Malnutrition upon Hospital Admission in Geriatric Patients: Why Assess It?
- Clinical Nutrition, Istituto Nazionale di Riposo e Cura per Anziani (IRCCS), Ancona, Italy
Objective: To assess the prevalence of malnutrition according to the new ESPEN definition in a population of geriatric hospital patients and to determine how malnutrition affects the length of hospital stay (LOS) and hospital mortality.
Design: A retrospective analysis of data gathered during nutritional screening surveys carried out three consecutive years, from 2012 to 2014, in an Italian geriatric research hospital (INRCA, Ancona) was performed. On the day of the study, demographic data, data on clinical conditions and the nutritional status of newly admitted patients were collected. Patients were screened for malnutrition risk using the Malnutrition Universal Screening Tool (MUST). Subsequently, malnutrition was diagnosed, for subjects at high risk, following the criteria suggested by the European Association for Clinical Nutrition and Metabolism [body mass index (BMI) < 18.5 kg/m2 or different combinations of unintentional weight loss over time and BMI values]. Sensitivity, specificity, positive and negative predictive value of MUST compared to ESPEN criteria were assessed. The characteristics of patients with a diagnosis of malnutrition were compared to those of non-malnourished patients. The impact of malnutrition on LOS and hospital mortality was investigated through logistic and linear regression models.
Setting: The study was performed in an Italian geriatric research hospital (INRCA, Ancona).
Subjects: Two hundred eighty-four newly hospitalized geriatric patients from acute care wards (mean age 82.8 ± 8.7 years), who gave their written consent to participate in the study, were enrolled.
Results: According to the MUST, high risk of malnutrition at hospitalization was found in 28.2% of patients. Malnutrition was diagnosed in 24.6% of subjects. The malnutrition was an independent predictor of both the LOS and hospital mortality. The multivariate analyses—linear and logistic regression—were performed considering different potential confounders contemporarily. The results showed that the malnutrition is an independent predictor of LOS and hospital mortality. Malnourished subjects were hospitalized almost 3 days longer compared to non-malnourished patients (p = 0.047; CI 0.04–5.80). The risk of death during hospitalization was 55% higher for malnourished patients (p = 0.037; CI 0.21–0.95).
Conclusion: A new ESPEN consensus of malnutrition was easily applicable in a population of geriatric hospital patients. Given that the nutritional status of geriatric patients was strongly correlated with the LOS and hospital mortality, the use of this simple and non-time consuming tool is highly recommended in clinical practice.
Introduction
Malnutrition is a broad term used to define different deviations from a normal nutritional state. The imbalance between nutritional intake and nutritional requirements may result in undernutrition (deficiency of one or more essential nutrients) or in overnutrition (excess of nutrients) (1–3). Protein-energy undernutrition, in particular, is a state of energy and protein insufficiency resulting either from reduced nutrient intake, impaired absorption and assimilation, increased energy expenditure, or a combination of these (4, 5). There is an extensive scientific literature on the clinical and economic consequences of protein-energy malnutrition (6, 7). It has been determined that malnutrition compromises the immune response and increases the risk of infections and infection-related complications, slows down the wound-healing process, delays recovery from illness, prolongs hospitalization, and increases the risk of death (8–10). Once the correlation between malnutrition and clinical outcomes was discovered, nutritional screening of hospital patients became mandatory in numerous countries. In order to develop an appropriate nutritional plan and intervene immediately, the screening of patients’ nutritional status is normally performed on hospital admission. For this purpose, numerous screening tools have been developed and validated (11, 12). Some studies found that more than 90% of newly admitted geriatric patients present with protein-energy malnutrition or are at risk of malnutrition (13, 14). During hospitalization, numerous conditions—underlying diseases, comorbidity, inflammatory states, and infections—increase patients’ energy expenditure, while reducing their normal intake (15–17). Therefore, during the later stages of hospitalization all patients should undergo an assessment of their nutritional status. The lack of an internationally accepted criterion for the diagnosis of malnutrition and the use of different indicators, some of which have been rejected by the most recent scientific evidence, probably explain a wide range of malnutrition prevalence rates reported in the literature. These rates vary from 20 to 60% in