- 1School of Psychology, University of Lincoln, Lincoln, United Kingdom
- 2Retired, West Sussex, United Kingdom
Dental fear/anxiety is a widely recognised problem affecting a large proportion of the population. It can result in avoidance and/or difficulty accepting dental care. We believe that psychological intrusion may play a role in the aetiology and maintenance of dental fear for at least some individuals. In this narrative review we will take a developmental perspective in order to understand its impact across the lifespan. We will consider the nature of ‘self,’ parenting styles, the details of intrusive parenting or parental psychological control, and briefly touch upon child temperament and parental anxiety. Finally, we draw together the supporting (largely unrecognised) evidence available in the dental literature. We illustrate the paper with clinical examples and discuss possibly effective ways of addressing the problem. We conclude that psychological intrusion appears to play an important role in dental fear, for at least some individuals, and we call for detailed research into the extent and exact nature of the problem. A simple means of identifying individuals who are vulnerable to psychological intrusion would be useful for dentists.
Introduction
Dental fear/anxiety is a widely recognised problem affecting a large proportion of the population, resulting in avoidance and/or difficultly in accepting dental care (Humphris et al., 2013; Armfield and Ketting, 2015). Two recent reviews of the field (Carter et al., 2014; Seligman et al., 2017) failed to identify any evidence for psychological intrusion being associated with the aetiology, maintenance or treatment of dental fear. Armfield (2011), Carrillo-Diaz et al. (2012), and Crego et al. (2013) have proposed a ‘cognitive vulnerability model’ of dental fear which references our model of dental fear (Chapman and Kirby-Turner, 1999), suggesting that relevant threat cognitions should be identifiable. However, we would argue that the process of psychological intrusion is insidious and will be largely unidentifiable by patients, except as a feeling of unease, though ‘clues’ may be offered to the alert practitioner.
This brief, narrative review of psychological intrusion or control will take a developmental perspective. To understand psychological intrusion in adulthood, it is necessary to first understand the development and impact of psychological intrusion in childhood and the vulnerabilities thus created in the individual. It will consider the nature of ‘self,’ parenting styles, the details of intrusive parenting or parental psychological control, briefly touch upon child temperament and parental anxiety and then consider how psychological intrusion or control may impact the individual across the lifespan.
Finally, we draw together the supporting (largely unrecognised) evidence available in the dental literature. We illustrate the paper with clinical examples and discuss possibly effective ways of addressing the problem.
In writing the paper we were aware of the conflicting needs of readers who are psychologists, and therefore well informed regarding the psychological issues covered, and readers with a dental background who may be less familiar with some or all of the issues covered. The paper seeks to address this.
The Nature of the Self
Individuals have a conscious model of the ‘self’ and of identity as ‘a self as one experiences oneself’ (Dagnan et al., 2002), that is it is only accessible to oneself. This is continually remodelled through social interactions which re/construct one’s core self-schema (Beck et al., 1979). A healthy inner model is achieved through the validation, by others of an outer, public self. This construction can be conscious or unconscious, but is the desired self (Dagnan et al., 2002).
This ‘psychological self,’ has been conceptualised as four ‘depths’ of self, (Scott, 1993; Geanellos, 2003) similar to the layers of physical interpersonal space (Figure 1):
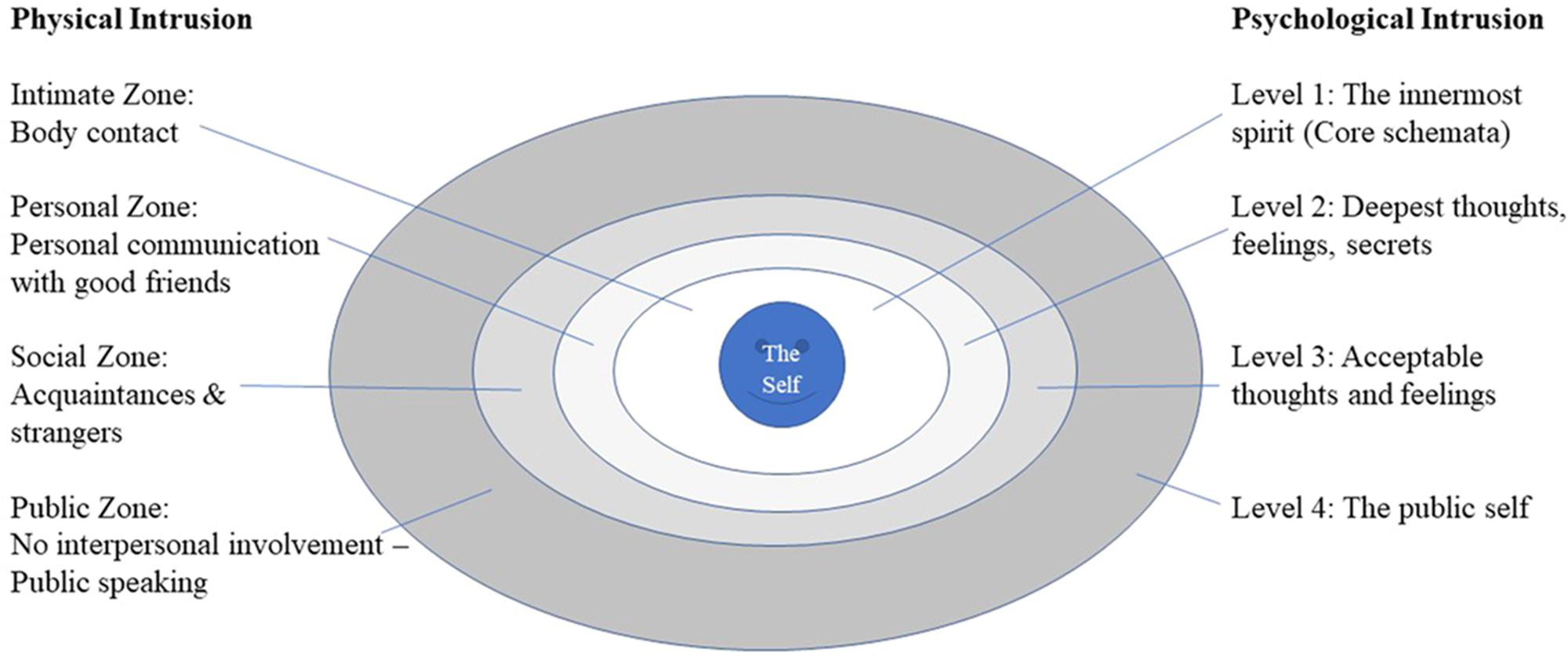
FIGURE 1. The four depths of psychological self and interpersonal space adapted from Scott (1993), with permission.
