- 1Department of Biophysics, GSI Helmholtzzentrum für Schwerionenforschung, Darmstadt, Germany
- 2Department of Physics, Trento Institute for Fundamental Physics and Applications (TIFPA), National Institute for Nuclear Physics (INFN), University of Trento, Trento, Italy
- 3Research Center Hospital for Charged Particle Therapy, National Institute of Radiological Sciences (NIRS), Chiba, Japan
Pancreatic ductal adenocarcinoma is the only cancer for which deaths are predicted to increase in 2014 and beyond. Combined radiochemotherapy protocols using gemcitabine and hypofractionated X-rays are ongoing in several clinical trials. Recent results indicate that charged particle therapy substantially increases local control of resectable and unresectable pancreas cancer, as predicted from previous radiobiology studies considering the high tumor hypoxia. Combination with chemotherapy improves the overall survival (OS). We compared published data on X-ray and charged particle clinical results with or without adjuvant chemotherapy calculating the biological effective dose. We show that chemoradiotherapy with protons or carbon ions results in 1 year OS significantly higher than those obtained with other treatment schedules. Further hypofractionation using charged particles may result in improved local control and survival. A comparative clinical trial using the standard X-ray scheme vs. the best current standard with carbon ions is crucial and may open new opportunities for this deadly disease.
Introduction
Pancreatic cancer (PC), usually ductal adenocarcinoma, is the fourth cause of cancer-related death in USA (1) and the only cancer for which deaths are predicted to increase in Europe for both men and women in 2015 (2). Even after surgery, the mortality from PC is very high. Radiotherapy is used for radical treatment in locally advanced unresectable tumors (LAUPC), generally in combination with chemotherapy, or prior to surgery for potentially resectable malignancies. However, prognosis remains very poor, with <5% of patients surviving for 5 years after diagnosis (3). This makes PC a priority for finding better ways to control it and better treatments. Early tumors usually do not cause symptoms, so that the disease is typically not diagnosed until it has spread beyond the pancreas itself, either with distal metastasis or with infiltration in the neuroplexus. This is one of the reasons for the poor survival rate. Moreover, PC is very hypoxic (4), which makes it radioresistant and promotes epithelial–mesenchymal transition; is resistant to apoptosis; and presents a dense tumor stroma, which acts as a barrier against immune cells, preventing immune suppression (5).
Radiobiology studies suggest that charged particle therapy (CPT) using protons or carbon ions is more effective for treatment of PC than X-rays. In fact, accelerated ions have a reduced oxygen enhancement ratio (OER), and are therefore exquisitely effective against hypoxic tumors (6). Moreover, high doses of densely ionizing radiation elicit a strong immune response, which can be exploited to destroy not only the primary tumor but also distal metastasis (7). Carbon ion radiotherapy (CIRT) is currently performed in only two centers in Europe (HIT in Germany and CNAO in Italy) and none in USA (where many centers use protons only for CPT), but much more experience has been accumulated in Asia, especially at the National Institute for Radiological Sciences (NIRS) in Chiba, Japan. A recent external review of 20 years of CIRT at NIRS highlighted treatment of PC as the most promising application of CIRT, with results clearly superior to any other treatment modalities, especially for LAUPC (8).
Based on these very promising preliminary Japanese results, the US National Cancer Institute (NCI), in his efforts to promote CIRT in USA, issued a solicitation for a prospective randomized phase-III trial comparing CIRT to X-ray therapy for LAUPC in combination with chemotherapy, having survival as main endpoint1. This trial may provide the first evidence of a superiority of CIRT in a common and deadly cancer. Planning of the trial is complicated by the many different variables – not only radiation quality but also chemotherapy regime, fractionation, and treatment plan. Here, we review all the current results in treatment of LAUPC and use a mathematical model to describe the dependence on survival on the biological effective dose (BED) with X-rays and CPT in combination with chemotherapy.
Materials and Methods
Data Collection
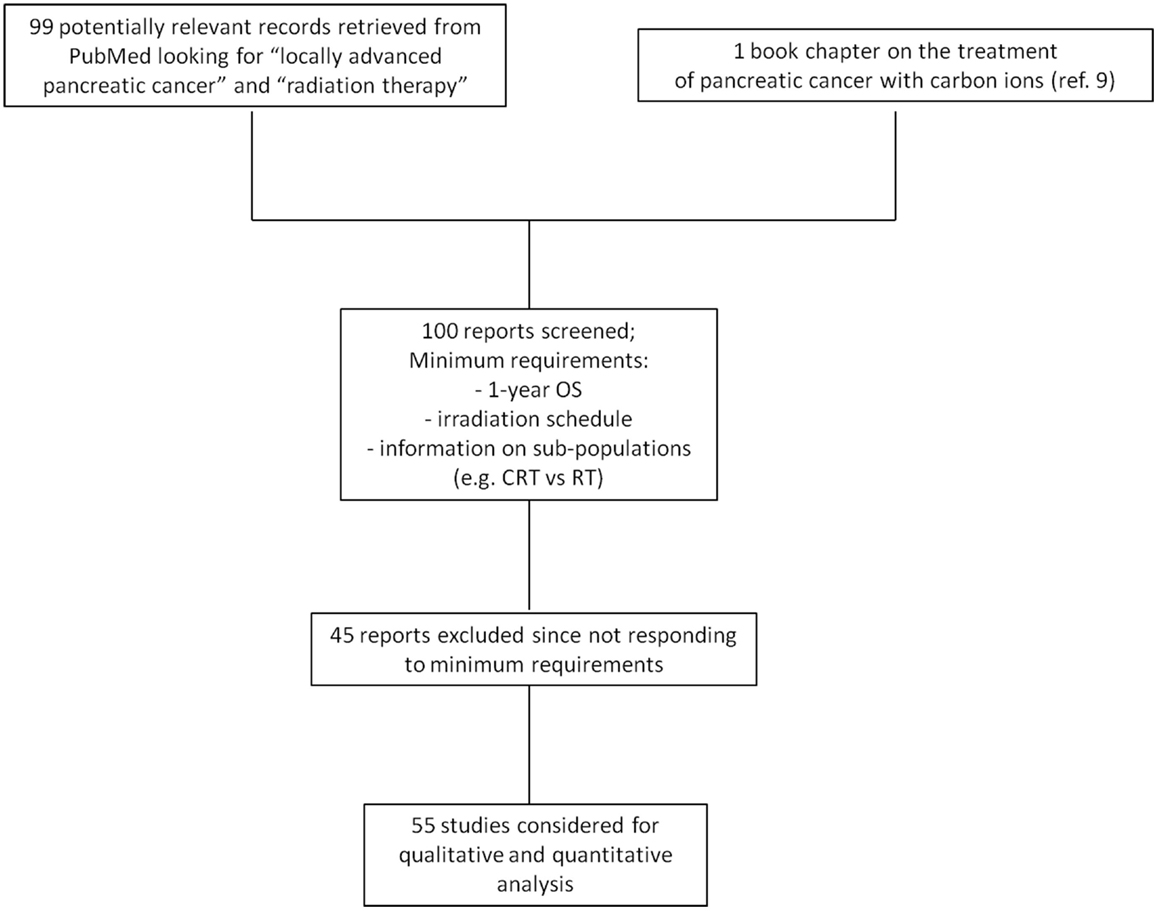
We searched the literature for all data available on radiotherapy, chemotherapy, and combined treatments. The research criteria and outcomes are summarized in the diagram shown in Figure 1. The patient populations generally consist of adults with adenocarcinoma histology, locally advanced tumor presentation, and generally tumors not in direct contact to duodenum and stomach. Radiotherapy included conformal radiotherapy (3DCRT), intensity-modulated radiation therapy (IMRT), stereotactic body radiotherapy (SBRT), protontherapy, and CIRT. Data from CIRT are limited to the NIRS experience and include data as yet only published in the institute annual report and in a recent book (9). Adjuvant, neo-adjuvant, or concomitant chemotherapies were all included in the search, using different drugs. Our data collection was compared with a recent meta-analysis of radiochemotherapy in LAUPC (10), and has been updated on April 2015.
Modeling
To compare the largely variable fractionation and chemotherapy schedules reported in the literature, we used the common quantity of BED (11), which has been extended to chemotherapy to quantify the effect of the drug in terms of radiation-equivalent dose (12). Because many published papers have short follow-up, and not all endpoints are reported, we concentrated on the 1-year overall survival (OS). We assumed that the overall 1-year survival probability OS is a combination of the survival probability following the radiation (RS) and chemotherapy (CS) treatment, i.e.,
Equation 1 implies a purely additive effect of chemotherapy and radiotherapy in the treatment of LAUPC. The dose–response for the OS probability can be expressed with the same functions used for the tumor control probability: Poisson, logistic, or probit models (13). We elected to use the logistic function, which is based on the linear-quadratic model, following the recent model of chemoradiation treatment in bladder cancer (14). Thus, we wrote:
where γ50 is the normalized dose-response gradient and D50 the BED corresponding to a survival in a radiotherapy only treatment of 50% at 1 year.
Combining Eqs 1 and 2, we finally obtain
In a recent analysis of chemoradiation therapy in LAUPC, Moraru et al. (15) used a radiosensitization factor in the BED formula and fitted the LAUPC 1 year OS data with a modified linear-quadratic formula. In general, it is very hard to distinguish additive from synergistic model in chemoradiation data (16). In vitro experiments can provide some information, but do not necessarily reflect the complex in vivo microenvironment. Some chemotherapy drugs used for LAUPC treatment apparently sensitize cell cultures to X-rays (17, 18), but simple additive effects are observed when the drugs are given in vitro concomitantly to charged particles (19, 20). Moreover, in many clinical protocols, chemotherapy is given as adjuvant or neo-adjuvant, and even when concomitant is often continued after the radiotherapy cycle. We therefore assumed, in our analysis, that the simple additive model of Eqs 1 and 3.