acute care among geriatric patients (18–20). In Italian hospitals, unfortunately, relatively little attention is given to nutritional issues, and neither nutritional screening, nor assessment, are routinely performed at hospital admission. Consequently, there are no reliable data on the nutritional status of in-hospital Italian patients, which is one of the oldest population worldwide. This manuscript presents the results of a retrospective analysis of data gathered during 1-day nutritional screening surveys. The surveys were performed for three consecutive years (2012–2014) in a geriatric research hospital—INRCA, Ancona–with the aim of assessing the prevalence of malnutrition risk among geriatric patients using the Malnutrition Universal Screening Tool (MUST). The data were also analyzed in light of the recently released consensus definition of malnutrition of the European Association for Clinical Nutrition and Metabolism (ESPEN) to assess the prevalence rate of malnutrition (21). To detect factors associated with malnutrition, the baseline characteristics of malnourished patients were confronted with those of patients without a malnutrition diagnosis. Multivariate analyses were performed to assess the impact of malnutrition on the length of hospital stay (LOS) and hospital mortality. The term malnutrition was exclusively used, synonymously, with undernutrition.
Materials and Methods
Settings and Sample
The Clinical Nutrition Unit, and the Medical Directorate, of the geriatric hospital INRCA-Ancona promoted a 1-day cross-sectional study among INRCA patients, for three consecutive years (2012–2014). After obtaining ethics committee approval, all newly admitted patients—i.e., patients admitted in the previous 48 h—were invited to participate in the study. Patients hospitalized in the emergency room and patients in post-acute care (long-term care and rehabilitation) were excluded. All patients gave their written informed consent for the collection and processing of their data for scientific purposes. Data on the outcomes of hospitalization were extrapolated from hospital archives.
Data Collection
A specific questionnaire was developed to collect demographic data (living arrangements, birth date, gender), data on patients’ clinical conditions (pathologies, disorders and comorbidities, immobilization, pressure ulcers, dysphagia, edentulism, history of weight loss, information on previous hospitalizations) and data on nutrition prescribed and administered during a hospitalization (diets and feeding routes). All questionnaires were filled out by trained staff (physicians, dieticians, and nurses) with the help of caregivers for non-collaborative patients. In addition, patients’ anthropometric data were gathered. Body weight was measured to the nearest 0.1 kg and height was determined to the nearest 0.1 cm, in subjects wearing light pajamas and without shoes. Height was measured with a height rod. Bedridden patients were weighed by bed scale and a special weighing set, complete with a digital scale and support spreader bar (Help 2000, Tassinari balance Srl). Bedridden patients’ heights were estimated from ulna length according to tables provided in the appendix of the MUST screening tool (22). The reduction of muscle mass was assessed from calf circumference, evaluated with a flexible tape measure at the proximal base of the inferior limb, under the knee, at the point of greatest diameter. On the same day, patient blood samples were collected by nurses and measurements of serum albumin (Alb) and serum prealbumin (Pab) were carried out in the hospital blood analysis laboratory. Patients’ body mass index (BMI) and Geriatric Nutrition Risk Index (GNRI), a tool to predict the risk of morbidity and mortality in hospitalized older patients, were determined based on collected data (23). Dysphagia screening, on admission, was performed by each ward with a bedside assessment technique. Data on the outcomes of hospitalization were gathered from hospital archives.
Malnutrition Screening
Malnutrition screening was performed with MUST. This tool allows the identification of patients with different levels of malnutrition risk (low, moderate, and high) and includes a management plan for nutritional intervention. The first step involves assigning a score to the patient’s BMI. The second step consists of setting up the patient’s unplanned Weight loss Score. During the third step, the acute disease effect score is assigned to each patient. The fourth step involves the estimate of malnutrition risk, which is calculated by the sum of single scores (0 = no risk, 1 = medium risk; score ≥ 2 = high risk). For each score, the management plan is provided within the fifth step. MUST is a validated and internationally accepted screening tool, which is easy to use and quick to perform. Its compilation requires from 3 to 5 min. It is particularly suited for hospital use both for its simplicity and because the effect of acute disease is considered.