• Level 1 – an inner core – core schemata
• Level 2 – deepest thoughts, feelings and secrets
• Level 3 – thoughts and feelings perceived as generally acceptable
• Level 4 – outermost layer - the public self.
In adulthood, the ‘self’ is vulnerable to exclusion and distance which result in insecurity, seeking to please and fear of failure to do so. It is also vulnerable to intrusion and control (Dagnan et al., 2002).
An intrusive ‘assault’ may leave the individual feeling coerced into presenting a different self to the world (Level 4) or, at a deeper level, that their core (Level 1) is being defined by another with a loss of autonomy, where another defines one’s sense of self (Dagnan et al., 2002). There may be a major fear of being ‘taken over’ by another. This often results in shame (Dagnan et al., 1998). Dental patients for whom this is relevant will be vulnerable to any sense of loss of control or threat to their ‘self’ or self-esteem at any of the 4 levels of psychological intrusion. In a broader context, intrusion is measured by the Self and Other Scale (Dexter-Smith et al., 2003; pp. 102–103) which includes items such as, ‘I dread being under someone else’s control.’ and ‘Often I wish people would give me space to be myself,’ which give a sense of how vulnerability in the dental clinic may arise.
We believe psychological assaults on the self can also happen to children at all four levels within the dental environment, though the exact ‘depth’ of danger will depend on the meaning of the assault to the patient. For example, the dentist runs a prophylaxis brush over a 6-year-old’s teeth. (He has gingivitis, so it bleeds as the dentist accidently clips the gum; it may be uncomfortable.) The child says, ‘That hurts.’ To which the dentist (and sometimes the mother) reply, ‘Oh, no it doesn’t. It can’t. It’s just an electric toothbrush.’ For some children, this will simply be taken as a denial of their painful experience (most likely impacting at Level 3; “It really was uncomfortable, no matter what you say.”) For others, (and this probably includes those where the mother joins in) this is imposing another’s sense of reality on the experience and will be intrusive at a deeper level, as, ‘My experience is wrong/unheard’ (“But I told you it hurts! Why don’t you believe me?”; Level 2) or, “I am such a wimp” (Level 1). Similarly, dentists are trained to prepare the patient for sensations/discomfort/pain using language that tends to diminish perceived sensation as a way of reducing fear. However, the child may experience this as an enormous, ‘Ouch.’ If this discrepancy is about a prophylaxis brush on an incisal edge, then reconstructing of pain scales is required (Chapman and Kirby-Turner, 2002, 2005) but if it is about a deep cavity with a local anaesthetic in place, it should never be denied as this is overtly intrusive. It is possible to imagine parallel experiences for adult patients. Wepman and Sonnenberg (1978) noted that dentists sometimes tried to shame children into changing their behaviour.
Parenting Style
Parenting styles (Baumrind, 1966; Baumrind, 2012) may be categorised as
1. authoritarian (high demand/low responsiveness; controlling, restrictive, disciplinarian approach, setting high standards with poor emotional support)
2. authoritative or ‘good enough’ (emotionally supportive environment where reasonable standards are set and expected consistently, with appropriate granting of autonomy fostering independence and development)
3. permissive or ‘laissez faire’ (low demand/high responsiveness; few demands are made, little discipline enforced and low levels of control imposed). Permissive parenting may be divided to create a neglectful group (low demand/low responsiveness) (Maccoby and Martin, 1983). Baumrind (2012) emphasised that both authoritarian and authoritative parenting are power-assertive, but it is the coercive nature of authoritarian parenting that is detrimental.
Self-reported parenting style (Robinson et al., 1995) is associated with internalising and externalising disorders in children (Berg-Nielsen et al., 2002) and has been found to influence dentist–child–parent interactions in the dental clinic (ten Berge et al., 2003; Aminabadi and Farahani, 2008; Armfield, 2010; Krikken et al., 2012a; Aminabadi et al., 2015), though this is not a consistent finding (Krikken and Veerkamp, 2008; Krikken et al., 2012a, 2013). Compared to permissive and authoritarian parenting, authoritative parenting is associated with ‘more positive’ behaviour in the dental clinic (Howenstein et al., 2015).
Simplifying parenting constructs, Barber and colleagues (Barber and Harmon, 2002; Barber et al., 2002) consider two categories of parenting:
• parental support (a unidimensional construct encompassing behaviours such as nurturing, warmth, responsiveness, and acceptance).
• parental control (behavioural and coercive psychological control or intrusion, which is discussed in more detail below). Psychological control interferes with a child’s ability to become independent, to develop a healthy sense of self and personal identity whilst appropriate behavioural control facilitates development by providing supervision and guidance (Smetana and Daddis, 2002).
• parental support relates to positive child development; maternal warmth can neutralise the negative impact of intrusive parental behaviour (Raudino et al., 2013). At least in early childhood, it may be that mothers’ parenting impacts more on daughters than sons (Ollendick and Horsch, 2007; Barnett and Scaramella, 2017).
Possibly because psychological control is such a complex construct, it has been found to be a separate construct from ‘autonomy granting’; they do not form either end of a continuum of parenting (Silk et al., 2003). The relationship, in children, between low levels of maternal autonomy granting and increased emotional reactivity and the emotion regulation strategies used, is moderated by child perceived control (Benoit Allen et al., 2016).
Parents and children both seek to control the private aspects of the child’s life such as preferences and choices of friends, activities, the state of his/her body and privacy. There is an age-related decrease in the areas perceived as legitimate for parental control and conflict between adolescents and their parents as to where the boundaries lie. Adolescents generally see parent control over moral and conventional issues as legitimate. However, if parents try to control personal issues, they are perceived as psychologically controlling (Smetana and Daddis, 2002). A dentist who is being too forthright regarding the need to clean one’s teeth may find her/himself similarly perceived. We have noticed that the flaunting of unhealthy eating habits (for example sugary snacks and drinks between meals) in defiance of professional advice and parental wishes, appears to be one of the few areas in which some children can seize control.
A large study of adolescents (Young et al., 2011) found that children’s perceptions of emotional neglect and control were not associated with objective measures of neglect and control and were independently associated with later psychiatric disorders. This reflects the problem for dentists; one child’s reassurance is another child’s intrusive threat, presumably based on the intrusiveness of their learning experiences within the family. For dentists this is a particular issue; non-cooperative behaviour may be interpreted as non-compliance and may result in intrusive coercion and threats by the dentist, or fear, which is likely to result in encouragement and reassurance (see below). These latter dentist behaviours are usually associated with reduced fear-related child behaviours, but may, apparently counter-intuitively, escalate the situation. This may partly be due to psychological intrusion. As we wrote this paper, NK-T ‘confessed’ to HC that, initially in their joint clinics, he had had to get HC to pause and get her to give the children a chance to think things through. Even as a dentist who was skilled in treating frightened children, she still had a tendency to ‘leap in and reassure and encourage,’ with a tendency to overwhelm the most vulnerable. Dentists are trained to problem solve and intervene; sometimes they need someone to say, ‘let’s pause here and find out a little more’ before they are unwittingly guilty of being intrusive like the parent.
