- Institute of Medical Microbiology, Semmelweis University, Budapest, Hungary
The major international sequence types/lineages of methicillin-resistant Staphylococcus aureus (MRSA), extended-spectrum β-lactamase (ESBL)-producing Klebsiella pneumoniae and ESBL-producing E. coli were demonstrated to have been advanced by favorable fitness balance associated with high-level resistance to fluoroquinolones. The paper shows that favorable fitness in the major STs/lineages of these pathogens was principally attained by the capacity of evolving mutations in the fluoroquinolone-binding serine residues of both the DNA gyrase and topoisomerase IV enzymes. The available information on fitness balance incurred by individual and various combinations of mutations in the enzymes is reviewed in multiple species. Moreover, strong circumstantial evidence is presented that major STs/lineages of other multi-drug resistant bacteria, primarily vancomycin-resistant Enterococcus faecium (VRE), emerged by a similar mechanism. The reason(s) why the major ST/lineage strains of various pathogens proved more adept at evolving favorable mutations than most isolates of the same species remains to be elucidated.
Introduction
It is well-established that major international clones and lineages of various multi-drug resistant hospital-associated pathogens emerged during the past three decades. High-risk clonal complexes of various species of bacteria have spread in the healthcare setting across large swathes of continents. We have been witnessing a dramatic expansion of some global clones/lineages of methicillin-resistant Staphylococcus aureus (MRSA) (Nübel et al., 2011; Grundmann et al., 2014), extended-spectrum β-lactamase (ESBL)-producing Klebsiella pneumoniae (Damjanova et al., 2008; Holt et al., 2015), ESBL-producing E. coli (Pitout and DeVinney, 2017), Clostridium difficile (He et al., 2013), and vancomycin-resistant Enterococcus faecium (VRE) (Willems et al., 2005) among others.
The question arises what may account for the “attack and successful takeover” of the clones?
Though the determinants of clonal dynamics are certainly multiple one of them appears to be “more equal than others.” Recent reports investigating the fitness cost associated with resistance to fluoroquinolones in MRSA, ESBL-producing K. pneumoniae, ESBL-producing E. coli and C. difficile clearly showed that favorable fitness linked to high-level resistance to fluoroquinolones substantially contributed to the emergence of the major international clones/lineages of these pathogens (Reviewed by Fuzi, 2016).
While minor clone/lineage strains of MRSA, ESBL-producing K. pneumoniae, ESBL-producing E. coli and C. difficile suffer considerable fitness cost upon developing high-level resistance to fluoroquinolones the major clone isolates retain most of their vitality allowing to achieve dominance in facilities where fluoroquinolones are in extensive use (Horváth et al., 2012; Knight et al., 2012; Holden et al., 2013; Tóth et al., 2014; Johnson et al., 2015; Wasels et al., 2015). The abundant literature on the clonal dynamics of these pathogens remains in complete agreement with the proposed “fitness cost advantage” concept (Reviewed by Fuzi, 2016).
The next question concerns the mechanism: in what respect do the major clone strains of MRSA, ESBL-producing K. pneumoniae, ESBL-producing E. coli and C. difficile differ from minor clone isolates that permits the preservation of fitness even at high levels of resistance to fluoroquinolones?
The Dominance of the Double-serine Mutations
Researchers investigating the clonal dynamics of the above pathogens are in concordance that the crucial difference between the major and minor clone strains lies in the formers' ability (or the inability of the latter) to develop favorable but not detrimental genetic alterations mutations in the DNA gyrase and topoisomerase IV genes (Horváth et al., 2012; Holden et al., 2013; Tóth et al., 2014; Johnson et al., 2015; Wasels et al., 2015). This capacity seems to be a prerequisite: successful clones have to be able to evolve mutations which confer high-level resistance to fluoroquinolones without appreciably compromising fitness (Fuzi, 2016). Consequently, the recognition of how individual mutations in the quinolone resistance-determining regions (QRDRs) in the DNA gyrase (gyrA, gyrB) and topoisomerase IV (parC/grlA, parE/grlB) genes impact pathogens is of utmost importance.
The two most successful clones/lineages of hospital-associated (HA)-MRSA in Europe and the United States, the ST22 and the new lineage of ST8, both characteristically carry two identical mutations: gyrA Ser84Leu and grlA Ser80Phe (Table 1; Witte et al., 2001; Coelho et al., 2011; Holden et al., 2013; Alam et al., 2015), while minor clone/lineage strains—suffering considerable fitness cost upon developing high-level resistance to fluoroquinolones—were reported to harbor other mutations or additional genetic alterations compromising vitality (Horváth et al., 2012).
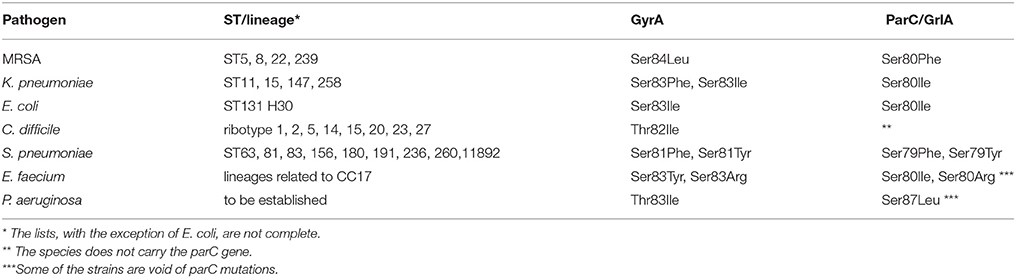
Table 1. Dominant serine/double-serine mutations in “fluoroquinolone-associated” STs/lineages of multi-drug resistant pathogens (see references in text).
Interestingly these double-serine mutations were also observed in rapidly expanding local strains (sublineages) of other sequence types of MRSA (Takano et al., 2008; Lozano et al., 2012; Chakrakodi et al., 2014; Khokhlova et al., 2015). Moreover, the double-serine mutations were reported the most frequent fluoroquinolone resistance mechanism in MRSA in multiple studies investigating the prevalence and genetic background of antibiotic resistance without determining the strains' clonal affiliation (Takahata et al., 1996; Deplano et al., 1997; Kaatz and Seo, 1998; Sierra et al., 2002; Noguchi et al., 2005; Iihara et al., 2006; Coskun-Ari and Bosgelmez-Tinaz, 2008).
Though the double-serine mutations seem to remain a “trademark” of successful HA-MRSA strains/lineages in the adult healthcare setting where fluoroquinolones are used extensively the isolates may also harbor additional DNA gyrase and/or topoisomerase IV mutations (Sierra et al., 2002; Noguchi et al., 2005; Iihara et al., 2006; Takano et al., 2008; Chakrakodi et al., 2014).
In a similar fashion to MRSA the corresponding double-serine residues were observed to mutate also in the strains of the major international sequence types of ESBL-producing K. pneumoniae (gyrA Ser83Phe or Ser83Ile; parC Ser80Ile) though will often be complemented with additional QRDR mutations (Alouache et al., 2014; Tóth et al., 2014; Nagasaka et al., 2015; Park et al., 2015; Zhou et al., 2016; Sekyere and Amoako, 2017). In contrast, fluoroquinolone resistant minor ST strains—losing considerable fitness (Tóth et al., 2014)—were reported to be either void of DNA gyrase/topoisomerase IV mutations; carried a “non-serine” mutation or harbored just one of the favorable serine mutations (Tóth et al., 2014; Nagasaka et al., 2015; Sekyere and Amoako, 2017).
Moreover, all ST258 strains—which are genetically related to the major ST11 group isolates and are largely responsible for the global dissemination of carbapenemases—carry the gyrA Ser83Ile, parC Ser80Ile double mutations (Table 1; Bowers et al., 2015).
Strains of the sole international ST131 H30 lineage of ESBL-producing E. coli also carry the two equivalent double-serine mutations (gyrA Ser83Leu or sometimes Ser83Ile and parC Ser80Ile). Furthermore, they harbor usually three or sometimes two supplementary mutations; typically: gyrA Asp87Asn, parC Glu84Val, and parE Ile529Leu (Table 1; Paltansing et al., 2013; Johnson et al., 2015; Kim et al., 2016; Röderova et al., 2017).
In contrast to the above species C. difficile carries a threonine residue in the corresponding 82 gyrA position and, interestingly, its genome is void of topoisomerase IV (Dridi et al., 2002). The major international ribotypes/lineages of C. difficile characteristically carry the gyrA Thr82Ile mutation (Table 1; Spigaglia et al., 2010; Wasels et al., 2015). The gyrA Thr82Ile mutation can either be harbored as a single genetic alteration or combined with additional gyrA and/or gyrB mutations (Huang et al., 2009, 2010; Spigaglia et al., 2010; Walkty et al., 2010; Lin et al., 2011; Dong et al., 2013; Aogáin et al., 2015; Kuwata et al., 2015).
In summary, the command of the double-serine mutations in specific positions in the DNA gyrase and topoisomerase IV genes has been shown to be a dominant feature of multi-drug resistant major STs/lineages in at least three species: S. aureus, K. pneumonia, and E. coli. In addition the carriage of an equivalent gyrA mutation in C. difficile is typical for the international ribotypes/lineages of the pathogen. These observations argue for a salient role for fluoroquinolones in the selection of these STs/lineages. Moreover, they strongly suggest that apart from incurring resistance to fluoroquinolones these mutations should confer some additional favorable trait on the bacteria.
The Energy Balance Associated with Individual QRDR Mutations
In a fluoroquinolone environment bacteria will be able to extensively disseminate if they can achieve high-level resistance against these antibiotics without suffering appreciable fitness cost.
It is well-established that the binding of fluoroquinolones to the DNA gyrase and topoisomerase IV molecules is mediated primarily by four amino acids. Two serine residues: gyrA Ser83 and parC Ser80 (based on E. coli numbering) and an acidic residue four amino acids downstream of both respective positions (Aldred et al., 2014). Recently a secondary binding mode for fluoroquinolones was demonstrated involving downstream gyrA and gyrB sequences (Mustaev et al., 2014; Malik et al., 2016).
The evolvement of QRDR mutations mainly reflects the mechanism of fluoroquinolone binding: the majority of the mutations observed to date in various bacteria will mostly affect the serine and/or acidic residues mentioned above though mutations affecting additional residues especially in the QRDR region are also common (Aldred et al., 2014; Hooper and Jacoby, 2015).
In most cases a single mutation in only one of the two target enzymes confers ≤ 10-fold drug resistance and mutations in both enzymes are usually required to attain a 10 – 100-fold rise in MIC value (Reviewed by Aldred et al., 2014). Thus, strains in general need to evolve minimum two but often even more mutations to reach the expedient level of fluoroquinolone resistance.
Though mutations at the crucial serine residues—in contrast to acidic mutations—did not appear to adversely affect catalytic activity in the absence of fluoroquinolones (Aldred et al., 2014) a review of fitness studies performed with various species carrying diverse QRDR mutations presents a more nuanced picture.
The literature supporting the beneficial nature of the gyrA Ser83 mutations are abundant.
The Ser83Ala gyrA mutation in E. coli was initially demonstrated to have no impact on the catalytic activity of the enzyme (Barnard and Maxwell, 2001) and subsequently both the Ser83Ala and Ser83Leu mutations were shown by multiple authors to confer a slight fitness advantage on the isolates (Komp Lindgren et al., 2005; Marcusson et al., 2009; Machuca et al., 2015; Huseby et al., 2017).
Similarly the gyrA Ser83Phe mutation was reported to be associated with some fitness gain in both Salmonella typhimurium (Giraud et al., 2003) and S. Typhi (Baker et al., 2013). In S. Typhi the gyrA Ser83Tyr mutation also proved energetically favorable (Baker et al., 2013).