The BED was calculated using the Fowler formula (11):
with:
– n: number of fractions
– d: dose/fraction
– T: overall treatment time
– α = 0.393 Gy−1, β = 0.058 Gy−2, α/β = 6.77 Gy (21)
– Td: tumor doubling time, fixed to 42 days (15).
The dose/fraction d was given in Gy for X-ray data, and Gy(RBE) (or GyE) for CPT. For protontherapy, 1 Gy(RBE) = 1.1 Gy (22). In CIRT, Gy(RBE) was calculated according to the NIRS model (23), whose results can be different, depending on the dose and target size, from those that would be obtained using the LEM model (24), implemented in the European CIRT facilities.
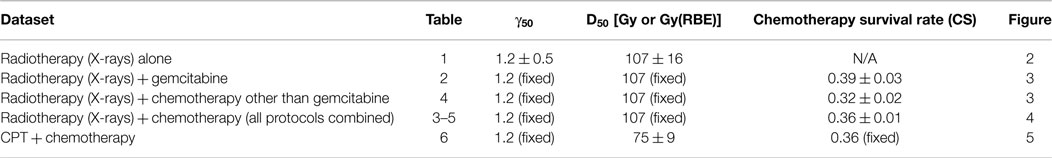
Fitting
Clinical data extracted from the published papers were weighted with a vertical error bar, given by the SD of the OS using Poisson statistics:
where ns and ntot indicate the number of surviving patients at 1 year and the total number of patients included in the study, respectively. When possible, a horizontal error bar was also included, corresponding to the range of the doses used. A first weighed fit of the radiotherapy-alone data was performed using Eq. 2 to estimate the two parameters γ50 and D50. The chemoradiation data were then fitted using Eq. 3 having CS as only fitting parameter: γ50 and D50 were indeed taken from the radiotherapy fit. Many different chemotherapy drugs were used in old and new studies. Gemcitabine is one of the most successful and currently adopted, also in the CIRT trials. We have therefore divided the data into gemcitabine only, other drugs, and gemcitabine plus other drugs. Overall, no statistically significant differences were noted among the three groups. We have therefore fitted the data together, even if we plotted the points in different colors. Finally, for fitting the CPT data, we expressed the BED in Gy(RBE) as described above, and used Eq. 3 with a fixed CS and γ50 taken from the fit of the chemoradiation data with X-rays. In fact, we assume that CPT has an impact on the D50 due to the putative improved dose distribution in the target and to the radiobiological properties beyond the calculated RBE used in the Gy(RBE).
Results
Single Treatment Data
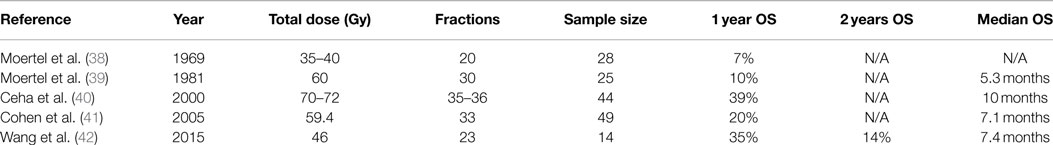
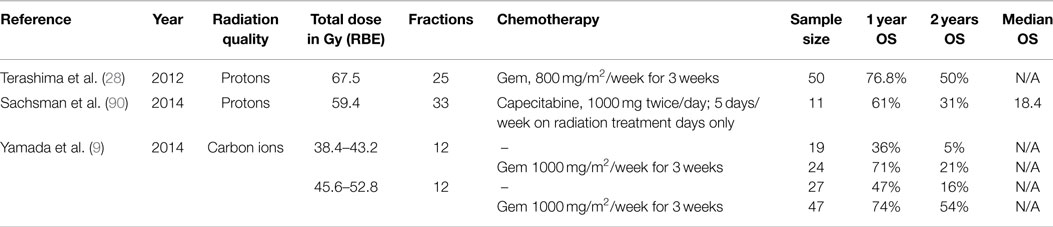
Chemoradiation is generally considered the best standard of cure for LAUPC. For this reason, only a few studies are available with radiotherapy alone, and some of them are old (Table 1). Some recent studies using SBRT have been excluded. An initial trial in Stanford using high-dose (25 Gy) single-fraction reports a 100% survival at 1 year, but this was limited to six patients (25). Later results from Stanford using SBRT are included in Table 2. On the other hand, a Danish study using 45 Gy in three fractions gave very low OS and high toxicity (26). This study was also excluded in our analysis, because these poor outcomes were likely a result of inaccurate positioning, lack of effective motion management techniques, and lack of dose constraints for OARs (27).
The data are plotted in Figure 2, along with the fit using Eq. 2. Fitting parameters are reported in Table 2. The D50 = 107 Gy clearly shows how impractical is the treatment of LAUPC with X-rays alone. For comparison, Dale et al. (16) estimated a BED at 50% complete response for bladder cancer of 54.4 Gy. From the analysis of the trials using chemotherapy alone (10), an average 1-year survival below 20% can be estimated.
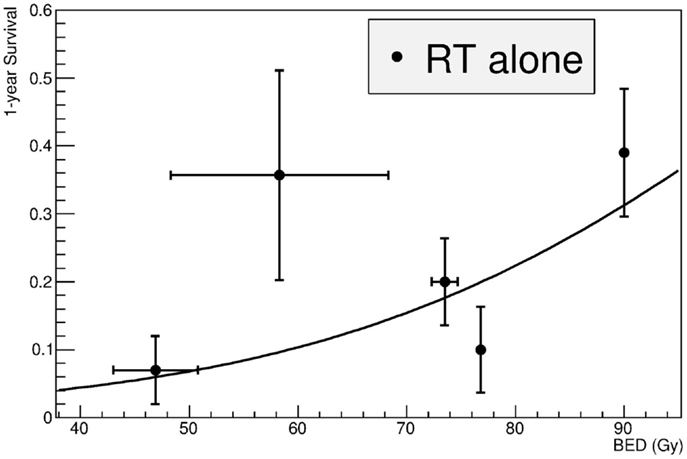
Figure 2. Fit of the clinical data for treatment of LAUPC with X-ray radiotherapy alone. Studies are listed in Table 1. BED is calculated by Eq. 4. Fitting was performed by Eq. 2 and fitting parameters are in Table 3.
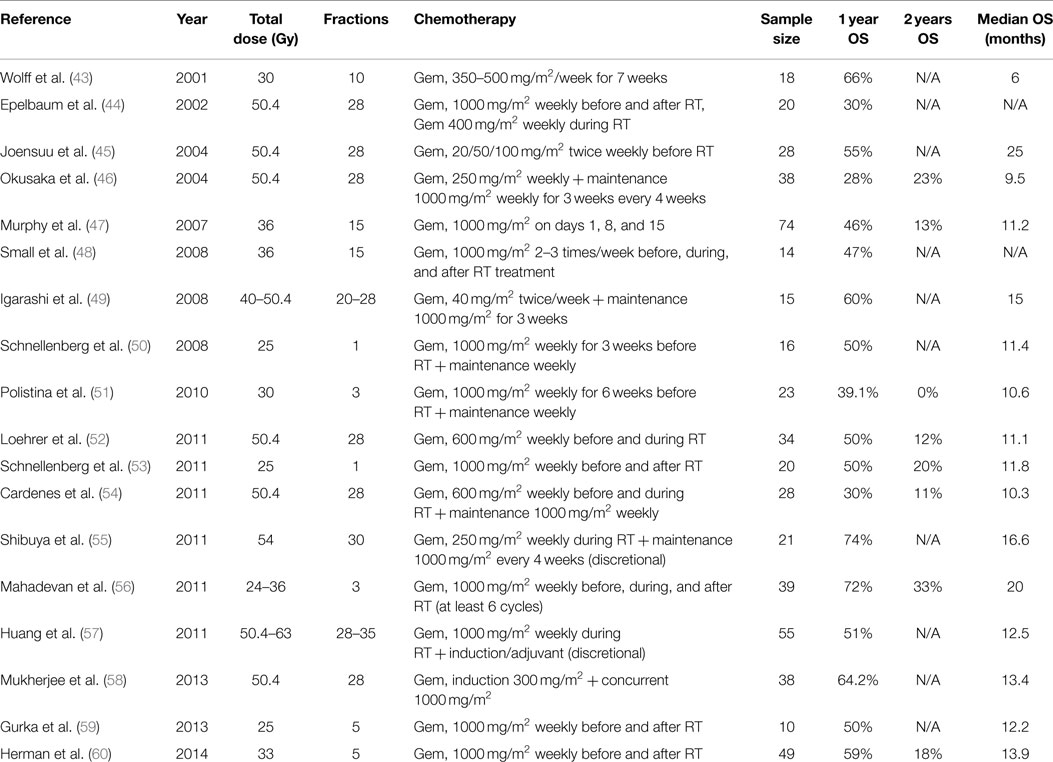
Chemoradiation
Meta-analysis of the clinical data has already shown an advantage in chemoradiation compared to radiotherapy or chemotherapy alone (10). Most clinical trials for LAUPC resort to chemoradiation protocols. Gemcitabine (Table 3) is often regarded as the standard treatment. Several other drugs, such as capecitabine, fluorouracil (5-FU), cisplatin, docetaxel, cetuximab, and fluoropyrimidine prodrug S-1, have been used in the past or in new trials (Table 4), and often combination of gemcitabine and any of the other drugs (Table 5) are applied. The standard X-ray course is 50.4 Gy in 1.8 Gy/fraction, giving a BED of 63 Gy. We did not find significant differences in the groups treated with different drugs, considering the very high scatter of the data also due to the completely different protocols adopted. Figure 3 shows, for example, a comparison of the data in Tables 3 and 4, pointing only to a slight trend for better results in protocols using gemcitabine compared to other drugs. Figure 4 shows the fit of all the data compared to X-rays alone. Having fixed the γ50 and D50 parameters, we estimated the only parameter CS = 0.36 ± 0.01 (Table 2). The radiation dose corresponding to this survival probability RS = CS can be estimated by Eq. 2 as
leading to a chemo-equivalent dose of 94 Gy. This high value underlines the large improvement that chemotherapy gives on the survival of LAUPC patients. Dale and co-workers (16) estimated 43.6 Gy for the BED chemo-equivalent in bladder cancer. They also demonstrated that the chemo-equivalent dose is not a constant and will be of course much lower if we calculate it for a higher survival level.
