- 1Division of Pharmacogenomics and Personalized Medicine, Department of Pathology, Faculty of Medicine, Ramathibodi Hospital, Mahidol University, Bangkok, Thailand
- 2Laboratory for Pharmacogenomics, Somdech Phra Debaratana Medical Center, Ramathibodi Hospital, Mahidol University, Bangkok, Thailand
- 3Manarom Hospital, Bangkok, Thailand
- 4Department of Pharmacology, Faculty of Medicine, Khon Kaen University, Khon Kaen, Thailand
- 5Division of Allergy and Clinical Immunology, Skin and Allergy Research Unit, Department of Medicine, Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand
- 6Division of Allergy Immunology and Rheumatology, Department of Medicine, Faculty of Medicine, Ramathibodi Hospital, Mahidol University, Bangkok, Thailand
- 7Pediatric Neurology Unit, Department of Pediatrics, Faculty of Medicine, Prince of Songkla University, Songkhla, Thailand
- 8Division of Pediatric Dermatology, Department of Pediatrics, Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand
- 9Division of Neurosurgery, Department of Surgery, King Chulalongkorn Memorial Hospital, Bangkok, Thailand
- 10Division of Neurology, Department of Pediatrics, Faculty of Medicine, Ramathibodi Hospital, Mahidol University, Bangkok, Thailand
- 11Ramathibodi Multidisciplinary Epilepsy Center, Faculty of Medicine, Ramathibodi Hospital, Mahidol University, Bangkok, Thailand
Background: Lamotrigine (LTG) is commonly used for treatment of epilepsy and bipolar disorder. It is one of the common cause of cutaneous adverse drug reactions (CADR). Clinical symptoms of LTG-induced CADR range from maculopapular exanthema (MPE) to severe cutaneous adverse reactions (SCAR). This study aimed to determine the association of the LTG-induced CADR with human leukocyte antigen (HLA) alleles in Thai patients.
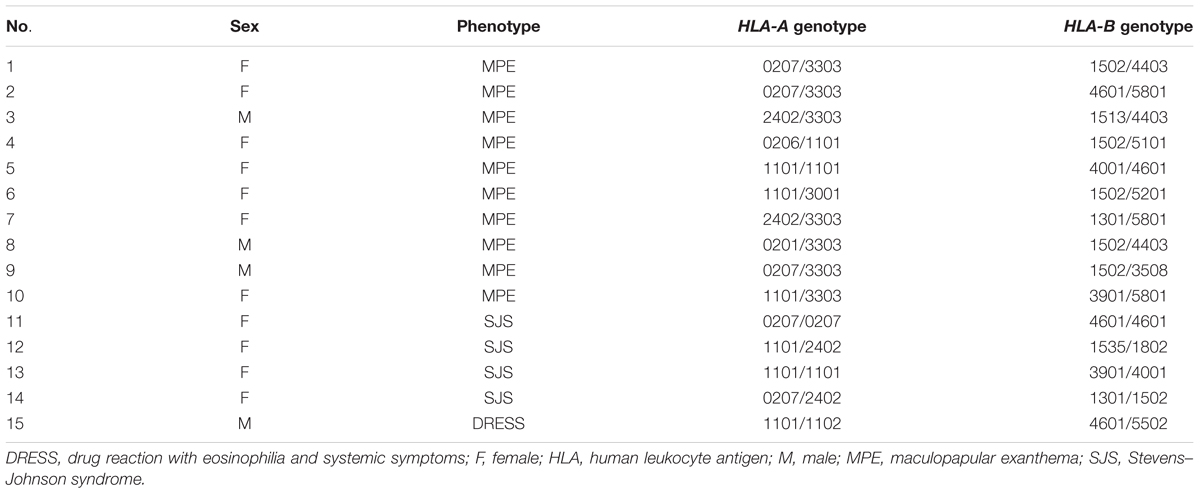
Methods: Fifteen patients with LTG-induced CADR [10 MPE; 4 Stevens–Johnson syndrome; and 1 drug reaction with eosinophilia and systemic symptoms] and 50 LTG-tolerant controls were included in the study. HLA-A and HLA-B genotyping was performed using polymerase chain reaction-sequence-specific oligonucleotides probes.
Results: The proportion of HLA-A∗02:07 and HLA-B∗15:02 allele carriers were significantly higher in the LTG-induced CADR group than in the tolerant controls [odds ratio (OR): 7.83; 95% confidence interval (CI): 1.60–38.25; P = 0.013, and OR: 4.89; 95% CI: 1.28–18.67; P = 0.014]. In addition, subjects with HLA-A∗33:03, HLA-B∗15:02, and HLA-B∗44:03 were significantly higher in the LTG-induced MPE group than in the tolerant controls (OR: 8.27; 95% CI: 1.83–37.41; P = 0.005, OR: 7.33; 95% CI: 1.63–33.02; P = 0.005; and OR: 10.29; 95% CI: 1.45–72.81; P = 0.029). In contrast to the LTG-induced MPE group, there were no significant differences between HLA alleles and LTG-induced SCAR group.
