- 1Department of Prosthetic Dentistry, Wroclaw Medical University, Wroclaw, Poland
- 2Department of Periodontology, Wroclaw Medical University, Wroclaw, Poland
- 3Department of Oral Surgery, Wroclaw Medical University, Wroclaw, Poland
Masticatory muscle pain (MMP) is the primary reason for chronic non-odontogenic orofacial pain in the human population. MMP has become a considerable social problem, which affects about 12–14% of the adult population and is 1.5–2 times more frequent in women than in men. This term defines a pain which has its origins in the masticatory muscles. Although MMP is typically felt in the face, jaws, and preauricular area, MMP can radiate to the ear, teeth, head, and neck. This systematic review explains the relationship between MMP and common mental states, such as anxiety, depression, mood and stress-related disorders, and is reported in accordance with PRISMA guidelines. We performed a search in the PubMed database for peer-reviewed articles published after November 1st 2006 in the context of MMP and mental states. According to the defined criteria, 38 studies were finally included into the systematic review, of which prospective cohort studies were found to be the most common. We investigated four primary outcomes (anxiety, depression, mood disorders, and stress-related disorders) and several secondary outcomes of search. Seventy-nine percent of studies concerned depression, 42% anxiety, 29% mood disorders, and 21% stress-related disorders. Most of the studies showed a relationship between MMP and alterations in mental status. Nonetheless, the researchers usually evidenced only the co-occurrence of psychiatric disorders and dysfunctions of the masticatory muscles among the group of patients, in large part in women. Moreover, some studies were marked with limited generalizability of the reported results, quality flaws and heterogeneity. In the light of the analyzed literature, the causal relationship between mental states and MMP is still not clearly established.
Introduction
A number of papers confirm that there is a correlation between pain sensitivity and mental states (Gatchel, 2004; Means-Christensen et al., 2008; Vaccarino et al., 2009; Haviland et al., 2011). Moreover, muscle pain also seems to be closely involved in this pathomechanism (Rollman and Gillespie, 2000; Haviland et al., 2011; Rees et al., 2011; Hung et al., 2016). Based on the previously cited papers (Rollman and Gillespie, 2000; Gatchel, 2004; Means-Christensen et al., 2008; Vaccarino et al., 2009; Haviland et al., 2011; Rees et al., 2011; Hung et al., 2016), this pathomechanism usually involves back, neck and orofacial muscles including masticatory muscles. Defining the onset of orofacial muscle pain related to psychoemotional status is controversial. Therefore researchers are still looking for a clear explanation of this important clinical issue (Durham et al., 2015; Glaros et al., 2016).
According to the literature, the term masticatory muscle pain (MMP) describes “the pain with origin in the masticatory muscles, including tendons and fasciae” and “is diagnosed by the presence of tenderness to palpation, e.g., of tender but not trigger points” (Gatchel, 2004). Alternatively, in the commonly applied research diagnostic criteria for temporomandibular disorders (RDC/ TMD) to define the same muscle condition, the term myofascial pain (MFP) is used. Interestingly, MFP is used to define the pain caused by trigger points (Gatchel, 2004). In our study, we consider these both symptoms of muscle pain dysfunction, i.e., related to trigger points and tenderness. MMP diagnosed based on muscle tenderness with palpation occurs in 12–14% of the examined population—there is a 1.5–2 times higher chance that women will suffer from this medical condition than men (Gatchel, 2004). Surprisingly, the prevalence of MMP in the age range 7–17 years is not higher in girls than boys (Gatchel, 2004).
The etiology and likely mechanism of muscle pain has aroused many controversies over the years. It can be associated with a peripheral mechanism of muscle pain excitation, outlasting sensitization of peripheral nociceptors, which are involved in the excitation of central neurons, and/or functional disorders (Haviland et al., 2011). However, numerous sources indicate that, regardless of the original muscle pain pathology, excessive muscle tension simultaneously appears as defensive muscle reaction, and results in increasing intensification of symptoms (Means-Christensen et al., 2008; Haviland et al., 2011). Increased muscle tension can be a local result of trauma, physiological function or dysfunction, and a defensive response to psychological burden (Means-Christensen et al., 2008; Haviland et al., 2011). The central mechanism of muscle pain development due to long-term overactivity mostly relates to those muscles which tense during psychological discomfort, anxiety, anger, and bad mood or under stress (Vaccarino et al., 2009; Haviland et al., 2011). The masseter, temporal muscle, sternocleidomastoid muscle and trapezius muscle, especially its upper part, are very good examples of mentioned central mechanism. These muscles tense in response to alterations in mental status, which may induce muscle pain related to mental disorders or chronic stress (Hung et al., 2016).
According to Okeson, the MMP can be divided into several types: protective co-contraction, local muscle soreness, MFP, myospasm (tonic contraction myalgia) and centrally mediated myalgia (Okeson, 2013). In many cases, the risk of the development of these MMP types is centrally modulated and is dependent on the mental state of the patient. Moreover, there are great similarities, and possible overlaps, between patients suffering from MMP and tension-type headache (TTH) and/or fibromyalgia (FM) (Rollman and Gillespie, 2000). A muscular pain was a cause of a headache in about 38% of adults (Rees et al., 2011).
We try to explain the relationship between MMP and psychological alterations and/or disorders such as anxiety, depression, mood and stress-related disorders, as well as systematically reviewing the current literature related to this issue and investigating it objectively.
Materials and Methods
We followed the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) guidelines for our systematic review and to collect and report data (Moher et al., 2009; Shamseer et al., 2015).
Eligibility Criteria for Initial Study Selection
Studies
We established the following inclusion criterion: clinical trials or experimental studies, which concern relationships between MMP and common mental states, such as anxiety, depression, mood disorders and stress-related disorders. Peer-reviewed, English-language and full text articles published after November 1st 2006 were included into our study. Articles which discussed the research topic only in the introduction or discussion were excluded.
Participants
Participants were males and females of any age with clinical diagnosis of MMP and/or TTH accompanied by psychological variables and/or mental disorders.
Outcomes
A study was included into this systematic review if it investigated at least one of the primary outcomes of interest: anxiety, depression, mood and stress-related disorders. Moreover, secondary outcomes such as pain, patient's quality of life, sleep disturbances, and somatization were also considered.
Data Sources and Searches
We searched the PubMed database to identify relevant publications. To make the process of searching more efficient, we added PubMed filters to find clinical trials, meta-analyzes, randomized controlled trials, and systematic reviews. Additional filters included articles published after November 1st 2006, available in English. Medical subject headings (MeSH) were used to develop a literature search strategy (Moher et al., 2009; Shamseer et al., 2015) as follows: each of three synonymous phrases, i.e., (1) masticatory muscle pain, (2) masticatory myofascial pain, and (3) myofascial pain syndrome, were combined with each mental status: (a) anxiety, (b) depression, (c) mood disorders, and (d) stress-related disorders, e.g., “masticatory muscle pain anxiety,” viz. (1)+(a); “masticatory muscle pain depression,” viz. (1)+(b); “masticatory myofascial pain mood disorders,” (2)+(c), etc. In this way, we obtained 12 queries. We also screened the reference list of included studies to trace potentially relevant papers.