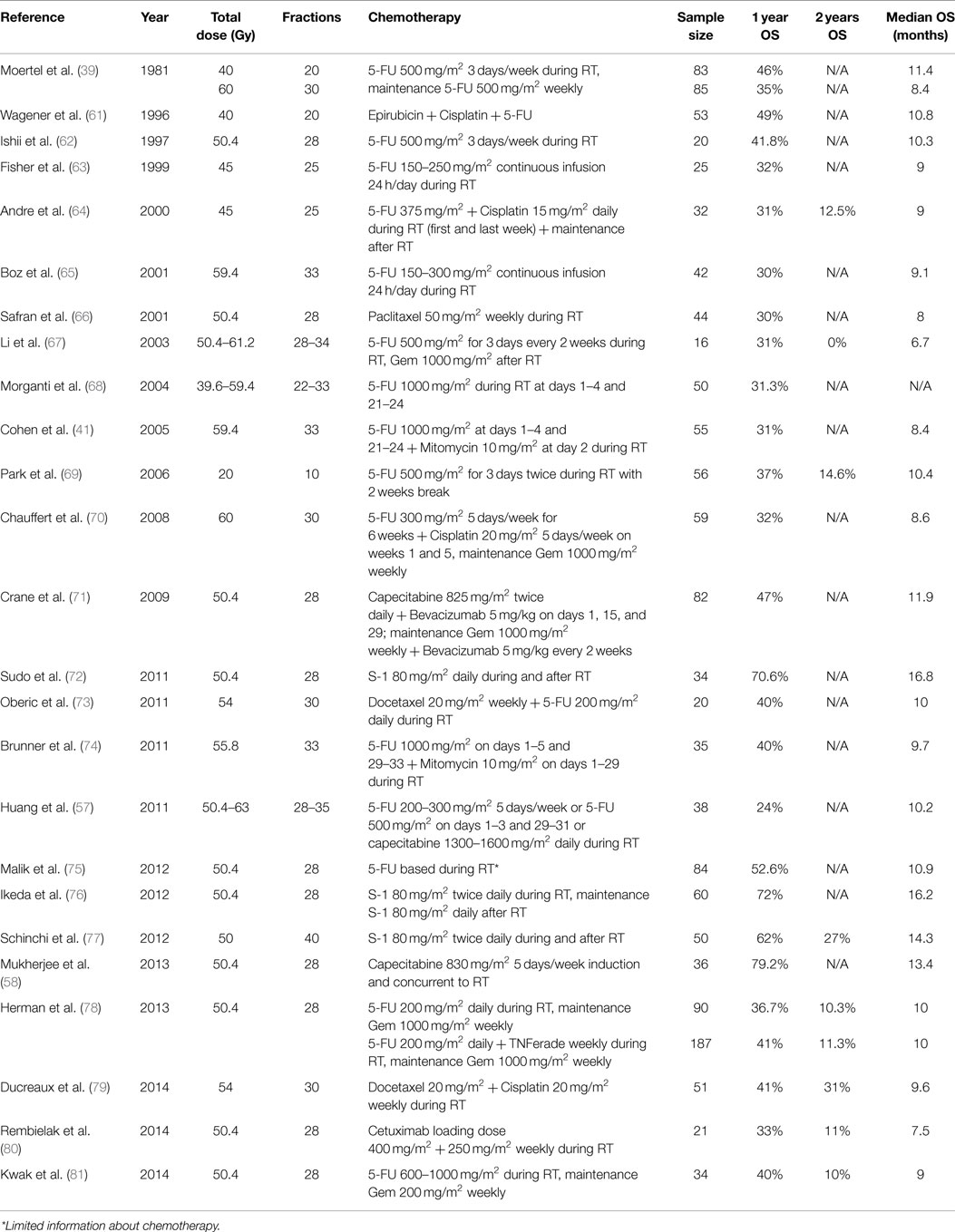
Table 4. Clinical data for treatment of LAUPC using X-ray therapy plus chemotherapy, excluding the trials with gemcitabine.
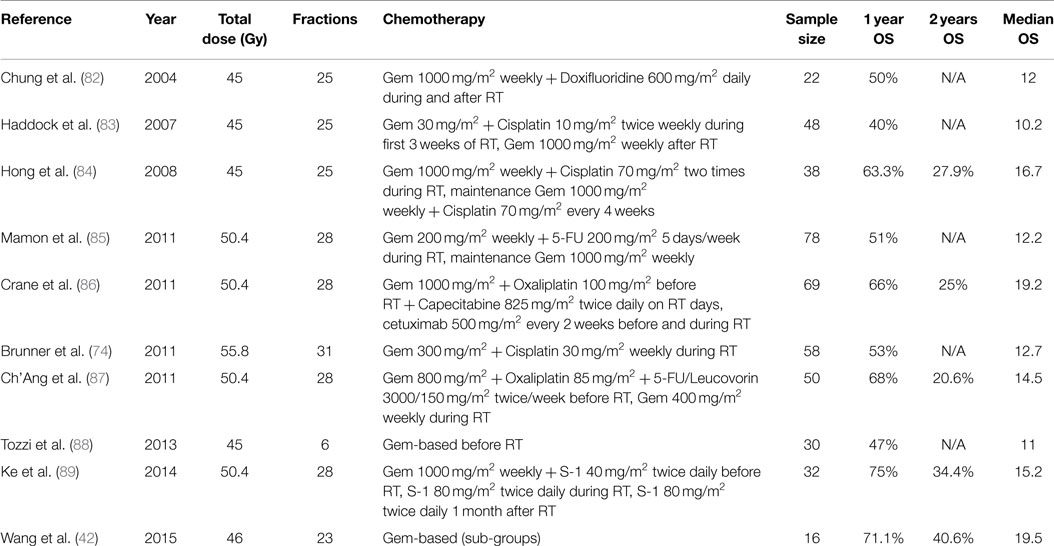
Table 5. Clinical data for treatment of LAUPC using X-ray therapy plus a chemotherapy cocktail including gemcitabine.
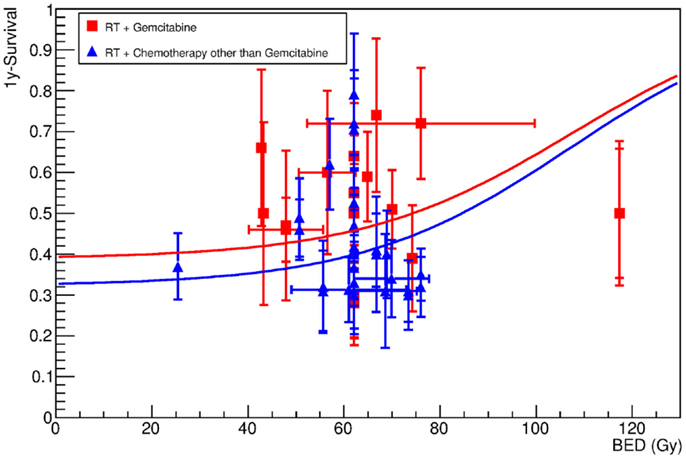
Figure 3. One-year survival as a function of the BED for patients undergoing X-ray radiotherapy plus gemcitabine (red symbols), or other chemotherapy drugs (blue symbols). Data are reported in Tables 2 and 4. The lines show the result of the fit (Eq. 3), which was performed assuming that γ50 and D50 are obtained by fitting the data in treatments using radiotherapy only (Figure 1). The only free fitting parameter is the chemotherapy survival CS (see Table 3). The results suggest that the final outcome does not strongly depend on the specific chemotherapy treatment, although some advantage seems to be associated to the use of gemcitabine.
