareTM Services of St. Joseph Hospital), Manchester, NH, USA: Kathy Rivet; FertilityCareTM Center of Omaha, Omaha, NE, USA: Jeanice Vinduska, Sue Elser, Andrea Mack, Gerianne Jensen, Sarah Aurit, VanNessa Krueger, and Emily Oxley; Intermountain FertilityCareTM Services, Salt Lake City, UT, USA: Kathy Davis, Vanessa Hecker, and Colette Child; FertilityCareTM Center of Kansas City, Kansas City, MO, USA: Sharon Drakes, Lisa Grasing, Angela Linville, and Stacy Mulder; St. John’s Mercy Medical Center Department of FertilityCareTM Services, St. Louis, MO, USA: Diane Daly, Ann Prebil, Jeanne Stoll, Mary Sharpe, Lucy Harris, Leah Baute, Mary Schurk, and Jessica Turntine; St. Joseph FertilityCareTM Center, Albuquerque, NM, USA: Angel Garcia and Jasmine Lyle; FertilityCareTM Center, Diocese of Lincoln, NE, USA: Michele Chambers, Kathy Burr, Lynn Kinkaid, Cyndi Ojeda, and Michelle Keuten; Northland Family Programs: A FertilityCareTM Center, Duluth, MN, USA: Joyce Cagle and Mary Marquis; Marguerite Bourgeoys FertilityCareTM Programme, Toronto, ON, Canada: Karen Hemingway, Vania Branker, Leslie Green, Laura Ostoya, Tanzel Picard, Denise Chun, Pilar Gordillo Sarmiento, and Sylvia Heald; FertilityCareTM Services: Diocese of Charleston, SC, USA: Nancy McGrath; Sacramento Diocese FertilityCareTM Services, Sacramento, CA, USA: Nancy Matteoli; Twin Cities FertilityCareTM Center, Minneapolis-St. Paul, MN, USA: Jennifer Mak, Sara Rogers, Amy Cummings, Brigid Barrett, and Beckie Ruff; Caritas FertilityCareTM Center, Pataskala, OH, USA: Lisa Ely and Emily Mauro; FertilityCareTM Center of the Upper Ohio Valley, Weirton, WV, USA: Kathy Hirkala; FertilityCareTM Center of North Texas, Fort Worth, TX, USA: Tammy Oropeza and Rosemary Mendiola; Women’s FertilityCareTM Services of Houston, TX, USA: Elizabeth Martinez and Laura Hilgers; Center for Women’s Health, Spirit FertilityCareTM Services, Camp Hill, PA, USA: Dorice Millar, Kim Lane, Erin Donley, Tammy Barbush, Brandi Defelice, and Kathy Rhoades. The following persons were study staff who contributed to the conduct and/or analysis of the study: Becky Crockett, Daisy Krakowiak, Michael Lowe, Nirupma Singh, Kaitlin Carruth, Kathryn Szczotka, Jared Hansen, Iris Musso, Sakineh Najmabadi, Yizhe Xu, and Jiqiang Wu. Xioaming Sheng served as a biostatistician during the design phase of the study. Sarah Pollard assisted with editing of the manuscript. We thank the experts who served as consultants to this study: Thomas W. Hilgers, MD, Warren B. Miller, MD, and James Trussell, PhD.
Funding
This study was funded primarily by the Office of Family Planning, Office of Population Affairs (Grant # 1FPRPA006035), and United States Department of Health and Human Services. Funding for the inclusion of the Toronto site was provided by the University of Utah, Department of Family and Preventive Medicine, Health Studies Fund. Additional funding for analysis of study data was provided by the American Academy of FertilityCareTM Professionals, the Catholic Medical Association, Linacre Fund, and the following individual donors: Phyllis White, Stephanie Buck, Julianna Jervis, Andrea Mack, Susan Gloss, Kathy Burr, Laura Weidner, Eileen Sirois, Robert Nerbun, Robert Chasuk, Linda Holt, Vanessa Hecker, Eaton Green, Elizabeth Tham, Meg Yates, Ladean Barnes, Laurie Weitzel, Nancy Malo, Robert Motley, Nora Ponder, Amanda Cox, Joyce Gibbar, Mary Marquis, Eric Donley, Gretchen Marsh, Denise Seeger, David Smith, Jeanne Stoll, Marguerite Duane, Debra Gramlich, Ann Prebil, Stacy Mulder, Michael Dixon, Donna Paolucci, Inge Collins, Brigette Diemand, Peter Danis, and Angela Linville.