More recently identified styles of ‘overparenting’ have been identified including the ‘hyper-parenting’ styles (Segrin et al., 2013; Janssen, 2015) of:
• “helicopter parents” who try to protect their child from all dangers and to solve all of his/her problems.
• “little emperor” parents who strive to give their children all the material goods they desire.
• “tiger moms” who push for and accept nothing less than exceptional achievement from their children. For example, HC once treated a 6-year-old who was undoubtedly intelligent, but claimed to have read the entirety of The Hobbit in 4 days.
• “concerted cultivation” the scheduling of several extracurricular activities to provide them with an advantage.
Overparenting includes risk aversion, a preoccupation with the child’s happiness, and the drive to pre-emptively solve the child’s problems. It is driven by parents’ over enthusiastic wish to ensure the success and happiness (defined in parental terms) of their child, by removing any obstacles along the way. It may represent enmeshment (Segrin et al., 2012) (see below).
Parental Psychological Control or Intrusive Parenting
The characteristics of parental psychological control or intrusion fall into 5 main categories (Barber and Harmon, 2002):
(1) In manipulative behaviour, the parent (usually the mother) attempts to manipulate the child’s behaviour and/or shift the emotional balance within the relationship by a variety of means, as illustrated by examples from HC’s dental clinic:
• Guilt induction/blaming – “You’ve got to have it done now– I’ve taken the morning off work to bring you” (Nelson and Crick, 2002).
• Contingent affection – parental affection and attention are contingent on the child being or behaving as the parent would like. “I’m not going to hold your hand unless you behave.”
• Trying to change how the child thinks. “Are you sure it feels OK?” (I wouldn’t like it!) (Nelson and Crick, 2002).
• Instilling anxiety, although this has been excluded from more recent measures of psychological control. “You wouldn’t catch me sitting in that dental chair” or “I don’t like the dentist.”
• Excluding outside influence - “I don’t care what Mrs Smith (class teacher) at school told you, she doesn’t know anything.”
• Being unfriendly when the child has a different point of view to the parent. “I know you don’t want to have the fissure sealants, but is that the way to pay me back for all the effort I’ve taken bringing you here” (Nelson and Crick, 2002).
• Expressions of disappointment/excessive criticism, which may be accompanied by a refusal to talk to the child. “I’m really upset with you. I thought you’d be braver than that” (Nelson and Crick, 2002).
• Shaming and laughing at child’s mistakes despite fact that child is trying very hard (Sroufe et al., 1993). “Your little brother is braver than you are.” Dentists can compound this by using a more confident, younger sibling as a role model.
• Bringing up past mistakes during criticism. “Oh, you are so difficult at the dentist; it’s just the same as you being difficult going to the doctor” (Nelson and Crick, 2002).
• Invalidation/ignoring of feelings. “Don’t be silly, that doesn’t hurt.”
• Derision (derogatory comments, sarcasm and scolding), especially in the company of others (Rubin et al., 2002). “Oh, don’t bother the dentist with such a silly question.” “Oh, come on Lucy, you’ve never managed to do it before, why do you think you can do it now?”
It is interesting to note how many of these scenarios are shame-inducing and may well feed into the model of the self which is described above.
(2) In constraining/binding behaviour, the child’s self-expression of his/her anxieties, conflicts and disagreements with parental rules is actively discouraged or limited to parental interests, thus undermining the child. “I know you don’t like the toothpaste, but that’s the one we buy because your Dad likes it.” “And please don’t start on about how you don’t want to miss football to come here – you are simply not missing lessons.” Self-expression and discovery are inhibited as the child is undermined in family interactions. Reflective learning opportunities about the self and others are lost.
(3) Expectations and achievement demands of the child are excessive and standards set are absolute. “He can’t come to an appointment then as he has to practise for his clarinet exam and we’re hoping he’ll do really well – he needs to get a distinction so that he can get a scholarship to college.”
(4) The parent may oscillate between caring and over-involvement to attacking behaviours. The parent may behave as a peer of the child or may defer to the child for direction. This confuses the child about his/her acceptability to the parent and thus maintains parental power (Sroufe et al., 1993). It may be associated with disorganised attachment (Wang et al., 2015).
(5) Parents are possessive; they may ‘baby’ the child, encourage psychological and emotional dependence, unduly emphasise the affectional bonds between the parent and child and limit the child to activities within the family realm (Wood, 2006). This overprotection can take several forms; age inappropriate and unnecessary help with self-help tasks such as dressing, which the child is capable of carrying out; use of baby words/language; excessive physical affection; invasions of privacy. These are intrusive because they oblige the child to function at an immature level (Wood et al., 2007). They include, for young children, sitting the child on the lap or initiating physical affection, such as kissing or caressing before a task is complete, i.e., it is distracting from the task which actually requires the child’s full attention (Wood, 2006). With older children, behaviours include not allowing the child to make decisions such as what to wear, encouraging dependency and restricting freedom (Parker et al., 1979). Overprotection appears to be particularly damaging for boys (Enns et al., 2002). HC has treated several only sons of much older parents who seem, to her, to be particularly vulnerable to infantilization.
Such inappropriate parental power is ensured by the child being totally subordinate to the parent by;
• having to conform to parental wishes (the mother who tries to insist that her reluctant teenager has orthodontic treatment, even though he doesn’t want it)
• seeking permission for everything (the child who looks to his mother before he is prepared to accept the proffered sticker for good behaviour)
• the parent attempting to shape the behaviour and attitude of the child according to an absolute standard of behaviour: “Come on Henry, you know I expect better of you than this. If you don’t do it I’ll throw away your bicycle [a birthday present].”
It can thus be seen that parental psychological control or intrusive parenting can impact the child’s experience in the dental clinic in many ways.
At its most corrosive, the possessiveness and dominance are so severe that there is a process of enmeshment in which there is a blurring of psychological boundaries in favour of a family identity (Barber and Buehler, 1996; Kivisto et al., 2015). Children from enmeshed families have increased levels of anxiety, mediated by their temperament and sensitivity to threat, their psychological flexibility and self-compassion (Rowsell et al., 2016; Berryhill et al., 2018).
Extremely intrusive and controlling parenting can be viewed, at its extreme, as child emotional abuse (CEA) (Bell and Higgins, 2015). However, it may be limited to verbal abuse, hostility, criticism and expressions of overt dislike of the child. It damages immediately, or gradually, the behavioural, affective and cognitive functioning of the child (Sanders and Becker-Lausen, 1995).