Trial Selection
Three authors were involved in the literature screening procedure (MW, JS, and NG). Firstly, the titles, abstracts and full texts were screened independently by two of these authors (JS and NG). Then, the full texts of potentially suitable articles were screened for key words, such as “masticatory,” “myofascial,” “orofacial,” “facial,” “pain,” “temporomandibular,” “masseter,” “temporalis” “myogenous,” “muscle,” “anxiety,” “depression,” “stress,” and “mood,” and the articles were then evaluated for their relevance in the context of the research question. The next step of paper selection involved a final evaluation of relevance and practical validity regarding the relationship between mental status and MMP. Eventually, the three authors jointly decided whether the identified articles met the inclusion criteria. Neither of the review authors was blind to the journal title or to the study authors or institutions (Tricco et al., 2012; Shamseer et al., 2015).
Data Extraction
After the final agreed decision, two reviewers conducted data extraction independently (JS, NG). Then, the third author (MW) checked the validity of all data extracted. The extraction process included information regarding study design, sample characteristics and size, diagnostics criteria, comparison groups, outcomes and tools used to measure those outcomes.
Data Synthesis and Analysis
The studies included in our systematic review are very heterogeneous. As a consequence, performance of a meta-analysis was impossible. We conducted a “narrative, qualitative summary” as recommended (Mao et al., 2015). The quality evidence for results was assessed employing the Grading of Recommendations Assessment, Development and Evaluation working group approach (Young et al., 2012; Shamseer et al., 2015)1. The quality evidence for each outcome was assessed as one of the following categories: very low, low, moderate or high.
Results
Description of Studies
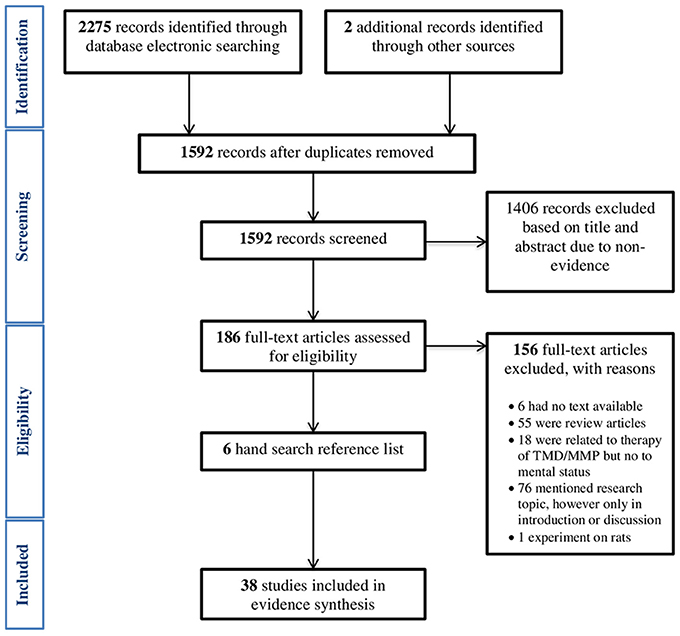
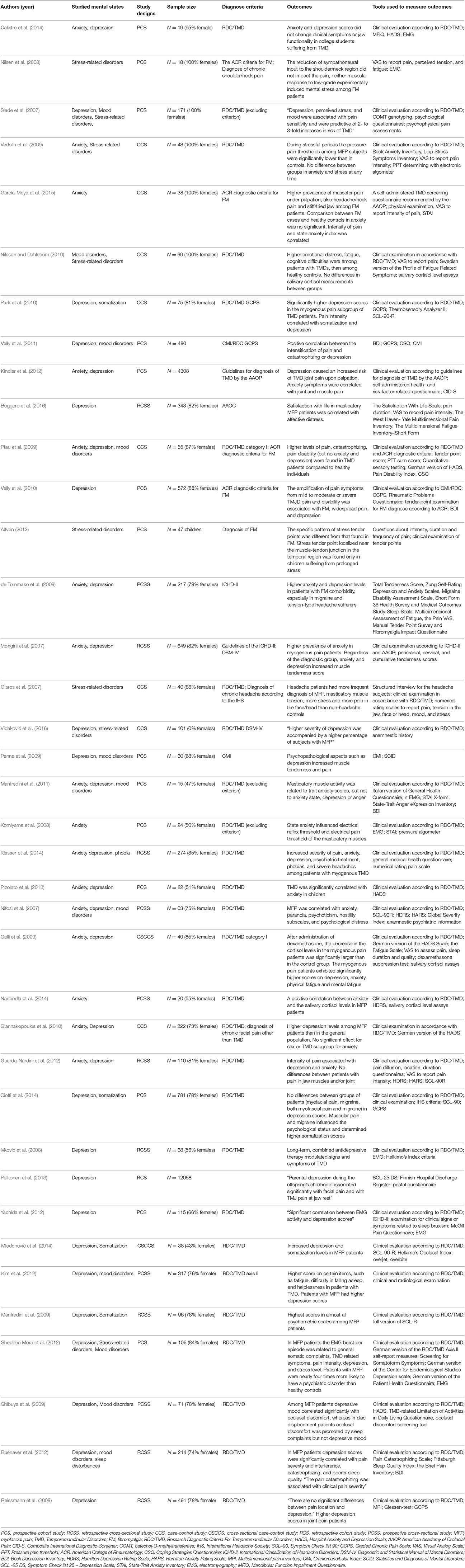
According to the above search protocol, we obtained 2,275 results from searches conducted up to and including October 2016. Thirty-nine articles were included. Although, we searched for clinical trials, meta-analyzes, randomized controlled trials, and systematic reviews, we did not find such types of studies. The main reasons for exclusion were study design (review articles and not systematic reviews), studies' relationship to the therapy of TMD (not accompanied by mental status reports), and mention of the research topic, however only in the introduction or discussion. The systematic review protocol is presented as a flow-chart in Figure 1. Most studies confirmed the relationship between MMP and at least one mental state, but there were also two studies that definitely did not support any of mentioned assertions (Nilsen et al., 2008; Calixtre et al., 2014). Qualified research in the majority of cases described the co-existence of MMP and mental disorders, but did not indicate their cause and effect relationship. The percentage contribution of the particular research designs is displayed in chart form (Figure 2). Another interesting issue to mention is that the problem was associated mainly with female gender. An overview of the content of qualifying studies is presented in Table 1.