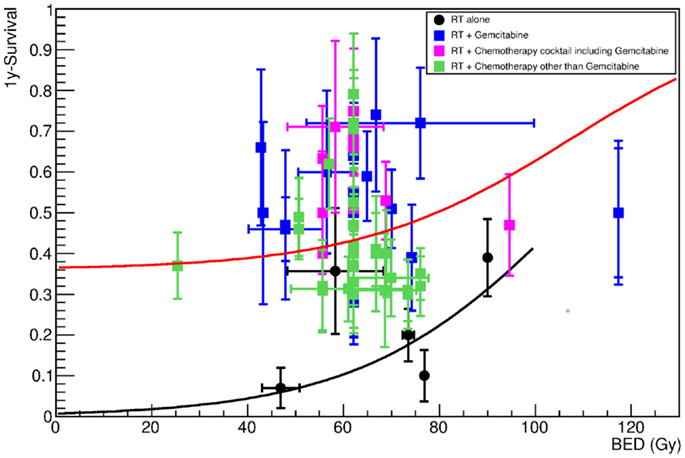
Figure 4. One-year survival as a function of the BED for patients undergoing X-ray radiotherapy alone (black symbols), or in combination with any chemotherapy treatments. Details about chemotherapy regimen are reported in Tables 4–6. The lines show the result of the fit (black for radiotherapy-alone data, red for all chemotherapy data pooled together), which was performed assuming that γ50 and D50 are obtained by fitting RT-alone data. Fitting parameters with Eq. 3 are in Table 3.
Charged Particle Therapy
Although only a few studies are available with CPT, the data in Table 6 show that they are the best current options for LAUPC. A 2-year survival rate around 50% was reached with protons (28) or C-ions (9) in combination with gemcitabine, a value far exceeding any other chemoradiation trial using X-rays and any cocktail of drugs. The data with CIRT alone (no chemotherapy) are clearly superior to those with X-rays alone and comparable to the results with chemoradiation at the same X-rays BED. The best 1-year OSs for combined chemotherapy (gemcitabine) and CPT are those from Hyogo (28) using protons up to 70.2 Gy(RBE) in 26 fractions, but they came at a cost of grade 3–5 toxicity in 10% of the patients, especially gastric ulcer and hemorrhage. CIRT toxicity was much more mild, with 17% of the patients experiencing grade 3 GI toxicity, in the form of appetite loss. Low toxicity was observed for the duodenum, both for protons and 12C-ions. The fit of the chemoradiation with CPT, using the same CS and γ50 parameters calculated for X-rays + chemotherapy, is shown in Figure 5. This fit assumes that CPT does not change the effect of the chemotherapy compared to X-rays, but results in a lower D50 due to biological and/or physical improvements compared to X-rays. Should these improvements be already included in the RBE model used to calculate the equivalent dose in Gy(RBE), we should see the same effect at the same BED [see Ref. (23) for CIRT in Japan; RBE = 1.1 for protons]. Instead, the best fit is reduced to D50 = 75 ± 9 Gy(RBE) for CPT (Table 2). This 50% improvement is caused either by a better physics, enabling treatment of infiltrations in the neuroplexus, or to a better biology, especially to a reduced OER (6) or to a stronger immune response (7) using CPT compared to X-rays.
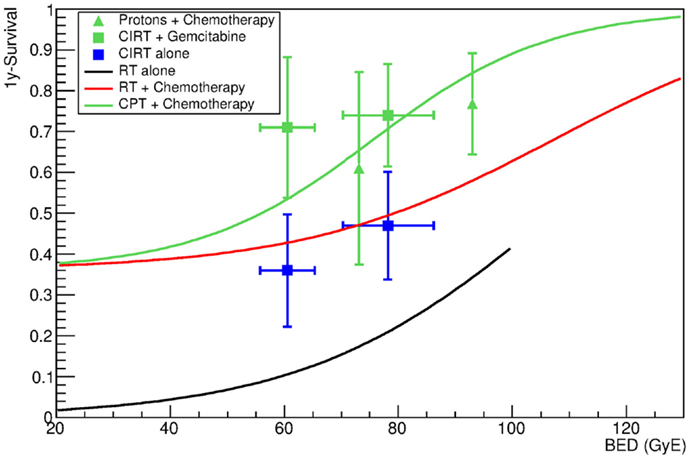
Figure 5. One-year survival as a function of the BED for patients undergoing CPT with or without additional chemotherapy. Blue symbols refer to patients receiving radiotherapy with C-ions without additional chemotherapy. Green symbols refer to data obtained with proton (triangles) and carbon ions (full squares) in combination with chemotherapy. Data are given in Table 6. The green line shows the result of the fit of data for chemotherapy combined with proton or carbon ions. The fit was performed using γ50 and CS from X-ray + chemotherapy data. The only free parameter is therefore D50. The black and red lines show the results of the fit for X-rays alone and X-rays plus chemotherapy, and are reported for comparison. Fitting parameters are in Table 3.
Discussion
The large interest for the use of CPT in LAUPC comes from the exceptional clinical results (8), supported by our clinical data analysis in Figure 5. These results reflect the biological rationale of reduced OER for high-LET radiation and possible dose escalation with limited side effects exploiting the Bragg peak. The high GI toxicity observed in the Hyogo trial (28) seems to set a threshold at a BED around 100 Gy(RBE). The question is whether the same threshold applies to CIRT, where the sharper dose edges of the treatment plan may reduce the exposure of the critical organs compared to protons, whose lateral scattering is much higher than for heavy ions (6). An example of a treatment plan of a pancreatic head cancer with carbon ions is shown in Figure 6. It is possible to give a high-dose against tumor and neuroplexus with acceptable doses to stomach or duodenum. The dose distribution can further improve using raster scanning instead of passive modulation, as shown in Figure 7. The new NIRS facility is now equipped with raster scanning, and so are the HIT and CNAO facilities now treating the first LAUPC patients with C-ions. Under these optimal conditions, it appears feasible to exceed a BED of 100 Gy(RBE) with acceptable toxicities.
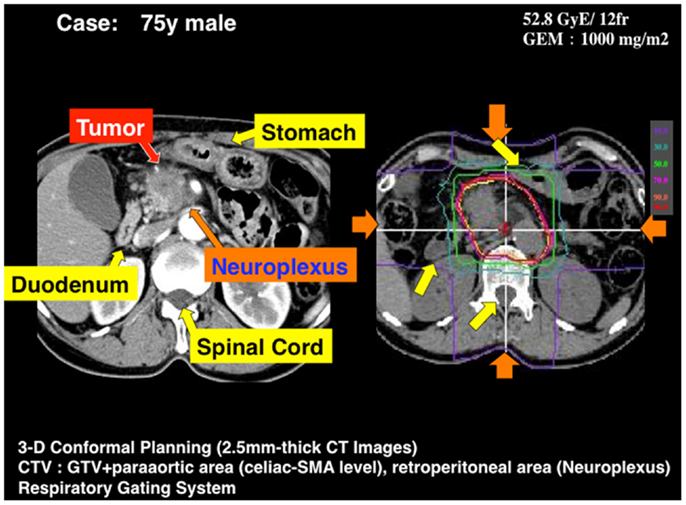
Figure 6. A typical treatment plan used at NIRS for a locally advanced pancreatic head cancer. The beam is shaped with passive modulation and four opposite fields are applied with respiratory gating. GTV includes the primary tumor and lymph nodes involved. CTV = PTV + neuroplexus infiltration (periarterial area) + proximal lymph nodes. PTV = CTV + 5 mm, excluding GI tract.
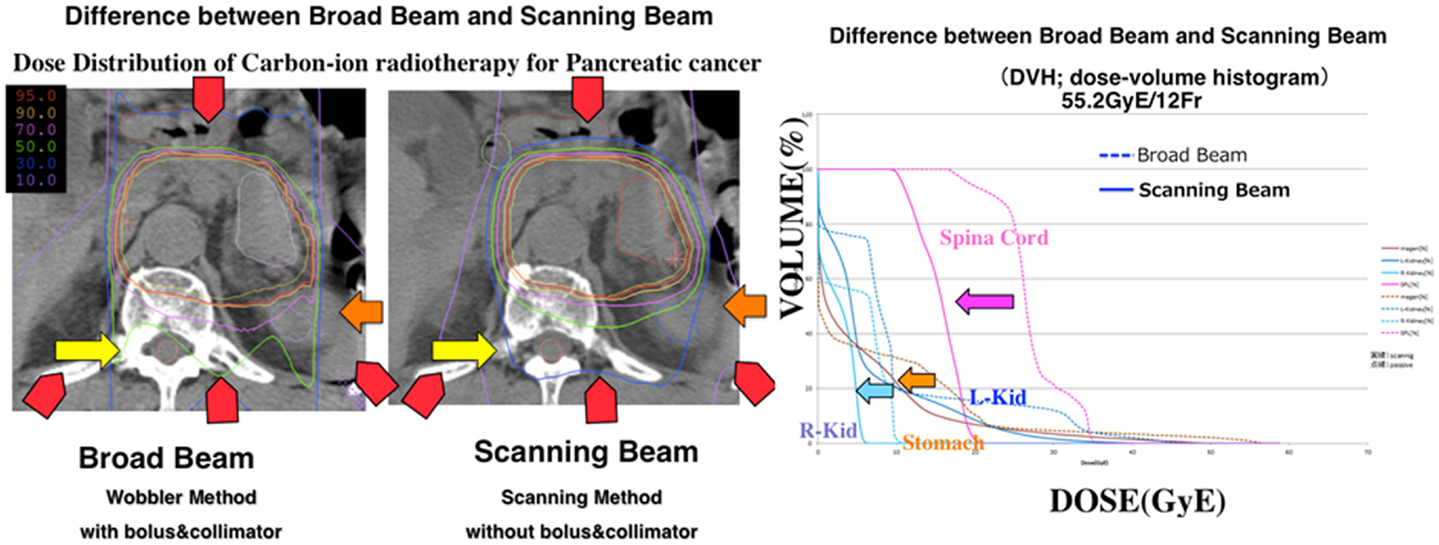
Figure 7. Comparison of the current passive beam modulation treatment plan with a spot scanning treatment plan for LAUPC. In the right panel, the dose–volume histogram for different organs is shown for passive modulation (dotted line) and raster scanning (solid line). Dose to the spinal cord and kidney are highly reduced. Potential reduction is also clear for stomach and duodenum, whose movements are, however, critical.
