- 1College of Medicine, China Medical University, Taichung, Taiwan
- 2Department of Family Medicine, China Medical University Hospital, Taichung, Taiwan
- 3Management Office for Health Data, China Medical University Hospital, Taichung, Taiwan
- 4Graduate Institute of Integrated Medicine, China Medical University, Taichung, Taiwan
- 5College of Medicine, Tzu Chi University, Hualien, Taiwan
- 6Department of Internal Medicine, Taichung Tzu Chi General Hospital, Taichung, Taiwan
Aim: Little is known regarding the relationship between use of oral corticosteroids and hip fracture in the elderly in Taiwan. The aim of the study was to examine this issue.
Methods: A retrospective population-based case-control study using the database of the Taiwan National Health Insurance Program (2000–2013) was conducted. We identified 4538 individuals aged ≥ 65 years with newly diagnosed hip fracture as the cases. We randomly selected 4538 individuals without hip fracture as the control subjects. The cases and the control subjects were matched with sex, age, comorbidities, and the year of index date. Individuals who never had a prescription for oral corticosteroids were defined as never use. Individuals who ever had at least one prescription for oral corticosteroids were defined as ever use. The odds ratio (OR) and 95% confidence interval (CI) of hip fracture associated with oral corticosteroids use was estimated by a multivariable unconditional logistic regression analysis.
Results: After adjustments for potential confounding factors, the multivariable logistic regression model showed that the adjusted OR of hip fracture was 1.17 for individuals with ever use of oral corticosteroids (95%CI 1.08, 1.28), compared to those with never use of oral corticosteroids. An sub-analysis showed that for every 1-mg increase in cumulative dose of oral corticosteroids, the adjusted OR of hip fracture was 1.01 (95% CI 1.01, 1.02). The adjusted ORs were 1.31 (95% CI 1.17, 1.47) for cumulative exposure to oral corticosteroids ≥ 3 months and 1.09 (95% CI 0.98, 1.20) for cumulative exposure < 3 months.
Conclusion: We conclude that oral corticosteroids use is associated with a trivial but statistically significant increase in risk of hip fracture in Taiwan. Additionally, the results suggest that there are dose-response and duration-response effects of oral corticosteroids on the risk of hip fracture. The results confirm our understanding of oral corticosteroid-associated hip fracture in the elderly.
Introduction
Hip fracture persists to be an important public health problem in the elderly worldwide due to its large socioeconomic burden, substantial morbidity and mortality. A systematic Review by Mohd-Tahir and Li (2017) reported that healthcare costs associated with hip fracture accounted for more than one third of gross domestic product (GDP) in some counties of Asia. A observational study in Taiwan by Huang et al. (2016) reported that if the hip-fractured older people had more comorbidities, they would be more likely to have poor outcomes on psychological conditions, such as cognitive impairment and depression. A prospective cohort study in Taiwan by Hung et al. (2014) reported that the hip-fractured older people were at higher risk of mortality compared with the non-fractured matched older people.
It is well-known that individuals with corticosteroids use are at an excess risk of osteoporotic fractures. A population-based case-control study in Denmark by Vestergaard et al. (2003) reported that corticosteroid users were at increased risk of hip fracture compared to never users. A meta-analysis by Kanis et al. (2004) reported that corticosteroids use correlated with high risk of hip fracture in the elderly aged 65–85 (relative risk 2.13–2.98).
Due to the following points: (a) hip fracture remains to be a public health problem in the elderly, (b) the hospitalization number of hip fracture and the total costs of hip fracture hospitalization substantially increased among the elderly in Taiwan reported by Chan et al. (2013) (c) to date, data on the effect of corticosteroids use and the risk of hip fracture is limited in the elderly in Taiwan, we made a rational link between corticosteroids use and hip fracture in the elderly. Therefore, in the present study we used the claim data from the Taiwan National Health Insurance Program to test the following objectives: (a) the relationship between use of oral corticosteroids and hip fracture in the elderly; (b) the dose-response and duration-response effects of oral corticosteroids on the risk of hip fracture.
Materials and Methods
Data Source and Study Design
Taiwan is an independent country with more than 23 million residents (Chao et al., 2015; Chen et al., 2015; Ho and Chang, 2015; Hsiao et al., 2015; Hung and Ku, 2015; Chen and Wu, 2016; Chen S.Y. et al., 2016; Chen Y.F. et al., 2016; Hsieh et al., 2016; Hsu and Yin, 2016; Huang and Chang, 2016; Lin and Lin, 2016; Maa and Leu, 2016; Ooi, 2016; Yu et al., 2016). The Taiwan National Health Insurance Program began in March 1995, and now it has covered around 99% of the residents living in Taiwan (National Health Insurance Research Database, 2017). The details of the program were written down in previous studies (Lai et al., 2010; Kuo et al., 2015; Yang et al., 2015; Chen H.Y. et al., 2016; Tsai et al., 2016). A retrospective population-based case-control study using the database of the Taiwan National Health Insurance Program (2000–2013) was conducted. The study was approved by the Research Ethics Committee of China Medical University and Hospital in Taiwan (CMUH-104-REC2-115).