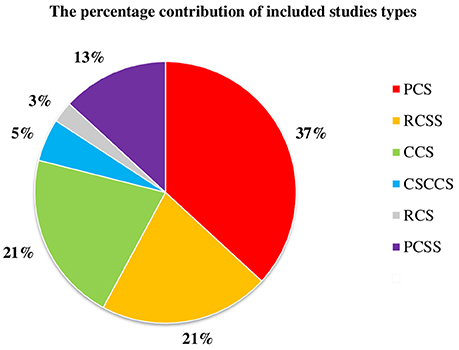
Figure 2. The percentage contribution of included studies types. PCS, prospective cohort study; RCSS, retrospective cross-sectional study; CCS, case-control study; CSCCS, cross-sectional case-control study; RCS, retrospective cohort study; PCSS, prospective cross-sectional study.
Characteristics of Subjects Included in the Primary Studies
The total number of participants included in the studies ranged from 12,058 to 18. In most studies subjects were adults, mainly females, and in five studies the sample was composed only of females. (Slade et al., 2007; Nilsen et al., 2008; Vedolin et al., 2009; Nilsson and Dahlström, 2010; García-Moya et al., 2015). In 70% of studies individuals were assessed based on RDC/TMD as a diagnostic criterion. Other diagnostic criteria were Graded Chronic Pain Scale (Park et al., 2010; Velly et al., 2011), Guideline of diagnosis of TMD by the American Academy of Orofacial Pain (Kindler et al., 2012; Boggero et al., 2016), Diagnostic Criteria for FM (Nilsen et al., 2008; Pfau et al., 2009; Velly et al., 2010; Alfvén, 2012; García-Moya et al., 2015), International Classification of Headache Disorders II (Mongini et al., 2007; de Tommaso et al., 2009), International Headache Society (Glaros et al., 2007), Diagnostic and Statistical Manual of Mental Disorders-IV (Mongini et al., 2007; Vidaković et al., 2016), Craniomandibular Index (Penna et al., 2009), and Craniomandibular Index/RDC (Velly et al., 2011). In three studies only healthy subjects were included and RDC/TMD were treated as excluding criteria (Slade et al., 2007; Komiyama et al., 2008; Manfredini et al., 2011). MMP patients examined in the included studies often suffered from other concomitant disorders, such as FM (Nilsen et al., 2008; Pfau et al., 2009; Velly et al., 2010; Alfvén, 2012; Klasser et al., 2014; García-Moya et al., 2015) and headaches (Glaros et al., 2007; Mongini et al., 2007; de Tommaso et al., 2009).
Outcome Measurement Tools
Studies differed in psychometric assessment tools. In all, about 20 different inventories were used to evaluate the mental status of studied individuals. The most common were Hospital Anxiety and Depression Scale, Symptom Check List 90/-R, Beck Depression Inventory, State-Trait Anxiety Inventory, Hamilton Depression and Anxiety Rating Scales, Symptom Check List 25—Depression Scale. Seventy-nine percent of studies concerned depression, 42% anxiety, 29% mood disorders, and 21% stress-related disorders. Other considered mental states were somatization, catastrophizing, sleep disturbances, phobia, paranoia, psychoticism, and hostility.
Quality Assessment
We finally included 38 papers, of which prospective cohort studies were found to be the most common research design. In addition, we considered prospective cohort studies to be the most reliable type of included research. However, there were also many cross-sectional studies. This type of study explores relationships occurring only at one point in time in the appropriate population; thus, no causal relationship can be established.
Evidence Synthesis
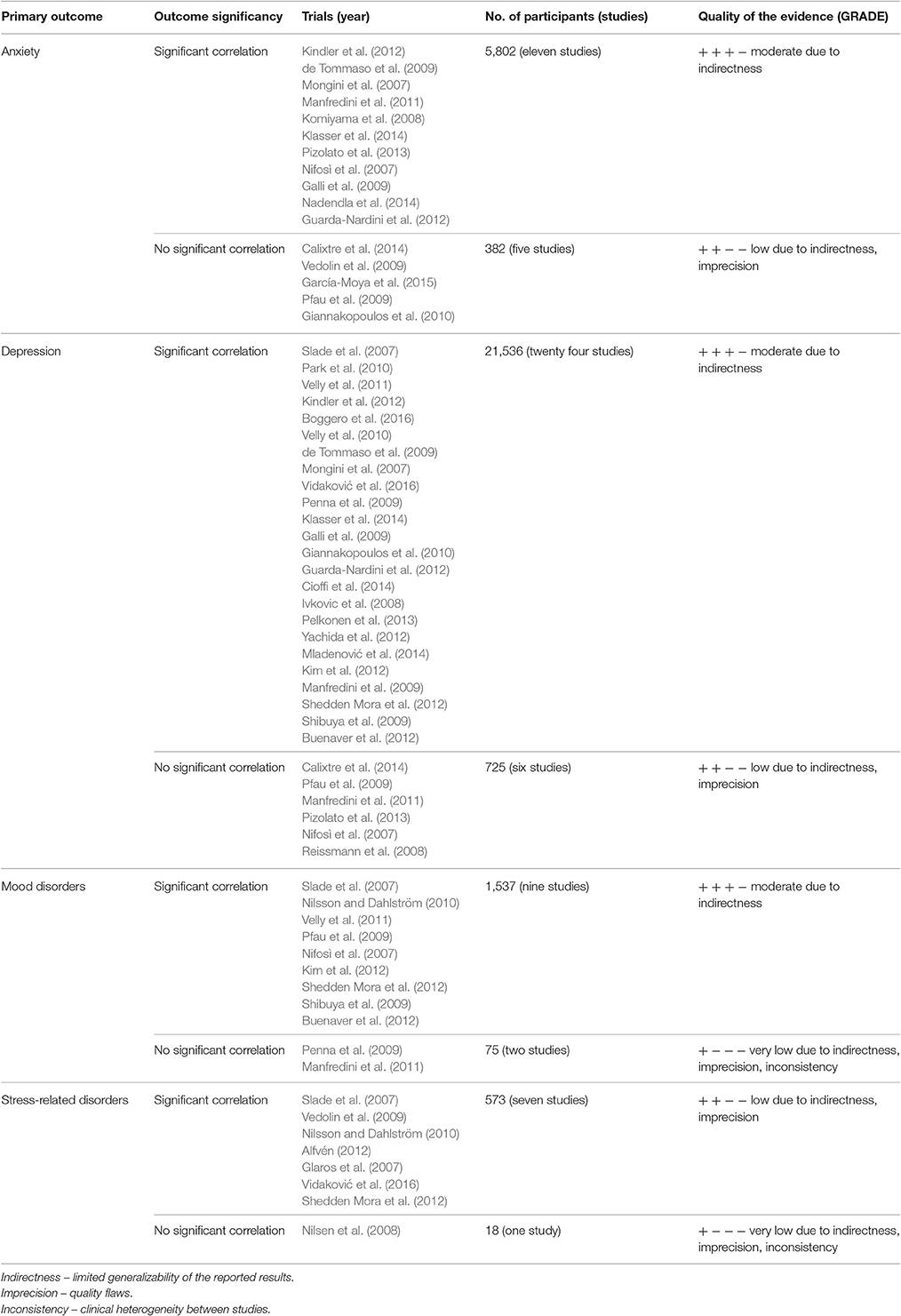
The quality of the evidence is presented in Table 2 as overall GRADE score for each primary outcome. Due to the study design (only observational studies, not randomized control trials or systematic reviews) the initial GRADE score of included studies was decreased1. Other common causes of score reduction included limited generalizability of the reported results, quality flaws and clinical heterogeneity between studies. Eventually, none of the outcome evidence was judged as high quality.