Malnutrition Diagnosis
According to the recent consensus definition released by ESPEN, the diagnosis of malnutrition is a two-step process. After fulfilling the criteria for being at risk of malnutrition, by any validated risk screening tool, which is mandatory, those who are identified, proceed in the diagnostic process. The diagnosis may be performed in two optional ways. The first option requires a BMI < 18.5 kg/m2. The second option encompasses unintentional weight loss (UwL) (>10% independent of time or >5% in the last 3 months), always combined with either a low BMI (<20 kg/m2 if <70 years old or <22 kg/m2 if ≥70 years old) or a low Fat Free Mass index (FFMI; <15 kg/m2 for women and <17 kg/m2 for men). In this study, malnutrition was diagnosed for patients who were at high risk of malnutrition according to the MUST (score ≥ 2) if they fulfilled one of the following criteria: BMI < 18.5 kg/m2 and UwL > 10% undefined length of time or >5% over the last 3 months, combined with BMI < 22 kg/m2. Data on patients’ FFMI were not available. Sensitivity and specificity of MUST tool compared to ESPEN definition for diagnosis of malnutrition were calculated to detect the ability of the MUST tool to detect the malnutrition (sensitivity) and its ability not to give a positive result when patients are not malnourished. Positive and negative predictive values were calculated to assess how many of the subjects whose test is positive truly are malnourished and how many of the subjects whose test was negative actually were not malnourished.
Statistical Analyses
Descriptive statistics were used to describe patient characteristics. Continuous variables were expressed as mean values ± SD. Categorical variables were expressed as relative frequencies. Chi-square, odds ratio, and t-test were used to describe differences between malnourished and non-malnourished patients. Kolmogorov–Smirnov test was used to verify if the continuous variables included in the multivariate analyses had a normal distribution. The impact of malnutrition on LOS was investigated using the linear regression model with LOS (measured as number of days spent in the hospital) as the dependent variable and risk of malnutrition (according to the ESPEN definition) as the independent variable. The correlation between malnutrition and the outcome variable LOS was adjusted for gender, age, and comorbidities. The impact of malnutrition on the outcomes of hospitalization—hospital mortality—was investigated through the logistic regression model with the outcome of hospitalization (death or discharge from hospital) as the dependent variable and risk of malnutrition as independent variable. The correlation between the malnutrition and the outcome variable “in hospital mortality” was adjusted for different pathologies (diagnoses). Statistical significance of estimated coefficients was assessed through the t-test. The validity and overall reliability of the model was evaluated by the F-test and R-squared. The level of significance for all tests was set at p < 0.05. Data collected were analyzed with the Statistical Package for Social Sciences (SPSS) version 19.0.
Results
The analyses included 284 patients, of which 51.0% were females and 49.0% were males. The patients had a mean age of 82.8 ± 8.7; 50% of the subjects were ≥85 years, the so-called “the oldest old.” Following malnutrition risk screening, performed with MUST, 28.2% of patients had a high risk of malnutrition. For 88.3% of those patients at high risk, or 24.6% of the total population, malnutrition was diagnosed using the new ESPEN consensus definition (Table 1). We assessed that MUST has a sensitivity of 98%, specificity of 96%, positive predictive value of 89%, and negative predictive value of 99% compared to ESPEN definition.
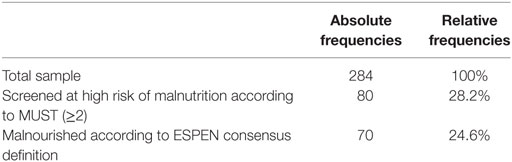
Table 1. Prevalence of high risk of malnutrition [Malnutrition Universal Screening Tool (MUST)] and of malnutrition (ESPEN consensus definition on malnutrition).