In Streptococcus pneumoniae both Gillespie et al. (2002) and Rozen et al. (2007) failed to observe loss of fitness in an isolate with the gyrA Ser81Phe mutation and—supporting the results —Pan et al. (2017) did not demonstrate any change in the activity of DNA gyrase (topoisomerase II) carrying the Ser81Phe gyrA mutation. However, Rozen et al. (2007) reported some fitness cost with the gyrA Ser81Tyr alteration.
Furthermore, mutations in the corresponding serine residues of the gyrA gene in MRSA and K. pneumoniae—though tested less meticulously—were reported to be associated with no fitness cost. Horváth et al., 2012) failed to observe any loss of vitality during the in vitro induction of fluoroquinolone resistance in an MRSA isolate upon the onset of the Ser84Ile gyrA mutation. Tóth et al. (2014) reported that a strain of K. pneumoniae harboring a Ser83Tyr gyrA mutation with an MIC to ciprofloxacin of 0,5 mg/L showed excellent vitality relative to other isolates.
In some species—Pseudomonas aeruginosa, Burkholderia cepacia, C. difficile, Campylobacter jejuni—the corresponding gyrA residue participating in the binding of fluoroquinolones are not serine but threonine. Moreover, some slow-growing bacteria—C. difficile, C. jejuni and the mycobacteria—are void of the topoisomerase IV enzyme (Dridi et al., 2002) and QRDR resistance will, thus, be confined to the DNA gyrase genes.
In P. aeruginosa Agnello et al. (2016) observed favorable fitness in strains with the corresponding single QRDR mutation—gyrA Thr83Ile—in which no other important fluoroquinolone resistance mechanisms could be detected. Moreover, the gyrA Thr83Ile mutation in B. cepacia and the corresponding Thr86Ile change in C. jejuni were observed to result in some fitness advantage (Pope et al., 2008; Han et al., 2012). In addition C. jejuni strains carrying the latter mutation were shown to outcompete wild type strains in an in vivo model (Luo et al., 2005). Moreover, the Thr86Ile mutation was reported to positively impact the molecule's activity concluding in an improvement in the enzyme's physiology (Han et al., 2012).
In C. difficile the gyrA mutation characteristic for the major international ribotypes/lineages—Thr82Ile—was observed to be associated with just a minimal cost of vitality (Wasels et al., 2015). Nevertheless, the Thr82Ile gyrA mutation in C. difficile is sometimes combined with additional gyrA alterations which the strains might need to attain adequate level of resistance (Huang et al., 2009; Spigaglia et al., 2010; Walkty et al., 2010; Dong et al., 2013; Kuwata et al., 2015).
In summary we can say that the mutation of the gyrA serine/threonine residue responsible for the binding of fluoroquinolones almost always exerts some positive effect on the isolate's physiology but is often insufficient to individually incur the adequate level of resistance to fluoroquinolones.
The energy balance of the second mutation of the double-serine pair - affecting the parC serine 80 residue in E. coli- proved more equivocal and was individually tested in just two species. In E. coli the parC Ser80Ile mutation's impact on fitness was investigated by Marcusson et al. (2009) who reported a slight fitness cost in the isolate. In contrast in S. Typhi Baker et al. (2013) observed a small fitness gain with the same mutation.
In S. pneumoniae one of the mutations in the corresponding parC residue (Ser79Phe) was observed to be associated with some fitness cost (Rozen et al., 2007), however, another mutation of the same residue (Ser79Tyr) did not result in any loss of vitality (Gillespie et al., 2002; Rozen et al., 2007).
The remaining QRDR mutations in both the DNA gyrase and topoisomerase IV genes were observed to mostly engender more or less fitness cost in various species (Komp Lindgren et al., 2005; Rozen et al., 2007; Pope et al., 2008; Marcusson et al., 2009; Baker et al., 2013; Wasels et al., 2015).
The exception is the parC Asp83Tyr mutation that was reported to confer some fitness advantage on S. pneumoniae (Rozen et al., 2007). Interestingly a Glu84Lys mutation in the corresponding parC residue in S. aureus will seriously compromise the enzyme's activity, however, if a proline substitution is located in the same position (Glu84Pro) the molecule's physiology remains intact (Hiasa, 2002).
The Energy Balance Associated with Multiple QRDR Mutations
Interestingly QRDR mutations will confer diverse MIC elevations for fluoroquinolones in various species.
Among bacteria thoroughly tested, the rise in MIC value for fluoroquinolones as a consequence of individual QRDR mutations proved low in E. coli, and in S. Typhi (Marcusson et al., 2009; Baker et al., 2013; Machuca et al., 2015). The elevation proved higher in S. pneumoniae (Gillespie et al., 2002; Rozen et al., 2007), P. aeruginosa (Agnello et al., 2016) and B. cepacia (Pope et al., 2008). The greatest rise in MIC was observed in C. difficile (Spigaglia et al., 2010; Lin et al., 2011; Wasels et al., 2015) and Campylobacter (Ge et al., 2005; Jesse et al., 2006).
Though we do not have comparable data for MRSA and K. pneumoniae it is well-established that both pathogens are capable of developing high-level resistance to fluoroquinolones by evolving double or triple QRDR mutations which suggests that an elevation in MIC value associated with individual mutations should be higher than in E. coli.
The highest MIC values for fluoroquinolones observed in C. jejuni and C. difficile may be related to the topoisomerase IV enzyme deficiency in these species (Cooper et al., 2002; Dridi et al., 2002; Ambur et al., 2009). These pathogens harbor just a single fluoroquinolone target molecule—DNA gyrase—whose mutation should result in a greater barrier for fluoroquinolones since a second enzyme is not available to bind to and compromise.
Since individual QRDR mutations elicit just a very slight increase in the level of fluoroquinolone resistance in E. coli (Marcusson et al., 2009; Machuca et al., 2015) the strains need to accumulate multiple genetic changes to collectively generate the adequate level of resistance. This is the reason why the sole international lineage of ESBL-producing E. coli (ST131 H30) characteristically carries four or rather five well-defined mutations (Paltansing et al., 2013; Johnson et al., 2015; Kim et al., 2016; Röderova et al., 2017).
The evolution of a really favorable array of mutations remains a serious challenge. Exclusively strains of the global ST131 H30 lineage proved capable to accomplish this feat and develop a suitable assortment of mutations that remains the principal determinant permitting the global dissemination of this group (Johnson et al., 2015; Fuzi, 2016). As already mentioned the double-serine mutations—affecting prominent binding spots for fluoroquinolones—form part of this genetic combination (Johnson et al., 2015).
Some excellent data are available on the fitness balance generated by combinations of three of the five QRDR mutations evolved by the ST131 H30 E. coli lineage. Marcusson et al. (2009) observed that the double-serine combination conferred significantly higher level of resistance to fluoroquinolones than other “pairs” of QRDR mutations, however, they were associated with a slight fitness cost. Interestingly when the double-serine mutations were completed with the gyrA Asp87Asn change the MIC of the isolate rose considerably and a very slight fitness benefit was observed.
Machuca et al. (2015) also observed that the double-serine mutations conferred the highest MIC value—relative to other pairs of mutations—for fluoroquinolones, nonetheless, they reported a significant fitness gain in their isolate and confirmed the favorable nature of the “triple arrangement” including an additional gyrA Asp87Asn.
Diverse clonal affiliation of the isolates in these studies could have influenced findings.
Furthermore, Huseby et al. (2017) very recently affirmed that the double-serine combination confers the highest MIC value for fluoroquinolones and demonstrated that the parC Ser80Ile mutation is acquiring an increasing selective advantage with an increasing fluoroquinolone concentration. This fitness benefit can not be detected in the absence of fluoroquinolones. They also showed that the triple mutation—gyrA Ser83Leu, Asp87Asn, and parC Ser80Ile—have a fitness advantage over other triple combinations in the presence of ciprofloxacin (Huseby et al., 2017).
The energetically positive balance generated by the addition of the individually detrimental acidic gyrase mutation to the double-serine changes and the observation that the fitness benefit of the double-serine mutations materialized only in the presence of fluoroquinolones are essential findings reflecting the nuanced effect of combined mutations.
Though the impact of the fourth and fifth E. coli mutations (parC E84V, parE I529L) have not been individually tested the global success of the ST131 H30 isolates carrying these genetic traits (Johnson et al., 2015) strongly suggest that they should complement the other mutations favorably: the dissemination of the clone has been demonstrated to be linked to the fitness benefit associated with its high-level resistance to fluoroquinolones (Johnson et al., 2015).
In S. Typhi the fitness balance associated with the double-serine mutations has not been investigated however a fitness gain was demonstrated for various other pairs of mutations (Baker et al., 2013). Nevertheless, the various double mutations tested conferred just a slight elevation of MIC for fluoroquinolones. Interestingly a fitness cost was reported for the gyrA Ser83Phe, Asp87Gly, parC Ser80Ile triple mutations—which almost correspond to the triple mutations investigated in E. coli (Baker et al., 2013). Consequently—in a similar fashion to E. coli—if fluoroquinolones will ever select a major multi-drug resistant S. Typhi clone or lineage it will certainly have to harbor more than three QRDR mutations.
In contrast to E. coli and S. Typhi the double-serine mutations (gyrA Ser81Tyr or Ser81Phe and parC Ser79Tyr or Ser79Phe) incur higher level resistance to fluoroquinolones in S. pneumoniae (Table 1; Pletz et al., 2004; Adam et al., 2007; Hsieh et al., 2010; Rodríguez-Avial et al., 2011; Schmitz et al., 2017).
Interestingly conflicting reports have been published on the fitness balance of the double-serine mutations in this species. While both Johnson et al. (2005) and Rozen et al. (2007) observed a fitness cost associated with the double-serine mutations of gyrA Ser81Phe and parC Ser79Tyr in genetically-engineered strains, Gillespie et al. (2002) found that the identical double-serine mutations failed to compromise vitality subsequent to in vitro induction. Unfortunately the clonal affiliation of the isolates - that could have influenced the findings - have not been determined in these studies.
Prior to the advent of vaccination fluoroquinolone resistant S. pneumoniae strains used to often disseminate clonally and the isolates primarily carried double-serine mutations (Pletz et al., 2004; Adam et al., 2007; Hsieh et al., 2010; Rodríguez-Avial et al., 2011). Interestingly strains from these fluoroquinolone-resistant S. pneumoniae clones did not show any fitness cost and even have sometimes exceeded wild type strains in propagation assays (Rudolf et al., 2011).
The anti-pneumococcal vaccination has reduced the rate of fluoroquinolone-resistance in S. pneumoniae. The previous resistant clones receded and have been partly replaced by novel STs. Some of these novel strains still proved capable of developing the double-serine mutations (Ceyssens et al., 2016; Schmitz et al., 2017). However, in a few locations “postvaccination strains” had not been able to evolve the energetically favorable double-serine changes. Interestingly these strains having failed to evolve the mutations conferring major elevations in MIC values often accumulated multiple alternative QRDR mutations to attain resistance to fluoroquinolones (Ceyssens et al., 2016; Takeuchi et al., 2017). The dearth of the energetically favorable double-serine mutations might have been responsible for their apparent inability to disseminate extensively (Ceyssens et al., 2016; Takeuchi et al., 2017).
The energy balance associated with the individual QRDR mutations have not been tested in MRSA, however, the dominance of these mutations in the successful healthcare associated STs and lineages—as mentioned earlier—argues strongly for a favorable fitness effect. In addition, Horváth et al., 2012) showed that minor clone strains of CA-MRSA suffering significant fitness costs upon developing resistance to fluoroquinolones either do not carry the double-serine mutations or harbor additional detrimental genetic changes. Moreover, Holden et al. (2013) demonstrated that the emergence of the major international ST22 clone in the United Kingdom has been linked to the evolvement of a novel clade wielding superior fitness relative to earlier variants and harboring—among other genetic features—the double-serine mutations.