Anxiety
Among the selected studies, 16 mentioned relationships between anxiety and MFP (Mongini et al., 2007; Nifosì et al., 2007; Komiyama et al., 2008; de Tommaso et al., 2009; Galli et al., 2009; Pfau et al., 2009; Vedolin et al., 2009; Giannakopoulos et al., 2010; Manfredini et al., 2011; Guarda-Nardini et al., 2012; Kindler et al., 2012; Pizolato et al., 2013; Calixtre et al., 2014; Klasser et al., 2014; Nadendla et al., 2014; García-Moya et al., 2015). Eleven of these, performed on a population of 5802 subjects, showed this relationship to be significantly correlated (Mongini et al., 2007; Nifosì et al., 2007; Komiyama et al., 2008; de Tommaso et al., 2009; Galli et al., 2009; Manfredini et al., 2011; Guarda-Nardini et al., 2012; Kindler et al., 2012; Klasser et al., 2014; Nadendla et al., 2014). The quality of evidence for this group was moderate. In five studies there was no significant relationship (Pfau et al., 2009; Vedolin et al., 2009; Giannakopoulos et al., 2010; Calixtre et al., 2014; García-Moya et al., 2015) and, due to the limited generalizability of the reported results and methodological flaws, their GRADE score was low.
Depression
Among the main outcomes, depression was studied most frequently. Thirty research teams have investigated the relationship between MFP and depression. Twenty-four of these (Mongini et al., 2007; Slade et al., 2007; Ivkovic et al., 2008; de Tommaso et al., 2009; Galli et al., 2009; Manfredini et al., 2009; Penna et al., 2009; Shibuya et al., 2009; Giannakopoulos et al., 2010; Park et al., 2010; Velly et al., 2010, 2011; Buenaver et al., 2012; Guarda-Nardini et al., 2012; Kim et al., 2012; Kindler et al., 2012; Shedden Mora et al., 2012; Yachida et al., 2012; Pelkonen et al., 2013; Cioffi et al., 2014; Klasser et al., 2014; Mladenović et al., 2014; Boggero et al., 2016; Vidaković et al., 2016) have found a significant correlation between these issues and six studies have not (Nifosì et al., 2007; Reissmann et al., 2008; Pfau et al., 2009; Manfredini et al., 2011; Pizolato et al., 2013; Calixtre et al., 2014). The quality of evidence in the first group was moderate due to the limited generalizability of the reported results, while in the second group the score was low.
Mood Disorders
Among the selected studies, ten investigated the relationship between MFP and mood disorders (Nifosì et al., 2007; Slade et al., 2007; Penna et al., 2009; Pfau et al., 2009; Shibuya et al., 2009; Nilsson and Dahlström, 2010; Park et al., 2010; Manfredini et al., 2011; Buenaver et al., 2012; Kim et al., 2012; Shedden Mora et al., 2012). Most of these found a significant correlation between these issues; however, two of these did not support this assertion (Penna et al., 2009; Manfredini et al., 2011). In the first group, the quality of evidence was moderate due to the limited generalizability of the reported results. In the second group this relationship was scored very low.
Stress-Related Disorders
Among the main outcomes, stress-related disorders seem to be examined least often. Eight studies mentioned this problem (Glaros et al., 2007; Slade et al., 2007; Nilsen et al., 2008; Vedolin et al., 2009; Nilsson and Dahlström, 2010; Alfvén, 2012; Shedden Mora et al., 2012; Vidaković et al., 2016), only one of which did not find any significant correlation between stress and MMF (Nilsen et al., 2008). Moreover, the quality of evidence for this outcome was either low or very low.
Discussion
Anxiety
Many research teams have tried to establish whether there is an association between anxiety and pain location (Mongini et al., 2007; Nifosì et al., 2007; Kindler et al., 2012; Klasser et al., 2014). Mongini et al. (2007) found that the prevalence of anxiety was higher in patients with myogenous pain than in those with arthrogenous TMD and neuropathic pain. Researchers concluded that, regardless of the pain localization, anxiety and depression independently increased the likelihood of greater muscle tenderness. Nifosì et al. (2007) reported similar findings. However, comparisons of patients divided in a twofold manner contributed to variations in results. Firstly, the group with a myofascial component scored higher on anxiety, paranoia, psychoticism, hostility subscales, and the global severity index than the group with only articular pain. Then, a similar comparison of the three TMD subgroups separately, i.e., (1) with muscle disorders (2) with painful joint disorder and (3) mixed, found no significant differences. Subjects with muscle involvement presented significantly more frequently with a positive psychiatric history and greater lifetime use of psychotropic drugs than did the other patients. Unfortunately, in both studies there was no healthy control group. Among studies comparing patients suffering from MFP with healthy controls (Galli et al., 2009; Pfau et al., 2009; Pizolato et al., 2013; Nadendla et al., 2014) or the general population (Giannakopoulos et al., 2010), there seems to be no certain convergence between the findings. Some of these studies (Manfredini et al., 2009; Pizolato et al., 2013; Nadendla et al., 2014) showed that patients with MFP scored higher on anxiety than healthy controls. However, there have been investigations (Pfau et al., 2009; Giannakopoulos et al., 2010) that do not support this result. Another two findings that did not show any relation between anxiety and MMF (Vedolin et al., 2009; Calixtre et al., 2014) were conducted among young adults. The first study investigated clinical symptoms and jaw functionality in 19 college students with TMD (Calixtre et al., 2014). The second study assessed the pressure pain threshold of masticatory muscles and the level of pain in 29 female dental students suffering from MMF compared to 16 asymptomatic controls (García-Moya et al., 2015).