References
1. Duane M, Contreras A, Jensen ET, White A. The performance of fertility awareness-based method apps marketed to avoid pregnancy. J Am Board Fam Med (2016) 29(4):508–11. doi:10.3122/jabfm.2016.04.160022
3. Manhart MD, Duane M, Lind A, Sinai I, Golden-Tevald J. Fertility awareness-based methods of family planning: a review of effectiveness for avoiding pregnancy using SORT. Osteopath Fam Physician (2013) 5(1):2–8. doi:10.1016/j.osfp.2012.09.002
4. Pallone SR, Bergus GR. Fertility awareness-based methods: another option for family planning. J Am Board Fam Med (2009) 22(2):147–57. doi:10.3122/jabfm.2009.02.080038
5. Vigil P, Blackwell LF, Cortés ME. The importance of fertility awareness in the assessment of a woman’s health: a review. Linacre Q (2012) 79(4):426–50. doi:10.1179/002436312804827109
6. Pyper CM. Fertility awareness and natural family planning. Eur J Contracept Reprod Health Care (1997) 2(2):131–46. doi:10.3109/13625189709167468
7. Oddens BJ. Women’s satisfaction with birth control: a population survey of physical and psychological effects of oral contraceptives, intrauterine devices, condoms, natural family planning, and sterilization among 1466 women. Contraception (1999) 59(5):277–86. doi:10.1016/S0010-7824(99)00034-7
8. Fehring RJ, Schneider M. Comparison of abstinence and coital frequency between 2 natural methods of family planning. J Midwifery Womens Health (2014) 59(5):528–32. doi:10.1111/jmwh.12216
9. Che Y, Cleland JG, Ali MM. Periodic abstinence in developing countries: an assessment of failure rates and consequences. Contraception (2004) 69(1):15–21. doi:10.1016/j.contraception.2003.08.006
10. World Health Organization. Medical Eligibility Criteria for Contraceptive Use. Geneva, Switzerland: World Health Organization (2015).
11. Grimes DA, Gallo M, Grigorieva V, Nanda K, Schulz K. Fertility awareness-based methods for contraception. Cochrane Database Syst Rev (2004) 4:CD004860. doi:10.1002/14651858.CD004860.pub2
12. Lamprecht V, Trussell J. Natural family planning effectiveness: evaluating published reports. Adv Contracept (1997) 13(2–3):155–65. doi:10.1023/A:1006595703472
13. Hilgers TW. The statistical evaluation of natural methods of family planning. Int Rev Nat Fam Plann (1984) 8(3):226–64.
14. Weschler T. Taking Charge of Your Fertility: The Definitive Guide to Natural Birth Control, Pregnancy Achievement, and Reproductive Health. 20th Anniversary Edition. New York: Harper Collins (2015). 560 p.
15. Stanford JB, Lemaire JC, Thurman PB. Women’s interest in natural family planning. J Fam Pract (1998) 46(1):65–71.
16. Stanford JB, Hutchinson AG, Payne JG. Utah couples’ potential use of natural family planning. Utahs Health Annu Rev (2003) 9(1):40–5.
17. Mikolajczyk RT, Stanford JB, Rauchfuss M. Factors influencing the choice to use modern natural family planning. Contraception (2003) 67(4):253–8. doi:10.1016/S0010-7824(02)00490-0
18. Klaus H, Fagan MU. Natural family planning: an analysis of change in procreative intention. J Am Med Womens Assoc (1982) 37(9):231–41.
19. Colombo B, Masarotto G. Daily fecundability: first results from a new data base. Demogr Res (2000) 3(5):39. doi:10.4054/DemRes.2000.3.5
20. Hilgers TW, Prebil AM. The ovulation method – vulvar observations as an index of fertility/infertility. Obstet Gynecol (1979) 53(1):12–22.
21. Hilgers TW. Introduction to the Creighton model system. In: Hilgers TW, editor. The Medical and Surgical Practice of NaProTechnology. Omaha: Pope Paul VI Institute Press (2004). p. 43–56.
22. Hilgers TW, Daly KD, Hilgers SK, Prebil AM. Creighton Model FertilityCare System: A Standardized, Case Management Appproach to Teaching, Book 1. 2nd ed. Omaha, NE: Pope Paul VI Institute Press (2002).
23. Hilgers TW. What is NaProTechnology? In: Hilgers TW, editor. The Medical and Surgical Practice of NaProTechnology. Omaha: Pope Paul VI Institute Press (2004). p. 19–28.
24. Doud J. Use-effectiveness of the Creighton model of NFP. Int Rev Nat Fam Plann (1985) 9(1):54–72.
25. Hilgers TW, Stanford JB. Creighton model NaProEducation technology for avoiding pregnancy. Use effectiveness. J Reprod Med (1998) 43(6):495–502.