In the major international STs of ESBL-producing K. pneumoniae the double-serine mutations (gyrA Ser83Ile, parC Ser80Ile) conferred high-level resistance to an isolate and were observed to be associated with just a very small fitness cost (Tóth et al., 2014). The triple-mutations (gyrA Ser83Phe, Asp87Ala, and parC Ser80Ile) also incurred high-level resistance and were associated with some loss of vitality in a strain-specific fashion (Tóth et al., 2014). In addition, as mentioned above, the preeminence of the double-serine mutations in the international STs of ESBL-producing K. pneumoniae also supports the beneficial nature of this combination.
In P. aeruginosa carrying a threonine residue in the gyrA 83 position Kugelberg et al. (2005) observed that the double gyrA Thr83Ile and parC Ser80Leu mutations conferred high-level resistance to fluoroquinolones but were associated with fitness cost. It has to be noted that the genetic change reported initially as parC Ser80Leu is actually parC Ser87Leu since the serine residue is located in the latter position in P. aeruginosa (Lee et al., 2005).
Recently Agnello et al. (2016) reported that the parC Ser87Leu mutation introduced into strains of P. aeruginosa already carrying the gyrA Ser83Ile mutation was associated with a slight fitness cost in five of six isolates. However, it conferred a small fitness benefit on one of the isolates suggesting that clonal affiliation is relevant also in this species. In addition, authors observed that the fitness cost was influenced by the genotype of the type III secretion system harbored by the isolates (Agnello et al., 2016). Moreover, the dominance of the gyrA Thr83Ile alteration often associated with the parC Ser87Leu change in fluoroquinolone resistant strains of P. aeruginosa (Higgins et al., 2003; Lee et al., 2005; Agnello and Wong-Beringer, 2012; Yang et al., 2015; Araujo et al., 2016; Nouri et al., 2016) argues strongly for the salient role of the double-threonine/serine mutations in selecting groups of bacteria with favorable fitness also in this species.
The influence genetic (clonal) differences exert on the evolution of favorable QRDR mutations in P. aeruginosa was reflected in the findings of Jørgensen et al., 2013). These investigators induced resistance to fluoroquinolones in vitro in their P. aeruginosa isolates. Surprisingly none of the strains proved capable of developing the gyrA 83 and parC 87 mutations which—as mentioned above—are the most common genetic alterations in clinical isolates. In contrast all of them evolved QRDR mutations in unorthodox positions (Jørgensen et al., 2013).
Further studies could unequivocally establish whether or not the double-threonine/serine mutations contributed to the clonal dynamics in P. aeruginosa.
In B. cepacia the gyrA Thr83Ile and parC Ser80Leu double mutations were reported to have conferred high level resistance to fluoroquinolones but were associated with significant fitness cost.
Species which lack the topoisomerase IV enzyme—C. difficile and C. jejuni—can-not evolve genetic combinations equivalent to the double mutations mentioned above. In the major international clones of C. difficile a single QRDR mutation—gyrA Thr82Ile—proved optimal, concurrently ensuring proper fluoroquinolone MIC value and adequate fitness balance (Table 1; (Wasels et al., 2015)). Some major clone strains may also carry a second QRDR mutation, that may be a consequence of excessive fluoroquinolone exposure, or more rarely a distinct mutation in the gyrA or gyrB genes (Spigaglia et al., 2010).
Similarly to C. difficile a single mutation—gyrA Thr86Ile—may confer the adequate level of resistance to C. jejuni (Iovine, 2013). It will often be supplemented with an additional QRDR alteration (Iovine, 2013).
In contrast to MRSA, ESBL-producing K. pneumoniae, ESBL-producing E. coli and C. difficile in C. jejuni the ability to evolve favorable mutation(s) was not restricted to a few STs/lineages. To our understanding C. jejuni may be the single pathogen among bacteria reviewed in this paper that has efficiently adapted to resistance against fluoroquinolones “as a species.” In this bacterium a multitude of genetic variants - not just a few clones—have been able to develope favorable mutational resistance (Luo et al., 2005; Zeitouni and Kempf, 2011). This excellent capacity of adaptation is most certainly the consequence of the hyperplasticity of the C. jejuni genome (Stahl and Stintzi, 2011).
In summary we can say that in a number of species which harbor both the DNA gyrase and topoisomerase IV genes the success of individual clones/lineages depend on their ability to evolve the double-serine—or equivalent—mutations often supplemented with additional appropriate changes in the QRDR regions.
It is well-established that E. coli belongs to this group. There is also in vitro and epidemiological evidence that the expansion of the major STs/lineages of both ESBL-producing K. pneumoniae and HA-MRSA have been the consequence of a similar process (see above). Moreover, there is some circumstantial evidence that a similar mechanism may have contributed to the dissemination of fluoroquinolone resistance in S. pneumoniae and P. aeruginosa (see above).
Slow-growing bacteria like C. difficile and C. jejuni lacking the topoisomerase IV gene had to embrace different strategies. However, even in these species the ability to evolve an energetically favorable gyrA threonine mutation proved crucial for dissemination—for major clones (C. difficile) or for the whole species (C. jejuni)—in a fluoroquinolone environment.
What Drives Evolution?
As we have seen individual STs/lineages of various species differ in their ability to develop favorable QRDR mutations. This trait, however, has been shown to be amenable to change. Clones/lineages are capable of undergoing a remarkable metamorphosis and improve their ability of evolving QRDR mutations.
ST239 and ST8 MRSAs remain minor clones in Hungary and the latter was observed to lack the favorable double-serine genetic combination (Horváth et al., 2012). In addition they are also on the retreat in many parts of Europe (Grundmann et al., 2014). In contrast the new lineage of the ST8 MRSA in the United States and some ST239 strains in Asia have been reported to carry the double-serine mutations that should have contributed to the success of these pathogens in those areas (Takano et al., 2008; Chakrakodi et al., 2014; Alam et al., 2015; Khokhlova et al., 2015).
Similarly, while some novel “postvaccination clone” isolates of S. pneumoniae investigated in Belgian and Japanese studies failed to develop the favorable double-serine mutations (Ceyssens et al., 2016; Takeuchi et al., 2017), other “novel clone-strains” in Belgium and Germany succeeded in evolving the genetic combination (Ceyssens et al., 2016; Schmitz et al., 2017).
Clones/lineages of additional species are certainly not impervious to a similar metamorphosis.
Consequently minor clone/lineage isolates can sometimes “assume” the ability to evolve favorably. It remains of utmost importance to identify the determinants driving this evolutionary process.
The Evolutionary Background of the Double-Serine Residues
The double-serine residues confer susceptibility to an important group of antibiotics, fluoroquinolones. In addition, the replacement of the gyrase serine residue (residue 83 in E. coli) is associated with a slight fitness advantage. The question arises, if these amino acids are not favorable why have they been evolutionarily preserved across species?
The most probable answer is that they confer resistance to naturally occurring substances microbes are sometimes exposed to.
Japanese scientists demonstrated a couple of years ago (Hiramatsu et al., 2012) that fluoroquinolone resistant S. aureus strains carrying the double-serine mutations (in the gyrA 84 and parC 80 residues) were all susceptible to a natural antibiotic (nybomycin, a quinolone-dione) produced by several streptomyces species. Conversely fluoroquinolone susceptible wild type isolates harboring both serine residues proved resistant. The parC serine mutation proved pivotal in incurring resistance (Hiramatsu et al., 2012). Interestingly nybomycin also showed activity against fluoroquinolone resistant enterococci (Hiramatsu et al., 2012).
In addition fluoroquinolone resistant S. aureus isolates carrying the double-serine mutations have also shown susceptibility to a natural flavonoid substance—apigenin—produced by various plants while fluoroquinolone susceptible isolates remained resistant (Morimoto et al., 2015). In contrast to nybomycin here the mutation of the gyrA 84 residue played an essential role in conferring protection (Morimoto et al., 2015).
It is tempting to speculate that ancient bacteria extensively exposed to herbal flavonoids (Hiramatsu et al., 2012) in order to protect themselves had to compromise the activity of their gyrase enzymes and consequently their fitness by evolving the gyrA serine residue. Thus, the change of the gyrA serine residue will prove favorable-in a non-flavonoid environment.
The Significance of Additional Fluoroquinolone Resistance Mechanisms and Virulence Factors
Though the QRDR mutations are pivotal in conferring high-level resistance to fluoroquinolones some additional mechanisms also form relevant part of the bacterial defense hardware.
Various efflux systems are well-established to participate in resistance against fluoroquinolone type antibiotics (Aldred et al., 2014). However, in contrast to some QRDR mutations the energy balance of efflux—unless it incurs just a slight elevation in the MIC value for fluoroquinolones—remains negative. An abundance of papers investigating diverse species of bacteria reported fitness cost associated with the activity of various efflux systems (Sánchez et al., 2002; Komp Lindgren et al., 2005; Marcusson et al., 2009; Martinez et al., 2009; Tóth et al., 2014; Machuca et al., 2015; Huseby et al., 2017). Consequently, bacteria are usually not supposed to extensively deploy their energy-consuming “efflux defense” if they are capable of evolving the energetically more favorable gyrA serine mutation combined with the parC serine change which together - and sometimes with additional mutations - will raise the MIC value for fluoroquinolones to the “requisite” level. And this is really what has been observed in those species which have already been investigated in that respect.
Tóth et al. (2014) tested the efflux activity in ESBL-producing major and minor ST K. pneumoniae isolates. Fluoroquinolone resistant major ST strains—harboring either the double-serine mutations or the double-serine plus one triple combination—were observed to have similar propagation rates to susceptible isolates and failed to show any efflux activity. Conversely efflux activity could be demonstrated in three of the four minor ST isolates tested. The fluoroquinolone resistant minor ST strains were void of QRDR mutations, carried a single mutation other than the double-serine or harbored just one of the two serine mutations (Tóth et al., 2014). The efflux systems of the wild type minor ST strains—prior to in vitro induction with ciprofloxacin - were inactive (Tóth et al., 2014). It seems obvious that these isolates proved unable to evolve the favorable QRDR mutations and could not, thus, raise their MIC values to the adequate level. Then trying just to survive the exposure to the increasing concentrations of ciprofloxacin turned on their efflux systems. However, driving the efflux required energy which resulted in fitness cost slowing the growth rates of the isolates conferring a serious liability vis-à-vis “well-energized” major ST strains in a fluoroquinolone environment.
Similarly Johnson et al. (2015) reported that in multi-drug resistant E. coli minor ST strains carried fewer QRDR mutations than the ST131 H30 major lineage isolates but showed significantly greater efflux activity. Comparable studies in other species have not been performed. Nevertheless, the use of efflux for the removal of fluoroquinolones from the bacterial cell should be common in minor ST isolates in many bacteria that may account for some findings reported in the literature. Bagel et al. (1999) reported just a minimal fitness cost associated with the gyrA Ser83Leu mutation in a strain of E. coli in which the alteration was genetically engineered. In contrast they observed a large fitness cost in a clinical isolate carrying just the same single mutation. It is tempting to suggest that the unorthodox finding was due to the clinical strain being a minor clone isolate. It carried a single QRDR mutation suggesting that it must had been exposed to fluoroquinolones. Since the sole mutation should not have conferred the adequate MIC value it could have turned on the energy consuming efflux.
In P. aeruginosa Kugelberg et al. (2005) observed high fitness cost in a clinical isolate with high MIC value carrying a single gyrA Thr83Ile mutation, however, an active efflux was also detected. Moreover, Agnello et al. (2016) demonstrated dissimilar fitness in clinical isolates harboring the sole Thr83Ile mutation and showed that all the strains with substantial loss of vitality run a highly active efflux system.
Additional fluoroquinolone resistance mechanisms include qnr proteins protecting target enzymes from quinolones and a variant of the aminoglycoside acetyltransferase enzyme - aac(6-)-Ib-cr- conferring reduced susceptibility to ciprofloxacin by N-acetylation of its piperazinyl amine. Both mechanisms confer low-level resistance to fluoroquinolones (Aldred et al., 2014).