The relevance of nutritional problems was confirmed by the mode of feeding and the types of hospital diet registered on the study days. Almost 13% of patients were artificially fed (by Nasogastric tube, Percutaneous endoscopic gastrostomy and Venous catheter), mostly because of severe dysphagia. Texture-modified diets were prescribed for 24.4% of patients and pathology-specific diets were prescribed for 22.6%. More than 7% of patients were prescribed light, pre- and post-operative diets, or were fasting prior to medical tests and blood analyses. Only 33.0% of patients consumed a standard 2,000 kcal diet comprising 18% proteins, 28% fat, and 54% carbohydrates.
To identify factors associated with malnutrition, the baseline characteristics of malnourished and non-malnourished patients were compared (Table 2).
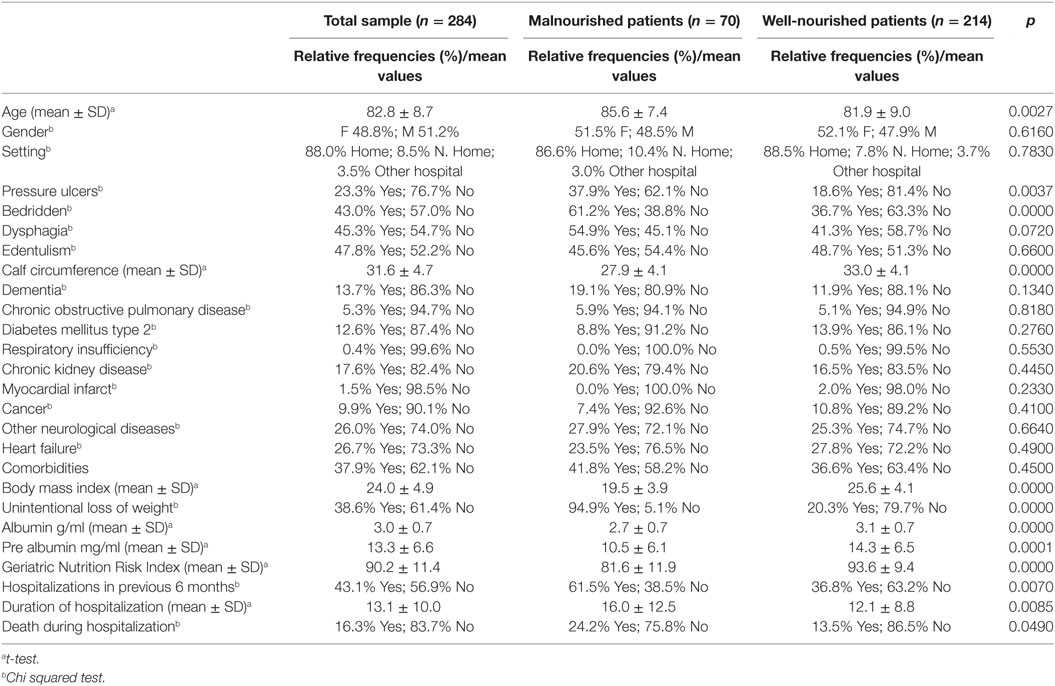
Table 2. Descriptive analysis of baseline sociodemographic, functional, and clinical parameters in the whole sample and in malnourished and non-malnourished patients—relative frequencies (%) and mean values (±SD).
Malnourished patients more frequently had symptoms of oropharingeal dysphagia, were older and bedridden, or were hospitalized in the previous 6 months. Statistically significant differences were also found between the two groups in the mean values of all the single indicators of nutritional status; GNRI, BMI, UwL, and between Alb and Pab values. The mean LOS for the sample population was 13.1 ± 10.0 days, while the overall hospital mortality rate was 16.3% with important differences in outcomes between the two groups of patients. To estimate the impact of the variable “malnutrition,” on the outcome variable “hospital mortality,” a multiple logistic regression analysis was performed (see Table 3). The results showed that the risk of dying during hospitalization was 55% higher for malnourished patients compared to non-malnourished subjects (p = 0.037; CI 0.21–0.95). The risk of hospital mortality was also strongly correlated with a cancer diagnosis; patients with cancer had a 68% higher probability of dying during hospitalization compared to other patients (p = 0.036; CI 0.11–0.93).