Identification of Cases and Control Subjects
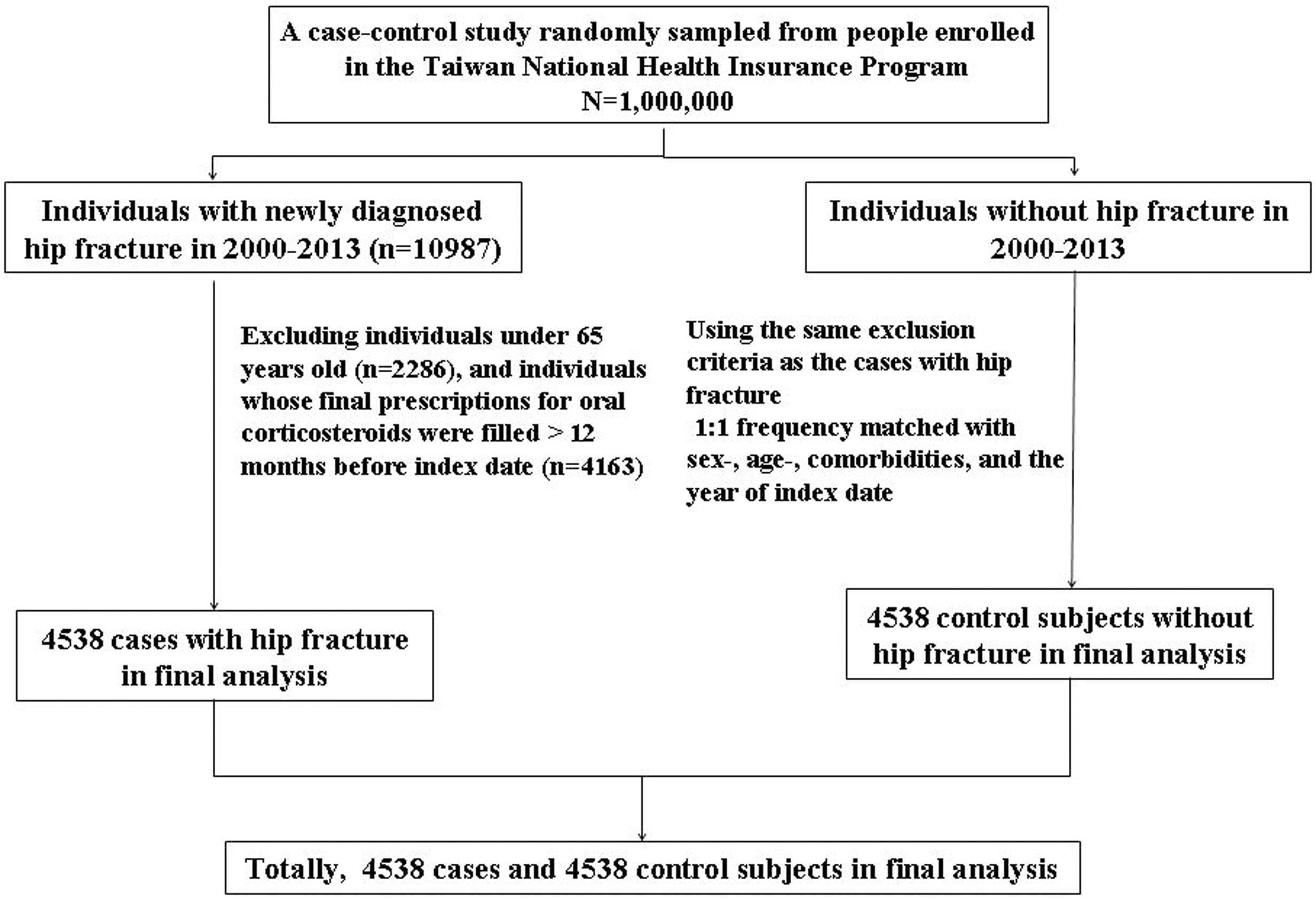
We identified individuals aged ≥ 65 years with newly diagnosed hip fracture in 2000–2013 as the cases with hip fracture [the International Classification of Diseases (ICD) 9th Revision, ICD-9 code 820]. The index date was defined as the date of cases being diagnosed with hip fracture. We assigned a random number for each individual without a diagnosis of hip fracture in the database by generating random numbers between 0 and 1 that were distributed uniformly. Individuals without hip fracture randomly selected were assigned as the control subjects who were matched in terms of sex, age (5-year interval), and comorbidities. The enrollment date for the control subjects was matched with the same year of cases with hip fracture, while the month and day were randomly assigned. The sample size of the control subjects was onefold as the cases with hip fracture. Therefore, it is unlikely that the control subjects were chosen intentionally (Figure 1).