Modeling chemotherapy in terms of equivalent radiation dose is an effective method to predict outcomes of dose-escalation trials (12, 16). The large scatter in the chemoradiation data leads, however, to a poor goodness-of-fit in Figures 3 and 4. This is due in part to the many different protocols used in chemotherapy for LAUPC, and to inclusion of data published in over 30 years using very different methods both for drug and radiation delivery. In this paper, we have decided to analyze all the data available in the literature, without including the treatment year as a function in the model. We have also assumed no synergistic interaction between chemicals and radiation. Finally, Eq. 4 should be modified for protons or carbon ions, where α/β is higher than for X-rays leading to a lower dependence on fractionation. Due to the lack of sufficient information leading to an educated guess for other parameters and models, we decided to stick to the conventional logistic function, replacing Gy with Gy(RBE) in Table 6. The basic assumption remains that a higher BED will result in a higher OS in LAUPC patients, an assumption clearly supported by the analysis of the several trials included in our data mining. Our analysis supports the concept that a dose escalation will improve OS, and toxicity is the limiting factor. In Table 7, we have calculated with the logistic model (Eq. 3) the expected survival in hypofractionated dose-escalation trials and compared with the standard chemoradiation treatment and other schedules proposed for SBRT using X-rays (15, 27). The standard at NIRS is 12 fractions in 3 weeks, and with the current maximum dose/fraction the OS at 1 year is expected to improve from 40 to 70% compared to the standard X-ray regime (50.4 Gy in 28 fractions). Reaching 18 fractions with the same dose/fraction, it could be possible to double the survival. Further hypofractionation, down to a single dose of 25 Gy(RBE) is very attractive in terms of expected survival, but raises concerns for the GI toxicity. C-ions delivered by raster scanning should provide the optimal dose distributions (Figure 7) compared to CIRT with passive scattering and protons, where the lateral scattering unavoidably leads to a dose penumbra around the PTV. However, for beam scanning, the issue of motion mitigation must be tackled very carefully, because of the known problem of the interplay. Currently, NIRS is using respiratory gating to compensate especially the movements of stomach and duodenum in the PTV (Figure 8). A treatment with high number of fractions compensates the interplay between beam scanning and organ motion, but this compensation is lost in radiosurgery (29). In the treatment of hepatocellular carcinoma with 12C-ions at the HIT facility in Heidelberg, it has been shown that the simple increase from 1 to 4 fractions substantially improved the dose target coverage and reduced overdosage (V107 from 32 to 4%) (30), this means that keeping the hypofractionation schemes above 4 fractions, major inhomogeneities should be avoided. Nevertheless, the range uncertainties due to bowel movement, stomach peristalsis, and breathing, have to be solved to reduce toxicity to the many critical organs surrounding the pancreas. Motion mitigation strategy include respiratory gating or layer stacking boost irradiation, such as used at NIRS for treating PC (31), and 4D optimization of the plan based on 4DCT (32). Patients with tumors in a favorable location, preferably >1 cm from the closest luminal organ, should be selected for the dose escalation.
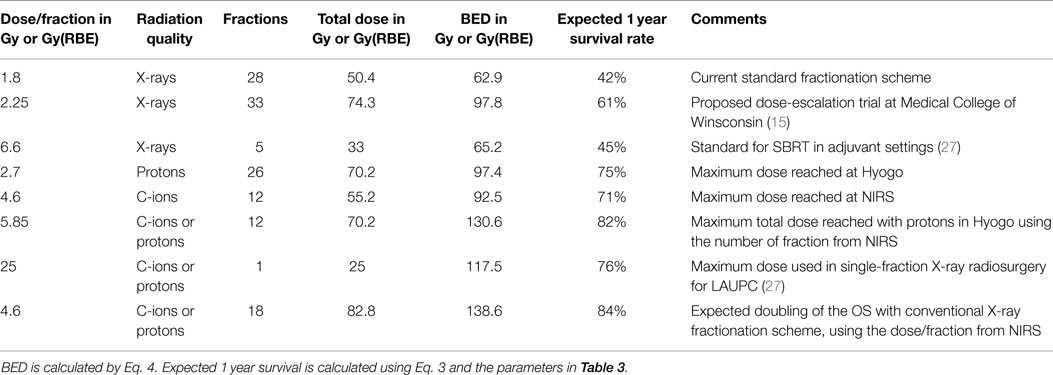
Table 7. Expected improvement in survival according to our model in chemoradiation trials using CPT.
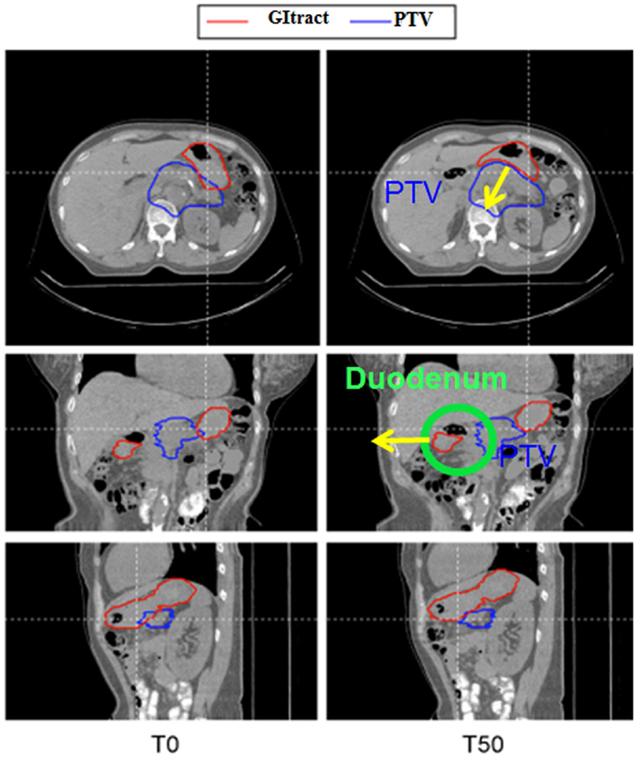
Figure 8. 4DCT analysis of the movement of the critical organs during treatment of LAUPC at NIRS with C-ions. T0 is the peak inhalation and T50 the peak exhalation phases. Stomach and duodenum move in and out the PTV in the two phases.
The solution of this problem is an important step to push toward higher doses and fewer fractions thus leading to a substantial improvement in survival can be expected using chemoradiation protocols with CPT rather than X-rays. The first clinical CIRT vs. IMRT trial for LAUPC should compare the standard chemoradiation treatment (Table 7, row 1), with the NIRS most advanced protocol (Table 7, row 5). The additional advantage of using the standard protocols is that at the dose/fraction of 4.6 Gy(RBE) reached in the escalation trial at NIRS, there is practically no difference between the biological dose calculated at NIRS and those predicted by LEM (24) and implemented in European CIRT facilities. However, in a multi-centric trial, it will be unavoidable to have different systems for dose delivery, motion management, patient selection, etc. For instance, NIRS is using passive modulation, CNAO raster scanning, and HIT can use the gantry. Nevertheless, a comparative trial for LAUPC is absolutely necessary to support the use of CIRT and to confirm the very promising data in the phase I–II trials at NIRS (8). The lack of comparative, phase-III clinical trials is generally considered as a major hindrance to a more widespread use of CPT in the clinics (33). A trial on LAUPC may definitely clarify the clinical advantage of CPT in such a lethal tumor.
Apart from the international comparative trial, further developments of phase-II trials with CPT should point to two directions. First, several molecular markers, such as mutations in SMAD4/DPC4, have been validated as prognostic factors in PCs (34). Whole-genome sequencing and copy number variation analysis suggest that PCs can be divided into four genetic subtypes, with potential clinical utility (35). Trials with CPT combined with molecular analysis of these genes are highly needed, because CPT may elicit different molecular pathways than conventional X-rays (36). Combined CIRT + gemcitabine may be especially effective against pancreatic stem-like cells, as suggested by a recent in vitro study (37), and hence, study of stem cells markers and genetic pathways will be highly desirable. In addition, further hypofractionation is desirable if the problems of the organ movements are tackled as described above. For instance, the use of 12 fractions (such as done at NIRS) with the total dose used for protons in Hyogo is expected to push the 1-year survival over 80% (Table 7, row 6). A careful motion mitigation strategy should be rapidly implemented to allow this further escalation.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The work was partly supported by the Portfolio Technologie und Medizin, Helmholtz Gemeinschaft and INFN-TIFPA (Trento).