Qnr proteins were reported to have been associated with both some fitness benefit and a slight fitness cost in E. coli (Michon et al., 2011; Machuca et al., 2014). They are, interestingly, sometimes absent from the ST131 major clone strains of ESBL-producing E. coli (Aoike et al., 2013; Paltansing et al., 2013; Reyna-Flores et al., 2013; Guillard et al., 2014). The evolutionary edge associated with the qnr proteins remains obscure. They have been observed to confer protection against some quinolone-like compounds of herbal origin but, interestingly, not against quinolone type quorum sensing molecules produced by pseudomonas species (Kwak et al., 2013).
In contrast to qnr proteins the carriage of the aac(6-)-Ib-cr gene is common in both major ST/lineage ESBL-producing K. pneumoniae and ESBL-producing E. coli isolates (Musumeci et al., 2012; Reyna-Flores et al., 2013; Guillard et al., 2014; Tóth et al., 2014; Park et al., 2015; Zhou et al., 2016).
Apart from diverse fitness costs associated with resistance to fluoroquinolones fitness balance linked to other groups of antibiotics have not been seriously implicated in the selection and promotion of the international STs/lineages of the above pathogens. Virulence factors, however, have often been suggested to prime the advancement of various major groups of bacteria.
A review of all the major virulence factors of the above pathogens remains way beyond the scope of this paper. Thus, only salient issues related to virulence in the international STs/lineages of ESBL-producing E. coli, ESBL-producing K. pneumoniae and HA-MRSA will briefly be covered.
Virulence factors have not been seriously implicated in the expansion of the E. coli ST131 H30 lineage. It is well-established that the lineage is a diverse group with regard to virulence. It consists of multiple “virotypes” showing distinct degrees of pathogenicity (Blanco et al., 2011; Olesen et al., 2014; Miyoshi-Akiyama et al., 2016). Moreover, non-ST131 E. coli strains were reported to be just as virulent as some ST131 isolates (Ciesielczuk et al., 2015). Though, Cha et al. (2016) recently alleged that the ST131 clone was more virulent than others, Han et al. (2017) showed that ST131 strains fail to excel in aggregate virulence. Furthermore, Dahbi et al. (2014) reported that ST131 isolates show diverse virulence and low-virulence isolates are common among them.
In ESBL-producing K. pneumoniae biofilm formation was supposed to further the expansion of the major ST11 sequence type (Andrade et al., 2014; Melegh et al., 2015), however, Diago-Navarro et al. (2014) observed “heterogeneity” in the formation of biofilm in ST258 strains of K. pneumoniae—a close relative of the ST11 major sequence type. Moreover, Kong et al. (2012) questioned the role of biofilm formation in the development of systemic infection with K. pneumoniae. Recently a possible role for yersiniabactin was proposed in ST15 K. pneumoniae isolates (Zhou et al., 2016). However, Lee et al. (2016) showed that yersiniabactin production is common also in minor clone isolates. Moreover, the probably most virulent K. pneumoniae sequence type, ST23 does not belong to the major groups of the pathogen (Struve et al., 2015).
In MRSA the production of biofilm and the carriage of the arginine catabolic mobile element (ACME) have been mentioned as potentially essential clonal enhancers, however, the incidence of these virulence factors remains at variance with the observed clonal shifts in HA-MRSA. The issue was recently reviewed (Fuzi, 2016).
In summary, virulence factors seem to play only a secondary role compared with diverse fitness cost associated with fluoroquinolone resistance in the selection and promotion of international ST/lineage isolates in the multi-drug resistant variants of at least three species.
The Possible Role of the Double-Serine QRDR Mutations in the Emergence of the Major International Lineages of VRE
As we have shown data available on S. pneumoniae and P. aeruginosa hint at a possible role for fluoroquinolones in the dissemination of these pathogens. However, in an additional species—vancomycin-resistant E. faecium (VRE)—both the genetic and epidemiological evidence for the involvement of a similar process remains much stronger.
It is well-established that a few lineages related to a single international clone of VRE (CC17) dominate the hospital setting worldwide (Willems et al., 2005; Leavis et al., 2006a; Cattoir and Leclercq, 2013; Freitas et al., 2016; Guzman Prieto et al., 2016) and the literature suggest that it also was selected and promoted by the extensive use of fluoroquinolones.
The process of clonal reduction was spectacular and has been well-documented in VRE. The use of a glycopeptide antibiotic in animal husbandry—avoparcin—promoted the dissemination and enteric carriage of the pathogen in the European population in the 1990s. An abundance of papers reported the often widespread carriage of VRE across the continent (Bingen et al., 1991; Jordens et al., 1994; Gordts et al., 1995; Moulin et al., 1996; van den Bogaard et al., 1997). These isolates of animal origin, however, proved unable to disseminate in the adult hospital setting (van den Braak et al., 1998).
Interestingly, not only the VRE clones of animal origin failed to disseminate in hospitals. The multiple clones of human VRE observed in that period (Clark et al., 1993; Sadowy et al., 2013) also suffered a substantial reduction and subsequently several lineages all related to a single clone of the pathogen (CC17) emerged in adult hospital wards worldwide (Willems et al., 2005; Cattoir and Leclercq, 2013). These internationally dominant groups of pathogens differ significantly from other human VRE clones and lineages and even more from those VRE clones adapted to various animals species (Willems et al., 2000, 2005; Werner et al., 2008; Qin et al., 2012).
Though these bacteria are called VRE, interestingly, some strains from these lineages remain susceptible to vancomycin (Willems et al., 2005; Leavis et al., 2006a; Coombs et al., 2014). However, most of them seem to be resistant to fluoroquinolones (Leavis et al., 2006a; Werner et al., 2010).
Moreover, Cattoir and Leclercq (2013) showed that the CC17 clone emerged as an ampicillin and fluoroquinolone resistant group that only subsequently acquired resistance to glycopeptides. Furthermore, the observation that among the various VRE clones/lineages exclusively the CC17-related strains harbor the well-known double-serine fluoroquinolone resistance mutations in the DNA gyrase and topoisomerase IV genes (Leavis et al., 2006b; Sadowy et al., 2013) constitutes a strong circumstantial evidence for the selective and promoting role of fluoroquinolones in the dissemination of these bacteria.
The CC17-related E. faecium strains' exceptional capacity to evolve the DNA gyrase and topoisomerase IV mutations was recently shown by French scientists. de Lastours et al. (2017) demonstrated that non-CC17-related lineages of VRE are generally unable to develop the favorable gyrA and parC mutations. 48 healthy volunteers were treated with ciprofloxacin and then, the fluoroquinolone resistance in E. faecium strains isolated from the enteric commensal flora was investigated. Remarkably none of the commensal E. faecium strains proved capable of evolving the favorable gyrA and parC mutations.
Though resistance to ampicillin has been a feature of CC17-related lineages for a long time (Cattoir and Leclercq, 2013) it is highly unlikely that it could have played a major role in the promotion of these groups of pathogens. Antibiotic resistance surveillence data collected by the European Union clearly show that not only vancomycin-resistant E. faecium strains are resistant to ampicillin; the overall resistance rate in most countries remains over 75 percent (http://atlas.ecdc.europa.eu/public/index.aspx).
Virulence factors have also been implicated in the advancement of the CC17-related lineages. Primarily the esp gene involved in biofilm formation was supposed to make a crucial contribution (Top et al., 2008). There is no doubt that the esp gene has contributed to the extensive dissemination of these lineages. However, the available data from the literature strongly suggest that its role remains less significant than the ability to evolve favorable QRDR mutations.
While it is well-established that the rate of fluoroquinolone resistance is consistently high in CC17-related VRE lineages the carriage rate for esp varies strongly across studies (Klare et al., 2005; Khan et al., 2008; Galloway-Peña et al., 2009; Mato et al., 2009; López et al., 2010; Bjørkeng et al., 2011; Fallico et al., 2011; Kang et al., 2014).
The Impact of Fluoroquinolone Use on the Incidence of “Major STs/Lineages” of Multi-Drug Resistant Pathogens
The available information on the influence of diverse fitness cost associated with fluoroquinolone resistance on the clonal dynamics of various multi-drug resistant pathogens suggests that the use of fluoroquinolone type antibiotics should profoundly impact the incidence of these bacteria provided they belong to “major STs/lineages.”
Since most HA-MRSA strains in adult hospital wards belong to “major STs” worldwide a decrease or increase in fluoroquinolone consumption should have a prompt effect on the pathogen's incidence. This is really what has been observed. A plethora of papers almost concordantly demonstrated that there is a direct link between the use of fluoroquinolones and the incidence of HA-MRSA in adult departments. The related literature was recently reviewed (Fuzi, 2016).
The proportion of the major ribotypes of C. difficile proved also high in the European surveillance system (Fawley et al., 2016). The United Kingdom launched a campaign about 10 years ago to reduce the incidence of C. difficile infections by decreasing the use of fluoroquinolones. The results were spectacular: a dramatic decline in the number of reported cases was instantly observed which was associated with the partial replacement of the major ribotypes of the pathogen by minor clones (Reviewed recently by Fuzi, 2016). Moreover, an abundance of papers from a variety of countries show that a reduction in the consumption of fluoroquinolones will result in a decrease in the incidence of C. difficile infections (Reviewed recently by Fuzi, 2016).
Though there are no reliable data on the prevalence of “major ST/lineage” strains of the remaining multi-drug resistant pathogens mentioned above it is certain that their proportion is smaller than those of HA-MRSA and C. difficile. Thus, we can expect a significant impact on the incidence of these bacteria—subsequent a decrease in the use of fluoroquinolones—exclusively if we have established that the proportion of the “major ST/lineage” isolates is high in the studied facility.
Consequently the judicious use of fluoroquinolones should be dynamic and a function of the clonal composition of the local multi-drug resistant pathogens. Should the proportion of the “fluoroquinolone-associated STs/lineages” exceed a “threshold” the consumption of fluoroquinolones should be abandoned. Conversely, if the proportion of the “fluoroquinolone-associated STs/lineages” remains low fluoroquinolones can certainly be used to great advantage.
Further studies exploring clonal affiliations would be needed to elucidate the impact of fluoroquinolone use on the incidence of various multi-drug resistant pathogens. These studies would also help to establish the “threshold proportions” for “major STs/lineages” indicators for the suspension or resumption of fluoroquinolone therapy. Though the judicious use of fluoroquinolones would not permanently resolve the problem of antibiotic resistance it would reduce the proportion of “major ST/lineage” strains and lower the incidence of multi-drug resistant pathogens ameliorating the situation.
In summary the ability of some STs/lineages of various multi-drug resistant bacteria to evolve the favorable DNA gyrase and topoisomerase IV mutations—primarily in the double-serine residues—advanced their dissemination in fluoroquinolone environments. The reason(s) why these “competent” pathogens are more adept to favorably mutate than most strains of the same species and how previously “non-mutating” strains develop the capacity to mutate remain to be elucidated. Furthermore, our better understanding of the mechanism of clonal dynamics permitting a more judicious use of fluoroquinolone type antibiotics would allow for the amelioration of the general antibiotic resistance situation.