Conclusion: HLA-A∗02:07 and HLA-B∗15:02 were associated with LTG-induced CADR in Thai patients. We also identified an association between HLA-A∗33:03, HLA-B∗15:02, and HLA-B∗44:03 and LTG-induced MPE in this population. These results suggest that these alleles could be useful screening markers for preventing CADR before LTG treatment in Thai patients, but further replication studies with larger sample sizes are needed.
Introduction
Lamotrigine (LTG) is a phenyltriazine derivative which is used in the treatment of epilepsy and bipolar disorder. It is one of the aromatic antiepileptic drugs (AEDs) which together are the most common cause of cutaneous adverse reactions (CADR) (Arif et al., 2007). The current widely used AEDs include carbamazepine (CBZ), oxcarbazepine (OXC), phenytoin (PHT), and phenobarbital (PB) (Maggs et al., 2000; Arif et al., 2007; Chung et al., 2010). CADR manifestations range from mild maculopapular exanthema (MPE) to severe cutaneous adverse reactions (SCAR), including Stevens–Johnson syndrome (SJS), toxic epidermal necrolysis (TEN), and drug reactions with eosinophilia and systemic symptoms (DRESS). The mortality rates are 1–5% of patients with AED-induced SJS and up to 30% in AED-induced TEN (Roujeau and Stern, 1994; Harr and French, 2010; Yang et al., 2011). The incidences of SJS and TEN range between 1 and 10 cases per 10,000 patients (Mockenhaupt et al., 2005).
Pharmacogenetic studies have identified genetic associations between the human leukocyte antigen (HLA) allele and AEDs-induced CADR. According to specific AEDs medication, AEDs-induced SJS/TEN has been associated with specific HLA alleles in various populations, namely HLA-B∗15:02 and CBZ in the Han Chinese and Thai populations (Chung et al., 2004; Lim et al., 2008; Locharernkul et al., 2008; Tassaneeyakul et al., 2010) but not in the Japanese (Kaniwa et al., 2008) and European population (Alfirevic et al., 2006), HLA-B∗15:02 and OXC in Chinese and Thai populations (Chen et al., 2017). LTG is the most common AED used in Thailand. It has a similar chemical structure to CBZ, and high cross-reactivity rates of skin reaction from the group of AEDs in Han Chinese epilepsy patients have been reported (Greenwood, 2000; Maggs et al., 2000; Wang et al., 2010). LTG-induced SJS/TEN has been associated with HLA-B∗44:03 in Korean patients but no association was found with HLA-B∗15:02 (An et al., 2010; Hung et al., 2010; Shi et al., 2011; Park et al., 2015). In addition, HLA-A∗30:01 and HLA-B∗13:02 have been associated with a higher risk of LTG-induced MPE in Han Chinese (Li et al., 2013). However, there are no specific HLA alleles associated with LTG-induced CADR and an association between LTG-induced CADR and HLA alleles in Thailand has not been identified. Therefore, we aimed to examine the association between HLA-A and HLA-B and LTG-induced CADR in the Thai population.
Materials and Methods
Subjects
A case–control study was performed at the Laboratory for Pharmacogenomics, Somdech Phra Debaratana Medical Center (SDMC), Ramathibodi Hospital, Thailand. Fifteen LTG-induced CADR (4 cases of SJS, 1 case of DRESS, and 10 cases of MPE) were recruited from the Faculty of Medicine, Ramathibodi Hospital, Mahidol University, Manarom Hospital, and Srinagarind Hospital between 2011 and 2015. All patients who developed CADR, as SJS, MPE, or DRESS, within 2 months after initiating LTG treatment were recruited for the study. The dermatological diagnosis was made by a dermatologist or allergist who reviewed photographs, pathological slides, clinical morphology, and medical records. MPE was defined as the presence of erythematous macules and papules without mucosal involvement, and in which the skin rash resolved after the drug was discontinued. The RegiSCAR criteria were used to establish SJS and DRESS. SJS was defined as skin detachment of BSA <10%, and TEN as skin detachment of BSA >30%. DRESS was defined as presenting with fever, maculopapular rash with internal organ involvement, and hematologic abnormalities. Patients who had been taking LTG for more than 6 months without evidence of cutaneous adverse effects were recruited as LTG-tolerant controls. In addition, the general population who had not taken LTG and had no history of drug-induced CADR were included in this study. Both case and control subjects were independently recruited with no family relationship. Data for this general control group were obtained from 369 and 986 subjects undergoing HLA-A and -B genotyping, respectively.