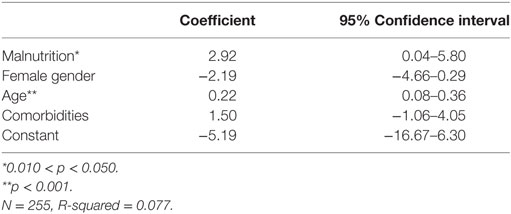
Table 3. Impact of malnutrition diagnosed using the ESPEN consensus definition on the outcomes of hospitalization.
The results of the linear regression analysis also showed that malnutrition was statistically significantly correlated with the LOS (Table 4). In fact, malnourished subjects, on average, spent almost 3 more days in the hospital compared with non-malnourished patients (p = 0.047; CI 0.04–5.80). Among control variables, only age was significantly correlated with the dependent variable; when age increased approximately 5 years, the LOS increased by 1 day. Gender and comorbidities were not significantly associated with the dependent variable (LOS).

Table 4. Impact of malnutrition diagnosed using ESPEN consensus definition on the length of hospital stay.
Discussion
Even though it has been repeatedly determined that protein-energy malnutrition can compromise clinical outcomes of hospitalized geriatric patients, screening and assessment of the nutritional status of this patient population is not routinely carried out in Italian hospitals (24, 25). Consequently, no reliable data on the prevalence of malnutrition among geriatric patients are available (26, 27). This important gap in knowledge stimulated the Clinical Nutrition Unit of the geriatric hospital, INRCA of Ancona, to carry out a 1-day nutritional screening survey, among newly admitted patients, for three subsequent years (2012–2014). The primary aim of the surveys was to collect reliable data on malnutrition risk at hospital admission. The MUST screening tool was used in each of the surveys (28, 29). Subsequently, a diagnosis of malnutrition was performed, for all patients at high risk, following the latest ESPEN consensus statement on the definition of malnutrition. The screening identified 28.2% of patients at high risk of malnutrition, of whom 88.3% suffered from malnutrition (24.6% of the total population). Unfortunately, the comparison of our results on malnutrition prevalence, with the results of other published studies, is very difficult due to the use of different screening and assessment tools and the specific populations analyzed. In some studies, significantly higher rates of malnutrition risk were found [Persson et al. (13), Thomas et al. (14)]. Other studies found rates that were quite similar to those reported in our investigation [Imoberdorf et al. (19), Sheen et al. (30)]. Our results showed a strong correlation between malnutrition and hospital mortality, with a 68% higher probability of malnourished patients dying during hospitalization. Previous evidence on this relation are contrasting. Numerous studies have identified malnutrition as an important predictive factor of in hospital mortality [Sullivan et al. (15), Caccialanza et al. (31), Gallagher-Allred et al. (32)], while other investigations find that the malnutrition upon hospitalizations is a predictive factor of mortality after hospital discharge [Lim et al. (7), Liu et al. (9), Personn et al. (13)]. According to our results, malnutrition at hospital admission also strongly influenced the LOS, which, on average, was 3 days longer for patients who were malnourished. This result coincides with the results of previous studies (Lim et al., Cederholm et al.) (7, 33). The present study provides also the first evidence of applying the novel ESPEN consensus definition of malnutrition in a population of hospitalized geriatric patients. The ESPEN approach was easily applicable. Only the measurement of FFM may represent some problem. It is so because, in some patients who are not collaborative and may have important physical impairments, it may be quite difficult to gather a reliable data. In addition, it has to be mentioned that BIA is not always available. The lack of data on FFM could result in the exclusion of an important portion of sarcopenic patients who have a normal BMI and no weight loss, but who have low FFM. According to the ESPEN consensus definition, any validated screening tool may be used to identify patients at risk of malnutrition. Different screening tools will vary in classifying patients according to malnutrition risk. The MUST tool, for example, defines three categories of risk. In this study, the second step of screening was performed only for patients at high risk of malnutrition (MUST score ≥ 2). Considering only the high risk group of patients, we found that MUST tool has an excellent sensitivity and specificity as well as positive and negative predictive values compared to ESPEN definition. It would be important to clarify, for each screening tool, the categories of patients for which a malnutrition diagnosis should be performed.