Confounding Factors
Comorbidities potentially associated with hip fracture before the index date were included as follows: alcohol-related disease, cardiovascular disease, chronic kidney disease, chronic obstructive pulmonary disease, diabetes mellitus, hyperlipidemia, and hypertension. All comorbidities were used based on ICD-9 codes. To increase the analysis accuracy, individuals who needed to have the same diagnosis for at least three consecutive records in the ambulatory care visit and/or at least one time of hospitalization diagnosis could be included in the study. Principal diagnosis and secondary diagnosis were used equally. Therefore, hip fracture and other comorbidities were addressed for three or more records in the ambulatory care and/or at least one record during hospitalization. Such strict criteria have been used in the previous study (Lai et al., 2015d, 2017a,b,c).
Measurements of Corticosteroids Use
The measurements of corticosteroids use were adapted from previous studies (Lai et al., 2015a, 2016, 2017c). Shortly speaking, there is much difficulty in measuring the dosage of topical corticosteroids use or inhaled corticosteroids use. Individuals with long-time use of injected corticosteroids at outpatient department are also rarely found. To measure the dosage accurately, only oral corticosteroids were included for statistical analysis. Therefore, topical, inhaled, and injected corticosteroids were combined together as other forms of corticosteroids for adjustments. The availability of oral corticosteroids in Taiwan was listed as follows: cortisone, dexamethasone, fludrocortisone, methylprednisolone, prednisolone, and triamcinolone. We colleted the prescription histories of oral corticosteroids before the index date. If individuals’ final prescriptions for oral corticosteroids were filled > 12 months before the index date, they were excluded from the study. Therefore, only individuals whose final prescriptions for oral corticosteroids were filled within 12 months before the index date could be included for statistical analysis. Individuals who never had a prescription for oral corticosteroids were defined as never use. Individuals who had at least one prescription for oral corticosteroids were defined as ever use.
Statistical Analysis
The Chi-square test was used to compare the differences of sex, age, oral corticosteroids use, other forms of corticosteroids use, and comorbidities between the cases and the control subjects. The t-test was used to compare the differences of mean ages and mean days of exposure to oral corticosteroids between the cases and the control subjects. The univariable and multivariable unconditional logistic regression models were used for statistical analysis. Variables which were found to be statistically significant in a univariable model were further examined in a multivariable model to measure the odds ratio (OR) and 95% confidence interval (CI) of hip fracture associated with oral corticosteroids use. We conducted the analysis to examine the dose-response and duration-response effects of oral corticosteroids on the risk of hip fracture. We conducted an additional analysis to examine the interaction effects between oral corticosteroids use and polypharmacy (use of five or more drugs) on the risk of hip fracture. All data processing and statistical analyses were performed with the SAS software version 9.2 (SAS Institute, Inc., Cary, NC, United States). A two-tailed P-value < 0.05 was considered statistically significant.
Results
Descriptive Information of the Study Population
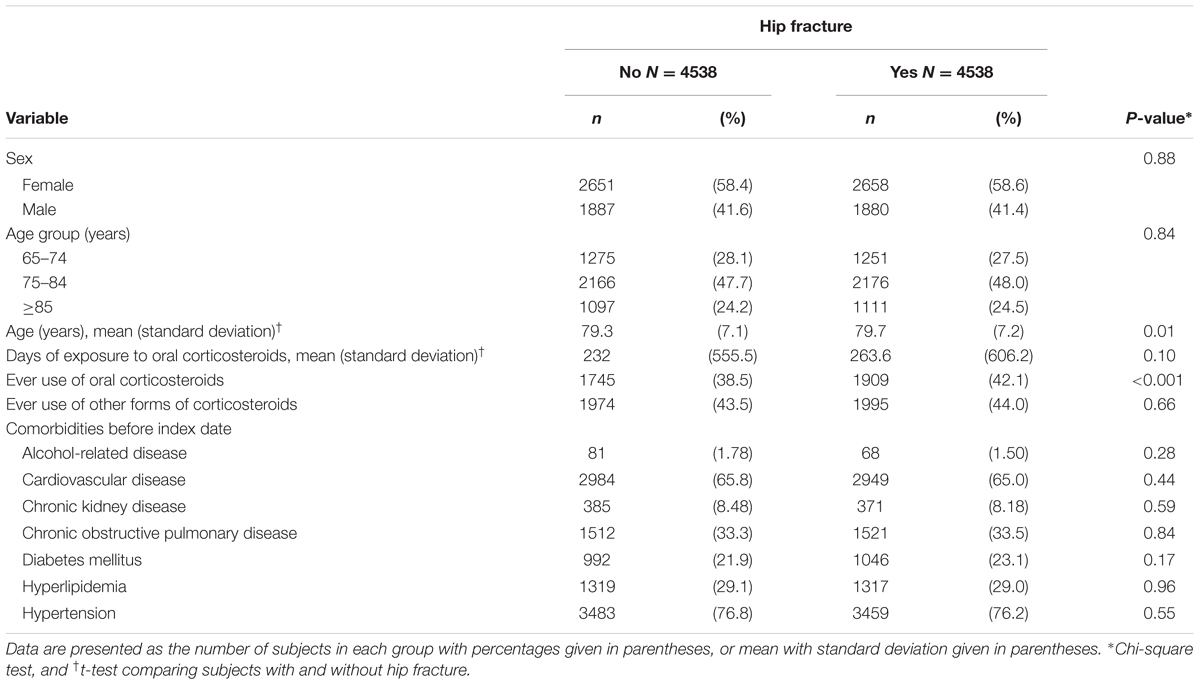
Table 1 shows 4538 new cases with hip fracture and 4538 control subjects without hip fracture (Table 1). The cases and the control subjects had similar distribution of sex. Females constituted a higher proportion in cases and control subjects (58%). The mean ages (standard deviation) were 79.7 (7.2) years in cases and 79.3 (7.1) years in control subjects, with statistical significance (t-test, P = 0.01). The mean durations (standard deviation) of exposure to oral corticosteroids were 263.6 (606.2) days for the cases and 232 (555.5) days for the control subjects, without statistic significance (t-test, P = 0.10). The cases were more likely to have a higher proportion of ever use of oral corticosteroids than the control subjects (42.1% vs. 38.5%, Chi-square test, P < 0.001). There were no significant differences of ever use of other forms of corticosteroids and comorbidities between the cases and the control subjects (Chi-square test, P > 0.05).
