Antenatal Consultation and Postnatal Stress in Mothers of Preterm Neonates (A Two-Center Observational Case–Control Study)
- 1Division of Neonatology, Department of Paediatrics, Medical University of Graz, Graz, Austria
- 2Department of Pediatrics, University of Alberta, Edmonton, AB, Canada
- 3Centre for the Studies of Asphyxia and Resuscitation, Royal Alexandra Hospital, Edmonton, AB, Canada
Background: During antenatal consultation of women hospitalized for preterm labor, information of possible adverse outcomes is provided. This may however create additional maternal stress and raise some ethical concerns.
Objective: The aim of the present study was to evaluate the influence of antenatal consultation by a neonatologist on maternal stress after delivery of a preterm infant admitted to NICU.
Methods: In this study, secondary outcome parameters of a prospective two-center pilot observational study were analyzed. Mothers of preterm neonates < 36 weeks of gestation admitted at two tertiary-level Neonatal-Intensive-Care-Units (NICU) were included. Maternal stress was assessed with the Parental-Stress-Scale:NICU (PSS:NICU) within 72 h after birth. PSS:NICU measures three scales: “relationship and parental role,” “sights and sounds,” and “baby looks and behaves.” Maternal sociodemographic data were collected by questionnaire administered at the same time. Mothers who received antenatal neonatal consultation were matched for gestational age and compared to mothers who had no antenatal consultation by a neonatologist.
Results: A total of 46 mothers of preterm neonates were included, 23 mothers in each group. There was no significant difference in sociodemographic data between the two groups regarding neonates and mothers. There were no significant differences between the two groups regarding stress scales of “sights and sounds” (2.00 ± 0.76 versus 2.19 ± 0.79; p = 0.402), “looks and behaves” (2.55 ± 0.90 versus 2.48 ± 0.94; p = 0.732) and “relationship and parental role” (3.28 ± 1.23 versus 3.46 ± 1.07; p = 0.517).
Conclusion: Our study demonstrated that antenatal consultation by a neonatologist had no substantial influence on postnatal maternal stress in mothers of preterm neonates admitted to the NICU.
Introduction
Already 70 years ago data suggested that maternal emotional stress during pregnancy might affect the fetus (1). Further, more than 50 years ago several studies demonstrated an association of maternal experiences and emotional stress during pregnancy and the health of the infant resulting in an impaired level of motor development (2). Many studies focused on maternal and paternal stress were published in the last decades. A meta-analysis recently reported that parents of preterm infants experienced more stress than parents of term infants (3). The differences in stress level between parents of preterm and term neonates are described to be small (4). However, neurobehavioral development of these sick neonates depends on parental stress and preterm birth is associated with altered parental mental health and family wellbeing after birth (3, 5, 6).
Low gestational age and birth weight are main factors affecting parental stress (2, 5–7). However, stress is determined by many other factors. Recently, we have demonstrated that the level of maternal stress after preterm birth increases with the length of antenatal hospital stay (8). This study suggested that antenatal intra-hospital management might have an influence on postnatal maternal stress. After hospital admission mothers with imminent preterm birth are generally informed by obstetricians about the imminent obstetrical management and by pediatricians/neonatologists about management and concerns about prematurity. A recent study reported that antenatal consultation by a neonatologist is perceived by women hospitalized for preterm labor as a source of stress and reassurance (9).
Different methods have been described to assess psychosocial stress such as physiological changes of heart rate, blood pressure, and cortisol level (10). Alternatively, stress may be assessed by using validated questionnaires such as the Trier Social Stress Test (TSST) (11), the Parenting Stress Index (PSI) (12), and the Parental Stressor Scale: Neonatal Intensive Care Unit (PSS:NICU) (13–16).
There are no data available, if antenatal consultation by a neonatologist has an impact on stress level of mothers after birth of premature infant admitted to NICU. The aim of the present study was therefore to evaluate the influence of antenatal consultation by a neonatologist for imminent premature birth on maternal stress level after birth of a premature neonate admitted to NICU. We hypothesized that antenatal consultation by a neonatologist for premature birth increases stress level due to information that is not only reassuring but also includes information of possible adverse outcome.