Psychological control is thus a covert, passive-aggressive and insidious form of control that is intrusive and manipulative of a child’s thoughts, feelings, and attachment to his/her parents (Walling et al., 2007). It reflects an underlying lack of sensitivity to the child’s needs by parent(s) who are relatively uninvolved with their children (Pettit and Laird, 2002). High levels of parental psychological control are consistently associated with internalising (anxiety and depression) and externalising (delinquency, aggression, antisocial behaviour and defiance) problems in children and adolescents. This is found across cultures and age groups (Olsen et al., 2002). Both fathers and mothers (the more thoroughly researched parent) can adopt this pattern of child rearing, the level of impact on the child varying with the type of parent–child dyad and the age of the child (Stone et al., 2002).
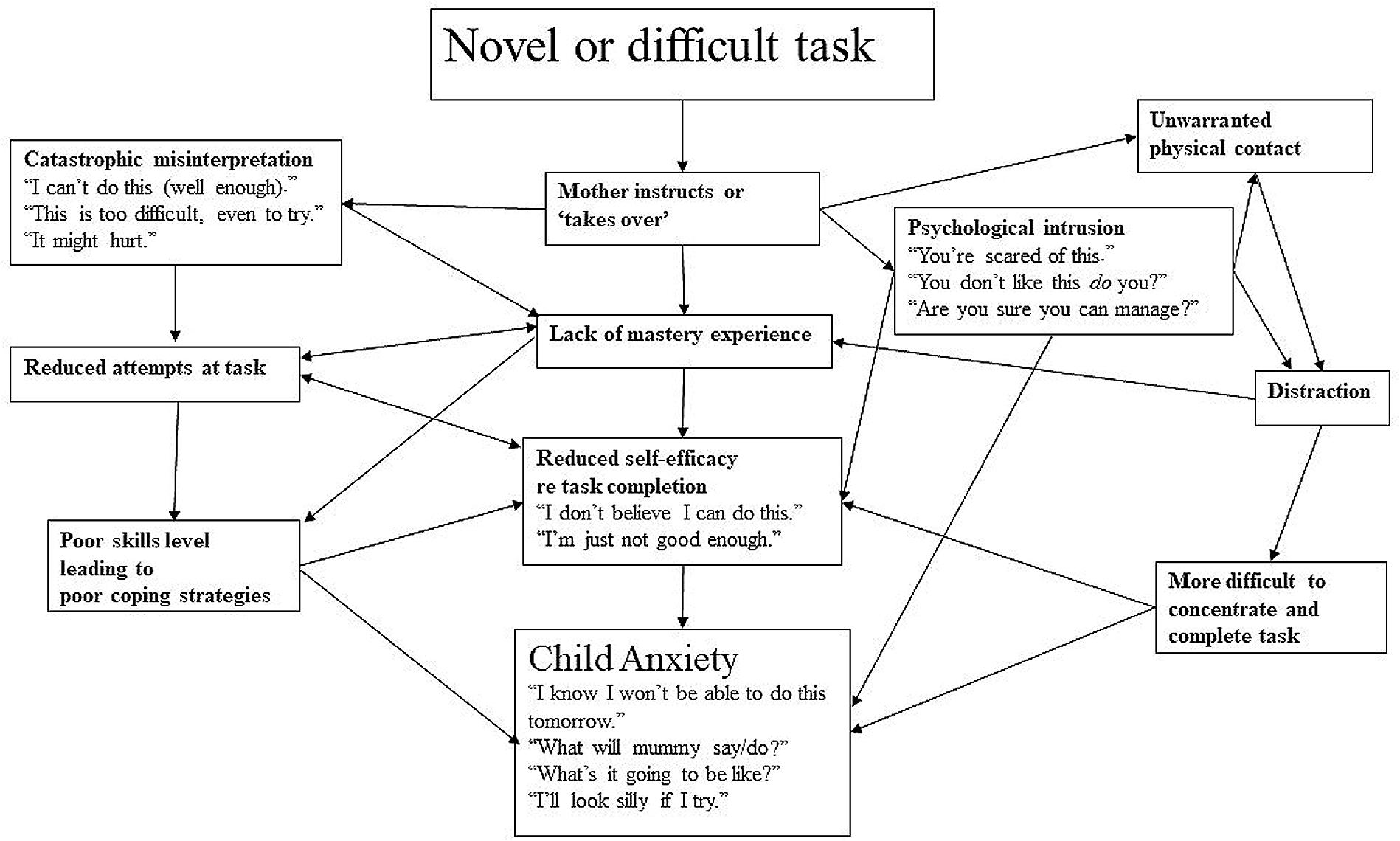
Overcontrol may reduce a child’s opportunities to learn, his sense of mastery and competence; the child’s self-efficacy is undermined (Barber and Harmon, 2002) and s/he becomes anxious when faced with a novel task (Affrunti and Ginsburg, 2012). S/he then goes on to be anxious when faced with separation. For the dental team, this forms the difficult vicious circle of an anxious child with a ‘difficult,’ intrusive parent, whom the team would like to exclude; however, that would increase the child’s anxiety.
Constant exposure to criticism and derision results in the development of negative schema and beliefs about the self and the child may withdraw from the social world (Rubin et al., 2002). This can be detrimental to the child’s personal and social development and is linked to adjustment problems in both children and adolescents.
We have summarised this process in Figure 2.
Child Temperament
Temperament refers to children’s behavioural style, or the manner in which they interact with their environment. Temperament has been quantified into nine temperament categories (including approach and withdrawal/avoidance) and five temperament constellations (easy, intermediate low, slow to warm up, intermediate high, difficult) (Chess and Thomas, 1986). More simply, these are categorised as inhibited who are restrained, cautious and avoidant of unfamiliar people, events, and places, and uninhibited children who display spontaneous approach to novelty (Kagan et al., 1994, 2007). Inhibited children are anxiety-prone, (Kagan, 1997; Rapee, 2002; Vervoort et al., 2010) and tend to remain so through adolescence and into adulthood (Schwartz et al., 2003). In young children, intrusive control is associated with behavioural inhibition (BI), predicting its stability and moderating the risk of anxiety in children with high BI (Chronis-Tuscano et al., 2015; Paulus et al., 2015).
An inhibited young child is likely to stand frozen at the mother’s side with his lips sealed. He will not make eye contact, talk or cooperate at all. It is easy, in these circumstances for the dentist to interpret this as non-compliance or to weigh in with coaxing and a ‘firm hand.’ If interpreted as fear, reassurance will be elicited. These behaviours direct significant levels of intrusive attention toward the child and may be counter-productive (Weinstein et al., 1982; Zhou et al., 2011; Zhou and Humphris, 2013). Chatting to the parent and, almost, ignoring the child gives him a chance to quietly assess the dentist’s demeanour, ‘threat level’ and to evaluate his surroundings.