Footnote
- ^Solicitation number BAA-N01CM51007-51 (April 17, 2015) available online through FedBizOpps at http://www.fbo.gov
References
1. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin (2015) 65:5–29. doi:10.3322/caac.21254
2. Malvezzi M, Bertuccio P, Rosso T, Rota M, Levi F, La Vecchia C, et al. European cancer mortality predictions for the year 2015: does lung cancer have the highest death rate in EU women? Ann Oncol (2015) 26:779–86. doi:10.1093/annonc/mdv001
3. Wolfgang CL, Herman JM, Laheru DA, Klein AP, Erdek MA, Fishman EK, et al. Recent progress in pancreatic cancer. CA Cancer J Clin (2013) 63:318–48. doi:10.3322/caac.21190
4. Koong AC, Mehta VK, Le QT, Fisher GA, Terris DJ, Brown JM, et al. Pancreatic tumors show high levels of hypoxia. Int J Radiat Oncol Biol Phys (2000) 48:919–22. doi:10.1016/S0360-3016(00)00803-8
5. Olive KP, Jacobetz MA, Davidson CJ, Gopinathan A, McIntyre D, Honess D, et al. Inhibition of Hedgehog signaling enhances delivery of chemotherapy in a mouse model of pancreatic cancer. Science (2009) 324:1457–61. doi:10.1126/science.1171362
6. Loeffler JS, Durante M. Charged particle therapy – optimization, challenges and future directions. Nat Rev Clin Oncol (2013) 10:411–24. doi:10.1038/nrclinonc.2013.79
7. Durante M, Reppingen N, Held KD. Immunologically augmented cancer treatment using modern radiotherapy. Trends Mol Med (2013) 19:565–82. doi:10.1016/j.molmed.2013.05.007
8. Kamada T, Tsujii H, Blakely EA, Debus J, De Neve W, Durante M, et al. Carbon ion radiotherapy in Japan: an assessment of 20 years of clinical experience. Lancet Oncol (2015) 16:e93–100. doi:10.1016/S1470-2045(14)70412-7
9. Yamada S, Terashima K, Shinoto M, Yasuda S, Shiomi M, Isozaki T. Pancreatic cancer. In: Tsujii H, Kamada T, Shirai K, Noda K, Tsuji H, Karasawa K, editors. Carbon Ion Radiotherapy. Berlin: Springer-Verlag (2014). p. 221–8.
10. Chen Y, Sun X-J, Jiang T-H, Mao A-W. Combined radiochemotherapy in patients with locally advanced pancreatic cancer: a meta-analysis. World J Gastroenterol (2013) 19:7461–71. doi:10.3748/wjg.v19.i42.7461
11. Fowler JF. 21 years of biologically effective dose. Br J Radiol (2010) 83:554–68. doi:10.1259/bjr/31372149
12. Jones B, Dale RG. The potential for mathematical modelling in the assessment of the radiation dose equivalent of cytotoxic chemotherapy given concomitantly with radiotherapy. Br J Radiol (2005) 78:939–43. doi:10.1259/bjr/40226390
13. Bentzen SM, Tucker SL. Quantifying the position and steepness of radiation dose-response curves. Int J Radiat Biol (1997) 71:531–42. doi:10.1080/095530097143860
14. Plataniotis G, Dale RG. Radio-chemotherapy for bladder cancer: contribution of chemotherapy on local control. World J Radiol (2013) 5:267–74. doi:10.4329/wjr.v5.i8.267
15. Moraru IC, Tai A, Erickson B, Li XA. Radiation dose responses for chemoradiation therapy of pancreatic cancer: an analysis of compiled clinical data using biophysical models. Pract Radiat Oncol (2014) 4:13–9. doi:10.1016/j.prro.2013.01.005
16. Plataniotis G, Dale RG. Assessment of the radiation-equivalent of chemotherapy contributions in 1-phase radio-chemotherapy treatment of muscle-invasive bladder cancer. Int J Radiat Oncol Biol Phys (2014) 88:927–32. doi:10.1016/j.ijrobp.2013.11.242
17. Pauwels B, Vermorken JB, Wouters A, Ides J, Van Laere S, Lambrechts HAJ, et al. The role of apoptotic cell death in the radiosensitising effect of gemcitabine. Br J Cancer (2009) 101:628–36. doi:10.1038/sj.bjc.6605145
18. Wouters A, Pauwels B, Burrows N, Baay M, Deschoolmeester V, Vu TN, et al. The radiosensitising effect of gemcitabine and its main metabolite dFdU under low oxygen conditions is in vitro not dependent on functional HIF-1 protein. BMC Cancer (2014) 14:594. doi:10.1186/1471-2407-14-594
19. El Shafie RA, Habermehl D, Rieken S, Mairani A, Orschiedt L, Brons S, et al. In vitro evaluation of photon and raster-scanned carbon ion radiotherapy in combination with gemcitabine in pancreatic cancer cell lines. J Radiat Res (2013) 54:i113–9. doi:10.1093/jrr/rrt052
20. Schlaich F, Brons S, Haberer T, Debus J, Combs SE, Weber K-J. Comparison of the effects of photon versus carbon ion irradiation when combined with chemotherapy in vitro. Radiat Oncol (2013) 8:260. doi:10.1186/1748-717X-8-260
21. Chapman JD. Can the two mechanisms of tumor cell killing by radiation be exploited for therapeutic gain? J Radiat Res (2014) 55:2–9. doi:10.1093/jrr/rrt111
22. Tommasino F, Durante M. Proton radiobiology. Cancers (Basel) (2015) 7:353–81. doi:10.3390/cancers7010353
23. Kanai T, Matsufuji N, Miyamoto T, Mizoe J, Kamada T, Tsuji H, et al. Examination of GyE system for HIMAC carbon therapy. Int J Radiat Oncol Biol Phys (2006) 64:650–6. doi:10.1016/j.ijrobp.2005.09.043
24. Steinsträter O, Grün R, Scholz U, Friedrich T, Durante M, Scholz M. Mapping of RBE-weighted doses between HIMAC- and LEM-based treatment planning systems for carbon ion therapy. Int J Radiat Oncol Biol Phys (2012) 84:854–60. doi:10.1016/j.ijrobp.2012.01.038
25. Koong AC, Le QT, Ho A, Fong B, Fisher G, Cho C, et al. Phase I study of stereotactic radiosurgery in patients with locally advanced pancreatic cancer. Int J Radiat Oncol Biol Phys (2004) 58:1017–21. doi:10.1016/j.ijrobp.2003.11.004
26. Hoyer M, Roed H, Sengelov L, Traberg A, Ohlhuis L, Pedersen J, et al. Phase-II study on stereotactic radiotherapy of locally advanced pancreatic carcinoma. Radiother Oncol (2005) 76:48–53. doi:10.1016/j.radonc.2004.12.022
27. Moningi S, Marciscano AE, Rosati LM, Ng SK, Teboh Forbang R, Jackson J, et al. Stereotactic body radiation therapy in pancreatic cancer: the new frontier. Expert Rev Anticancer Ther (2014) 14:1461–75. doi:10.1586/14737140.2014.952286
28. Terashima K, Demizu Y, Hashimoto N, Jin D, Mima M, Fujii O, et al. A phase I/II study of gemcitabine-concurrent proton radiotherapy for locally advanced pancreatic cancer without distant metastasis. Radiother Oncol (2012) 103:25–31. doi:10.1016/j.radonc.2011.12.029
29. Bert C, Durante M. Particle radiosurgery: a new frontier of physics in medicine. Phys Med (2014) 30:535–8. doi:10.1016/j.ejmp.2014.04.011
30. Richter D, Saito N, Chaudhri N, Härtig M, Ellerbrock M, Jäkel O, et al. Four-dimensional patient dose reconstruction for scanned ion beam therapy of moving liver tumors. Int J Radiat Oncol Biol Phys (2014) 89:175–81. doi:10.1016/j.ijrobp.2014.01.043
31. Mori S, Shinoto M, Yamada S. Four-dimensional treatment planning in layer-stacking boost irradiation for carbon-ion pancreatic therapy. Radiother Oncol (2014) 111:258–63. doi:10.1016/j.radonc.2014.02.014
32. Graeff C. Motion mitigation in scanned ion beam therapy through 4D-optimization. Phys Med (2014) 30:570–7. doi:10.1016/j.ejmp.2014.03.011
33. Mitin T, Zietman AL. Promise and pitfalls of heavy-particle therapy. J Clin Oncol (2014) 32:2855–63. doi:10.1200/JCO.2014.55.1945
34. Vincent A, Herman J, Schulick R, Hruban RH, Goggins M. Pancreatic cancer. Lancet (2011) 378:607–20. doi:10.1016/S0140-6736(10)62307-0
35. Waddell N, Pajic M, Patch AM, Chang DK, Kassahn KS, Bailey P, et al. Whole genomes redefine the mutational landscape of pancreatic cancer. Nature (2015) 518:495–501. doi:10.1038/nature14169
36. Durante M. New challenges in high-energy particle radiobiology. Br J Radiol (2014) 87:20130626. doi:10.1259/bjr.20130626
37. Sai S, Wakai T, Vares G, Yamada S, Kamijo K, Kamada T, et al. Combination of carbon ion beam and gemcitabine causes irreparable DNA damage and death of radioresistant pancreatic cancer stem-like cells in vitro and in vivo. Oncotarget (2015) 6:5517–35.