Materials and Methods
The present observational case–control study is part of a two-center observational study at the Royal Alexandra Hospital of Edmonton/Canada and the Department of Pediatrics, Medical University of Graz/Austria (8). Secondary outcome parameters were analyzed. This study was carried out in accordance with the recommendations of Regional Committees on Biomedical Research Ethics with written informed consent from all subjects. All subjects gave written informed consent in accordance with the Declaration of Helsinki. The protocol was approved by the (i) The Royal Alexandra Hospital Research Committee and Health Ethics Research Board, University of Alberta and (ii) Ethikkommission, Medizinische Universität Graz.
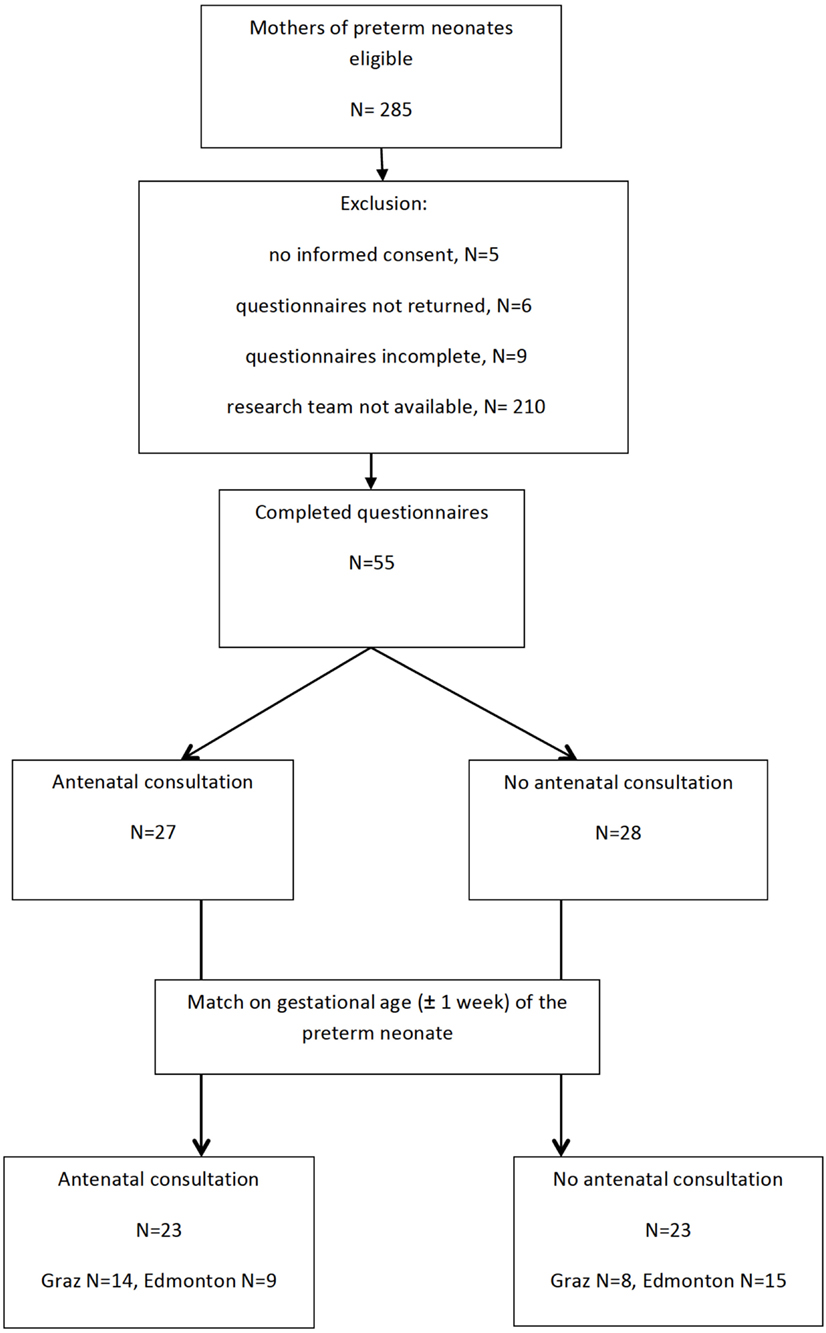
Mothers of preterm infants born at < 36 weeks of gestation admitted to the NICUs were included. Exclusion criteria were neonatal congenital malformation and or chromosomal anomalies. Information was collected from data sources including parental questionnaire and accessing hospital charts. Mothers with antenatal consultation by a neonatologist were compared to mothers without antenatal consultation by a neonatologist. Mothers were matched for gestational age (±1 week) of their preterm babies.