One early study using non-standard measures found that BI was associated with behavioural signs of distress/non-compliance (Hammock, 1999). Behaviourally inhibited (Radis et al., 1994; Arnrup et al., 2002, 2007) shy, or ‘slow to warm up’ children are at increased risk of isolated dental behaviour management problems (DBMPs) (Quinonez et al., 1997), or DBMPs in combination with dental fear (Klingberg and Broberg, 1998; de Oliveira et al., 2006). Indeed, a proportion (16%) of parents in a study in the Netherlands attributed their child’s dental fear to temperament (ten Berge et al., 2001). Temperament, as measured by the EASI was associated with dental anxiety at 15 years of age (Stenebrand et al., 2013). DBMPs can represent fearful behaviour or non-compliance because of an externalising disorder. However, a vicious circle operates as intrusive parenting results in child externalising problems and reduced effortful control which then provoke intrusive parenting (Eisenberg et al., 2015). Arnrup et al. (2004) found that children with an inhibited temperament retained and increased their risk of being dentally fearful at follow-up, whilst those with an externalising temperament demonstrated an increased risk of non-compliance. Care has to be taken interpreting studies, as the treatment children are expected to accept is sometimes an examination, prophylaxis and fluoride application (Hammock, 1999), or even a filling with a local anaesthetic and the use of rubber dam at a single, often initial visit (O’Callaghan et al., 2006; Allen and Wallace, 2013). These are a significant, potentially overwhelming challenge for young, treatment-naïve children.
Significant correlations were found between 3 aspects of temperament (activity, impulsiveness, and emotional lability) and dental anxiety in 15-year-old adolescents. A regression analysis showed that activity and impulsivity were predictive of dental anxiety (Stenebrand et al., 2013). This is somewhat surprising as these aspects of temperament are associated with approach rather than withdrawal. The distinction between dental fear and dental behaviour management problems (DBMP) is important. Dentists are more likely to identify DBMP than dental fear and children in studies are often referred on basis of DBMP. It is often assumed that DBMPs are the equivalent of dental fear. In one study only 27% children with DBMP had dental fear and 61% of the dentally fearful children had DBMP (Klingberg and Broberg, 2007). This suggests that there is a continuum of uncooperative behaviour in the dental surgery with most cases being mixed fearful and DBMP (ten Berge, 2003). Interestingly, referrals made to HC’s clinic were always on the basis of ‘fear.’ Perhaps this was because parents appeared to find any suggestion that their child is ‘naughty’ very threatening. The effectiveness of treatment of dental anxiety is often assessed using measures of behavioural compliance, although children’s self-report measures are increasingly being used (Fenlon et al., 1993; Kotsanos et al., 2005; Cox et al., 2011).
An interview study in Brazil (de Oliveira et al., 2006, p. 474) found that mothers’ beliefs about their children’s refusal to accept dental treatment were strongly linked to perceptions of
• the children’s temperament (fearful, insecure, shy, dependent, aggressive, responsible, difficult, jealous, uneasy, aggressive, tantrum, perfectionistic)
• a category labelled ‘lack of affection’, which included lack of love and emotionally deprived
• a category labelled ‘protecting children’ which included protection, overindulgence, overprotection, pity, authority and suggests interactions which may be at the level of intrusiveness.
When mothers respond to their child’s fearfulness with intrusive and overprotective behaviours, they are either pushing the child toward a feared, novel stimulus too forcefully or are over-involved in challenges; in ‘helping’ (Kiel and Buss, 2010). This takes control away from the child, minimizing the child’s authentic responses and opportunities to learn how to master unfamiliar situations (Chorpita and Barlow, 1998). These parental strategies may be used with the very best of intentions – to protect their child by discouraging fear reactions which might have negative personal or social consequences, or by protecting the child from experiencing any consequent distress. However, these may increase the risk of undermining healthy emotion regulation development and social interaction (Rubin et al., 2002; Buss and Kiel, 2011). They may be maladaptive for both fearful (Kiel and Buss, 2010) and fearless (Waller et al., 2017) children. Thus, for fearful children, a vicious circle operates, with fearful behaviour triggering intrusion or overprotection and this having long term implications for the development of internalising and externalising behaviours in middle to late childhood (Barrett et al., 1996; Kiel and Buss, 2010).
Interestingly, a large, longitudinal study (Gallitto, 2015) found that, for children with difficult/unadaptable temperaments, exposure to more positive parenting reduced behavioural management problems, demonstrating that positive parenting helps children face challenges. This implies that coaching a parent retains the child’s secure base and provides a modified learning environment for the child and, indeed, a learning environment for the parent. We have found that the dentally fearful parent learns appropriate support and coaching techniques and observes their children develop appropriate and highly functional coping skills. They have reported shifting this learning to other interactions with their children and to taking the skills learned into their own treatment setting. One dentally anxious mother, whose 3 children had been very, very seriously and repeatedly traumatised by their family dentist, told HC, “For various reasons I was not able to change practices, so when I go to the dentist (the one who traumatised the children) and things get difficult for me, I close my eyes and I put myself back here [HC’s clinic] with you and I know I will cope.”
A study with adults found that the emotional lability aspect of temperament was related to dental fear and general psychological distress. However, there were no temperamental differences compared to non-fearful controls (Lundgren et al., 2007). This suggests that temperament and its implications for tolerance of intrusion may play less of a role in dental fear in adults.
Parents with high behavioural inhibition sensitivity (BIS) may overprotect their children to avoid new situations they themselves find threatening. Overprotection may be motivated by concern that something objectively negative could happen (Zelenski and Larsen, 2002) or to avoid a subjectively negative consequence, like their children’s distress, which parents high in BIS may find unpleasant. Overprotection may moderate the link between maternal BIS sensitivity and child internalising behaviour (Kiel and Maack, 2012).
Maternal embarrassment is related to the child’s inhibited behaviour (Kiel and Buss, 2013) suggesting that care should be taken not to further shame or humiliate the mother in the dental surgery, for example by heavy handed feedback about the implications of missing previous appointments.
Parental Anxiety
Parental psychological control appears to arise from parental separation anxiety, maladaptive perfectionism (Soenens et al., 2006) or hostility toward the child (Pettit and Laird, 2002). The parents are not acting to socialise their children, but to protect their own feelings and needs (Barber and Harmon, 2002). The parent seeks to maintain and defend his/her own psychological status within the family and particularly with the child. This occurs at the child’s expense; the child is not allowed to develop as an individual apart from the parent.