There have also been studies relevant to anxiety, MMF and comorbid conditions such as FM (de Tommaso et al., 2009; García-Moya et al., 2015). According to García-Moya et al. (2015), the palpation pain of the masseter was significantly greater in FM patients and the pain intensity and state anxiety was correlated only among FM sufferers. Notwithstanding this fact, no significant differences in anxiety were observed between FM and control group. Unfortunately, the study sample size was limited. de Tommaso et al. showed a comorbidity of FM in tension-type headache (de Tommaso et al., 2009). The total tenderness score was higher in FM patients. FM patients (especially tension-type headache sufferers) scored significantly higher in terms of anxiety and depression.
Two studies investigated relationships between masticatory muscle activity according to anxiety using electromyography (EMG) (Komiyama et al., 2008; Manfredini et al., 2011) and aimed to clarify how psychological aspects affect masticatory muscles activity. Manfredini et al. (2011) reported that an above median value for the temperamental anxiety score, depression and anger was correlated to EMG-assessed non-functional nocturnal masticatory activity. Unfortunately, the study was conducted on an insufficiently representative sample and sleep-related EMG recordings were performed only once. Also, Komiyama et al. (2008) showed that anxiety impacts on the reflexes and pain reactions associated with masticatory muscles.
Two investigations presented that salivary cortisol level was related to anxiety scores among MMF patients, but without any dependences among healthy controls. Galli et al. (2009) showed that after administration of dexamethasone patients with chronic myogenous TMD exhibited enhanced and persisting suppression of cortisol levels. Their psychological evaluation revealed that they scored significantly higher in terms of depression, anxiety, physical and mental fatigue. Nadendla et al. (2014) found that awakening salivary cortisol levels and anxiety scores were significantly greater among patients with MFP (without any other joint symptoms).
Depression
Many researchers have attempted to establish whether depression episodes influence pain location (Reissmann et al., 2008; Manfredini et al., 2009; Giannakopoulos et al., 2010; Park et al., 2010; Kim et al., 2012; Klasser et al., 2014; Boggero et al., 2016). Most of these have found that patients with muscle disorders have significantly higher depression scores (Manfredini et al., 2009; Park et al., 2010; Kim et al., 2012; Klasser et al., 2014; Boggero et al., 2016). Klasser et al. (2014) showed that patients with myogenous TMD more often reported not only depression, but also anxiety, psychiatric treatment, phobias and severe headaches than arthrogenous TMD. In this study, the psychosocial assessment of the sample was based on a dichotomous medical questionnaire and there was no verification of the accuracy of self-reported co-existing conditions. The absence of healthy controls and a reliable psychometric inventory make comparisons with other studies difficult. Similar findings were reported by Giannakopoulos et al. (2010), who established that patients with MFP were significantly more depressed than patients with joint pain. However, some researchers have not found any significant relationships between depression and muscle pain when comparing three groups of patients suffering from (1) muscle disorder, (2) arthralgia and/or osteoarthritis, and (3) both (Reissmann et al., 2008; Manfredini et al., 2009; Guarda-Nardini et al., 2012). Unfortunately in all these studies, there were no controls to compare with.
Depression was often considered the main factor to be reported in the included studies; however, other factors defined as secondary outcomes were also investigated. Some researchers have studied somatization along with depression (Park et al., 2010; Guarda-Nardini et al., 2012; Kindler et al., 2012; Shedden Mora et al., 2012; Yachida et al., 2012; Cioffi et al., 2014; Mladenović et al., 2014). Mladenović et al. (2014) investigated psychological and dentition-related aspects of TMD in class III patients referred for orthognathic surgery and showed that MFP was related to higher grades of depression and somatization (Mladenović et al., 2014). Similar findings were reported by Shedden Mora et al. (2012), who recorded nocturnal masseter activity and found that in MFP patients one component of nocturnal masseter activity, namely burst per episode, was related to general somatic complaints, TMD related symptoms, pain intensity, depression, and stress level. Patients with MFP were nearly four times more likely to have a psychiatric disorder than healthy controls. Also, Cioffi et al. (2014) found an increased incidence of episodes of depression and somatization in patients with orofacial pain. Catastrophizing was also considered as an issue accompanying MMP. Velly et al. (2010, 2011) found a positive correlation between the intensification of pain symptoms in the 18 months and catastrophizing or depression. One study mentioned post-traumatic stress disorder (Vidaković et al., 2016). This described a higher appearance of MFP syndrome among Croatian soldiers who had taken an active part in war. Fifty-nine percent of the respondents had MFP syndrome, which more often concerned patients with severe and moderate depression.
In some studies, researchers have used EMG to find correlations between muscle activity and depression (Ivkovic et al., 2008; Yachida et al., 2012). Ivkovic et al. conducted a study whose aim was to evaluate the long-term effects of antidepressant therapy on chronic pain and related disability, and masseter silent periods in psychiatric depressive patients with TMD (Ivkovic et al., 2008). The study showed lower occurrence of muscular TMD subtype and chronic muscle pain in patients on antidepressant therapy protocols. Also, Yachida et al. compared the EMG activity of masseter muscles during sleep in patients with orofacial pain and in a control group and found a positive correlation between increased myogenic activity of facial muscles and depression (Yachida et al., 2012).
Mood Disorders
Along with mood disorders, research teams have studied sleep disturbances and their influence on participants' habitual life (Shibuya et al., 2009; Buenaver et al., 2012). Shibuya et al. (2009) reported that in patients with MFP a depressive mood was common and this aggravated occlusal discomfort and sleep complaints. Buenaver et al. (2012) reported similar findings. Pain catastrophizing, defined as a “negative cognitive-affective response to pain involving rumination, helplessness, and magnification,” was strongly correlated with increased levels of pain severity and sleep disturbances. Other scientists have also studied muscle pain as a possible result of mood disorders. Pfau et al. investigated psychological parameters among TMD myogenic patients, FM patients and healthy controls (Pfau et al., 2009). Higher levels of pain, catastrophizing, disability index (but not anxiety and depression) were found in TMD patients compared to healthy individuals. Nilsson and Dahlström (2010) found that there were no differences in fatigue, emotional distress, cognitive symptoms, or somatic symptoms between patients with different TMD diagnoses. Nonetheless, the psychometric scale scores were significantly higher among TMD patients than in controls.