The parental stress scale: neonatal intensive care unit (PSS:NICU) questionnaire was given to mothers of preterm infants within 72 h after birth and were asked to complete it within 24 h. The PSS:NICU questionnaire measures parental stress in three different scales: “relationship and parental role,” “sights and sounds,” and “baby looks and behaves” (14).
In the subscale “relationship and role” mothers are asked how they are affected by their relationship to the neonate and their role at the NICU, “sights and sounds” how mothers are affected by the visual and acoustic surrounding and, “babies looks and behaves” how mothers are affected by the neonate’s looks and behavior.
Maternal sociodemographic data were collected and the infant’s medical chart was accessed to record time of admission of the mother, time of birth, gestational age, birth weight, gender, need of respiratory support (nasal CPAP or mechanical ventilation), hemodynamic treatment (e.g., catecholamines), or the presence of cerebral injury (defined as intraventricular hemorrhage of any grade). The study was designed as a pilot study and therefore a convenient representative sample was used (17).
Differences between groups were analyzed using a Student’s t-test or Mann–Whitney U test for continuous parametric and non-parametric variables, respectively. To analyze differences in categorical variables Chi Square test and, when appropriate, Fisher’s Exact test were used. Continuous data are presented as median (interquartile range) or mean (SD). A p-value < 0.05 was considered significant.
Results
During the study period, 155 preterm infants in Edmonton and 130 in Graz were eligible (Figure 1). Twenty-three mothers of preterm infants with antenatal consultation by a neonatologist were matched for gestational age to 23 mothers of preterm infants without antenatal consultation by a neonatologist. Median gestational age of preterm infants with and without antenatal consultation was 31 (27–34) weeks. Indications for preterm birth in mothers with antenatal consultation were spontaneous preterm labor (n = 11), premature preterm rupture of membrane (n = 4), eclampsia (n = 3), and others (n = 5). Indications for preterm birth in mothers without antenatal consultation were spontaneous preterm labor (n = 9), premature preterm rupture of membrane (n = 5), eclampsia (n = 4), and others (n = 5). There were no significant differences in maternal and neonatal demographic and clinical data between the two groups (Table 1).
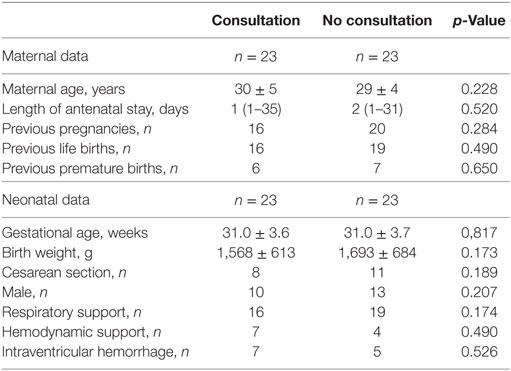
Table 1. Demographic data of mothers and preterm neonates with and without antenatal neonatal consultation.
There were no significant differences in the stress level between both groups regarding the stress scales of “sights and sounds,” “looks and behaves,” and “relationship and parental role” assessed with the PSS:NICU questionnaire (Table 2).
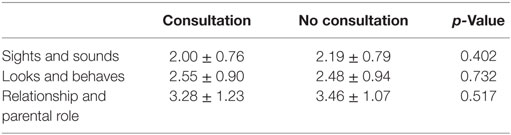
Table 2. PSS:NICU results of mothers of preterm neonates with and without antenatal neonatal consultation.
Moreover, there were no significant differences between the two centers in stress scales: “sights and sounds” (2.25 ± 0.78 versus 1.89 ± 0.72; p = 0.08) “looks and behaves” (2.68 ± 0.94 versus 2.42 ± 0.91; p = 0.29) and “relationship and parental role” (3.31 ± 1.17 versus 3.37 ± 1.16; p = 0.85).
Discussion
This is the first study to compare stress in mothers of preterm neonates admitted to NICU with and without antenatal consultation by a neonatologist. Overall, we found no substantial association between antenatal consultation by a neonatologist and postnatal maternal stress. The stress level of mothers of preterm neonates admitted to NICU was within the range of formerly published studies (3, 8). Compared to published stress levels of term neonates the present stress levels in preterm neonates were elevated (3).