Association of Hip Fracture with Oral Corticosteroids Use, Other Forms of Corticosteroids Use, and Comorbidities in the Elderly
After adjustments for potential confounding factors, the multivariable logistic regression model showed that the adjusted OR of hip fracture was 1.17 for individuals with ever use of oral corticosteroids (95% CI 1.08, 1.28), compared to individuals with never use of oral corticosteroids (Table 2). In addition, for every 1-year increase in age, the adjusted OR of hip fracture was 1.01 (95% CI 1.00, 1.01).

TABLE 2. Odds ratio and 95% confidence interval of hip fracture associated with corticosteroids use, other forms of corticosteroids, and comorbidities in the elderly.
Association of Hip Fracture with Cumulative Dosage of Oral Corticosteroids Use in the Elderly
We conducted an analysis for the dose-response effect of oral corticosteroids on the risk of hip fracture (Table 3). After adjustments for potential confounding factors, for every 1-mg increase in cumulative dose of oral corticosteroids, the adjusted OR of hip fracture was 1.01 (95% CI 1.01, 1.02), compared to individuals with never use of oral corticosteroids.
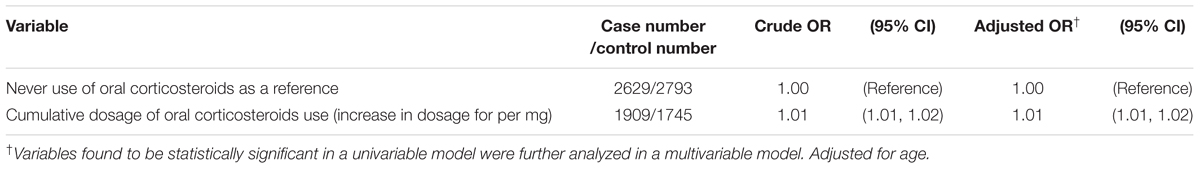
TABLE 3. Association of hip fracture with cumulative dosage of oral corticosteroids use in the elderly.
Association of Hip Fracture with Cumulative Duration of Oral Corticosteroids Use in the Elderly
We conducted an analysis for the duration-response effect of oral corticosteroids on the risk of hip fracture (Table 4). When stratified by cumulative duration of usage, the adjusted OR of hip fracture was 1.09 (95% CI 0.98, 1.20) when cumulative exposure to oral corticosteroids < 3 months. The adjusted OR increased to 1.31 (95% CI 1.17, 1.47) when cumulative exposure to oral corticosteroids ≥ 3 months, compared to individuals with never use of oral corticosteroids.
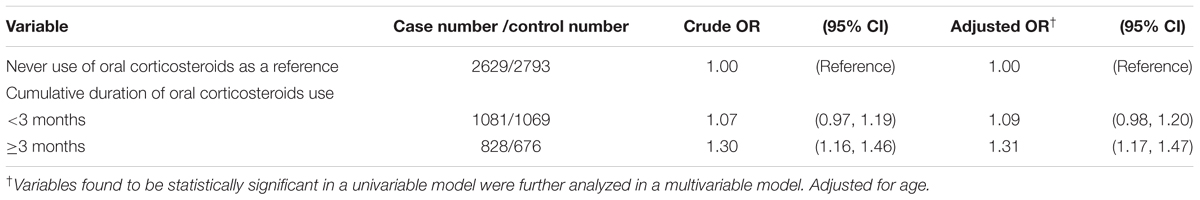
TABLE 4. Association of hip fracture with cumulative duration of oral corticosteroids use in the elderly.