38. Moertel CG, Childs DS, Reitemeier RJ, Colby MY, Holbrook MA. Combined 5-fluorouracil and supervoltage radiation therapy of locally unresectable gastrointestinal cancer. Lancet (1969) 2(7626):865–7. doi:10.1016/S0140-6736(69)92326-5
39. Moertel CG, Frytak S, Hahn RG, O’Connell MJ, Reitemeier RJ, Rubin J, et al. Therapy of locally unresectable pancreatic carcinoma: a randomized comparison of high dose (6000 rads) radiation alone, moderate dose radiation (4000 rads + 5-fluorouracil), and high dose radiation + 5-fluorouracil. The Gastrointestinal Tumor Study Group. Cancer (1981) 48:1705–10. doi:10.1002/1097-0142(19811015)48:8<1705::AID-CNCR2820480803>3.0.CO;2-4
40. Ceha HM, van Tienhoven G, Gouma DJ, Veenhof CH, Schneider CJ, Rauws EA, et al. Feasibility and efficacy of high dose conformal radiotherapy for patients with locally advanced pancreatic carcinoma. Cancer (2000) 89:2222–9. doi:10.1002/1097-0142(20001201)89:11<2222::AID-CNCR10>3.0.CO;2-V
41. Cohen SJ, Dobelbower R, Lipsitz S, Catalano PJ, Sischy B, Smith TJ, et al. A randomized phase III study of radiotherapy alone or with 5-fluorouracil and mitomycin-C in patients with locally advanced adenocarcinoma of the pancreas: Eastern Cooperative Oncology Group Study E8282. Int J Radiat Oncol Biol Phys (2005) 62:1345–50. doi:10.1016/j.ijrobp.2004.12.074
42. Wang Z, Ren Z-G, Ma N-Y, Zhao J-D, Zhang Z, Ma X-J, et al. Intensity modulated radiotherapy for locally advanced and metastatic pancreatic cancer: a mono-institutional retrospective analysis. Radiat Oncol (2015) 10:4–11. doi:10.1186/s13014-014-0312-5
43. Wolff RA, Evans DB, Gravel DM, Lenzi R, Pisters PW, Lee JE, et al. Phase I trial of gemcitabine combined with radiation for the treatment of locally advanced pancreatic adenocarcinoma. Clin Cancer Res (2001) 7:2246–53.
44. Epelbaum R, Rosenblatt E, Nasrallah S, Faraggi D, Gaitini D, Mizrahi S, et al. Phase II study of gemcitabine combined with radiation therapy in patients with localized, unresectable pancreatic cancer. J Surg Oncol (2002) 81:138–43. doi:10.1002/jso.10159
45. Joensuu TK, Kiviluoto T, Kärkkäinen P, Vento P, Kivisaari L, Tenhunen M, et al. Phase I-II trial of twice-weekly gemcitabine and concomitant irradiation in patients undergoing pancreaticoduodenectomy with extended lymphadenectomy for locally advanced pancreatic cancer. Int J Radiat Oncol Biol Phys (2004) 60:444–52. doi:10.1016/j.ijrobp.2004.03.026
46. Okusaka T, Ito Y, Ueno H, Ikeda M, Takezako Y, Morizane C, et al. Phase II study of radiotherapy combined with gemcitabine for locally advanced pancreatic cancer. Br J Cancer (2004) 91:673–7. doi:10.1038/sj.bjc.6602001
47. Murphy JD, Adusumilli S, Griffith KA, Ray ME, Zalupski MM, Lawrence TS, et al. Full-dose gemcitabine and concurrent radiotherapy for unresectable pancreatic cancer. Int J Radiat Oncol Biol Phys (2007) 68:801–8. doi:10.1016/j.ijrobp.2006.12.053
48. Small W, Berlin J, Freedman GM, Lawrence T, Talamonti MS, Mulcahy MF, et al. Full-dose gemcitabine with concurrent radiation therapy in patients with nonmetastatic pancreatic cancer: a multicenter phase II trial. J Clin Oncol (2008) 26:942–7. doi:10.1200/JCO.2007.13.9014
49. Igarashi H, Ito T, Kawabe K, Hisano T, Arita Y, Kaku T, et al. Chemoradiotherapy with twice-weekly administration of low-dose gemcitabine for locally advanced pancreatic cancer. World J Gastroenterol (2008) 14:5311–5. doi:10.3748/wjg.14.5311
50. Schellenberg D, Goodman KA, Lee F, Chang S, Kuo T, Ford JM, et al. Gemcitabine chemotherapy and single-fraction stereotactic body radiotherapy for locally advanced pancreatic cancer. Int J Radiat Oncol Biol Phys (2008) 72:678–86. doi:10.1016/j.ijrobp.2008.01.051
51. Polistina F, Costantin G, Casamassima F, Francescon P, Guglielmi R, Panizzoni G, et al. Unresectable locally advanced pancreatic cancer: a multimodal treatment using neoadjuvant chemoradiotherapy (gemcitabine plus stereotactic radiosurgery) and subsequent surgical exploration. Ann Surg Oncol (2010) 17:2092–101. doi:10.1245/s10434-010-1019-y
52. Loehrer PJ, Feng Y, Cardenes H, Wagner L, Brell JM, Cella D, et al. Gemcitabine alone versus gemcitabine plus radiotherapy in patients with locally advanced pancreatic cancer: an Eastern Cooperative Oncology Group trial. J Clin Oncol (2011) 29:4105–12. doi:10.1200/JCO.2011.34.8904
53. Schellenberg D, Kim J, Christman-Skieller C, Chun CL, Columbo LA, Ford JM, et al. Single-fraction stereotactic body radiation therapy and sequential gemcitabine for the treatment of locally advanced pancreatic cancer. Int J Radiat Oncol Biol Phys (2011) 81:181–8. doi:10.1016/j.ijrobp.2010.05.006
54. Cardenes HR, Moore AM, Johnson CS, Yu M, Helft P, Chiorean EG, et al. A Phase II Study of Gemcitabine in combination with radiation therapy in patients with localized, unresectable, pancreatic cancer. Am J Clin Oncol (2011) 34:460–5. doi:10.1097/COC.0b013e3181e9c103
55. Shibuya K, Oya N, Fujii T, Doi R, Nakamura A, Matsuo Y, et al. Phase II study of radiation therapy combined with weekly low-dose gemcitabine for locally advanced, unresectable pancreatic cancer. Am J Clin Oncol (2011) 34:115–9. doi:10.1097/COC.0b013e3181c4c7a8
56. Mahadevan A, Miksad R, Goldstein M, Sullivan R, Bullock A, Buchbinder E, et al. Induction gemcitabine and stereotactic body radiotherapy for locally advanced nonmetastatic pancreas cancer. Int J Radiat Oncol Biol Phys (2011) 81:615–22. doi:10.1016/j.ijrobp.2011.04.045
57. Huang J, Robertson JM, Margolis J, Balaraman S, Gustafson G, Khilanani P, et al. Long-term results of full-dose gemcitabine with radiation therapy compared to 5-fluorouracil with radiation therapy for locally advanced pancreas cancer. Radiother Oncol (2011) 99:114–9. doi:10.1016/j.radonc.2011.05.038
58. Mukherjee S, Hurt CN, Bridgewater J, Falk S, Cummins S, Wasan H, et al. Gemcitabine-based or capecitabine-based chemoradiotherapy for locally advanced pancreatic cancer (SCALOP): a multicentre, randomised, phase 2 trial. Lancet Oncol (2013) 14:317–26. doi:10.1016/S1470-2045(13)70021-4
59. Gurka MK, Collins SP, Slack R, Tse G, Charabaty A, Ley L, et al. Stereotactic body radiation therapy with concurrent full-dose gemcitabine for locally advanced pancreatic cancer: a pilot trial demonstrating safety. Radiat Oncol (2013) 8:44. doi:10.1186/1748-717X-8-44
60. Herman JM, Chang DT, Goodman KA, Dholakia AS, Raman SP, Hacker-Prietz A, et al. Phase 2 multi-institutional trial evaluating gemcitabine and stereotactic body radiotherapy for patients with locally advanced unresectable pancreatic adenocarcinoma. Cancer (2015) 121:1128–37. doi:10.1002/cncr.29161
61. Wagener DJT, Hoogenraad WJ, Rougier P, Lusinchi A, Taal BG, Veenhof CHN, et al. Results of a phase II trial of epirubicin and cisplatin (EP) before and after irradiation and 5-fluorouracil in locally advanced pancreatic cancer: an EORTC GITCCG study. Eur J Cancer (1996) 32:1310–3. doi:10.1016/0959-8049(96)00070-6
62. Ishii H, Okada S, Tokuuye K, Nose H, Okusaka T, Yoshimori M, et al. Protracted 5-fluorouracil infusion with concurrent radiotherapy as a treatment for locally advanced pancreatic carcinoma. Cancer (1997) 79:1516–20. doi:10.1002/(SICI)1097-0142(19970415)79:8<1516::AID-CNCR11>3.3.CO;2-5
63. Fisher BJ, Perera FE, Kocha W, Tomiak A, Taylor M, Vincent M, et al. Analysis of the clinical benefit of 5-fluorouracil and radiation treatment in locally advanced pancreatic cancer. Int J Radiat Oncol Biol Phys (1999) 45:291–5. doi:10.1016/S0360-3016(99)00197-2
64. André T, Balosso J, Louvet C, Hannoun L, Houry S, Huguier M, et al. Combined radiotherapy and chemotherapy (cisplatin and 5-fluorouracil) as palliative treatment for localized unresectable or adjuvant treatment for resected pancreatic adenocarcinoma: results of a feasibility study. Int J Radiat Oncol Biol Phys (2000) 46:903–11. doi:10.1016/S0360-3016(99)00478-2
65. Boz G, De Paoli A, Innocente R, Rossi C, Tosolini G, Pederzoli P, et al. Proceedings of the 25th National Congress of the Italian Association of Pancreatology Study (AISP). Cernobbio, Como (Italy). September 20-22, 2001. JOP (2001) 2(5 Suppl):330–54.