Parental Sensitivity to hurt and disapproval of negative emotion are associated with the use of psychological control (Walling et al., 2007). These parents will be vulnerable to any sense of perceived criticism, so care must be taken when tackling, for example, the subjects of diet and oral hygiene. We have noticed that they also appear to be vulnerable to any perceived criticism of their parenting, such as an inference that their child has behavioural problems rather than being scared. Based on clinical observation, we would hypothesise that a fear of being judged as a parent for having a non-cooperative child, has an impact on parent-child interaction under stress.
Inappropriate help with coping may occur because of parental anxiety. Anxious parents are more likely to endorse avoidant coping (Dadds and Barrett, 1996), and are more likely to express fearfulness in front of their children (Muris et al., 1996), possibly as a way of expressing empathy rather than being psychologically intrusive.
During tasks which were relatively unstructured and designed to reflect achievement and social themes, anxious parents of anxious children were more likely to respond with negative behaviours. Non-anxious parents of non-anxious children responded with more warmth. The behaviour of both groups of children mirrored that of their parents, thereby forming feedback loops (Williams et al., 2012).
Parents may interpret ambiguous circumstances as threatening, even when their children do not (Gifford et al., 2008). It may be that anxious parents disambiguate ambiguous situations for their children in an anxiety-fostering manner, thus training their children toward negative appraisals of situations. Children then learn to interpret situations as they would expect their mothers to do so for them (Lester et al., 2010). This may be mediated by information processing biases (Hadwin et al., 2006) such as attention to angry faces (Perez-Olivas et al., 2008). This overinvolvement is a form of over protection. It is the motivation behind the intervention which is crucial to understanding the family dynamic. It is possible to see that this would be a potential mechanism for the links commonly found between maternal and child dental fear (see below).
Anxious children may elicit overprotection which is then exacerbated by parental anxiety (Hudson and Rapee, 2002; Eley et al., 2010). Parental overinvolvement occurs with other, non-anxious, siblings as well as with the anxiety-disordered child (Hudson and Rapee, 2001). Regardless of their own anxiety level, mothers of anxious children are less warm, grant less autonomy and were more likely to catastrophise (Moore P.S. et al., 2004).
Whilst they are capable of accurately predicting, in anxiety provoking situations, the level of ‘challenge’ their children can undertake, parents overestimate the associated levels of distress that children experience and may thus be prompted to use inappropriate coping such as reassurance and overprotection (Cobham and Rapee, 1999). In the dental clinic parents also have a tendency to overestimate their child’s fear, though the parents of highly anxious children underestimated their fear (Krikken et al., 2012b), and the accuracy of such assessments has been called into question (Luoto et al., 2010).
A review (Themessl-Huber et al., 2010) demonstrated that, despite some mixed findings, an association was present between child and parental dental anxiety, though the origins may be various; modelling, informational as well as traumatic conditioning. Since this review, further studies have been published, mostly confirming an association (Olak et al., 2013; Tanaka et al., 2016; Vasiliki et al., 2016; Busato et al., 2017; Shinde and Hegde, 2017).
In the dental clinic parents can be very keen to jump in with information, which is often inaccurate and likely to foster anxiety. However, it is our experience that most parents do this only when they believe their child is not getting enough information. If the dentist truly is providing enough information to alleviate the child’s anxiety (and for some children, ‘less is more’) then this needs to be pointed out very carefully to the parent. Information should be combined with a stop signal and subjective units of distress scale (SUDS) to give an overt indicator of fear level and need for behavioural and informational control (Chapman and Kirby-Turner, 2002). This can then be pointed out to the mother. This process tends to contain maternal catastrophising. Similarly, the mother who, on the way to the appointment, answers an anxious child’s questions with information that reflects her own fears, can be contained by suggesting that the child has a notebook in which ‘Mummy helps you write down your question so that you don’t forget. Then the dentist can tell you what you want to know when you get there.’
A classic example of an overinvolvement and over protectiveness is that mother who, on bringing her toddler into the dental clinic for the first time for an examination says, “She’s [the dentist’s] not going to hurt you,” intending to reassure, but, instead, raising the possibility that the child will be hurt. This has been assessed as a problem with invasive medical procedures (McMurtry et al., 2010). However, some intrusive parenting witnessed in the dental clinic may not reflect the home situation; an anxious mother under pressure may display a different parenting style to the one she habitually uses. This may be because she is struggling to contain her own, situationally triggered anxieties, or because she fears being judged or shamed as an inadequate parent for ‘not being able to support or control’ her child in the clinic or for allowing them to develop dental decay.
Parental self-reports of parenting interactions differ from those observed in studies (Bennetts et al., 2016). Parents under pressure, such as those taking a frightened child to the dentist, theoretically may behave in subtly different ways to their normal behaviour, although the authors are unaware of any relevant literature. Care has to be taken with labelling parental behaviour as unhelpful as, in stressful situations, well-intentioned parental ‘helpful’ coping such as reassurance, criticism, apology, giving control to the child and empathy can backfire and promote distress in medical situations (Blount et al., 2001; Salmon and Pereira, 2002).
The children of depressed parents are more likely to develop internalising and externalising problems. In boys, but not girls, this is associated with intrusive parenting (Gruhn et al., 2016). As dentists, we often see whole families; parents will disclose their medical history. We should be mindful that current and previous parental depression may impact on the children’s ability to accept treatment.
Dentists often [more frequently in North American than in Europe (Marcum et al., 1995; Crossley and Joshi, 2002)] prefer to exclude parents on the basis that children behave better, that is are more compliant, when seen on their own (Marzo et al., 2003; Cox et al., 2011). For only mildly anxious children, it may be that, in the absence of the mother, they inhibit protest and thus appear to be fearless and more easily treated (Shaw and Routh, 1982). However, other stated reasons include that it wastes time and makes the dentist uncomfortable (Marcum et al., 1995). It is tempting to hypothesise that dentists themselves may find anxious, over-protective mothers psychologically intrusive; a threat to their sense of professional autonomy and sense of control. This has been established as an important factor in stress-related practise for dentists (Chapman et al., 2015). However, there are increasing parental requests to remain in the clinic (Shroff et al., 2015) and this is associated with greater levels of parental satisfaction with their child’s visit (Kim et al., 2012).
Effects on the Individual
Most of the research to date has been conducted on adolescents as it is believed that the greatest effects are seen within this age group. However, younger age groups are now being investigated using observational studies and children as young as 9 years old can report aspects of psychological control by their parents. We believe that aspects of parental behaviour may be apparent in clinical situations at an even younger age. The impact of childhood intrusive parenting on adults has received little attention in comparison.
Intrusive parenting serves to limit the child’s self-expression, define his emotional experience and inhibit his thinking processes (Barber, 2002). The child may be harmed in a number of ways:
• It limits free decision-making, self-expression and self-discovery.