We made a further analysis to show the interaction effects between oral corticosteroids use and polypharmacy on the risk of hip fracture (Table not shown). When compared to individuals with never use of oral corticosteroids and without polypharmacy, the adjusted OR of hip fracture was 1.15 (95% CI 1.03, 1.27) among individuals with ever use of oral corticosteroids alone and without polypharmacy. The adjusted OR increased to 1.36 (95% CI 1.21, 1.54) among individuals with ever use of oral corticosteroids and polypharmacy.
Discussion
In the present study, we observed that oral corticosteroid use correlated with a trivial but statistically significant increase in odds of hip fracture, compared to never use (adjusted OR 1.17). To reduce the confounding effects caused by comorbidities, the cases and the control subjects were matched with comorbidities. There were no significant differences of ever use of other forms of corticosteroids and comorbidities between the cases and control subjects (Table 1). Therefore, the increased odds of hip fracture could not be totally attributed to the confounding effects caused by other forms of corticosteroids and comorbidities.
In a further analysis, we observed that the odds of hip fracture increased with the cumulative dosage of oral corticosteroid use (Table 3), which was compatible with previous studies showing that increasing cumulative dosage of corticosteroid use was associated with increased odds of hip fracture (Van Staa et al., 2000; Vestergaard et al., 2003). These findings suggest that there seems to be a dose-response relationship between oral corticosteroid use and the risk of hip fracture. That is, the higher the cumulative dosage of oral corticosteroid, the greater risk of hip fracture.
In a further analysis, we observed that despite not reaching statistic significance, the risk of hip fracture became slightly higher when cumulative exposure to oral corticosteroids < 3 months (adjusted OR 1.09). This finding was partially compatible with Van Staa et al. (2002) meta-analysis showing that the fracture risk increased more markedly within 3–6 months of initiating oral corticosteroid use. These findings suggest that the risk of hip fracture might increase within the first months of initiating oral corticosteroid use.
In addition, we observed that the odds of hip fracture significantly increased to 1.31 when cumulative exposure to oral corticosteroids ≥ 3 months (Table 4), which was compatible with previous studies showing that there was a duration-response relationship between oral corticosteroid use and the risk of hip fracture (Van Staa et al., 2000; Steinbuch et al., 2004). That is, the longer of exposure to oral corticosteroid, the greater risk of hip fracture. A cross-sectional study by Baron et al. (1999) showed that bone mineral density was lower among post-menopausal women using long-term corticosteroids. A cross-sectional study by Shiga et al. (2009) showed that increased bone resorption and decreased bone formation of hip contributed to a greater risk of hip fracture for older women with osteoporosis. Based on the above review and discussion, we confirm previous observational studies that oral corticosteroid-induced osteoporosis might be associated with a trivial but statistically significant increase in the risk of hip fracture in the elderly.
In a previous study, we observed that polypharmacy (use five or more drugs) was associated with increased risk of hip fracture in the elderly (Lai et al., 2010). In a further analysis, we observed that individuals with ever use of oral corticosteroids alone and without polypharmacy remained to have a trivial but statistically significant increase in odds of hip fracture (adjusted OR 1.15). This finding suggests that oral corticosteroids use has an additional effect on the risk of hip fracture, independent of polypharmacy. If individuals concurrently had oral corticosteroids use and polypharmacy, the odds would markedly increase to 1.36. This finding suggests that there is an interaction effect between oral corticosteroids use and polypharmacy on the risk of hip fracture in the elderly.
Some limitations should be discussed in the present study. First, due to the inherent limitation of claim data, there was no record on bone mineral density. We could not examine the status of bone mineral density at the time of hip fracture. That is why we were unable to include osteoporosis for statistical analysis. However, it indicates a research direction on the status of bone mineral density when the elderly developed hip fracture. Second, due to the same limitation, we were unable to make sure whether patients really used oral corticosteroids or not. Therefore, the prescription histories of oral corticosteroids were used for instead. Third, due to the same limitation, there was no record on the indications why oral corticosteroids were prescribed. Thus, we could not explain the high rates of ever use of oral corticosteroids both in cases with hip fracture and in control subjects (42.1% vs. 38.5%). Fourth, we should examine the interaction between oral corticosteroids and other bone-related medications, or the interaction between oral corticosteroids and other falling-related medications. Furthermore, there is much difficulty in designing such a case-control study which needs to include all concomitant medications for adjustments. The more appropriate option was to examine the relative risk of hip fracture associated with one potential drug. That is why we only included oral corticosteroids for statistical analysis. However, it indicates a research direction on the relationship between all concomitant medications in detail and the risk of hip fracture. Fifth, due to unable to obtain specific ICD-9 codes for falls, gait and balance disorders, we were unable to include these disorders for statistical analysis. This point has been addressed in a previous study (Lai et al., 2015b). Sixth, although the diagnosis of all comorbidities was based on ICD-9 codes, the accuracy of ICD-9 codes has been fully discussed in previous studies (Lin et al., 2013; Lai et al., 2015b,c; Shen et al., 2016; Liao et al., 2017a,b; Hung et al., 2017).