Stress-Related Disorders
Some researchers investigated the impact of emotional distress on pain sensitivity and muscle tenderness (Slade et al., 2007; Vedolin et al., 2009; Alfvén, 2012). According to Slade et al. (2007), stress, and also depression and mood disorders were associated with pain sensitivity and were qualified as risk factors of TMD. Vedolin et al. (2009) reported that during stressful periods, the pressure pain thresholds of masticatory muscles in MFP subjects were significantly lower than in controls. Notwithstanding the fact, that both groups were equally anxious and depressed, the MFP individuals had lower pain tolerance. Scientists have reasoned that the external stressor, that is academic examination, had a potential influence on masticatory muscle tenderness. A study conducted among children experiencing psychosomatic pain showed that there was a specific pattern of stress tender points, different from that found in FM sufferers (Alfvén, 2012). A stress tender point localized near the muscle-tendon junction in the temporal region was found only in patients suffering from prolonged stress.
Glaros et al. raised the problem of headache and TMD overlap (Glaros et al., 2007). Participants suffering from headache were significantly more likely to be diagnosed as having MFP, more tension in the jaw, face, head, and stress than those in the non-headache control group.
There was one study employing a salivary cortisol level assay (Nilsson and Dahlström, 2010). It was reported that there were no differences in awakening salivary cortisol levels between TMD patients and the healthy control group and the same held for cortisol levels and emotional distress. Nonetheless, the psychometric scale scores were significantly higher among TMD patients than in controls. An important drawback of the study is the single collection of salvia samples.
Limitations of the Study
The studies included in our systematic review are very heterogeneous. Inconsistences arising from many sources greatly impeded systematic comparisons; thus, we conducted a “narrative, qualitative summary,” as is recommended (Shamseer et al., 2015). Discrepancies related to differences in primary diagnostic criteria employed in the studies were relatively slight, but even if the diagnostic criteria were similar, the structure of comparison groups differed considerably. Some researchers divided their subjects into two (e.g., with myogenous and arthrogenous TMD; Klasser et al., 2014), three (e.g., with MFP, with joint pain and mixed; Park et al., 2010) or even four groups, when the control group was included (Giannakopoulos et al., 2010). Next, they differed in psychometric assessment tools. In all, about 20 different inventories were used to evaluate the mental status of studied individuals. Finally, the studies often differed in their design, sample strength, age and health status of enrolled participants. Thus, the evidence cannot be considered as definitively confirming a cause-and-effect relationship. However the coexistence of anxiety, depression, mood and stress-related disorders among the MMP patients, which is an indisputable scientific fact, must be taken into consideration. Clinicians' improved knowledge and awareness of this multifaceted problem would facilitate an appropriate approach to patients and the making of accurate therapeutic decisions.
Conclusions
The study of the concomitance of masticatory muscle pain with psychological variables requires careful statistical analysis before any clear conclusions about causality can be made. Unfortunately, in the light of the analyzed literature the causal relationship between mental status and MMP is still not clearly established. As a consequence, no clear explanation of any correlation between masticatory muscle pain and common psychological states, such as anxiety, depression, stress, and disturbances in mood, can be provided. Although the studies consider this question, the researchers usually prove only the co-occurrence of these mental states and dysfunctions of the masticatory muscles among the group of patients, typically in women. The evidence synthesis for main outcomes revealed that studies showing a positive relationship between particular psychological states and masticatory muscle pain provided higher GRADE score than investigations not showing any such relationship. We still need further, properly planned long-term clinical trials and laboratory tests to conclusively prove and describe the pathomechanism inducing masticatory muscle pain in terms of psychological variables.
Author Contributions
MW created a review concept, wrote and edited the manuscript. NG and JS made articles selection, wrote and edited the manuscript. MZ and DZ edited the manuscript and finally revised it before submission. All authors read and approved the final manuscript.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Abbreviations
MMP, masticatory muscle pain; RDC/TMD, Research Diagnostic Criteria for Temporomandibular Disorders; MFP, Myofacial pain; TTH, Tension-type headache; FM, Fibromyalgia; MeSH, Medical Subject Headings; TMD, Temporomandibular Disorders; TMJ, Temporomandibular Joint; CMI, Craniomandibular Index; TMJD, Temporomandibular Joint Disorders; EMG, Electromyography.
Footnotes
References
Alfvén, G. (2012). Recurrent pain, stress, tender points and fibromyalgia in childhood: an exploratory descriptive clinical study. Acta Paediatr. 101, 283–291. doi: 10.1111/j.1651-2227.2011.02491.x
Boggero, I. A., Rojas-Ramirez, M. V., de Leeuw, R., and Carlson, C. R. (2016). Satisfaction with life in orofacial pain disorders: associations and theoretical implications. J. Oral Facial Pain Headache 30, 99–106. doi: 10.11607/ofph.1526
Buenaver, L. F., Quartana, P. J., Grace, E. G., Sarlani, E., Simango, M., Edwards, R. R., et al. (2012). Evidence for indirect effects of pain catastrophizing on clinical pain among myofascial temporomandibular disorder participants: the mediating role of sleep disturbance. Pain 153, 1159–1166. doi: 10.1016/j.pain.2012.01.023
Calixtre, L. B., Grüninger, B. L., Chaves, T. C., and Oliveira, A. B. (2014). Is there an association between anxiety/depression and temporomandibular disorders in college students? J. Appl. Oral Sci. 22, 15–21. doi: 10.1590/1678-775720130054
Cioffi, I., Perrotta, S., Ammendola, L., Cimino, R., Vollaro, S., Paduano, S., et al. (2014). Social impairment of individuals suffering from different types of chronic orofacial pain. Prog. Orthod. 15:27. doi: 10.1186/s40510-014-0027-z
de Tommaso, M., Sardaro, M., Serpino, C., Costantini, F., Vecchio, E., Prudenzano, M. P., et al. (2009). Fibromyalgia comorbidity in primary headaches. Cephalalgia 29, 453–464. doi: 10.1111/j.1468-2982.2008.01754.x
Durham, J., Raphael, K. G., Benoliel, R., Ceusters, W., Michelotti, A., and Ohrbach, R. (2015). Perspectives on next steps in classification of orofacial pain–part 2: role of psychosocial factors. J. Oral Rehabil. 42, 942–955. doi: 10.1111/joor.12329
Galli, U., Gaab, J., Ettlin, D. A., Ruggia, F., Ehlert, U., and Palla, S. (2009). Enhanced negative feedback sensitivity of the hypothalamus-pituitary-adrenal axis in chronic myogenous facial pain. Eur. J. Pain 13, 600–605. doi: 10.1016/j.ejpain.2008.07.010
García-Moya, E. J., Montiel-Company, J. M., and Almerich-Silla, J. M. (2015). Case-control study of craniomandibular disorders in patients with fibromyalgia. J. Clin. Exp. Dent. 7, 293–298. doi: 10.4317/jced.51816
Gatchel, R. J. (2004). Comorbidity of chronic pain and mental health disorders: the biopsychosocial perspective. Am. Psychol. 59, 795–805. doi: 10.1037/0003-066X.59.8.795
Giannakopoulos, N. N., Keller, L., Rammelsberg, P., Kronmüller, K. T., and Schmitter, M. (2010). Anxiety and depression in patients with chronic temporomandibular pain and in controls. J. Dent. 38, 369–376. doi: 10.1016/j.jdent.2010.01.003
Glaros, A. G., Marszalek, J. M., and Williams, K. B. (2016). Longitudinal multilevel modeling of facial pain, muscle tension, and stress. J. Dent. Res. 95, 416–422. doi: 10.1177/0022034515625216
Glaros, A. G., Urban, D., and Locke, J. (2007). Headache and temporomandibular disorders: evidence for diagnostic and behavioural overlap. Cephalalgia 27, 542–549. doi: 10.1111/j.1468-2982.2007.01325.x
Guarda-Nardini, L., Pavan, C., Arveda, N., Ferronato, G., and Manfredini, D. (2012). Psychometric features of temporomandibular disorders patients in relation to pain diffusion, location, intensity and duration. J. Oral Rehabil. 39, 737–743. doi: 10.1111/j.1365-2842.2012.02320.x
Haviland, M. G., Banta, J. E., and Przekop, P. (2011). Fibromyalgia: prevalence, course, and co-morbidities in hospitalized patients in the United States, 1999–2007. Clin. Exp. Rheumatol. 29, 79–87.