The study was approved by the Ramathibodi Hospital Ethical Review Board, and informed, written consent was obtained from all participants.
HLA Genotyping
Genomic DNA samples were extracted from EDTA blood using a MagNA pure compact Nucleic Acid Isolation Kit on a MagNApure Compact machine. HLA alleles were genotyped using polymerase chain reaction-sequence-specific oligonucleotides (PCR-SSOs) according to the manufacturer’s protocol. In brief, diluted DNA samples were amplified by PCR using a GeneAmp®PCR System 9700 (Applied Biosystems, Waltham, MA, United States). The PCR products were then hybridized against a panel of oligonucleotide probes on coated polystyrene microspheres that had sequences complementary to stretches of polymorphisms within the target HLA-A, B alleles (a LABType®SSO, One Lambda Inc. Kit). The amplicon–probe complex was visualized using a colorimetric reaction and fluorescence detection technology (Luminex®IS 100). Data analysis for the HLA assays was performed with the software package HLA fusion 2.0.
Statistical Analysis
Statistical analyses were performed using SPSS for Windows (version 16.0; SPSS, Chicago, IL, United States). Means and standard deviations were calculated for continuous variables. Dosages of LTG intake were described as median and interquartile range (IQR). To detect differences in the clinical characteristics between the case and control groups, an independent t-test was used for continuous variables. Chi-square test and Fisher’s exact test were used to describe the differences in frequencies of the HLA-A, B alleles between the groups. Haplotype association analysis was carried out using the “haplo.stats” package. The level of statistical significance was set at p < 0.05 (two-sided).
Results
Patients and Characteristics
DNA samples from 15 LTG-induced CADR patients (10 cases with MPE, 4 cases with SJS, and 1 case with DRESS) and 50 LTG-tolerant controls and the general population group were genotyped. The mean age of the LTG-induced CADR patients was 35.2 ± 22.1 and 73.3% were female. The median LTG dosage was 50 mg per day. There were no significant differences in gender, age, dosage of LTG, and concomitant use of valproic acid between the LTG-induced CADR patients and the LTG-tolerant patients (Table 1).
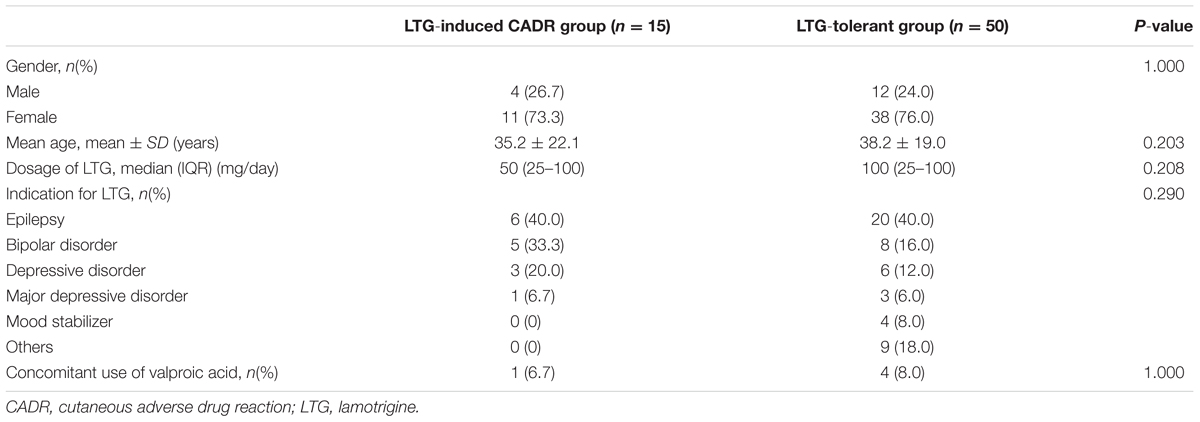
TABLE 1. Clinical characteristics of patients in the lamotrigine (LTG)-induced cutaneous adverse drug reactions group and the LTG-tolerant group.