Despite the above limitations, some strengths of the present study deserve discussion. Although it is well-known that corticosteroids use creates increased risk of osteoporotic fractures, this is a straight-forward study to examine the relationship between use of oral corticosteroids and hip fracture in the elderly in Taiwan. We present confirmatory data from Taiwan on this adverse drug reaction. We emphasize the dose-response and the duration-response effects of oral corticosteroids on the risk of hip fracture. The topic is an important one and deserves a practical value. The used methodology (case-control study) and the analysis seem adequate. The discussion comprises the essential topics. This manuscript provides the updated evidence to the readers. The study extends our knowledge of this correlation to an Asian country having a well-organized health care system where such an analysis could be performed based on a reliable database.
We conclude that oral corticosteroids use is associated with a trivial but statistically significant increase in the risk of hip fracture in the elderly in Taiwan. Additionally, the results suggest that there are dose-response and duration-response effects of oral corticosteroids on the risk of hip fracture. These findings confirm our understanding of oral corticosteroid-associated hip fracture in the elderly.
Author Contributions
S-WL planned and conducted this study. He contributed to the conception of the article, initiated the draft of the article, and revised the article. C-LL conducted the data analysis and revised the article. K-FL planned and conducted this study. He participated in the data and revised the article.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
This study was supported in part by Taiwan Ministry of Health and Welfare Clinical Trial Center (MOHW106-TDU-B-212-113004), China Medical University Hospital, Academia Sinica Taiwan Biobank Stroke Biosignature Project (BM10601010036), Taiwan Clinical Trial Consortium for Stroke (MOST 106-2321-B-039-005), Tseng-Lien Lin Foundation, Taichung, Taiwan, Taiwan Brain Disease Foundation, Taipei, Taiwan, and Katsuzo and Kiyo Aoshima Memorial Funds, Japan. These funding agencies did not influence the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
Baron, Y. M., Brincat, M. P., and Galea, R. (1999). Increased reduction in bone density and skin thickness in postmenopausal women taking long-term corticosteroid therapy: a suggested role for estrogen add-back therapy. Climacteric 2, 189–196. doi: 10.3109/13697139909038061
Chan, D. C., Lee, Y. S., Wu, Y. J., Tsou, H. H., Chen, C. T., Hwang, J. S., et al. (2013). A 12-year ecological study of hip fracture rates among older Taiwanese adults. Calcif. Tissue Int. 93, 397–404. doi: 10.1007/s00223-013-9759-x
Chao, P. C., Chuang, H. J., Tsao, L. Y., Chen, P. Y., Hsu, C. F., Lin, H. C., et al. (2015). The Malnutrition Universal Screening Tool (MUST) and a nutrition education program for high risk cancer patients: strategies to improve dietary intake in cancer patients. Biomedicine 5, 30–35. doi: 10.7603/s40681-015-0017-6
Chen, H. F., and Wu, K. J. (2016). Epigenetics, TET proteins, and hypoxia in epithelial-mesenchymal transition and tumorigenesis. Biomedicine 6, 1–8. doi: 10.7603/s40681-016-0001-9
Chen, H. X., Lai, C. H., Hsu, H. Y., Huang, J. C., Wu, H. S., Ho, M. W., et al. (2015). The bacterial interactions in the nasopharynx of children receiving adenoidectomy. Biomedicine 5, 39–43. doi: 10.7603/s40681-015-0006-9
Chen, H. Y., Lin, C. L., Lai, S. W., and Kao, C. H. (2016). Association of selective serotonin reuptake inhibitor use and acute angle-closure glaucoma. J. Clin. Psychiatry 77:e692-6. doi: 10.4088/JCP.15m10038
Chen, S. Y., Hsu, Y. M., Lin, Y. J., Huang, Y. C., Chen, C. J., Lin, W. D., et al. (2016). Current concepts regarding developmental mechanisms in diabetic retinopathy in Taiwan. Biomedicine 6:7. doi: 10.7603/s40681-016-0007-3
Chen, Y. F., Wu, K. J., Huang, W. S., Hsieh, Y. W., Wang, Y. W., Tsai, H. Y., et al. (2016). Neuroprotection of Gueichih-Fuling-Wan on cerebral ischemia/reperfusion injury in streptozotocin-induced hyperglycemic rats via the inhibition of the cellular apoptosis pathway and neuroinflammation. Biomedicine 6, 15–23. doi: 10.7603/s40681-016-0021-5