Some study limitations have to be mentioned. First, this is a retrospective study and, as it is known, retrospective studies have more potential sources of bias and confounding than the prospective ones. The investigation concentrated on malnutrition at hospital admission. But, it is well known that malnutrition frequently occurs during hospitalization, which may involve patients who are not at risk on admission. Considering that our study was performed in hospitalized patients, hospital-acquired malnutrition should have also been investigated. In addition, patients’ food intake should have been assessed. To overcome the latter limitation, hospital menus and patients’ food intake were investigated and confronted with their requirements during the last survey in 2014, but given the limited number of observations collected, the results of that analysis were not presented. This investigation was performed with relatively low number of participants; future studies on larger populations should be carried out to confirm our findings. No information on functional independence of patients were collected in our study but that information should be gathered in order to test how it influences the LOS and hospital mortality. Considering that the inflammation is also an important etiologic factor for malnutrition, data on inflammatory markers would also be useful and their correlation to LOS and hospital mortality should be tested. The readmission rates and post-discharge mortality (34) as well as the costs and benefits of nutritional interventions should also be evaluated in the future (35).
Ethics Statement
The study was approved by Ethics Commitee of INRCA IRCCS (Ancona). After the approval, patients were invited to participate in the study. All patients enrolled gave their informed consent for the collection and processing of data for scientific purposes.
Author Contributions
The corresponding author of this manuscript is PO. PO, SD, CV, and AC participated in the study design. All authors have directly participated in data collection during surveys. MR and NJP carried out statistical analyses. NJP discussed results of analyses with PO and CV. NJP wrote the final version of the manuscript. All authors gave important suggestions for the final version of the content of the article, read its final version and approved it.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Norman K, Pichard C, Lochs H, Pirlich M. Prognostic impact of disease-related malnutrition. Clin Nutr (2008) 27:5–15. doi:10.1016/j.clnu.2007.10.007
2. Derrick J. The Assessment of Nutritional Status of the Community. Geneva: World Health Organization (WHO) (1966).
3. Keller HH. Malnutrition in institutionalized elderly: how and why? J Am Geriatr Soc (1993) 41:1212–8. doi:10.1111/j.1532-5415.1993.tb07305.x
4. Hoffer LJ. Clinical nutrition: 1. Protein-energy malnutrition in the inpatient. CMAJ (2001) 165(10):1345–9.
5. Jeejeebhoy KN. Nutritional assessment. Nutrition (2000) 6(7–8):585–90. doi:10.1016/S0899-9007(00)00243-4
6. Correia MI, Waitzberg DL. The impact of malnutrition on morbidity, mortality, length of hospital stay and costs evaluated through a multivariate model analysis. Clin Nutr (2003) 22:235–9. doi:10.1016/S0261-5614(02)00215-7
7. Lim SL, Ong KCB, Chan YH, Loke WC, Ferguson M, Daniels L. Malnutrition and its impact on cost of hospitalization, length of stay, readmission and 3-year mortality. Clin Nutr (2012) 3:345–50. doi:10.1016/j.clnu.2011.11.001
8. Barker LA, Gout BS, Crowe TC. Review hospital malnutrition: prevalence, identification and impact on patients and the healthcare system. Int J Environ Res Public Health (2011) 2:514–27. doi:10.3390/ijerph8020514
9. Liu L, Bopp MM, Roberson PK, Sullivan DH. Undernutrition and risk of mortality in elderly patients within 1 year of hospital discharge. J Gerontol (2002) 57:741–6. doi:10.1093/gerona/57.11.M741
10. Nur Fazimah S, Sakinah H, Rosminah M. Hospitalized geriatric malnutrition: a perspective of prevalence, identification and implications to patient and healthcare cost. Health Environ J (2013) 4(1):55–67.