Women hospitalized for preterm labor and interviewed for their perspectives of antenatal consultation by a neonatologist expected the consultation as a stressor as well as a source of reassurance (9). During antenatal consultation, neonatologists are mandated to discuss potential postnatal medical management, prognosis, and possible adverse outcome of premature birth. In particular, information about short- and/or long-term adverse outcomes could act as a maternal stressor influencing postnatal stress levels. In a recent study, most women at risk of preterm delivery receiving antenatal consultation by a neonatologist reported a positive experience (18). Miquel-Verges et al. reported that mothers of neonates with known congenital anomalies want specific and realistic information during antenatal consultation (4). They also described that receiving conflicting information increased anxiety and decreased confidence. In comparison, our study suggests that information about adverse outcomes does not increase maternal stress once preterm neonates are admitted to the NICU. In the present study, antenatal neonatal consultations were performed by experienced neonatologists aiming to provide not only information of adverse outcomes but also reassurance and support. The latter might have caused the lack of increased stress after antenatal consultation (9). Limitations include that individual content of each consultation and the number of different neonatologists were not recorded. Another limitation is that the negative results might be due to the small sample size. However, due to the similar results in the subscales of the PSS:NICU, when both groups are compared, a substantial influence of antenatal neonatal consultation on maternal stress after delivery of a preterm infant admitted to NICU can be ruled out. A strength of our study was the two-center approach to compare maternal stress after preterm birth (Canada/Austria).
Conclusion
Antenatal neonatal consultation in women hospitalized for imminent preterm birth does not substantially influence maternal stress after preterm birth. Information of possible adverse outcome and reassurance seems to balance maternal stress after preterm birth. However, maternal stress levels after preterm birth are increased after NICU admission when compared to maternal stress levels after term deliveries and no NICU admission. New strategies for antenatal consultation need to be developed to reduce maternal stress after preterm birth.
Ethics Statement
This study was carried out in accordance with the recommendations of Regional Committees on Biomedical Research Ethics with written informed consent from all subjects. All subjects gave written informed consent in accordance with the Declaration of Helsinki. The protocol was approved by the (i) The Royal Alexandra Hospital Research Committee and Health Ethics Research Board, University of Alberta and (ii) Ethikkommission, Medizinische Universität Graz.
Author Contributions
Conception and design; analysis and interpretation of the data: EP-S, GP, BU, P-YC, and GS. Collection and assembly of data: EP-S, GP, NB-S, BS, BU, and GS. Drafting of the article: EP-S, GP, and GS. Critical revision of the article for important intellectual content; final approval of the article: EP-S, GP, NB-S, BS, BU, P-YC, and GS.
Conflict of Interest Statement
The authors have no financial relationships relevant to this article to disclose. No current funding source for this study. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Funding
We would like to thank the public for donation to our funding agencies: GS is a recipient of the Heart and Stroke Foundation/University of Alberta Professorship of Neonatal Resuscitation and a Heart and Stroke Foundation Canada and a Heart and Stroke Foundation Alberta New Investigator Award.
Abbreviations
PSS:NICU, parental stressor scale: neonatal intensive care unit; NICU, neonatal intensive care unit.