Author Contributions
MF devised and wrote the manuscript. DS and RC helped with their advice and provided relevant literature.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
Adam, H. J., Schurek, K. N., Nichol, K. A., Hoban, C. J., Baudry, T. J., Laing, N. M., et al. (2007). Molecular characterization of increasing fluoroquinolone resistance in Streptococcus pneumoniae isolates in Canada, 1997 to 2005. Antimicrob. Agents Chemother. 51, 198–207. doi: 10.1128/AAC.00609-06
Agnello, M., Finkel, S. E., and Wong-Beringer, A. (2016). Fitness cost of fluoroquinolone resistance in clinical isolates of Pseudomonas aeruginosa differs by type III secretion genotype. Front. Microbiol. 7:1591. doi: 10.3389/fmicb.2016.01591
Agnello, M., and Wong-Beringer, A. (2012). Differentiation in quinolone resistance by virulence genotype in Pseudomonas aeruginosa. PLoS ONE 7:e42973. doi: 10.1371/journal.pone.0042973
Alam, M. T., Read, T. D., Petit, R. A. III, Boyle-Vavra, S., Miller, L. G., Eells, S. J., et al. (2015). Transmission and microevolution of USA300 MRSA in U.S. households: evidence from whole-genome sequencing. MBio 6:e00054. doi: 10.1128/mBio.00054-15
Aldred, K. J., Kerns, R. J., and Osheroff, N. (2014). Mechanism of quinolone action and resistance. Biochemistry 53, 1565–1574. doi: 10.1021/bi5000564
Alouache, S., Estepa, V., Messai, Y., Ruiz, E., Torres, C., and Bakour, R. (2014). Characterization of ESBLs and associated quinolone resistance in Escherichia coli and Klebsiella pneumoniae isolates from an urban wastewater treatment plant in Algeria. Microb Drug Resist. 20, 30–38. doi: 10.1089/mdr.2012.0264
Ambur, O. H., Davidsen, T., Frye, S. A., Balasingham, S. V., Lagesen, K., Rognes, T., et al. (2009). Genome dynamics in major bacterial pathogens. FEMS Microbiol Rev. 33, 453–470. doi: 10.1111/j.1574-6976.2009.00173.x
Andrade, L. N., Vitali, L., Gaspar, G. G., Bellissimo-Rodrigues, F., Martinez, R., and Darini, A. L. (2014). Expansion and evolution of a virulent, extensively drug-resistant (polymyxin B-resistant), QnrS1-, CTX-M-2-, and KPC-2-producing Klebsiella pneumoniae ST11 international high-risk clone. J. Clin. Microbiol. 52, 2530–2535. doi: 10.1128/JCM.00088-14
Aoike, N., Saga, T., Sakata, R., Yoshizumi, A., Kimura, S., Iwata, M., et al. (2013). Molecular characterization of extraintestinal Escherichia coli isolates in Japan: relationship between sequence types and mutation patterns of quinolone resistance-determining regions analyzed by pyrosequencing. J. Clin. Microbiol. 51, 1692–1698. doi: 10.1128/JCM.03049-12
Aogáin, M. I. M., Kilkenny, S., Walsh, C., Lindsay, S., Moloney, G., Morris, T., et al. (2015). Identification of a novel mutation at the primary dimer interface of GyrA conferring fluoroquinolone resistance in Clostridium difficile. J. Glob. Antimicrob. Res. 3, 295–299. doi: 10.1016/j.jgar.2015.09.007
Araujo, B. F., Ferreira, M. L., Campos, P. A., Royer, S., Batistão, D. W., Dantas, R. C., et al. (2016). Clinical and molecular epidemiology of multidrug-resistant P. aeruginosa carrying aac(6′)-Ib-cr, qnrS1 and blaSPM genes in Brazil. PLoS ONE 11:e0155914. doi: 10.1371/journal.pone.0155914
Bagel, S., Hüllen, V., Wiedemann, B., and Heisig, P. (1999). Impact of gyrA and parC mutations on quinolone resistance, doubling time, and supercoiling degree of Escherichia coli. Antimicrob.Agents Chemother. 43, 868–875.
Baker, S., Duy, P. T., Nga, T. V., Dung, T. T., Phat, V. V., Chau, T. T., et al. (2013). Fitness benefits in fluoroquinolone-resistant Salmonella Typhi in the absence of antimicrobial pressure. Elife 2:e01229. doi: 10.7554/eLife.01229
Barnard, F. M., and Maxwell, A. (2001). Interaction between DNA gyrase and quinolones: effects of alanine mutations at GyrA subunit residues Ser83 and Asp87. Antimicrob. Agents Chemother. 45, 1994–2000. doi: 10.1128/AAC.45.7.1994-2000.2001
Bingen, E. H., Denamur, E., Lambert-Zechovsky, N. Y., and Elion, J. (1991). Evidence for the genetic unrelatedness of nosocomial vancomycin-resistant Enterococcus faecium strains in a pediatric hospital. J. Clin. Microbiol. 29, 1888–1892.
Bjørkeng, E., Rasmussen, G., Sundsfjord, A., Sjöberg, L., Hegstad, K., and Söderquist, B. (2011). Clustering of polyclonal VanB-type vancomycin-resistant Enterococcus faecium in a low endemic area was associated with CC17-genogroup strains harbouring transferable vanB2 Tn5382 and pRUM-like repA containing plasmids with axe-txe plasmid addiction systems. APMIS 119, 247–258. doi: 10.1111/j.1600-0463.2011.02724.x
Blanco, J., Mora, A., Mamani, R., López, C., Blanco, M., Dahbi, G., et al. (2011). National survey of Escherichia coli causing extraintestinal infections reveals the spread of drug-resistant clonal groups O25b:H4-B2-ST131, O15:H1-D-ST393 and CGA-D-ST69 with high virulence gene content in Spain. J. Antimicrob. Chemother. 66, 2011–2021. doi: 10.1093/jac/dkr235
Bowers, J. R., Kitchel, B., Driebe, E. M., MacCannell, D. R., Roe, C., Lemmer, D., et al. (2015). Genomic analysis of the emergence and rapid global dissemination of the clonal group 258 Klebsiella pneumoniae pandemic. PLoS ONE 10:e0133727. doi: 10.1371/journal.pone.0133727
Cattoir, V., and Leclercq, R. (2013). Twenty-five years of shared life with vancomycin-resistant enterococci: is it time to divorce? J. Antimicrob. Chemother. 68, 731–742. doi: 10.1093/jac/dks469
Ceyssens, P. J., Van Bambeke, F., Mattheus, W., Bertrand, S., Fux, F., Van Bossuyt, E., et al. (2016). Molecular analysis of rising fluoroquinolone resistance in Belgian non-invasive Streptococcus pneumoniae isolates (1995-2014). PLoS ONE 11:e0154816. doi: 10.1371/journal.pone.0154816
Cha, M. K., Kang, C. I., Kim, S. H., Cho, S. Y., Ha, Y. E., Wi, Y. M., et al. (2016). Comparison of the microbiological characteristics and virulence factors of ST131 and non ST131 clones among extended-spectrum β-lactamase-producing Escherichia coli causing bacteremia. Diagn. Microbiol. Infect. Dis. 84, 102–104. doi: 10.1016/j.diagmicrobio.2015.10.015
Chakrakodi, B., Prabhakara, S., Nagaraj, S., Etienne, J., and Arakere, G. (2014). High prevalence of ciprofloxacin resistance in community associated Staphylococcus aureus in a tertiary care Indian hospital. Adv. Microbiol. 4, 133–141. doi: 10.4236/aim.2014.42018
Ciesielczuk, H., Betts, J., Phee, L., Doumith, M., Hope, R., Woodford, N., et al. (2015). Comparative virulence of urinary and bloodstream isolates of extra-intestinal pathogenic Escherichia coli in a Galleria mellonella model. Virulence 6, 145–151. doi: 10.4161/21505594.2014.988095
Clark, N. C., Cooksey, R. C., Hill, B. C., Swenson, J. M., and Tenover, F. C. (1993). Characterization of glycopeptide-resistant enterococci from U.S. hospitals. Antimicrob. Agents Chemother. 37, 2311–2317. doi: 10.1128/AAC.37.11.2311
Coelho, C., Torres, C., Radhouani, H., Pinto, L., Lozano, C., Gómez-Sanz, E., et al. (2011). Molecular detection and characterization of methicillin-resistant Staphylococcus aureus (MRSA) isolates from dogs in Portugal. Microb. Drug Resist. 17, 333–337. doi: 10.1089/mdr.2010.0080
Coombs, G. W., Pearson, J. C., Daley, D. A., Le, T., Robinson, O. J., Gottlieb, T., et al. (2014). Molecular epidemiology of enterococcal bacteremia in Australia. J. Clin. Microbiol. 52, 897–905. doi: 10.1128/JCM.03286-13
Cooper, R., Segal, H., Lastovica, A. J., and Elisha, B. G. (2002). Genetic basis of quinolone resistance and epidemiology of resistant and susceptible isolates of porcine Campylobacter coli strains. J. Appl. Microbiol. 93, 241–249. doi: 10.1046/j.1365-2672.2002.01650.x
Coskun-Ari, F. F., and Bosgelmez-Tinaz, G. (2008). GrlA and gyrA mutations and antimicrobial susceptibility in clinical isolates of ciprofloxacin- methicillin-resistant Staphylococcus aureus. Eur. J. Med. Res. 13, 366–370.
Dahbi, G., Mora, A., Mamani, R., López, C., Alonso, M. P., Marzoa, J., et al. (2014). Molecular epidemiology and virulence of Escherichia coli O16:H5-ST131: comparison with H30 and H30-Rx subclones of O25b:H4-ST131. Int. J. Med. Microbiol. 304, 1247–1257. doi: 10.1016/j.ijmm.2014.10.002
Damjanova, I., Tóth, A., Pászti, J., Hajbel-Vékony, G., Jakab, M., Berta, J., et al. (2008). Expansion and countrywide dissemination of ST11, ST15 and ST147 ciprofloxacin resistant CTX-M-15-type beta-lactamase-producing Klebsiella pneumoniae epidemic clones in Hungary in 2005–the new ‘MRSAs’? J. Antimicrob. Chemother. 62, 978–985. doi: 10.1093/jac/dkn287
de Lastours, V., Maugy, E., Mathy, V., Chau, F., Rossi, B., Guérin, F., et al. (2017). Ecological impact of ciprofloxacin on commensal enterococci in healthy volunteers. J. Antimicrob. Chemother. 72, 1574–1580. doi: 10.1093/jac/dkx043
Deplano, A., Zekhnini, A., Allali, N., Couturier, M., and Struelens, M. J. (1997). Association of mutations in grlA and gyrA topoisomerase genes with resistance to ciprofloxacin in epidemic and sporadic isolates of methicillin-resistant Staphylococcus aureus. Antimicrob. Agents Chemother. 41, 2023–2025.
Diago-Navarro, E., Chen, L., Passet, V., Burack, S., Ulacia-Hernando, A., Kodiyanplakkal, R. P., et al. (2014). Carbapenem-resistant Klebsiella pneumoniae exhibit variability in capsular polysaccharide and capsule associated virulence traits. J. Infect. Dis. 210, 803–813. doi: 10.1093/infdis/jiu157
Dong, D., Zhang, L., Chen, X., Jiang, C., Yu, B., Wang, X., et al. (2013). Antimicrobial susceptibility and resistance mechanisms of clinical Clostridium difficile from a Chinese tertiary hospital. Int. J. Antimicrob. Agent 41, 80–84. doi: 10.1016/j.ijantimicag.2012.08.011
Dridi, L., Tankovic, J., Burghoffer, B., Barbut, F., and Petit, J. C. (2002). GyrA and gyrB mutations are implicated in cross-resistance to ciprofloxacin and moxifloxacin in Clostridium difficile. Antimicrob. Agents Chemother. 46, 3418–3421. doi: 10.1128/AAC.46.11.3418-3421.2002
Fallico, L., Boldrin, C., Grossato, A., Franchin, E., De Canale, E., Tommasini, T., et al. (2011). Molecular epidemiology of Enterococcus faecium isolates from an Italian hospital. Infection 39, 127–133. doi: 10.1007/s15010-011-0086-8
Fawley, W. N., Davies, K. A., Morris, T., Parnell, P., Howe, R., and Wilcox, M. H. (2016). on behalf of the Clostridium difficile Ribotyping Network (CDRN) Working Group Enhanced surveillance of Clostridium difficile infection occurring outside hospital, England, 2011 to 2013. Euro Surveill. 21:30295. doi: 10.2807/1560-7917.ES.2016.21.29.30295
Freitas, A. R., Tedim, A. P., Francia, M. V., Jensen, L. B., Novais, C., Peixe, L., et al. (2016). Multilevel population genetic analysis of vanA and vanB Enterococcus faecium causing nosocomial outbreaks in 27 countries (1986-2012). J. Antimicrob. Chemother. 71, 3351–3366. doi: 10.1093/jac/dkw312
Fuzi, M. (2016). Dissimilar fitness associated with resistance to fluoroquinolones influences clonal dynamics of various multiresistant bacteria. Front. Microbiol. 7:1017. doi: 10.3389/fmicb.2016.01017
Galloway-Peña, J. R., Nallapareddy, S. R., Arias, C. A., Eliopoulos, G. M., and Murray, B. E. (2009). Analysis of clonality and antibiotic resistance among early clinical isolates of Enterococcus faecium in the United States. J. Infect. Dis. 200, 1566–1573. doi: 10.1086/644790
Ge, B., McDermott, P. F., White, D. G., and Meng, J. (2005). Role of efflux pumps and topoisomerase mutations in fluoroquinolone resistance in Campylobacter jejuni and Campylobacter coli. Antimicrob. Agents Chemother. 49, 3347–3354. doi: 10.1128/AAC.49.8.3347-3354.2005
Gillespie, S. H., Voelker, L. L., and Dickens, A. (2002). Evolutionary barriers to quinolone resistance in Streptococcus pneumoniae. Microb. Drug Resist. 8, 79–84. doi: 10.1089/107662902760190617
Giraud, E., Cloeckaert, A., Baucheron, S., Mouline, C., and Chaslus-Dancla, E. (2003). Fitness cost of fluoroquinolone resistance in Salmonella enterica serovar Typhimurium. J. Med. Microbiol. 52, 697–703. doi: 10.1099/jmm.0.05178-0
Gordts, B., Van Landuyt, H., Leven, M., Vandamme, P., and Goossens, H. (1995). Vancomycin-resistant enterococci colonizing intestinal tracts of hospitalized patients. J. Clin. Microbiol. 33, 2842–2846.