11. Neelemaat F, Meijers J, Kruizenga H, van Ballegooijen H, van Bokhorst-de van der Schueren M. Comparsion of five malnutrition screening tools in one hospital inpatient sample. J Clin Nurs (2011) 20:2144–51. doi:10.1111/j.1365-2702.2010.03667.x
12. Poulia KA, Yannakoulia M, Karageorgou D, Gamaletsou M, Panagiotakos DB, Sipsas NV, et al. Evaluation of the efficacy of six nutritional screening tools to predict malnutrition in the elderly. Clin Nutr (2012) 31:378–85. doi:10.1016/j.clnu.2011.11.017
13. Persson MD, Brismar KE, Katzarski KS, Nordenström J, Cederholm TE. Nutritional status using mini nutritional assessment and subjective global assessment predict mortality in geriatric patients. JAGS (2002) 50(12):1996–2002. doi:10.1046/j.1532-5415.2002.50611
14. Thomas DR, Zdrowski CD, Wilson MM, Conright KC, Lewis C, Tariq S, et al. Malnutrition in subacute care. Am J Clin Nutr (2002) 75:308–13.
15. Sullivan DH, Sun S, Walls RC. Protein-energy undernutrition among elderly hospitalized patients. A prospective study. JAMA (1999) 281(21):2013–9. doi:10.1001/jama.281.21.2013
16. Bokhorst-de van der Schueren MAE, Roosemalen MM, Weijs PJM, Langius JAE. High waste contributes to low food intake in hospitalized patients. Nutr Clin Pract (2012) 27(2):274–80. doi:10.1177/0884533611433602
17. Dupertuis YM, Kossovsky MP, Kyle UG, Raguso CA, Genton L, Pichard C. Food intake in 1707 hospitalised patients: a prospective comprehensive hospital survey. Clin Nutr (2003) 22(2):115–23. doi:10.1054/clnu.2002.0623
18. Agarwal E, Miller M, Yaxley A, Isenring E. Review malnutrition in the elderly: a narrative review. Maturitas (2013) 76:296–302. doi:10.1016/j.maturitas.2013.07.013
19. Imoberdorf R, Meier R, Krebs P, Hangartner PJ, Hess B, Staübli M, et al. Prevalence of undernutrition on admission to Swiss hospitals. Clin Nutr (2010) 1:38–41. doi:10.1016/j.clnu.2009.06.005
20. Kubrak C, Jensen L. Malnutrition in acute care patients: a narrative review. Int J Nurs Stud (2007) 44:1036–54. doi:10.1016/j.ijnurstu.2006.07.015
21. Guerra RS, Fonseca I, Sousa AS, Jesus A, Pichel F, Amaral TF. ESPEN diagnostic criteria for malnutrition A validation study in hospitalized patients. Clin Nutr (2016) 36(5):1326–32. doi:10.1016/j.clnu.2016.08.022
22. MAG Malnutrition Advisory Group A Standing Comittee of BAPEN. Malnutrition Universal Screening Tool. Redditch: BAPEN (2004).
23. Bouillanne O, Morineau G, Dupont C, Coulombel I, Vincent JP, Nicolis I, et al. Geriatric Nutritional Risk Index: a new index for evaluating at-risk elderly medical patients. Am J Clin Nutr (2005) 82:777–83.