Ho, T. F., and Chang, C. C. (2015). A promising “TRAIL” of tanshinones for cancer therapy. Biomedicine 5, 29–35. doi: 10.7603/s40681-015-0023-8
Hsiao, I. H., Cho, D. Y., and Liu, C. L. (2015). Multifocal osteolytic lesions of the skull: a primary cavernous hemangioma mimicking a neoplastic invasive lesion. Biomedicine 5, 39–41. doi: 10.7603/s40681-015-0012-y
Hsieh, T. C., Wu, Y. C., Sun, S. S., Yen, K. Y., and Kao, C. H. (2016). Treating hepatocellular carcinoma with 90Y-bearing microspheres: a review. Biomedicine 6:19. doi: 10.7603/s40681-016-0019-z
Hsu, Y. M., and Yin, M. C. (2016). EPA or DHA enhanced oxidative stress and aging protein expression in brain of d-galactose treated mice. Biomedicine 6, 23–30. doi: 10.7603/s40681-016-0017-1
Huang, Y. F., Liang, J., and Shyu, Y. L. (2016). Number of comorbidities negatively influence psychological outcomes of the elderly following hip fracture in Taiwan. J. Aging Health 28, 1343–1361. doi: 10.1177/0898264315618922
Huang, Y. P., and Chang, N. W. (2016). PPARalpha modulates gene expression profiles of mitochondrial energy metabolism in oral tumorigenesis. Biomedicine 6, 17–22. doi: 10.7603/s40681-016-0003-7
Hung, C. C., and Ku, Y. W. (2015). Influencing and moderating factors analyzed in the group art therapy of two schizophrenic inpatients. Biomedicine 5, 36–38. doi: 10.7603/s40681-015-0024-7
Hung, L. W., Tseng, W. J., Huang, G. S., and Lin, J. (2014). High short-term and long-term excess mortality in geriatric patients after hip fracture: a prospective cohort study in Taiwan. BMC Musculoskelet. Disord. 15:151. doi: 10.1186/1471-2474-15-151
Hung, S. C., Lin, C. H., Hung, H. C., Lin, C. L., and Lai, S. W. (2017). Use of selective serotonin reuptake inhibitors and risk of hip fracture in the elderly: a case-control study in Taiwan. J. Am. Med. Dir. Assoc. 18, 350–354. doi: 10.1016/j.jamda.2016.12.003
Kanis, J. A., Johansson, H., Oden, A., Johnell, O., de Laet, C., Melton, I. L., et al. (2004). A meta-analysis of prior corticosteroid use and fracture risk. J. Bone Miner. Res. 19, 893–899. doi: 10.1359/JBMR.040134
Kuo, S. C., Lai, S. W., Hung, H. C., Muo, C. H., Hung, S. C., Liu, L. L., et al. (2015). Association between comorbidities and dementia in diabetes mellitus patients: population-based retrospective cohort study. J. Diabetes Complicat. 29, 1071–1076. doi: 10.1016/j.jdiacomp.2015.06.010
Lai, S. W., Lai, H. C., Lin, C. L., and Liao, K. F. (2015a). Finasteride use and acute pancreatitis in Taiwan. J. Clin. Pharmacol. 55, 657–660. doi: 10.1002/jcph.462
Lai, S. W., Lin, C. L., Chen, W. C., and Liao, K. F. (2015b). Correlation between use of zopiclone and risk of hip fracture in elderly adults: a case-control study in Taiwan. J. Am. Geriatr. Soc. 63, 2534–2537. doi: 10.1111/jgs.13823
Lai, S.-W., Lin, C.-L., and Liao, K.-F. (2015c). Increased risk of hip fracture in diabetic elderly. Kuwait Med. J. 47, 115–117.
Lai, S. W., Lin, C. L., Liao, K. F., and Chang-Ou, K. C. (2015d). Increased risk of Parkinson’s disease in cataract patients: a population-based cohort study. Parkinsonism. Relat. Disord. 21, 68–71. doi: 10.1016/j.parkreldis.2014.11.005
Lai, S. W., Liao, K. F., Liao, C. C., Muo, C. H., Liu, C. S., and Sung, F. C. (2010). Polypharmacy correlates with increased risk for hip fracture in the elderly: a population-based study. Medicine 89, 295–299. doi: 10.1097/MD.0b013e3181f15efc
Lai, S. W., Lin, C. H., Lin, H. F., Lin, C. L., Lin, C. C., and Liao, K. F. (2017a). Herpes zoster correlates with increased risk of Parkinson’s disease in older people: a population-based cohort study in Taiwan. Medicine 96:e6075. doi: 10.1097/MD.0000000000006075
Lai, S. W., Lin, C. L., and Liao, K. F. (2017b). Glaucoma correlates with increased risk of Parkinson’s disease in the elderly: a national-based cohort study in Taiwan. Curr. Med. Res. Opin. 33, 1511–1516. doi: 10.1080/03007995.2017.1322570
Lai, S. W., Lin, C. L., and Liao, K. F. (2017c). Nation-based case-control study investigating the relationship between oral corticosteroids use and pulmonary tuberculosis. Eur. J. Intern. Med. doi: 10.1016/j.ejim.2017.05.020 [Epub ahead of print].