The HLA Allele and LTG-Induced CADR
The HLA-A and HLA-B genotypes of the LTG-induced CADR patients are shown in Table 2. The HLA genotypes for the treatment tolerant controls and the comparison of the HLA allele found in the CADR patients and control groups (LTG-tolerant controls and general population) are shown in Supplementary Tables 1, 2. The HLA alleles that showed a significant association when compared with the tolerant controls and general population are presented in Table 3. We found the HLA-B∗15:02 allele in 40.0% of patients who developed CADR and in 12.0% of the tolerant patients. The proportion of patients carrying the HLA-B∗15:02 allele was significantly higher in LTG-induced CADR cases than in both the treatment controls and general population groups with odds ratios (OR) of 4.89, 95% CI = 1.28–18.66, P-value = 0.014 and OR = 3.63, 95% CI = 1.27–10.34, P-value = 0.027, respectively. In addition, we also found a significant association between LTG-induced CADR patients and both HLA-B∗35:08 and HLA-B∗39:01 when compared with the general population with OR = 70.36, 95% CI = 4.19–1182.21, P-value = 0.030 and OR = 10.68, 95% CI = 2.20–51.83, P-value = 0.022, respectively.
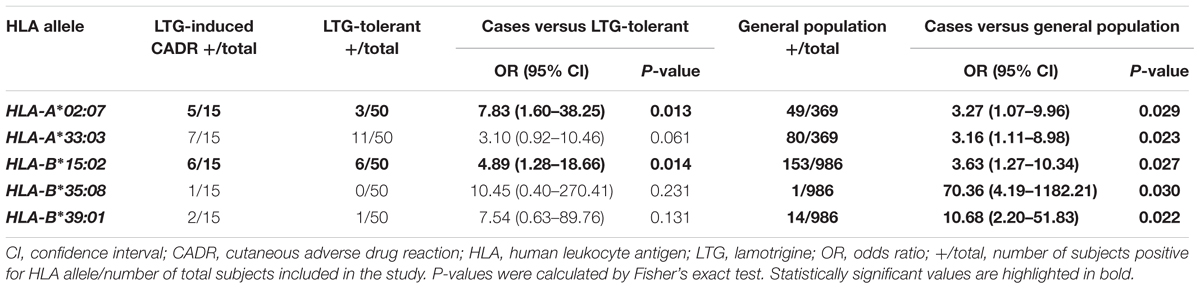
TABLE 3. List of HLA alleles that showed a significant association with LTG-induced cutaneous adverse drug reactions.
In subgroup analysis of LTG-induced CADR, a significant association between LTG-induced MPE and HLA-B∗15:02 was found when compared with the tolerant controls and general population (OR = 7.33, 95% CI = 1.63–33.02, P-value = 0.005 and OR = 5.44, 95% CI = 1.56–19.03, P-value = 0.003, respectively). Interestingly, a significant association between LTG-induced MPE and HLA-B∗44:03 was found when compared with both control groups (OR = 10.29, 95% CI = 1.45–72.81, P-value = 0.029 and OR = 4.73, 95% CI = 1.20–18.62, P-value = 0.046, respectively), whereas HLA-B∗35:08 was significantly associated only with the general population (OR = 109.44, 95% CI = 6.34–1889.11, P-value = 0.020) (Table 4); nevertheless, no significant associations were found in LTG-induced SCAR.
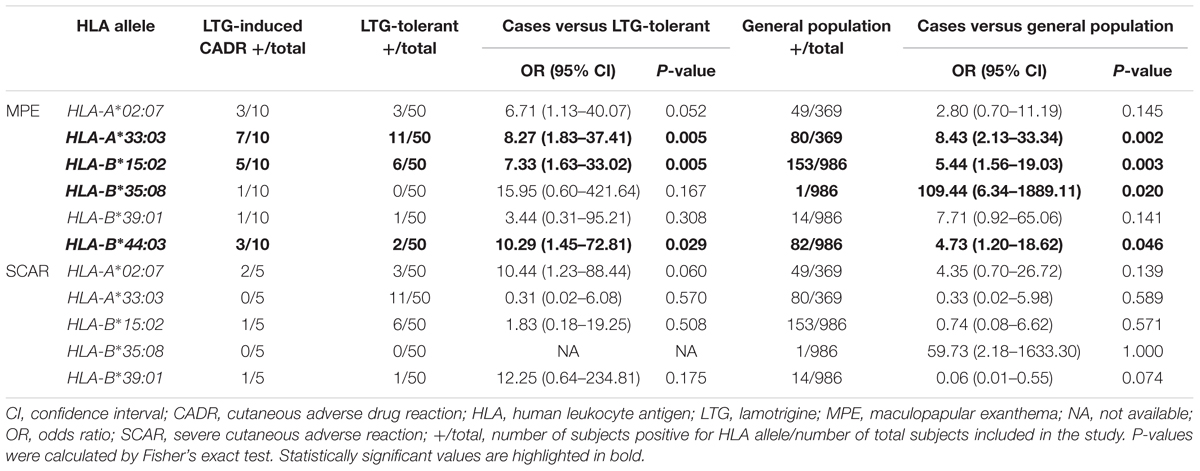
TABLE 4. The associations of individual HLA alleles with LTG-induced cutaneous adverse drug reactions among the different subgroups.