24. Meijers JM, Schols JM, van Bokhorst-de van der Schueren MA, Dassen T, Janssen MA, Halfens RJ. Malnutrition prevalence in the Netherlands: results of the Annual Dutch National Prevalence Measurement of Care Problems. Br J Nutr (2009) 3:417–23. doi:10.1017/S0007114508998317
25. Vanderwee K, Clays E, Bocquaert I, Gobert M, Folens B, Defloor T. Malnutrition and associated factors in elderly hospital patients: a Belgian cross-sectional, multi-centre study. Clin Nutr (2010) 29:469–76. doi:10.1016/j.clnu.2009.12.013
26. Donini LM, Neri B, De Chiari S, Poggiogalle E, Muscaritoli M. Nutritional care in a nursing home in Italy. PLoS One (2013) 8(2):e55804. doi:10.1371/journal.pone.0055804
27. Lucchin L, D’Amicis A, Gentile MG, Battistini NC, Fusco MA, Palmo A, et al. A nationally representative survey of hospital malnutrition: the Italian PIMAI (Project: Iatrogenic MAlnutrition in Italy) study. Mediterr J Nutr Metab (2009) 2:171. doi:10.1007/s12349-009-0054-3
28. Stratton RJ, Hackston A, Longmore D, Dixon R, Price S, Stroud M, et al. Malnutrition in hospital outpatients and inpatients: prevalence, concurrent validity and ease of use of the “Malnutrition Universal Screening Tool” (“MUST”) for adults. Br J Nutr (2004) 92:799–808. doi:10.1079/BJN20041258
29. Kondrup J, Allison SP, Elia M, Vellas B, Plauth M, Educational and Clinical Practice Committee. ESPEN Guidelines for Nutrition Screening 2002. Clin Nutr (2003) 22(4):415–21. doi:10.1016/S0261-5614(03)00098-0
30. Sheen PM, Peterson SJ, Chen Y, Liu D, Lateef O, Braunschweig CA. Utilizing multiple methods to classify malnutrition among elderly patients admitted to the medical and surgical intensive care units (ICU). Clin Nutr (2013) 32:752–7. doi:10.1016/j.clnu.2012.12.012
31. Caccialanza R, Cereda M, Klersy C. Letter: malnutrition, age and in hospital mortality. CMAJ (2011) 183(7):826. doi:10.1503/cmaj.111-2038
32. Gallagher-Allred CR, Voss AC, Finn SC, McCamish MA. Malnutrition and clinical outcomes: the case for medical nutrition therapy. J Am Diet Assoc (1996) 96(4):361–6.
33. Cederholm T, Jägrén C, Hellström K. Outcome of protein-energy malnutrition in elderly medical patients. Am J Med (1995) 98(1):67–74. doi:10.1016/S0002-9343(99)80082-5
34. Sriram K, Sulo S, VanDerBosch G, Partridge J, Feldstein J, Hegazi RA, et al. A comprehensive nutrition-focused quality improvement program reduces 30-day readmissions and length of stay in hospitalized patients. J Parenter Enteral Nutr (2016) 20:384–91. doi:10.1177/0148607116681468
Keywords: geriatrics, in-hospital patients, nutritional screening, malnutrition, hospitalization outcomes
Citation: Orlandoni P, Venturini C, Jukic Peladic N, Costantini A, Di Rosa M, Cola C, Giorgini N, Basile R, Fagnani D, Sparvoli D and David S (2017) Malnutrition upon Hospital Admission in Geriatric Patients: Why Assess It? Front. Nutr. 4:50. doi: 10.3389/fnut.2017.00050
Received: 26 September 2016; Accepted: 05 October 2017;
Published: 30 October 2017
Edited by:
Maurizio Muscaritoli, Sapienza Università di Roma, ItalyReviewed by:
Stéphane Michel Schneider, University of Nice Sophia Antipolis, FranceMarcello Maggio, University of Parma, Italy
Copyright: © 2017 Orlandoni, Venturini, Jukic Peladic, Costantini, Di Rosa, Cola, Giorgini, Basile, Fagnani, Sparvoli and David. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Paolo Orlandoni, p.orlandoni@inrca.it
 Paolo Orlandoni
Paolo Orlandoni Claudia Venturini
Claudia Venturini Nikolina Jukic Peladic
Nikolina Jukic Peladic Annarita Costantini
Annarita Costantini
 Mirko Di Rosa
Mirko Di Rosa Claudia Cola
Claudia Cola Natascia Giorgini
Natascia Giorgini Debora Sparvoli
Debora Sparvoli