26. Howard MP, Stanford JB. Pregnancy probabilities during use of the Creighton Model FertilityCare System. Arch Fam Med (1999) 8(5):391–402. doi:10.1001/archfami.8.5.391
27. Fehring RJ, Lawrence D, Philpot C. Use effectiveness of the Creighton-model ovulation method of natural family planning. J Obstet Gynecol Neonatal Nurs (1994) 23(4):303–9. doi:10.1111/j.1552-6909.1994.tb01881.x
28. Stanford JB. Measuring effectiveness and pregnancy rates of the CrMS. In: Hilgers TW, editor. The Medical and Surgical Practice of NaProTechnology. Omaha: Pope Paul VI Institute Press (2004). p. 215–31.
29. Hilgers TW, Stanford JB. Achieving-related pregnancy rate and evidence to its ability to be naturally adaptable. In: Hilgers TW, editor. The Medical and Surgical Practice of NaProTechnology. Omaha: Pope Paul VI Institute Press (2004). p. 231–40.
30. Stanford JB, Smith KR, Varner MW. Impact of instruction in the Creighton Model FertilityCare System on time to pregnancy in couples of proven fecundity: results of a randomised trial. Paediatr Perinat Epidemiol (2014) 28(5):391–9. doi:10.1111/ppe.12141
31. Miller WB. Reproductive decisions: how we make them and how they make us. Adv Popul (1994) 2:1–27.
32. Miller WB. Childbearing motivations, desires, and intentions: a theoretical framework. Genet Soc Gen Psychol Monogr (1994) 120(2):223–58.
33. Miller WB. Childbearing motivation and its measurement. J Biosoc Sci (1995) 27(4):473–87. doi:10.1017/S0021932000023087
34. Miller WB, Pasta DJ. Behavioral intentions: which ones predict fertility behavior in married couples? J Appl Soc Psychol (1995) 25(6):530–55. doi:10.1111/j.1559-1816.1995.tb01766.x
35. Hilgers TW, Hilgers SK, Prebil AM, Daly KD. Creighton Model Fertilitycare System: A Standardized, Case Management Approach to Teaching-Book 2: Advanced Teaching Skills. Omaha, NE: Pope Paul VI Institute Press (2003).
36. Adsera A. Marital fertility and religion in Spain, 1985 and 1999. Popul Stud (2006) 60(2):205–21. doi:10.1080/00324720600684817
37. Adsera A. Reply to the note by Neuman ‘Is fertility indeed related to religiosity?’ Popul Stud (2007) 61(2):225–30. doi:10.1080/00324720701300339
38. Stanford JB, Smith KR. Characteristics of women associated with continuing instruction in the Creighton Model FertilityCare System. Contraception (2000) 61(2):121–9. doi:10.1016/S0010-7824(00)00084-6
39. Brennan JJ, Klaus H. Terminology and core curricula in natural family planning. Fertil Steril (1982) 38(1):117–8. doi:10.1016/S0015-0282(16)46409-5
40. Hilgers TW. Achieving- and avoiding-related behavior (use). In: Hilgers TW, editor. The Medical and Surgical Practice of NaProTechnology. Omaha: Pope Paul VI Institute Press (2004). p. 173–6.
41. Trussell J, Kippley JF, Hilgers TW, Stanford JB. Analyzing contraceptive failure [letters]. J Reprod Med (1999) 44(5):478–81.
42. Ajzen I, Fishbein M. Understanding Attitudes and Predicting Social Behavior. Englewood, NJ: Prentice Hall (1980). p. 1–264.
Keywords: natural family planning, family planning, behavioral methods, cervical mucus method, knowledge, attitudes, practice, pregnancy intentions
Citation: Stanford JB and Porucznik CA (2017) Enrollment, Childbearing Motivations, and Intentions of Couples in the Creighton Model Effectiveness, Intentions, and Behaviors Assessment (CEIBA) Study. Front. Med. 4:147. doi: 10.3389/fmed.2017.00147
Received: 27 May 2017; Accepted: 18 August 2017;
Published: 08 September 2017
Edited by:
Patrick P. Yeung, Saint Louis University, United StatesReviewed by:
Maria Wolfs, University of Toronto, CanadaChristine Louise Cimo Hemphill, Gianna Center of the Gulf South, United States
Mark Francis Stegman, St. Anthony’s Medical Center, United States
Copyright: © 2017 Stanford and Porucznik. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Joseph B. Stanford, joseph.stanford@utah.edu
 Joseph B. Stanford
Joseph B. Stanford Christina A. Porucznik
Christina A. Porucznik