Compared with the HLA-B allele, HLA-A∗02:07 was present in 33.3% of LTG-induced CADR patients and showed significantly higher frequencies than both the treatment control and general population groups with OR = 7.83, 95% CI = 1.60–38.25, P-value = 0.013 and OR = 3.27, 95% CI = 1.07–9.96, P-value = 0.029, respectively; in addition, HLA-A∗33:03 also had a significantly higher frequency than in the general population (OR = 3.16, 95% CI = 1.11–8.98, P-value = 0.023). Moreover, we found a significant association of LTG-induced MPE with HLA-A∗33:03 compared with the tolerant controls group (OR = 8.27, 95% CI = 1.83–37.41, P-value = 0.005) and general population group (OR = 8.43, 95% CI = 2.13–33.34, P-value = 0.002) as shown in Table 4.
The analysis of HLA-A and HLA-B haplotypes have demonstrated that the HLA-A∗02:07/HLA-B∗15:02 and HLA-A∗33:03/HLA-B∗15:02 haplotypes were not found to be associated with LTG-induced CADR (data not shown).
Discussion
In the present study, we found the significant association between LTG-induced CADR and HLA-A∗02:07 and HLA-B∗15:02 when compared with both tolerant and general population controls. In addition, the HLA-A∗33:03 allele was present at a significantly higher rate in LTG-induced CADR patients than in the general population controls. These results suggest that HLA-B∗15:02, alone, might not be the only risk factor for LTG-induced CADR, but HLA-A∗02:07 and HLA-A∗33:03 may also be risk factors for LTG-induced CADR. The subgroup analysis revealed that the proportion of patients carrying the HLA-B∗15:02 allele was significantly higher in LTG-induced MPE cases than in both the tolerant control and general population groups, which is very different from previous studies in which HLA-B∗15:02 was not found to be associated with LTG-induced MPE (An et al., 2010; Shi et al., 2011). We demonstrated that HLA-A∗33:03 may be a risk factors for LTG-induced MPE, which again is different from the findings of a previous study in the Han Chinese population which found that patients carrying HLA-A∗33:03 had a lower risk for LTG-induced MPE (Li et al., 2013). The same study also found that patients carrying either of the HLA-A∗30:01 or HLA-B∗13:02 alleles had increased risk for LTG-induced MPE (Li et al., 2013). In this study, we did not find a significant association between HLA-A∗30:01 or HLA-B∗13:02 and LTG-induced MPE. One study found the HLA-A∗30:01 allele in 1 of 10 LTG-induced MPE patients, while HLA-B∗13:02 was absent in the same 10 LTG-induced MPE patients, which the authors suggested could be because of the low frequency of HLA-B∗13:02 (1.4%) in the Thai population (Puangpetch et al., 2015).
Conversely, no significant association between LTG-induced SCAR and HLA-B∗15:02 was found when compared with the two control groups, nor did we find significant differences in the other HLA alleles between the LTG-induced SCAR group and the two control groups. Earlier studies on CBZ-induced SJS/TEN and the HLA-B∗15:02 allele reported no associations with the MPE group (Chung et al., 2004; Hung et al., 2006). The chemical structure of LTG includes aromatic rings similar to CBZ and shared a common risk allele causing SJS/TEN which similarities with other aromatic AEDs, namely PHT and OXC (Hung et al., 2010). Previous studies have found an association between LTG-induced SJS/TEN and HLA-B∗15:02 in Han Chinese (An et al., 2010; Hung et al., 2010), but other studies have found no association in Japanese patients (Kaniwa et al., 2008) or European population (Alfirevic et al., 2006), due to the fact that the HLA-B∗15:02 allele is rare in the Japanese population (0.1%) and people of European descent (0%), according to data from Lee et al. (2010). However, data from all of these studies were limited due to the small sample sizes of LTG-induced SJS patients; therefore, association studies between the HLA genotype and LTG-induced SJS could not be performed.
In this study, we report for the first time a significant association between HLA-B∗35:08 and LTG-induced CADR or MPE, although this allele has been reported in only one case of LTG-induced MPE and once in the general population, as a result of this allele being very rare in the Thai population (less than 1%, data from Puangpetch et al., 2015). The interpretation of data from studies with a small sample size can only be tentative, and further investigations with larger sample sizes are needed. Similarly to HLA-B∗35:08, the association of LTG-induced MPE and HLA-B∗44:03 alleles was firstly reported in the Thai population. One recent study from Korea found that HLA-B∗44:03 was associated with LTG-induced SJS/TEN (OR: 12.75, 95% CI: 1.03–157.14, and P-value = 0.053) (Park et al., 2016).