• It controls self-will and reduces self-reliance, self-confidence, self-esteem, self-efficacy and self-regulation of emotions, all of which have implications for the ability to accept dental treatment.
• This interferes with psychosocial maturity (individuation, development of identity and individuality, independence, emotional autonomy) which usually helps to develop a sense of boundary between the self and the outside world. These boundaries may be culturally sensitive (Nucci and Smetana, 1996; Barber, 2002).
As well as the wealth of cross-sectional data for the detrimental effects of psychological control on children, longitudinal research (with children from the age of 5–6 years old to 7–8 years old) has found that maternal, but not paternal, psychological control, in combination with high levels affection, predicts levels of internalising and externalising disorders. Behavioural control, in combination with low levels of psychological control, decreased externalising problems (Aunola and Nurmi, 2005).
When separated from their parents and faced with, even routine tasks which are novel to them, children who are infantilized and have low self-efficacy suffer an increase in anxiety levels. This in turn causes distress and thus impairs learning and skills acquisition (Wood, 2006).
Psychological control (over-protection, lack of warmth and intrusiveness) appears to be related to the later childhood development of internalizing problems; withdrawn behaviour, passive resistance, eating disorders, suicidal ideation, somatic symptoms, simple phobias, separation anxiety disorder, depression, (though not generalised anxiety disorder) in cross-sectional (Arrindell et al., 1983; Gerlsma et al., 1990; Barber et al., 1994; Barber, 1996; Overbeek et al., 2004; Wood, 2006; Wood et al., 2007; Reitman and Asseff, 2010) and longitudinal studies (Enns et al., 2002). However, there are less consistent associations with externalising problems (aggression, antisocial behaviour, defiance and, most commonly, delinquency) (Barber et al., 1994; Barber, 1996; Barber and Harmon, 2002; Pettit and Laird, 2002). Overparenting is reported to have similar outcomes for children (Gar and Hudson, 2008). This association continues into emerging adulthood (Desjardins and Leadbeater, 2017).
Depending on the particular nature of parents’ psychological control, emerging adults reported both higher, and inappropriate, levels of dependence on parents with implications for emerging adults’ feelings about the upcoming transition to adulthood (Lindell et al., 2017). As young adults they have an increased sense of entitlement and higher levels of narcissism, believing that others can, and perhaps should, solve their problems and provide assistance and support. This is associated with ineffective coping skills (Segrin et al., 2012, 2013). It is theoretically possible that adult dental patients who are quick to be angry, rather than display anxiety (Linehan, 1993), have had this type of upbringing. The patient who demands appointment exactly when convenient to them, with no allowances for the complexities of the appointment book; their job, unlike other people’s is far too important to miss.
It may be that there are differential effects depending on gender, with only female anxiety being associated with maternal control and paternal acceptance (Reitman and Asseff, 2010).
Helicopter parenting in childhood is associated, in college students, with reduced engagement with education (Padilla-Walker and Nelson, 2012), higher levels of depression, less satisfaction with family life (Givertz and Segrin, 2014; Schiffrin et al., 2014), increased use of prescription medication to treat anxiety and depression and with the recreational consumption of pain pills (LeMoyne and Buchanan, 2011). The students’ reduced well-being is largely associated with reduced autonomy granting and perceived competence (Barnett et al., 2010; Schiffrin et al., 2014).
Ironically, helicopter parenting is also associated with positive aspects of parenting such as involvement, guidance, warmth, disclosure and emotional support (Padilla-Walker and Nelson, 2012). It does seem to hinder the development of adult independence (Lindell et al., 2017).
Parental over-involvement can lead to low self-esteem in adults (Winefield et al., 1990). Middle-aged adults who had been subject to parental control as children were found to have more problems with interpersonal relationships suggesting that interpersonal competence in childhood is an important influence on adult mental health (Rodgers, 1996a,b). This pattern may be influenced by the early maladaptive schemas developed as a result of intrusion; mistrust, shame, fear of abandonment. It persists into adult life and impacts on interpersonal relationships (Messman-Moore and Coates, 2007) and is associated with depression (Ono et al., 2017).
Adults whose parenting has been overinvolved or ‘helicopter’ show lower levels of self-efficacy (Givertz and Segrin, 2014; Darlow et al., 2017). The reduction in self-efficacy has been found to be associated with anxiety, depression, life satisfaction and physical health (Reed et al., 2016). Helicopter parenting has to be carefully distinguished from the related construct of ‘autonomy supporting’ which is directly related to life satisfaction and physical health (Reed et al., 2016). Low levels of self-efficacy have implications for preventive dental behaviours (Kakudate et al., 2010) and dental fear is linked to low self-efficacy in adults (Kent and Gibbons, 1987). It is therefore theoretically possible that self-efficacy mediates an association between intrusive parenting and child and adult dental fear.
Gelotophobia is the fear of being laughed at. This can be learned vicariously from parents, but is also associated with parental psychological control in childhood (Proyer et al., 2012) and, presumably, the threat of humiliation and being shamed.
Stalker et al. (2005) highlight the fact that victims of childhood sexual abuse (CSA) may be particularly vulnerable to perceived judgement and criticism. These patients have increased levels of dental fear (Willumsen, 2001, 2004). Many may have developed mental schema or beliefs about themselves as undeserving or bad, rendering ambiguous comments or ill-advised attempts at humour liable to be interpreted to fit these mental models of the self.
There is evidence that eating disorders may be associated with intrusive parenting (Rorty et al., 1994, 2000; Soenens et al., 2008; Ketisch et al., 2014) and some evidence that dental fear levels are raised in this group (Sirin et al., 2011). This suggests that when treating known and about-to-be-diagnosed (for example, the dentist notices severe palatal erosion) patients with eating disorders, dentists need to be mindful of the patients’ increased vulnerability to intrusion – putdowns, sarcasm, belittlement and perceived criticism.
We hypothesise that this learned model, which is internalised during childhood, can continue to function through childhood and into adulthood. It may be that a well-intentioned dentist can come to represent the intrusive parent. The balance between the concerned professional persisting in giving advice regarding diet and oral hygiene techniques may fall into this role. The quote below is from a dentist in a previous study (Chapman et al., 2015) who had seen that continual encouragement/nagging could be counterproductive.
“The patient who isn’t responding to your suggestions of tooth brushing, well, you still have to try to; you shouldn’t give up on them, even if they don’t respond. You’ve still got to try to motivate them; to get them to see why you’re telling them these things. Or else you just agree with them to disagree and warn them of the down sides of not complying with you. Effectively you say, look, I’ve told you how to do this; shown you. If you don’t, your mouth’s going to suffer, but if you’d rather I didn’t nag every time, let’s just agree that this is how things are and that you know that it would be the best for you that you do it.”