Lai, S. W., Lin, C. L., and Liao, K. F. (2016). Use of methimazole and risk of acute pancreatitis: a case-control study in Taiwan. Indian J. Pharmacol. 48, 192–195. doi: 10.4103/0253-7613.178841
Liao, K. F., Cheng, K. C., Lin, C. L., and Lai, S. W. (2017a). Etodolac and the risk of acute pancreatitis. Biomedicine 7, 25–29. doi: 10.1051/bmdcn/2017070104
Liao, K. F., Huang, P. T., Lin, C. C., Lin, C. L., and Lai, S. W. (2017b). Fluvastatin use and risk of acute pancreatitis: a population-based case-control study in Taiwan. Biomedicine 7, 24–28. doi: 10.1051/bmdcn/2017070317
Lin, H.-F., Lai, S.-W., Liao, K.-F., Muo, C.-H., and Hsieh, D. P. H. (2013). Synergistic interaction between alcoholism and polypharmacy on the risk of falls in the elderly. Int. J. Gerontol. 7, 122–123. doi: 10.1016/j.ijge.2012.07.010
Lin, W. C., and Lin, C. H. (2016). Multidetector computed tomography in the evaluation of pediatric acute abdominal pain in the emergency department. Biomedicine 6, 20–24. doi: 10.7603/s40681-016-0010-8
Maa, M. C., and Leu, T. H. (2016). Src is required for migration, phagocytosis, and interferon beta production in Toll-like receptor-engaged macrophages. Biomedicine 6, 5–9. doi: 10.7603/s40681-016-0014-4
Mohd-Tahir, N. A., and Li, S. C. (2017). Economic burden of osteoporosis-related hip fracture in Asia: a systematic review. Osteoporos. Int. 28, 2035–2044. doi: 10.1007/s00198-017-3985-4
National Health Insurance Research Database (2017). National Health Insurance Research Database. Available at: http://nhird.nhri.org.tw/en/index.html
Ooi, H. (2016). Bedside pleuroscopy in Taiwan: a great vision for critically-ill patients and intensivists. Biomedicine 6:13. doi: 10.7603/s40681-016-0013-5
Shen, M. L., Liao, K. F., Tsai, S. M., Lin, C. L., and Lai, S. W. (2016). Herpes zoster correlates with pyogenic liver abscesses in Taiwan. Biomedicine 6, 24–29. doi: 10.7603/s40681-016-0022-4
Shiga, T., Tsuji, Y., Fujioka, M., and Kubo, T. (2009). Risk factors for hip fracture in Japanese elderly women with osteoporosis: applicability of biochemical markers in bone turnover. Geriatr. Gerontol. Int. 9, 69–74. doi: 10.1111/j.1447-0594.2008.00510.x
Steinbuch, M., Youket, T. E., and Cohen, S. (2004). Oral glucocorticoid use is associated with an increased risk of fracture. Osteoporos. Int. 15, 323–328. doi: 10.1007/s00198-003-1548-3
Tsai, T. Y., Lin, C. C., Peng, C. Y., Huang, W. H., Su, W. P., Lai, S. W., et al. (2016). The association between biliary tract inflammation and risk of digestive system cancers: a population-based cohort study. Medicine 95:e4427. doi: 10.1097/MD.0000000000004427
Van Staa, T. P., Leufkens, H. G., Abenhaim, L., Zhang, B., and Cooper, C. (2000). Use of oral corticosteroids, and risk of fractures. J. Bone Miner. Res. 15, 993–1000. doi: 10.1359/jbmr.2000.15.6.993
Van Staa, T. P., Leufkens, H. G., and Cooper, C. (2002). The epidemiology of corticosteroid-induced osteoporosis: a meta-analysis. Osteoporos. Int. 13, 777–787. doi: 10.1007/s001980200108
Vestergaard, P., Olsen, M. L., Paaske Johnsen, S., Rejnmark, L., Sorensen, H. T., and Mosekilde, L. (2003). Corticosteroid use and risk of hip fracture: a population-based case-control study in Denmark. J. Intern. Med. 254, 486–493. doi: 10.1046/j.1365-2796.2003.01219.x
Yang, S. P., Muo, C. H., Wang, I. K., Chang, Y. J., Lai, S. W., Lee, C. W., et al. (2015). Risk of type 2 diabetes mellitus in female breast cancer patients treated with morphine: a retrospective population-based time-dependent cohort study. Diabetes. Res. Clin. Pract. 110, 285–290. doi: 10.1016/j.diabres.2015.10.005
Keywords: elderly, hip fracture, oral corticosteroids
Citation: Lai S-W, Lin C-L and Liao K-F (2017) Use of Oral Corticosteroids and Risk of Hip Fracture in the Elderly in a Case-Control Study. Front. Pharmacol. 8:625. doi: 10.3389/fphar.2017.00625
Received: 05 July 2017; Accepted: 25 August 2017;
Published: 11 September 2017.
Edited by:
Jean-Paul Deslypere, Proclin Therapeutic Research Pte. Ltd., SingaporeReviewed by:
Robert L. Lins, BVBA DR LINS, BelgiumSandor Kerpel-Fronius, Department of Pharmacology and Pharmacotherapy, Semmelweis University, Hungary
Copyright © 2017 Lai, Lin and Liao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kuan-Fu Liao, kuanfuliaog@gmail.com
 Shih-Wei Lai
Shih-Wei Lai Cheng-Li Lin
Cheng-Li Lin Kuan-Fu Liao
Kuan-Fu Liao