One study found that LTG-induced CADR in the Japanese population was associated with HLA class II alleles, including HLA-DRB1∗04:05, HLA-DQB1∗04:01, and HLA-DQA1∗03:03 (Ito et al., 2015), but HLA class II genotyping was not performed in this current study. However, it would be interesting to investigate the association of HLA class II and LTG-induced CADR in each population and with a large number of patients to better understand any association. Nevertheless, previous studies identified age and concomitant use of LTG and valproic acid as risk factors for LTG-induced CADR (Cheung et al., 2013; Egunsola et al., 2015). However, in our study we did not find that age and concomitant therapy with valproic acid were risk factors for LTG-induced CADR.
Apart from the HLA alleles, drug-metabolizing enzymes may be a risk factor for developing CADR. LTG is primarily metabolized by uridine diphosphate glucuronosyltransferases (UGT), including UGT1A4 and UGT2B7 (Perucca, 2006). 2-N-Glucuronide conjugates are the major inactive metabolite of LTG and elimination from the body by any enzyme variant either than one of these UGT enzymes will affect the risk of cutaneous adverse drug reactions (Rowland et al., 2006). A recent study on drug metabolizing enzymes found that the cytochrome P4502C9 (CYP2C9) influenced PHT-induced SCAR in the Thai population (Tassaneeyakul et al., 2016). Further association studies are required to determine the association between the glucuronidation metabolic pathway and LTG-induced CADR.
Conclusion
We found a statistically significant association of the HLA-A∗02:07 and HLA-B∗15:02 alleles with LTG-induced CADR in the Thai population. Therefore, these two alleles might be potential risk markers for LTG-induced CADR in Thailand. To confirm these findings, further large-scale studies are required.
Ethics Statement
The project has been reviewed and approved by the Committee on Human Right Related to Research Involving Human Subjects, based on the Declaration of Helsinki (MURA2012/307/S2, June 16).
Author Contributions
CS, WT, and NK designed the research study. TR, TT, and JK diagnosed and recruited the subjects. VT, AP, and TD collected the clinical data; NK, TJ, SS, UI, and AV performed genotyping and evaluated the results. JP and PS analyzed the data. CS, JP, and PS wrote the manuscript. CS and AP reviewed and edited the manuscript.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The reviewer ZR-P and handling editor declared their shared affiliation.
Acknowledgments
This study was supported by grants from (1) the Faculty of Medicine, Ramathibodi Hospital, Mahidol University, (2) the THAI-SCAR project: WCU-002-HR-57, Chulalongkorn University, and (3) the Royal Golden Jubilee Ph.D. (RGJ-PHD) Program: PHD/0153/2559.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2017.00879/full#supplementary-material
References
Alfirevic, A., Jorgensen, A. L., Williamson, P. R., Chadwick, D. W., Park, B. K., and Pirmohamed, M. (2006). HLA-B locus in Caucasian patients with carbamazepine hypersensitivity. Pharmacogenomics 7, 813–818. doi: 10.2217/14622416.7.6.813
An, D. M., Wu, X. T., Hu, F. Y., Yan, B., Stefan, H., and Zhou, D. (2010). Association study of lamotrigine-induced cutaneous adverse reactions and HLA-B∗1502 in a Han Chinese population. Epilepsy Res. 92, 226–230. doi: 10.1016/j.eplepsyres.2010.10.006
Arif, H., Buchsbaum, R., Weintraub, D., Koyfman, S., Salas-Humara, C., Bazil, C. W., et al. (2007). Comparison and predictors of rash associated with 15 antiepileptic drugs. Neurology 68, 1701–1709. doi: 10.1212/01.wnl.0000261917.83337.db
Chen, C. B., Hsiao, Y. H., Wu, T., Hsih, M. S., Tassaneeyakul, W., Jorns, T. P., et al. (2017). Risk and association of HLA with oxcarbazepine-induced cutaneous adverse reactions in Asians. Neurology 88, 78–86. doi: 10.1212/WNL.0000000000003453