Grundmann, H., Schouls, L. M., Aanensen, D. M., Pluister, G. N., Tami, A., Chlebowicz, M., et al. (2014). The dynamic changes of dominant clones of Staphylococcus aureus causing bloodstream infections in the European region: results of a second structured survey. Euro. Surveill. 19:20987. doi: 10.2807/1560-7917.ES2014.19.49.20987
Guillard, T., Bertrand, X., de Champs, C., Cholley, P., Bajolet, O., and Gbaguidi-Haore, H. (2014). aac(6′)-Ib-cr is the major plasmid-mediated quinolone resistance determinant in extended-spectrum-β-lactamase-producing Escherichia coli in eastern France. J. Glob. Antimicrob. Resist. 2, 111–113. doi: 10.1016/j.jgar.2014.01.006
Guzman Prieto, A. M., van Schaik, W., Rogers, M. R., Coque, T. M., Baquero, F., Corander, J., et al. (2016). Global emergence and dissemination of enterococci as nosocomial pathogens: attack of the clones? Front. Microbiol. 7:788. doi: 10.3389/fmicb.2016.00788
Han, J. H., Garrigan, C., Johnston, B., Nachamkin, I., Clabots, C., Bilker, W. B., et al. (2017). Epidemiology and characteristics of Escherichia coli sequence type 131 (ST131) from long-term care facility residents colonized intestinally with fluoroquinolone-resistant Escherichia coli. Diagn. Microbiol. Infect. Dis. 87, 275–280. doi: 10.1016/j.diagmicrobio.2016.11.016
Han, J., Wang, Y., Sahin, O., Shen, Z., Guo, B., Shen, J., et al. (2012). A fluoroquinolone resistance associated mutation in gyrA affects DNA supercoiling in Campylobacter jejuni. Front. Cell. Infect. Microbiol. 2:21. doi: 10.3389/fcimb.2012.00021
He, M., Miyajima, F., Roberts, P., Ellison, L., Pickard, D. J., Martin, M. J., et al. (2013). Emergence and global spread of epidemic healthcare-associated Clostridium difficile. Nat. Genet. 45, 109–113. doi: 10.1038/ng.2478
Hiasa, H. (2002). The glu-84 of the parC subunit plays critical roles in both topoisomerase IV–quinolone and topoisomerase IV–DNA interactions. Biochemistry 41, 11779–11785. doi: 10.1021/bi026352v
Higgins, P. G., Fluit, A. C., Milatovic, D., Verhoef, J., and Schmitz, F. J. (2003). Mutations in GyrA, ParC, MexR and NfxB in clinical isolates of Pseudomonas aeruginosa. Int. J. Antimicrob. Agents 21, 409–413. doi: 10.1016/S0924-8579(03)00009-8
Hiramatsu, K., Igarashi, M., Morimoto, Y., Baba, T., Umekita, M., and Akamatsu, Y. (2012). Curing bacteria of antibiotic resistance: reverse antibiotics, a novel class of antibiotics in nature. Int. J. Antimicrob. Agents 39, 478–485. doi: 10.1016/j.ijantimicag.2012.02.007
Holden, M. T., Hsu, L. Y., Kurt, K., Weinert, L. A., Mather, A. E., Harris, S. R., et al. (2013). A genomic portrait of the emergence, evolution, and global spread of a methicillin resistant Staphylococcus aureus pandemic. Genome Res. 23, 653–664. doi: 10.1101/gr.147710.112
Holt, K. E., Wertheim, H., Zadoks, R. N., Baker, S., Whitehouse, C. A., Dance, D., et al. (2015). Genomic analysis of diversity, population structure, virulence, and antimicrobial resistance in Klebsiella pneumoniae, an urgent threat to public health. Proc. Natl. Acad. Sci. U.S.A. 112, E3574–E3581. doi: 10.1073/pnas.1501049112
Hooper, D. C., and Jacoby, G. A. (2015). Mechanisms of drug resistance: quinolone resistance. Ann. N.Y. Acad. Sci. 1354:1231. doi: 10.1111/nyas.12830
Horváth, A., Dobay, O., Kardos, S., Ghidán, Á., Tóth, Á., Pászti, J., et al. (2012). Varying fitness cost associated with resistance to fluoroquinolones governs clonal dynamic of methicillin- resistant Staphylococcus aureus. Eur. J. Clin. Microbiol. Infect. Dis. 31, 2029–2036. doi: 10.1007/s10096-011-1536-z
Hsieh, Y. C., Chang, L. Y., Huang, Y. C., Lin, H. C., Huang, L. M., Hsueh, P. R., et al. (2010). Circulation of international clones of levofloxacin non-susceptible Streptococcus pneumoniae in Taiwan. Clin. Microbiol. Infect. 16, 973–978. doi: 10.1111/j.1469-0691.2009.02951.x
Huang, H., Weintraub, A., Fang, H., Wu, S., Zhang, Y., and Nord, C. E. (2010). Antimicrobial susceptibility and heteroresistance in Chinese Clostridium difficile strains. Anaerobe 16, 633–635. doi: 10.1016/j.anaerobe.2010.09.002
Huang, H., Wu, S., Wang, M., Zhang, Y., Fang, H., Palmgren, A.-C., et al. (2009). Clostridium difficile infections in a Shanghai hospital: antimicrobial resistance, toxin profiles and ribotypes. Int. J. Antimicrob. Agents 33, 339–342. doi: 10.1016/j.ijantimicag.2008.09.022
Huseby, D. L., Pietsch, F., Brandis, G., Garoff, L., Tegehall, A., and Hughes, D. (2017). Mutation supply and relative fitness shape the genotypes of ciprofloxacin-resistant Escherichia coli. Mol. Biol. Evol. 34, 1029–1039. doi: 10.1093/molbev/msx052
Iihara, H., Suzuki, T., Kawamura, Y., Ohkusu, K., Inoue, Y., Zhang, W., et al. (2006). Emerging multiple mutations and high-level fluoroquinolone resistance in methicillin- resistant Staphylococcus aureus isolated from ocular infections. Diagn. Microbiol. Infect. Dis. 56, 297–303. doi: 10.1016/j.diagmicrobio.2006.04.017
Iovine, N. M. (2013). Resistance mechanisms in Campylobacter jejuni. Virulence 4, 230–240. doi: 10.4161/viru.23753
Jesse, T. W., Englen, M. D., Pittenger-Alley, L. G., and Fedorka-Cray, P. J. (2006). Two distinct mutations in gyrA lead to ciprofloxacin and nalidixic acid resistance in Campylobacter coli and Campylobacter jejuni isolated from chickens and beef cattle. J. Appl. Microbiol. 100, 682–688. doi: 10.1111/j.1365-2672.2005.02796.x
Johnson, C. N., Briles, D. E., Benjamin, W. H. Jr., Hollingshead, S. K., and Waites, K. B. (2005). Relative fitness of fluoroquinolone-resistant Streptococcus pneumoniae. Emerging Infect. Dis. 11, 814–820. doi: 10.3201/eid1106.040840
Johnson, J. R., Johnston, B., Kuskowski, M. A., Sokurenko, E. V., and Tchesnokova, V. (2015). Intensity and mechanisms of fuoroquinolone resistance within the H30 and H30Rx subclones of Escherichia coli sequence type 131 compared with other fluoroquinolone resistant E. coli. Antimicrob. Agents Chemother. 59, 4471–4480. doi: 10.1128/AAC.00673-15
Jordens, J. Z., Bates, J., and Griffiths, D. T. (1994). Faecal carriage and nosocomial spread of vancomycin-resistant Enterococcus faecium. J. Antimicrob. Chemother. 3, 515–528. doi: 10.1093/jac/34.4.515
Jørgensen, K. M., Wassermann, T., Jensen, P. Ø., Hengzuang, W., Molin, S., Høiby, N., et al. (2013). Sublethal ciprofloxacin treatment leads to rapid development of high-level ciprofloxacin resistance during long-term experimental evolution of Pseudomonas aeruginosa. Antimicrob. Agents Chemother. 57, 4215–4221. doi: 10.1128/AAC.00493-13
Kaatz, G. W., and Seo, S. M. (1998). Topoisomerase mutations in fluoroquinolone-resistant and methicillin-susceptible and resistant clinical isolates of Staphylococcus aureus. Antimicrob. Agents Chemother. 42, 197–198.