Hung, C. I., Liu, C. Y., Yang, C. H., and Wang, S. J. (2016). Headache: an important factor associated with muscle soreness/pain at the two-year follow-up point among patients with major depressive disorder. J. Headache Pain 17:57. doi: 10.1186/s10194-016-0648-3
Ivkovic, N., Mladenovic, I., Petkoci, S., and Stojic, D. (2008). TMD chronic pain and masseter silent period in psychiatric patients on antidepressive therapy. J. Oral Rehabil. 35, 424–432. doi: 10.1111/j.1365-2842.2007.01819.x
Kim, Y. K., Kim, S. G., Im, J. H., and Yun, P. Y. (2012). Clinical survey of the patients with temporomandibular joint disorders, using Research Diagnostic Criteria (Axis II) for TMD: preliminary study. J. Craniomaxillofac. Surg. 40, 366–372. doi: 10.1016/j.jcms.2011.05.018
Kindler, S., Samietz, S., Houshmand, M., Grabe, H. J., Bernhardt, O., Biffar, R., et al. (2012). Depressive and anxiety symptoms as risk factors for temporomandibular joint pain: a prospective cohort study in the general population. J. Pain 13, 1188–1197. doi: 10.1016/j.jpain.2012.09.004
Klasser, G. D., Bassiur, J., and de Leeuw, R. (2014). Differences in reported medical conditions between myogenous and arthrogenous TMD patients and its relevance to the general practitioner. Quintessence Int. 45, 157–167. doi: 10.3290/j.qi.a30999
Komiyama, O., Wang, K., Svensson, P., Arendt-Nielsen, L., Kawara, M., and De Laat, A. (2008). The influence of psychological state on the masseteric exteroceptive suppression reflex and somatosensory function. Clin. Neurophysiol. 119, 2321–2328. doi: 10.1016/j.clinph.2008.07.004
Manfredini, D., Fabbri, A., Peretta, R., Guarda-Nardini, L., and Lobbezoo, F. (2011). Influence of psychological symptoms on home-recorded sleep-time masticatory muscle activity in healthy subjects. J. Oral Rehabil. 38, 902–911. doi: 10.1111/j.1365-2842.2011.02226.x
Manfredini, D., Marini, M., Pavan, C., Pavan, L., and Guarda-Nardini, L. (2009). Psychosocial profiles of painful TMD patients. J. Oral Rehabil. 36, 193–198. doi: 10.1111/j.1365-2842.2008.01926.x
Mao, C., Yang, Z. Y., Chung, V. C. H., Qin, Y., Tam, W., Kwong, J. S. W., et al. (2015). Tong-xin-luo capsule for patients with coronary heart disease after percutaneous coronary intervention. Cochrane Database Syst. Rev. CD010237. doi: 10.1002/14651858.CD010237.pub2
Means-Christensen, A. J., Roy-Byrne, P. P., Sherbourne, C. D., Craske, M. G., and Stein, M. B. (2008). Relationships among pain, anxiety, and depression in primary care. Depress. Anxiety 25, 593–600. doi: 10.1002/da.20342
Mladenović, I., Dodić, S., Stošić, S., Petrović, D., Cutović, T., and Kozomara, R. (2014). TMD in class III patients referred for orthognathic surgery: psychological and dentition-related aspects. J. Craniomaxillofac. Surg. 42, 1604–1609. doi: 10.1016/j.jcms.2014.04.029
Moher, D., Liberati, A., Tetzlaff, J., and Altman, D. G. and PRISMA Group (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 21:b2535. doi: 10.1136/bmj.b2535
Mongini, F., Ciccone, G., Ceccarelli, M., Baldi, I., and Ferrero, L. (2007). Muscle tenderness in different types of facial pain and its relation to anxiety and depression: a cross-sectional study on 649 patients. Pain 131, 106–111. doi: 10.1016/j.pain.2006.12.017
Nadendla, L. K., Meduri, V., Paramkusam, G., and Pachava, K. R. (2014). Evaluation of salivary cortisol and anxiety levels in myofascial pain dysfunction syndrome. Korean J. Pain 27, 30–34. doi: 10.3344/kjp.2014.27.1.30
Nifosì, F., Violato, E., Pavan, C., Sifari, L., Novello, G., Guarda Nardini, L., et al. (2007). Psychopathology and clinical features in an Italian sample of patients with myofascial and temporomandibular joint pain: preliminary data. Int. J. Psychiatry Med. 37, 283–300. doi: 10.2190/PM.37.3.f
Nilsen, K. B., Sand, T., Borchgrevink, P., Leistad, R. B., Rø, M., and Westgaard, R. H. (2008). A unilateral sympathetic blockade does not affect stress-related pain and muscle activity in patients with chronic musculoskeletal pain. Scand. J. Rheumatol. 37, 53–61. doi: 10.1080/03009740701716850
Nilsson, A. M., and Dahlström, L. (2010). Perceived symptoms of psychological distress and salivary cortisol levels in young women with muscular or disk-related temporomandibular disorders. Acta Odontol. Scand. 68, 284–288. doi: 10.3109/00016357.2010.494620
Okeson, J. P. (ed.). (2013). “Pains of muscle origin,” in Bell's Oral and Facial Pain, 7th Edn. (Quintessence Publishing Company), 287–311.