Cheung, Y. K., Cheng, S. H., Chan, E. J., Lo, S. V., Ng, M. H., and Kwan, P. (2013). HLA-B alleles associated with severe cutaneous reactions to antiepileptic drugs in Han Chinese. Epilepsia 54, 1307–1314. doi: 10.1111/epi.12217
Chung, W. H., Hung, S. I., and Chen, Y. T. (2010). Genetic predisposition of life-threatening antiepileptic-induced skin reactions. Expert Opin. Drug Saf. 9, 15–21. doi: 10.1517/14740330903427969
Chung, W. H., Hung, S. I., Hong, H. S., Hsih, M. S., Yang, L. C., Ho, H. C., et al. (2004). Medical genetics: a marker for Stevens–Johnson syndrome. Nature 428:486. doi: 10.1038/428486a
Egunsola, O., Choonara, I., and Sammons, H. M. (2015). Safety of lamotrigine in paediatrics: a systematic review. BMJ Open 5:e007711. doi: 10.1136/bmjopen-2015-007711
Greenwood, R. S. (2000). Adverse effects of antiepileptic drugs. Epilepsia 41, S42–S52. doi: 10.1111/j.1528-1157.2000.tb01523.x
Harr, T., and French, L. E. (2010). Toxic epidermal necrolysis and Stevens-Johnson syndrome. Orphanet J. Rare Dis. 5:39. doi: 10.1186/1750-1172-5-39
Hung, S. I., Chung, W. H., Jee, S. H., Chen, W. C., Chang, Y. T., Lee, W. R., et al. (2006). Genetic susceptibility to carbamazepine-induced cutaneous adverse drug reactions. Pharmacogenet. Genomics 16, 297–306. doi: 10.1097/01.fpc.0000199500.46842.4a
Hung, S. I., Chung, W. H., Liu, Z. S., Chen, C. H., Hsih, M. S., Hui, R. C., et al. (2010). Common risk allele in aromatic antiepileptic-drug induced Stevens-Johnson syndrome and toxic epidermal necrolysis in Han Chinese. Pharmacogenomics 11, 349–356. doi: 10.2217/pgs.09.162
Ito, A., Shimada, H., Ishikawa, K., Takeo, N., Hatano, Y., Katagiri, K., et al. (2015). Association between HLA-DRB1∗0405, -DQB1∗0401 and -DQA1∗0303 alleles and lamotrigine-induced cutaneous adverse drug reactions. A pilot case-control study from Japan. J. Affect. Disord. 179, 47–50.
Kaniwa, N., Saito, Y., Aihara, M., Matsunaga, K., Tohkin, M., Kurose, K., et al. (2008). HLA-B locus in Japanese patients with anti-epileptics and allopurinol-related Stevens-Johnson syndrome and toxic epidermal necrolysis. Pharmacogenomics 9, 1617–1622. doi: 10.2217/14622416.9.11.1617
Lee, M. T., Hung, S. I., Wei, C. Y., and Chen, Y. T. (2010). Pharmacogenetics of toxic epidermal necrolysis. Expert Opin. Pharmacother. 11, 2153–2162. doi: 10.1517/14656566.2010.495120
Li, L. J., Hu, F. Y., Wu, X. T., An, D. M., Yan, B., and Zhou, D. (2013). Predictive markers for carbamazepine and lamotrigine-induced maculopapular exanthema in Han Chinese. Epilepsy Res. 106, 296–300. doi: 10.1016/j.eplepsyres.2013.05.004
Lim, K. S., Kwan, P., and Tan, C. T. (2008). Association of HLA-B∗1502 allele and carbamazepine induced severe adverse cutaneous drug reaction among Asians, a review. Neurol. Asia 13, 15–21.
Locharernkul, C., Loplumlert, J., Limotai, C., Korkij, W., Desudchit, T., Tongkobpetch, S., et al. (2008). Carbamazepine and phenytoin induced Stevens-Johnson syndrome is associated with HLA-B∗1502 allele in Thai population. Epilepsia 49, 2087–2091. doi: 10.1111/j.1528-1167.2008.01719.x
Maggs, J. L., Naisbitt, D. J., Tettey, J. N., Pirmohamed, M., and Park, B. K. (2000). Metabolism of lamotrigine to a reactive arene oxide intermediate. Chem. Res. Toxicol. 13, 1075–1081. doi: 10.1021/tx0000825
Mockenhaupt, M., Messenheimer, J., Tennis, P., and Schlingmann, J. (2005). Risk of Stevens-Johnson syndrome and toxic epidermal necrolysis in new users of antiepileptics. Neurology 64, 1134–1138. doi: 10.1212/01.WNL.0000156354.20227.F0
Park, H. J., Kim, S. R., Leem, D. W., Moon, I. J., Koh, B. S., Park, K. H., et al. (2015). Clinical features of and genetic predisposition to drug-induced Stevens-Johnson syndrome and toxic epidermal necrolysis in a single Korean tertiary institution patients-investigating the relation between the HLA -B∗4403 allele and lamotrigine. Eur. J. Clin. Pharmacol. 71, 35–41. doi: 10.1007/s00228-014-1764-0