Kang, M., Xie, Y., He, C., Chen, Z. X., Guo, L., Yang, Q., et al. (2014). Molecular characteristics of vancomycin-resistant Enterococcus faecium from a tertiary care hospital in Chengdu, China: molecular characteristics of VRE in China. Eur. J. Clin. Microbiol. Infect. Dis. 33, 933–939. doi: 10.1007/s10096-013-2029-z
Khan, M. A., van der Wal, M., Farrell, D. J., Cossins, L., van Belkum, A., Alaidan, A., et al. (2008). Analysis of VanA vancomycin-resistant Enterococcus faecium isolates from Saudi Arabian hospitals reveals the presence of clonal cluster 17 and two new Tn1546 lineage types. J. Antimicrobial. Chemother. 62, 279–283. doi: 10.1093/jac/dkn173
Khokhlova, O. E., Hung, W. C., Wan, T. W., Iwao, Y., Takano, T., Higuchi, W., et al. (2015). Healthcare- and community-associated methicillin-resistant Staphylococcus aureus (MRSA) and fatal pneumonia with pediatric deaths in Krasnoyarsk, Siberian Russia: Unique MRSA'smultiplevirulence factors, genome, and stepwise evolution. PLoS One 10:e0128017. doi: 10.1371/journal.pone.0128017
Kim, S. Y., Park, Y. J., Johnson, J. R., Yu, J. K., Kim, Y. K., and Kim, Y. S. (2016). Prevalence and characteristics of Escherichia coli sequence type 131 and its H30 and H30Rx subclones: a multicenter study from Korea. Diagn. Microbiol. Infect. Dis. 84, 97–101. doi: 10.1016/j.diagmicrobio.2015.10.016
Klare, I., Konstabel, C., Mueller-Bertling, S., Werner, G., Strommenger, B., Kettlitz, C., et al. (2005). Spread of ampicillin/vancomycin-resistant Enterococcus faecium of the epidemic-virulent clonal complex-17 carrying the genes esp and hyl in German hospitals. Eur. J. Clin. Microbiol. Infect. Dis. 24, 815–825. doi: 10.1007/s10096-005-0056-0
Knight, G. M., Budd, E. L., Whitney, L., Thornley, A., Al-Ghusein, H., Planche, T., et al. (2012). Shift in dominant hospital-associated methicillin-resistant Staphylococcus aureus (HA-MRSA) clones over time. J. Antimicrob. Chemother. 67, 2514–2522. doi: 10.1093/jac/dks245
Komp Lindgren, P., Marcusson, L. L., Sandvang, D., Frimodt-Møller, N., and Hughes, D. (2005). Biological cost of single and multiple norfloxacin resistance mutations in Escherichia coli implicated in urinary tract infections. Antimicrob. Agents Chemother. 49, 2343–2345 doi: 10.1128/AAC.49.6.2343-2351.2005
Kong, Q., Beanan, J. M., Olson, R., Macdonald, U., Shon, A. S., Metzger, D. J., et al. (2012). Biofilm formed by a hypervirulent (hypermucoviscous) variant of Klebsiella pneumoniae doeS not enhance serum resistance or survival in an in vivo abscess model. Virulence 3, 309–318. doi: 10.4161/viru.20383
Kuwata, Y., Tanimoto, S., Sawabe, E., Shima, M., Takahashi, Y., Ushizawa, H., et al. (2015). Molecular epidemiology and antimicrobial susceptibility of Clostridium difficile isolated from a university teaching hospital in Japan. Eur. J. Clin. Microbiol. Infect. Dis. 34, 763–772. doi: 10.1007/s10096-014-2290-9
Kwak, Y. G., Jacoby, G. A., and Hooper, D. C. (2013). Induction of plasmid-carried qnrS1 in Escherichia coli by naturally occurring quinolones and quorum-sensing signal molecules. Antimicrob. Agents Chemother. 57, 4031–4034. doi: 10.1128/AAC.00337-13
Leavis, H. L., Bonten, M. J., and Willems, R. J. (2006a). Identification of high-risk enterococcal clonalcomplexes: global dispersion and antibiotic resistance. Curr. Opin. Microbiol. 9, 454–460. doi: 10.1016/j.mib.2006.07.001
Leavis, H. L., Willems, R. J. L., Top, J., Marc, J., and Bonten, M. (2006b). High-level ciprofloxacin resistance from point mutations in gyrA and parC confined to global hospital-adapted clonal lineage CC17 of Enterococcus faecium. J. Clin. Microbiol. 44, 1059–1064. doi: 10.1128/JCM.44.3.1059-1064.2006
Lee, I. R., Molton, J. S., Wyres, K. L., Gorrie, C., Wong, J., Hoh, C. H., et al. (2016). Differential host susceptibility and bacterial virulence factors driving Klebsiella liver abscess in an ethnically diverse population. Sci. Rep. 6:29316. doi: 10.1038/srep29316
Lee, J. K., Lee, Y. S., Park, Y. K., and Kim, B. S. (2005). Alterations in the GyrA and GyrB subunits of topoisomerase II and the ParC and ParE subunits of topoisomerase IV in ciprofloxacin-resistant clinical isolates of Pseudomonas aeruginosa. Int. J. Antimicrob. Agents 25, 290–295. doi: 10.1016/j.ijantimicag.2004.11.012
Lin, Y. C., Huang, Y. T., Tsai, P. J., Lee, T. F., Lee, N. Y., Liao, C. H., et al. (2011). Antimicrobial susceptibilities and molecular epidemiology of clinical isolates of Clostridium difficile in taiwan. Antimicrob. Agents Chemother. 55, 1701–1705. doi: 10.1128/AAC.01440-10
Kugelberg, E., Löfmark, S., Wretlind, B., and Andersson, D. I. (2005). Reduction of the fitness burden of quinolone resistance in Pseudomonas eruginosa. J.Antimicrob. Chemother. 55, 22–30. doi: 10.1093/jac/dkh505
López, M., Sáenz, Y., Alvarez-Martínez, M. J., Marco, F., Robredo, B., Rojo-Bezares, B., et al. (2010). Tn1546 structures and multilocus sequence typing of vanA-containing enterococci of animal, human and food origin. J. Antimicrob. Chemother. 65, 1570–1575. doi: 10.1093/jac/dkq192
Lozano, C., Rezusta, A., Gómez, P., Gómez-Sanz, E., Báez, N., Martin-Saco, G., et al. (2012). High prevalence of spa types associated with the clonal lineage CC398 among tetracycline resistant methicillin-resistant Staphylococcus aureus strains in a Spanish hospital. J. Antimicrob. Chemother. 67, 330–334. doi: 10.1093/jac/dkr497
Luo, N., Pereira, S., Sahin, O., Lin, J., Huang, S., Michel, L., et al. (2005). Enhanced in vivo fitness of fluoroquinolone-resistant Campylobacter jejuni in the absence of antibiotic selectio pressure. Proc. Natl. Acad. Sci. U.S.A. 102, 541–546. doi: 10.1073/pnas.0408966102
Machuca, J., Briales, A., Díaz-de-Alba, P., Martínez-Martínez, L., Pascual, Á., and Rodríguez-Martínez, J. M. (2015). Effect of the efflux pump QepA2 combined with chromosomally mediated mechanisms on quinolone resistance and bacterial fitness in Escherichia coli. J. Antimicrob. Chemother. 70, 2524–2527. doi: 10.1093/jac/dkv144
Machuca, J., Briales, A., Labrador, G., Díaz-de-Alba, P., López-Rojas, R., Docobo-Pérez, F., et al. (2014). Interplay between plasmid mediated and chromosomal-mediated fluoroquinolone resistance and bacterial fitness in Escherichia coli. J. Antimicrob. Chemother. 69, 320315 doi: 10.1093/jac/dku308
Miyoshi-Akiyama, T., Sherchan, J. B., Doi, Y., Nagamatsu, M., Sherchan, J. B., Tandukar, S., et al. (2016). Comparative genome analysis of extended-spectrum-β-lactamase-producing Escherichia coli sequence type 131 strains from Nepal and Japan. mSphere. 1:e00289-16. doi: 10.1128/mSphere.00289-16
Malik, M., Mustaev, A., Schwanz, H. A., Luan, G., Shah, N., Oppegard, L. M., et al. (2016). Suppression of gyrase-mediated resistance by C7 aryl fluoroquinolones. Nucleic Acids Res. 44, 3304–3316. doi: 10.1093/nar/gkw161
Marcusson, L. L., Frimodt-Møller, N., and Hughes, D. (2009). Interplay in the selection of fluoroquinolone resistance and bacterial fitness. PLoS Pathog. 5:e1000541. doi: 10.1371/journal.ppat.1000541
Martinez, J. L., Sánchez, M. B., Martínez-Solano, L., Hernandez, A., Garmendia, L., Fajardo, A., et al. (2009). Functional role of bacterial multidrug efflux pumps in microbial natural ecosystems. FEMS Microbiol. Rev. 33, 430–449. doi: 10.1111/j.1574-6976.2008.00157.x
Mato, R., Almeida, F., Pires, R., Rodrigues, P., Ferreira, T., and Santos-Sanches, I. (2009). Assessment of high-level gentamicin and glycopeptide-resistant Enterococcus faecalis and E. faecium clonal structure in a Portuguese hospital over a 3-year period. Eur. J. Clin. Microbiol. Infect. Dis. 28, 855–859. doi: 10.1007/s10096-009-0704-x
Melegh, S., Schneider, G., Horváth, M., Jakab, F., Emody, L., and Tigyi, Z. (2015). Identification and characterization of CTX-M-15 producing Klebsiella pneumoniae clone ST101 in aHungarian university teaching hospital. Acta Microbiol. Immunol. Hung. 62, 233–245. doi: 10.1556/030.62.2015.3.2
Michon, A., Allou, N., Chau, F., Podglajen, I., Fantin, B., and Cambau, E. (2011). Plasmidic qnrA3 enhances Escherichia coli fitness in absence of antibiotic exposure. PLoS ONE 6:e24552. doi: 10.1371/journal.pone.0024552
Morimoto, Y., Baba, T., Sasaki, T., and Hiramatsu, K. (2015). Apigenin as an anti-quinolone-resistance antibiotic. Int. J. Antimicrob. Agents 4, 666–673. doi: 10.1016/j.ijantimicag.2015.09.006
Moulin, F. S., Saulnier, D. P., Chachaty, E., Loubeyre, C., Brugieres, L., and Andremont, A. (1996). Surveillance of intestinal colonisation and infection by vancomycin resistant enterococci in hospitalized cancer patients. Clin. Microbiol. Infect. 2, 192–201. doi: 10.1016/S1198-743X(14)65142-9
Mustaev, A., Malik, M., Zhao, X., Kurepina, N., Luan, G., Oppegard, L. M., et al. (2014). Fluoroquinolone-gyrase-DNA complexes: two modes of drug binding. J. Biol. Chem. 289, 12300–12312. doi: 10.1074/jbc.M113.529164
Musumeci, R., Rausa, M., Giovannoni, R., Cialdella, A., Bramati, S., Sibra, B., et al. (2012). Prevalence of plasmid-mediated quinolone resistance genes in uropathogenic Escherichia coli isolated in a teaching hospital of northern Italy. Microb. Drug Resist. 18, 33–41. doi: 10.1089/mdr.2010.0146
Nagasaka, Y., Kimura, K., Yamada, K., Wachino, J., Jin, W., Notake, S., et al. (2015). Genetic profiles of fluoroquinolone-nonsusceptible Klebsiella pneumoniae among cephalosporin-resistant K. pneumoniae. Microb. Drug Resist. 21, 224–233. doi: 10.1089/mdr.2014.0150
Noguchi, N., Okihara, T., Namiki, Y., Kumaki, Y., Yamanaka, Y., Koyama, M., et al. (2005). Susceptibility and resistance genes to fluoroquinolones in methicillin-resistant Staphylococcus aureus isolated in 2002. Int. J. Antimicrob. Agents 25, 374–379. doi: 10.1016/j.ijantimicag.2004.11.016
Nouri, R., Ahangarzadeh Rezaee, M., Hasani, A., Aghazadeh, M., and Asgharzadeh, M. (2016). The role of gyrA and parC mutations in fluoroquinolones-resistant Pseudomonas aeruginosa isolates from Iran. Braz. J. Microbiol. 47, 925–930. doi: 10.1016/j.bjm.2016.07.016
Nübel, U., Strommenger, B., Layer, F., and Witte, W. (2011). From types to trees: reconstructing the spatial spread of Staphylococcus aureus based on DNA variation. Int. J. Med. Microbiol. 301, 614–618. doi: 10.1016/j.ijmm.2011.09.007
Olesen, B., Frimodt-Møller, J., Leihof, R. F., Struve, C., Johnston, B., Hansen, D. S., et al. (2014). Temporal trends in antimicrobial resistance and virulence-associated traits within the Escherichia coli sequence type 131 clonal group and its H30 and H30-Rx subclones, 1968 to 2012. Antimicrob. Agents Chemother. 58, 6886–6895. doi: 10.1128/AAC.03679-14