66. Safran H, Moore T, Iannitti D, Dipetrillo T, Akerman P, Cioffi W, et al. Paclitaxel and concurrent radiation for locally advanced pancreatic cancer. Int J Radiat Oncol Biol Phys (2001) 49:1275–9. doi:10.1016/S0360-3016(00)01527-3
67. Li C-P, Chao Y, Chi K-H, Chan W-K, Teng H-C, Lee R-C, et al. Concurrent chemoradiotherapy treatment of locally advanced pancreatic cancer: gemcitabine versus 5-fluorouracil, a randomized controlled study. Int J Radiat Oncol Biol Phys (2003) 57:98–104. doi:10.1016/S0360-3016(03)00435-8
68. Morganti AG, Valentini V, Macchia G, Mattiucci GC, Costamagna G, Deodato F, et al. 5-fluorouracil-based chemoradiation in unresectable pancreatic carcinoma: phase I-II dose-escalation study. Int J Radiat Oncol Biol Phys (2004) 59:1454–60. doi:10.1016/j.ijrobp.2004.01.035
69. Park JK, Ryu JK, Lee JK, Yoon WJ, Lee SH, Kim YT, et al. Gemcitabine chemotherapy versus 5-fluorouracil-based concurrent chemoradiotherapy in locally advanced unresectable pancreatic cancer. Pancreas (2006) 33:397–402. doi:10.1097/01.mpa.0000236725.26672.be
70. Chauffert B, Mornex F, Bonnetain F, Rougier P, Mariette C, Bouché O, et al. Phase III trial comparing intensive induction chemoradiotherapy (60 Gy, infusional 5-FU and intermittent cisplatin) followed by maintenance gemcitabine with gemcitabine alone for locally advanced unresectable pancreatic cancer. Definitive results of the 2. Ann Oncol (2008) 19:1592–9. doi:10.1093/annonc/mdn281
71. Crane CH, Winter K, Regine WF, Safran H, Rich TA, Curran W, et al. Phase II study of bevacizumab with concurrent capecitabine and radiation followed by maintenance gemcitabine and bevacizumab for locally advanced pancreatic cancer: Radiation Therapy Oncology Group RTOG 0411. J Clin Oncol (2009) 27:4096–102. doi:10.1200/JCO.2009.21.8529
72. Sudo K, Yamaguchi T, Ishihara T, Nakamura K, Hara T, Denda T, et al. Phase II study of oral S-1 and concurrent radiotherapy in patients with unresectable locally advanced pancreatic cancer. Int J Radiat Oncol Biol Phys (2011) 80:119–25. doi:10.1016/j.ijrobp.2010.01.027
73. Oberic L, Viret F, Baey C, Ychou M, Bennouna J, Adenis A, et al. Docetaxel- and 5-FU-concurrent radiotherapy in patients presenting unresectable locally advanced pancreatic cancer: a FNCLCC-ACCORD/0201 randomized phase II trial’s pre-planned analysis and case report of a 5.5-year disease-free survival. Radiat Oncol (2011) 6:124. doi:10.1186/1748-717X-6-124
74. Brunner TB, Sauer R, Fietkau R. Gemcitabine/cisplatin versus 5-fluorouracil/mitomycin C chemoradiotherapy in locally advanced pancreatic cancer: a retrospective analysis of 93 patients. Radiat Oncol (2011) 6:88. doi:10.1186/1748-717X-6-88
75. Malik NK, May KS, Chandrasekhar R, Ma WW, Flaherty L, Iyer R, et al. Treatment of locally advanced unresectable pancreatic cancer: a 10-year experience. J Gastrointest Oncol (2012) 3:326–34. doi:10.3978/j.issn.2078-6891.2012.029
76. Ikeda M, Ioka T, Ito Y, Yonemoto N, Nagase M, Yamao K, et al. A multicenter phase II trial of S-1 with concurrent radiation therapy for locally advanced pancreatic cancer. Int J Radiat Oncol Biol Phys (2013) 85:163–9. doi:10.1016/j.ijrobp.2012.03.059
77. Shinchi H, Maemura K, Mataki Y, Kurahara H, Sakoda M, Ueno S, et al. A phase II study of oral S-1 with concurrent radiotherapy followed by chemotherapy with S-1 alone for locally advanced pancreatic cancer. J Hepatobiliary Pancreat Sci (2012) 19:152–8. doi:10.1007/s00534-011-0400-y
78. Herman JM, Wild AT, Wang H, Tran PT, Chang KJ, Taylor GE, et al. Randomized phase iii multi-institutional study of tnferade biologic with fluorouracil and radiotherapy for locally advanced pancreatic cancer: final results. J Clin Oncol (2013) 31:886–94. doi:10.1200/JCO.2012.44.7516
79. Ducreux M, Giovannini M, Baey C, Llacer C, Bennouna J, Adenis A, et al. Radiation plus docetaxel and cisplatin in locally advanced pancreatic carcinoma: a non-comparative randomized phase II trial. Dig Liver Dis (2014) 46:950–5. doi:10.1016/j.dld.2014.06.006
80. Rembielak AI, Jain P, Jackson AS, Green MM, Santorelli GR, Whitfield GA, et al. Phase II trial of cetuximab and conformal radiotherapy only in locally advanced pancreatic cancer with Concurrent Tissue Sampling Feasibility Study. Transl Oncol (2014) 7:55–64. doi:10.1593/tlo.13724
81. Kwak Y, Lee JH, Lee M, Chun H, Kim D, You YK, et al. Definitive concurrent chemoradiotherapy in locally advanced pancreatic cancer. Radiat Oncol J (2014) 32:49–56. doi:10.3857/roj.2014.32.2.49
82. Chung HW, Bang SM, Park SW, Chung JB, Kang JK, Kim JW, et al. A prospective randomized study of gemcitabine with doxifluridine versus paclitaxel with doxifluridine in concurrent chemoradiotherapy for locally advanced pancreatic cancer. Int J Radiat Oncol Biol Phys (2004) 60:1494–501. doi:10.1016/j.ijrobp.2004.05.061
83. Haddock MG, Swaminathan R, Foster NR, Hauge MD, Martenson JA, Camoriano JK, et al. Gemcitabine, cisplatin, and radiotherapy for patients with locally advanced pancreatic adenocarcinoma: results of the North Central Cancer Treatment Group Phase II Study N9942. J Clin Oncol (2007) 25:2567–72. doi:10.1200/JCO.2006.10.2111
84. Hong SP, Park JY, Jeon TJ, Bang S, Park SW, Chung JB, et al. Weekly full-dose gemcitabine and single-dose cisplatin with concurrent radiotherapy in patients with locally advanced pancreatic cancer. Br J Cancer (2008) 98:881–7. doi:10.1038/sj.bjc.6604247
85. Mamon HJ, Niedzwiecki D, Hollis D, Tan BR, Mayer RJ, Tepper JE, et al. A phase 2 trial of gemcitabine, 5-fluorouracil, and radiation therapy in locally advanced nonmetastatic pancreatic adenocarcinoma: cancer and Leukemia Group B (CALGB) 80003. Cancer (2011) 117:2620–8. doi:10.1002/cncr.25742
86. Crane CH, Varadhachary GR, Yordy JS, Staerkel GA, Javle MM, Safran H, et al. Phase II trial of cetuximab, gemcitabine, and oxaliplatin followed by chemoradiation with cetuximab for locally advanced (T4) pancreatic adenocarcinoma: correlation of Smad4(Dpc4) immunostaining with pattern of disease progression. J Clin Oncol (2011) 29:3037–43. doi:10.1200/JCO.2010.33.8038
87. Ch’Ang HJ, Lin YL, Wang HP, Chiu YF, Chang MC, Hsu CH, et al. Induction chemotherapy with gemcitabine, oxaliplatin, and 5-fluorouracil/leucovorin followed by concomitant chemoradiotherapy in patients with locally advanced pancreatic cancer: a Taiwan cooperative oncology group phase II study. Int J Radiat Oncol Biol Phys (2011) 81:e749–57. doi:10.1016/j.ijrobp.2010.10.034
88. Tozzi A, Comito T, Alongi F, Navarria P, Iftode C, Mancosu P, et al. SBRT in unresectable advanced pancreatic cancer: preliminary results of a mono-institutional experience. Radiat Oncol (2013) 8:148. doi:10.1186/1748-717X-8-148
89. Ke Q. S-1 plus gemcitabine chemotherapy followed by concurrent radiotherapy and maintenance therapy with S-1 for unresectable pancreatic cancer. World J Gastroenterol (2014) 20:13987. doi:10.3748/wjg.v20.i38.13987
Keywords: pancreatic cancer, protontherapy, heavy ion therapy, chemoradiotherapy, gemcitabine
Citation: Durante M, Tommasino F and Yamada S (2015) Modeling combined chemotherapy and particle therapy for locally advanced pancreatic cancer. Front. Oncol. 5:145. doi: 10.3389/fonc.2015.00145
Received: 03 April 2015; Accepted: 15 June 2015;
Published: 06 July 2015
Edited by:
Chris Schultz, Medical College of Wisconsin, USAReviewed by:
Kevin Camphausen, National Cancer Institute, USANitin Ohri, Albert Einstein College of Medicine, USA
Copyright: © 2015 Durante, Tommasino and Yamada. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Marco Durante, Department of Biophysics, GSI Helmholtzzentrum für Schwerionenforschung, Planckstraße 1, Darmstadt 64291, Germany, m.durante@gsi.de
 Marco Durante
Marco Durante Francesco Tommasino
Francesco Tommasino Shigeru Yamada
Shigeru Yamada