Park, H. J., Kim, Y. J., Kim, D. H., Kim, J., Park, K. H., Park, J. W., et al. (2016). HLA allele frequencies in 5802 Koreans: varied allele types associated with SJS/TEN according to culprit drugs. Yonsei Med. J. 57, 118–126. doi: 10.3349/ymj.2016.57.1.118
Perucca, E. (2006). Clinically relevant drug interactions with antiepileptic drugs. Br. J. Clin. Pharmacol. 61, 246–255. doi: 10.1111/j.1365-2125.2005.02529.x
Puangpetch, A., Suwannarat, P., Chamnanphol, M., Koomdee, N., Ngamsamut, N., Limsila, P., et al. (2015). Significant association of HLA-B alleles and genotypes in thai children with autism spectrum disorders: a case-control study. Dis. Markers 2015:724935. doi: 10.1155/2015/724935
Roujeau, J. C., and Stern, R. S. (1994). Severe adverse cutaneous reactions to drugs. N. Engl. J. Med. 331, 1272–1285. doi: 10.1056/NEJM199411103311906
Rowland, A., Elliot, D. J., Williams, J. A., Mackenzie, P. I., Dickinson, R. G., and Miners, J. O. (2006). In vitro characterization of lamotrigine N2-glucuronidation and the lamotrigine-valproic acid interaction. Drug Metab. Dispos. 34, 1055–1062. doi: 10.1124/dmd.106.009340
Shi, Y. W., Min, F. L., Liu, X. R., Zan, L. X., Gao, M. M., and Yu, M. J., et al. (2011). HLA-B alleles and lamotrigine-induced cutaneous adverse drug reactions in the Han Chinese population. Basic Clin. Pharmacol. Toxicol. 109, 42–46. doi: 10.1111/j.1742-7843.2011.00681.x
Tassaneeyakul, W., Prabmeechai, N., Sukasem, C., Kongpan, T., Konyoung, P., Chumworathayi, P., et al. (2016). Associations between HLA class I and cytochrome P450 2C9 genetic polymorphisms and phenytoin-related severe cutaneous adverse reactions in a Thai population. Pharmacogenet. Genomics 26, 225–234. doi: 10.1097/FPC.0000000000000211
Tassaneeyakul, W., Tiamkao, S., Jantararoungtong, T., Chen, P., Lin, S. Y., Chen, W. H., et al. (2010). Association between HLA-B∗1502 and carbamazepine-induced severe cutaneous adverse drug reactions in a Thai population. Epilepsia 51, 926–930. doi: 10.1111/j.1528-1167.2010.02533.x
Wang, X. Q., Lang, S. Y., Shi, X. B., Tian, H. J., Wang, R. F., and Yang, F. (2010). Cross-reactivity of skin rashes with current antiepileptic drugs in Chinese population. Seizure 19, 562–566. doi: 10.1016/j.seizure.2010.09.003
Keywords: lamotrigine, HLA-A, HLA-B, cutaneous adverse drug reactions, Thai population
Citation: Koomdee N, Pratoomwun J, Jantararoungtong T, Theeramoke V, Tassaneeyakul W, Klaewsongkram J, Rerkpattanapipat T, Santon S, Puangpetch A, Intusoma U, Tempark T, Deesudchit T, Satapornpong P, Visudtibhan A and Sukasem C (2017) Association of HLA-A and HLA-B Alleles with Lamotrigine-Induced Cutaneous Adverse Drug Reactions in the Thai Population. Front. Pharmacol. 8:879. doi: 10.3389/fphar.2017.00879
Received: 20 June 2017; Accepted: 13 November 2017;
Published: 29 November 2017.
Edited by:
Vita Dolzan, University of Ljubljana, SloveniaReviewed by:
Eleni Aklillu, Karolinska Institute (KI), SwedenZvonka Rener-Primec, University Children’s Hospital, University Medical Centre Ljubljana, Slovenia
Copyright © 2017 Koomdee, Pratoomwun, Jantararoungtong, Theeramoke, Tassaneeyakul, Klaewsongkram, Rerkpattanapipat, Santon, Puangpetch, Intusoma, Tempark, Deesudchit, Satapornpong, Visudtibhan and Sukasem. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chonlaphat Sukasem, chonlaphat.suk@mahidol.ac.th
†Co-first authors
 Napatrupron Koomdee
Napatrupron Koomdee Jirawat Pratoomwun
Jirawat Pratoomwun Thawinee Jantararoungtong
Thawinee Jantararoungtong Voralaksana Theeramoke3
Voralaksana Theeramoke3 Ticha Rerkpattanapipat
Ticha Rerkpattanapipat Patompong Satapornpong
Patompong Satapornpong Chonlaphat Sukasem
Chonlaphat Sukasem