Paltansing, S., Kraakman, M. E., Ras, J. M., Wessels, E., and Bernards, A. T. (2013). Characterization of fluoroquinolone and cephalosporin resistance mechanisms in Enterobacteriaceae isolated in a Dutch teaching hospital reveals the presence of an Escherichia coli ST131 clone with a specific mutation in parE. J. Antimicrob. Chemother. 68, 40–45. doi: 10.1093/jac/dks365
Pan, X. S., Yague, G., and Fisher, L. M. (2017). Quinolone resistance mutations in Streptococcus pneumoniae GyrA and ParC proteins: mechanistic insights into quinolone action from enzymatic analysis, intracellular levels, and phenotypes of wild-type and mutant proteins. Antimicrob. Agents Chemother. 45, 3140–3147. doi: 10.1128/AAC.45.11.3140-3147.2001
Park, D. J., Yu, J. K., Park, K. G., and Park, Y. J. (2015). Genotypes of ciprofloxacin-resistant Klebsiella pneumoniae in Korea and their characteristics according to the genetic lineages. Microb. Drug Resist. 21, 622–630. doi: 10.1089/mdr.2015.0001
Pitout, J. D., and DeVinney, R. (2017). Escherichia coli ST131: a multidrug-resistant clone primed for global domination. F1000Res. 6:195. doi: 10.12688/f1000research.10609.1
Pletz, M. W., McGee, L., Jorgensen, J., Beall, B., Facklam, R. R., Whitney, C. G., et al. (2004). Levofloxacin-resistant invasive Streptococcus pneumoniae in the United States: evidence for clonal spread and the impact of conjugate pneumococcal vaccine. Antimicrob. Agents Chemother. 48, 3491–3497. doi: 10.1128/AAC.48.9.3491-3497.2004
Pope, C. F., Gillespie, S. H., Pratten, J. R., and McHugh, T. D. (2008). Fluoroquinolone-resistant mutants of Burkholderia cepacia. Antimicrob. Agents Chemother. 52, 1201–1203. doi: 10.1128/AAC.00799-07
Qin, X., Galloway-Peña, J. R., Sillanpaa, J., Roh, J. H., Nallapareddy, S. R., Chowdhury, S., et al. (2012). Complete genome sequence of Enterococcus faecium strain TX16 and comparative genomic analysis of Enterococcus faecium genomes. BMC Microbiol. 12:135. doi: 10.1186/1471-2180-12-135
Reyna-Flores, F., Barrios, H., Garza-Ramos, U., Sánchez-Pérez, A., Rojas-Moreno, T., Uribe-Salas, F. J., et al. (2013). Molecular epidemiology of Escherichia coli O25b-ST131 isolates causing community acquired UTIs in Mexico. Diagn. Microbiol. Infect. Dis. 76, 396–398. doi: 10.1016/j.diagmicrobio.2013.03.026
Röderova, M., Halova, D., Papousek, I., Dolejska, M., Masarikova, M., Hanulik, V., et al. (2017). Characteristics of quinolone resistance in Escherichia coli Isolates from humans, animals, and the environment in the Czech Republic. Front. Microbiol. 7:2147. doi: 10.3389/fmicb.2016.02147
Rodríguez-Avial, I., Ramos, B., Ríos, E., Cercenado, E., Ordobás, M., Sanz, J. C., et al. (2011). Clonal spread of levofloxacin-resistant Streptococcus pneumoniae invasive isolates in Madrid, Spain, 2007 to 2009. Antimicrob. Agents Chemother. 55, 2469–2471. doi: 10.1128/AAC.01380-10
Rozen, D. E., McGee, L., Levin, B. R., and Klugman, K. P. (2007). Fitness costs of fluoroquinolone resistance in Streptococcus pneumoniae. Antimicrob. Agents Chemother. 51, 412–416. doi: 10.1128/AAC.01161-06
Rudolf, D., Michaylov, N., van der Linden, M., Hoy, L., Klugman, K. P., Welte, T., et al. (2011). International pneumococcal clones match or exceed the fitness of other strains despite the accumulation of antibiotic resistance. Antimicrob. Agents Chemother. 55, 4915–4917. doi: 10.1128/AAC.00250-11
Sadowy, E., Sienko, A., Gawryszewska, I., Bojarska, A., Malinowska, K., and Hryniewicz, W. (2013). High abundance and diversity of antimicrobial resistance determinants among early vancomycin-resistant Enterococcus faecium in Poland. Eur. J. Clin. Microbiol. Infect. Dis. 32, 1193–1203. doi: 10.1007/s10096-013-1868-y
Sánchez, P., Linares, J. F., Ruiz-Díez, B., Campanario, E., Navas, A., Baquero, F., et al. (2002). Fitness of in vitro selected Pseudomonas aeruginosa nalB and nfxB multidrug resistant mutants. J. Antimicrob. Chemother. 50, 657–664. doi: 10.1093/jac/dkf185
Schmitz, J., van der Linden, M., Al-Lahham, A., Levina, N., Pletz, M. W., and Imöhl, M. (2017). Fluoroquinolone resistance in Streptococcus pneumoniae isolates in Germany from 2004–2005 to 2014–2015. Int. J. Med. Microbiol. 307, 216–222. doi: 10.1016/j.ijmm.2017.04.003
Sekyere, O. I., and Amoako, D. G. (2017). Genomic and phenotypic characterisation of fluoroquinolone resistance mechanisms in Enterobacteriaceae in Durban, South Africa. PLoS ONE 12:e0178888. doi: 10.1371/journal.pone.0178888
Sierra, J. M., Marco, F., Ruiz, J., Jiménez de Anta, M. T., and Vila, J. (2002). Correlation between the activity of different fluoroquinolones and the presence of mechanisms of quinolone resistance in epidemiologically related and unrelated strains of methicillin-susceptible and -resistant Staphylococcus aureus. Clin. Microbiol. Infect. 8, 781–790. doi: 10.1046/j.1469-0691.2002.00400.x
Spigaglia, P., Carattoli, A., Barbanti, F., and Mastrantonio, P. (2010). Detection of gyrA and gyrB mutations in Clostridium difficile isolates by real-time PCR. Mol. Cell. Probes 24, 61–67. doi: 10.1016/j.mcp.2009.10.002
Stahl, M., and Stintzi, A. (2011). Identification of essential genes in C. jejuni genome highlights hyper-variable plasticity regions. Funct. Integr. Genomics 11, 241–257. doi: 10.1007/s10142-011-0214-7
Struve, C., Roe, C. C., Stegger, M., Stahlhut, S. G., Hansen, D. S., Engelthaler, D. M., et al. (2015). Mapping the evolution of hypervirulent Klebsiella pneumoniae. MBio. 6:e00630. doi: 10.1128/mBio.00630-15
Takahata, M., Yonezawa, M., Kurose, S., Futakuchi, N., Matsubara, N., Watanabe, Y., et al. (1996). Mutations in the gyrA and grlA genes of quinolone-resistant clinical isolates of methicillin-resistant Staphylococcus aureus. J. Antimicrob. Chemother. 38, 543–546. doi: 10.1093/jac/38.3.543
Takeuchi, N., Ohkusu, M., Hoshino, T., Naito, S., Takaya, A., Yamamoto, T., et al. (2017). Emergence of quinolone-resistant strains in Streptococcus pneumoniae isolated from paediatric patients since the approval of oral fluoroquinolones in Japan. J. Infect. Chemother. 23, 218–223. doi: 10.1016/j.jiac.2016.12.012
Takano, T., Higuchi, W., Zaraket, H., Otsuka, T., and Baranovich, T., Enany, S., et al. (2008). Novel characteristics of community-acquired methicillin-resistant Staphylococcus aureus strains belonging to multilocus sequence type 59 in Taiwan. Antimicrob. Agents Chemother. 52, 837–845. doi: 10.1128/AAC.01001-07
Top, J., Willems, R., van der Velden, S., Asbroek, M., and Bonten, M. (2008). Emergence of clonal complex 17 Enterococcus faecium in the Netherlands. J. Clin. Microbiol. 46, 214–219. doi: 10.1128/JCM.01351-07
Tóth, A., Kocsis, B., Damjanova, I., Kristóf, K., Jánvári, L., Pászti, J., et al. (2014). Fitness cost associated with resistance to fluoroquinolones is diverse across clones of Klebsiella pneumoniae and may select for CTX-M-15 type extended-spectrum β lactamase. Eur. J. Clin. Microbiol. Infect. Dis. 33, 837–843. doi: 10.1007/s10096-013-2022-6
van den Bogaard, A. E., Mertens, P., London, N. H., and Stobberingh, E. E. (1997). High prevalence of colonization with vancomycin- and pristinamycin-resistant enterococci in healthy humans and pigs in the Netherlands: is the addition of antibiotics to animal feeds to blame? J. Antimicrob. Chemother. 40, 454–456. doi: 10.1093/jac/40.3.454
van den Braak, N., van Belkum, A., van Keulen, M., Vliegenthart, J., Verbrugh, H. A., and Endtz, H. P. (1998). Molecular characterization of vancomycin-resistant enterococci from hospitalized patients and poultry products in the Netherlands. J. Clin. Microbiol. 36, 1927–1932.
Walkty, A., Boyd, D. A., Gravel, D., Hutchinson, J., McGeer, A., Moore, D., et al. (2010). Molecular characterization of moxifloxacin resistance from Canadian Clostridium difficile clinical isolates. Diagn. Microbiol. Infect. Dis. 66, 419–424. doi: 10.1016/j.diagmicrobio.2009.12.002
Wasels, F., Kuehne, S. A., Cartman, S. T., Spigaglia, P., Barbanti, F., Minton, N. P., et al. (2015). Fluoroquinolone resistance does not impose a cost on the fitness of Clostridium difficile in vitro. Antimicrob. Agents Chemother. 59, 1794–1796. doi: 10.1128/AAC.04503-14
Werner, G., Coque, T. M., Hammerum, A. M., Hope, R., Hryniewicz, W., Johnson, A., et al. (2008). Emergence and spread of vancomycin resistance among enterococci in Europe. Euro. Surveill. 13, 19046.
Werner, G., Fleige, C., Ewert, B., Laverde-Gomez, J. A., Klare, I., and Witte, W. (2010). High-level ciprofloxacin resistance among hospital-adapted Enterococcus faecium (CC17). Int. J. Antimicrob. Agents 35, 119–125. doi: 10.1016/j.ijantimicag.2009.10.012
Willems, R. J., Top, J., van Den Braak, N., van Belkum, A., Endtz, H., Mevius, D., et al. (2000). Host specificity of vancomycin-resistant Enterococcus faecium. J. Infect. Dis. 182, 816–823. doi: 10.1086/315752
Willems, R. J., Top, J., van Santen, M., Robinson, D. A., Coque, T. M., Baquero, F., et al. (2005). Global spread of vancomycin-resistant Enterococcus faecium from distinct nosocomial genetic complex. Emerg. Infect. Dis. 11, 821–828. doi: 10.3201/1106.041204
Witte, W., Enright, M., Schmitz, F. J., Cuny, C., Braulke, C., and Heuck, D. (2001). Characteristics of a new epidemic MRSA in Germany ancestral to United Kingdom EMRSA 15. Int. J. Med. Microbiol. 290, 677–682. doi: 10.1016/S1438-4221(01)80006-0
Yang, X., Xing, B., Liang, C., Ye, Z., and Zhang, Y. (2015). Prevalence and fluoroquinolone resistance of Pseudomonas aeruginosa in a hospital of South China. Int. J. Clin. Exp. Med. 8, 1386–1390.
Zeitouni, S., and Kempf, I. (2011). Fitness cost of fluoroquinolone resistance in Campylobacter coli and Campylobacter jejuni. Microb. Drug Resist. 17, 171–179. doi: 10.1089/mdr.2010.0139
Keywords: double-serine, QRDR, International clones, multiresistant pathogens, promotion of dissemination
Citation: Fuzi M, Szabo D and Csercsik R (2017) Double-Serine Fluoroquinolone Resistance Mutations Advance Major International Clones and Lineages of Various Multi-Drug Resistant Bacteria. Front. Microbiol. 8:2261. doi: 10.3389/fmicb.2017.02261
Received: 30 June 2017; Accepted: 02 November 2017;
Published: 16 November 2017.
Edited by:
Manuela Caniça, Istituto Nacional de Saúde, PortugalReviewed by:
Max Maurin, Université Grenoble Alpes, FranceZiad Daoud, University of Balamand, Lebanon
Copyright © 2017 Fuzi, Szabo and Csercsik. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Miklos Fuzi, miklosfuzi@gmail.com
 Miklos Fuzi
Miklos Fuzi Dora Szabo
Dora Szabo