References
1. Sonntag LW. The significance of fetal environmental differences. Amer J Obstet Gynec (1941) 42:996. doi:10.1016/S0002-9378(41)90265-X
2. Abramson JH, Singh AR, Mbambo V. Antenatal stress and the baby’s development. Arch Dis Child (1961) 36:42–9. doi:10.1136/adc.36.185.42
3. Schappin R, Wijnroks L, Uniken Venema MM, Jongmans MJ. Rethinking stress in parents of preterm infants: a meta-analysis. PLoS One (2013) 8(2):e54992. doi:10.1371/journal.pone.0054992
4. Miquel-Verges F, Woods SL, Aucott SW, Boss RD, Sulpar LJ, Donohue PK. Prenatal consultation with a neonatologist for congenital anomalies: parental perceptions. Pediatrics (2009) 124(4):e573–9. doi:10.1542/peds.2008-2865
5. Treyvaud K, Anderson VA, Howard K, Bear M, Hunt RW, Doyle LW, et al. Parenting behavior is associated with the early neurobehavioral development of very preterm children. Pediatrics (2009) 123(2):555–61. doi:10.1542/peds.2008-0477
6. Spittle AJ, Thompson DK, Brown NC, Treyvaud K, Cheong JLY, Lee KJ, et al. Neurobehaviour between birth and 40 weeks’ gestation in infants born <30 weeks’ gestation and parental psychological wellbeing: predictors of brain development and child outcomes. BMC Pediatr (2014) 14:111. doi:10.1186/1471-2431-14-111
7. Treyvaud K, Lee KJ, Doyle LW, Anderson PJ. Very preterm birth influences parental mental health and family outcomes seven years after birth. J Pediatr (2014) 164(3):515–21. doi:10.1016/j.jpeds.2013.11.001
8. Pichler-Stachl E, Pichler G, Baik N, Urlesberger B, Alexander A, Urlesberger P, et al. Maternal stress after preterm birth: impact of length of antepartum hospital stay. Women Birth (2016) 29(6):e105–9. doi:10.1016/j.wombi.2016.04.008
9. Gaucher N, Payot A. From powerlessness to empowerment: mothers expect more than information from prenatal consultation for preterm labour. Paediatr Child Health (2011) 16:638–42. doi:10.1093/pch/16.10.638
10. Campbell J, Ehlert U. Acute psychosocial stress: does the emotional stress response correspond with physiological responses? Psychoneuroendocrinology (2012) 37(8):1111–34. doi:10.1016/j.psyneuen.2011.12.010
11. Hellhammer J, Schubert M. The physiological response to trier social stress test relates to subjective measures of stress during but not before or after the test. Psychoneuroendocrinology (2012) 37(1):119–24. doi:10.1016/j.psyneuen.2011.05.012
12. Huhtala M, Korja R, Lehtonen L, Haataja L, Lapinleimu H, Rautava P, et al. Parental psychological well-being and behavioral outcome of very low birth weight infants at 3 years. Pediatrics (2012) 129(4):e937–44. doi:10.1542/peds.2011-2411
13. Miles MS, Funk SG, Kasper MA. The neonatal intensive care unit environment: sources of stress for parents. AACN Clin Issues Crit Care Nurs (1991) 2(2):346–54. doi:10.4037/15597768-1991-2022
14. Miles MS, Funk SG, Carlson J. Parental stressor scale: neonatal intensive care unit. Nurs Res (1993) 42(3):148–52. doi:10.1097/00006199-199305000-00005
15. Miles MS, Brunssen SH. Psychometric properties of the parental stressor scale: infant hospitalization. Adv Neonatal Care (2003) 3(4):189–96. doi:10.1016/S1536-0903(03)00138-3
16. Franck LS, Cox S, Allen A, Winter I. Measuring neonatal intensive care unit-related parental stress. J Adv Nurs (2005) 49:608–15. doi:10.1111/j.1365-2648.2004.03336.x
17. Thabane L, Ma J, Chu R, Cheng J, Ismaila A, Rios LP, et al. A tutorial on pilot studies: the what, why and how. BMC Med Res Methodol (2010) 10:1. doi:10.1186/1471-2288-10-1
Keywords: neonatologist, antenatal consultation, preterm birth, neonatal intensive care unit, maternal stress
Citation: Pichler-Stachl E, Baik-Schneditz N, Schwaberger B, Urlesberger B, Pichler G, Cheung P-Y and Schmölzer GM (2017) Antenatal Consultation and Postnatal Stress in Mothers of Preterm Neonates (A Two-Center Observational Case–Control Study). Front. Pediatr. 5:275. doi: 10.3389/fped.2017.00275
Received: 15 August 2017; Accepted: 06 December 2017;
Published: 20 December 2017
Edited by:
Eugene Dempsey, University College Cork, IrelandReviewed by:
Roland H. Hentschel, Universitätsklinikum Freiburg, GermanyGunnar Naulaers, KU Leuven, Belgium
Copyright: © 2017 Pichler-Stachl, Baik-Schneditz, Schwaberger, Urlesberger, Pichler, Cheung and Schmölzer. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gerhard Pichler, gerhard.pichler@medunigraz.at
 Elisabeth Pichler-Stachl1,2,3
Elisabeth Pichler-Stachl1,2,3
 Bernhard Schwaberger
Bernhard Schwaberger Berndt Urlesberger
Berndt Urlesberger Gerhard Pichler
Gerhard Pichler Po-Yin Cheung
Po-Yin Cheung Georg M. Schmölzer
Georg M. Schmölzer