Park, J. W., Clark, G. T., Kim, Y. K., and Chung, J. W. (2010). Analysis of thermal pain sensitivity and psychological profiles in different subgroups of TMD patients. Int. J. Oral Maxillofac. Surg. 39, 968–974. doi: 10.1016/j.ijom.2010.06.003
Pelkonen, E. S., Mäki, P. H., Kyllönen, M. A., Miettunen, J. A., Taanila, A. M., and Sipilä, K. K. (2013). Pain-related symptoms of temporomandibular disorders in the offspring of antenatally depressed mothers and depressed parents: a 31-year follow-up of the Northern Finland Birth Cohort 1966. Eur. J. Pain 17, 1048–1057. doi: 10.1002/j.1532-2149.2012.00270.x
Penna, P. P., Recupero, M., and Gil, C. (2009). Influence of psychopathologies on craniomandibular disorders. Braz. Dent. J. 20, 226–230. doi: 10.1590/S0103-64402009000300010
Pfau, D. B., Rolke, R., Nickel, R., Treede, R. D., and Daublaender, M. (2009). Somatosensory profiles in subgroups of patients with myogenic temporomandibular disorders and fibromyalgia syndrome. Pain 147, 72–83. doi: 10.1016/j.pain.2009.08.010
Pizolato, R. A., Freitas-Fernandes, F. S., and Gavião, M. B. (2013). Anxiety/depression and orofacial myofacial disorders as factors associated with TMD in children. Braz. Oral Res. 27, 156–162. doi: 10.1590/S1806-83242013000100021
Rees, C. S., Smith, A. J., O'Sullivan, P. B., Kendall, G. E., and Straker, L. M. (2011). Back and neck pain are related to mental health problems in adolescence. BMC Public Health 11:382. doi: 10.1186/1471-2458-11-382
Reissmann, D. R., John, M. T., Wassell, R. W., and Hinz, A. (2008). Psychosocial profiles of diagnostic subgroups of temporomandibular disorder patients. Eur. J. Oral Sci. 116, 237–244. doi: 10.1111/j.1600-0722.2008.00528.x
Rollman, G. B., and Gillespie, J. M. (2000). The role of psychosocial factors in temporomandibular disorders. Curr. Rev. Pain 4, 71–81. doi: 10.1007/s11916-000-0012-8
Shamseer, L., Moher, D., Clarke, M., Ghersi, D., Liberati, A., Petticrew, M., et al. (2015). Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 349:7647. doi: 10.1136/bmj.g7647
Shedden Mora, M., Weber, D., Borkowski, S., and Rief, W. (2012). Nocturnal masseter muscle activity is related to symptoms and somatization in temporomandibular disorders. J. Psychosom. Res. 73, 307–312. doi: 10.1016/j.jpsychores.2012.07.008
Shibuya, T., Kino, K., Sugisaki, M., Sato, F., Haketa, T., Nishiyama, A., et al. (2009). Comparison of occlusal discomfort in patients with temporomandibular disorders between myofascial pain and disc displacement. J. Med. Dent. Sci. 56, 139–147.
Slade, G. D., Diatchenko, L., Bhalang, K., Sigurdsson, A., Fillingim, R. B., Belfer, I., et al. (2007). Influence of psychological factors on risk of temporomandibular disorders. J. Dent. Res. 86, 1120–1125. doi: 10.1177/154405910708601119
Tricco, A., Chit, A., Hallett, D., Soobiah, C., Meier, G., Chen, M., et al. (2012). Effect of influenza vaccines against mismatched strains: a systematic review protocol. Syst. Rev. 1:35. doi: 10.1186/2046-4053-1-35
Vaccarino, A. L., Sills, T. L., Evans, K. R., and Kalali, A. H. (2009). Multiple pain complaints in patients with major depressive disorder. Psychosom. Med. 71, 159–162. doi: 10.1097/PSY.0b013e3181906572
Vedolin, G. M., Lobato, V. V., Conti, P. C., and Lauris, J. R. (2009). The impact of stress and anxiety on the pressure pain threshold of myofascial pain patients. J. Oral Rehabil. 36, 313–321. doi: 10.1111/j.1365-2842.2008.01932.x
Velly, A. M., Look, J. O., Carlson, C., Lenton, P. A., Kang, W., Holcroft, C. A., et al. (2011). The effect of catastrophizing and depression on chronic pain–a prospective cohort study of temporomandibular muscle and joint pain disorders. Pain 152, 2377–2383. doi: 10.1016/j.pain.2011.07.004
Velly, A. M., Look, J. O., Schiffman, E., Lenton, P. A., Kang, W., Messner, R. P., et al. (2010). The effect of fibromyalgia and widespread pain on the clinically significant temporomandibular muscle and joint pain disorders–a prospective 18-month cohort study. J. Pain 11, 1155–1164. doi: 10.1016/j.jpain.2010.02.009
Vidaković, B., Uljanić, I., Perić, B., Grgurević, J., and Sonicki, Z. (2016). Myofascial pain of the head and neck among Croatian war veterans treated for depression and posttraumatic stress disorder. Psychiatr. Danub. 28, 73–76.
Yachida, W., Castrillon, E. E., Baad-Hansen, L., Jensen, R., Arima, T., Tomonaga, A., et al. (2012). Craniofacial pain and jaw-muscle activity during sleep. J. Dent. Res. 91, 562–567. doi: 10.1177/0022034512446340
Young, M., Stevens, A., Porath-Waller, A., Pirie, T., Garritty, C., Skidmore, B., et al. (2012). Effectiveness of brief interventions as part of the screening, brief intervention and referral to treatment (SBIRT) model for reducing the non-medical use of psychoactive substances: a systematic 91 review protocol. Syst. Rev. 1:22. doi: 10.1186/2046-4053-1-22
Keywords: myofascial pain syndrome, masticatory muscle pain, masseter muscle pain, mental disorders, anxiety, depression, mood disorders, stress-related disorders
Citation: Wieckiewicz M, Zietek M, Smardz J, Zenczak-Wieckiewicz D and Grychowska N (2017) Mental Status as a Common Factor for Masticatory Muscle Pain: A Systematic Review. Front. Psychol. 8:646. doi: 10.3389/fpsyg.2017.00646
Received: 30 November 2016; Accepted: 11 April 2017;
Published: 09 May 2017.
Edited by:
Alexandrina L. Dumitrescu, Dental Private Practice, RomaniaReviewed by:
Letícia Bojikian Calixtre, São Carlos Federal University, BrazilRichard Ohrbach, University at Buffalo, USA
Copyright © 2017 Wieckiewicz, Zietek, Smardz, Zenczak-Wieckiewicz and Grychowska. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mieszko Wieckiewicz, m.wieckiewicz@onet.pl
 Mieszko Wieckiewicz
Mieszko Wieckiewicz Marek Zietek2
Marek Zietek2 Joanna Smardz
Joanna Smardz Natalia Grychowska
Natalia Grychowska