Psychological Intrusion in Dentistry – Evidence From the Literature
We have previously argued that psychological intrusion can be a problem for patients in the dental clinic (Chapman and Kirby-Turner, 1999; Chapman and Kirby-Turner, 2005). There are fewer indications that psychological intrusion has an impact on dental fear than for physical intrusion, but they are present. A summary of questionnaire items which might indicate a fear of psychological intrusion is presented in Table 1.
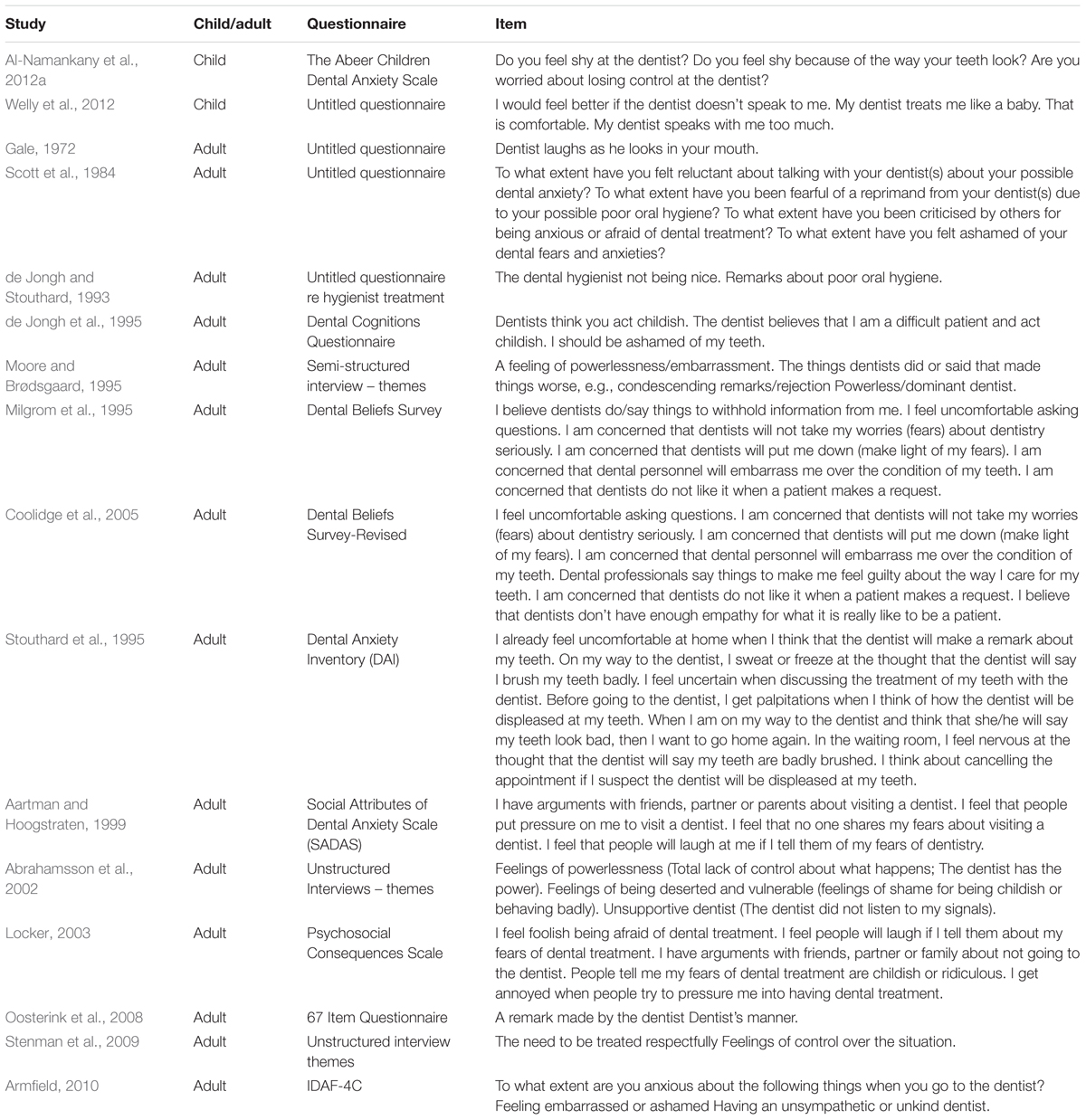
TABLE 1. Examples of items from various questionnaires revealing possible dental psychological intrusion.
In questionnaire measures used with older adolescents and adults a number of items suggest an element of psychological intrusion, though it is not possible to definitely assert this without a deeper understanding of the meaning of the question/fear to the patients concerned. For example, the item, “The dental hygienist not being nice,” (de Jongh and Stouthard, 1993) could mean different things to different people; Does the hygienist put you down? Is s/he generally grumpy? Does s/he nag?
Threats from intrusion to the definition of the self are often presented as threats to self-esteem within the dental literature (Stouthard and Hoogstraten, 1987; Chapman and Kirby-Turner, 1999, 2005). Poor self-esteem is associated with dental fear/anxiety (Stouthard and Hoogstraten, 1987; Schuurs et al., 1988; Kvale et al., 2002; Locker, 2003). Significant differences were found in the answers to questions (which could be interpreted as measuring threats to self-esteem) between fearful and non-fearful students (Scott et al., 1984). Success in accepting dental treatment is associated with an increase in reported self-esteem (Kvale et al., 2002).
Shame has been found to be related to dental anxiety (de Jongh et al., 1995; Abrahamsson et al., 2002; Armfield, 2010). In the dental literature this appears, sometimes, to be labelled as embarrassment (Moore R. et al., 2004) and is the result of ‘put downs’ (Moore et al., 1993). Later research (Moore et al., 1996) found that a history of putdowns was reported by 34.2% of Americans (and was significantly associated with avoidance) and 11.7% of Taiwanese. This implies a cultural element to this psychological threat to the sense of self as suggested by Nucci and Smetana (1996).
Belittlement forms part of the Dental Beliefs Survey (DBS) (Milgrom et al., 1995) and explains a significant proportion of dental fear; indeed Johansson and Berggren (1992) found that the most strongly correlated relationship was between dental fear and the belittlement subscale (‘Dentists make me feel guilty, Dentists don’t take my worries seriously. I worry what dentists think of me.’) of the DBS. It is interesting to note that although the original version of the Dental Beliefs Scale had a belittlement subscale, this was lost in the Revised Scale (Milgrom et al., 1995; Coolidge et al., 2005).
Moore et al. (1993) also noted a strong relationship between dental fear and the dentist being angry. We don’t know the meaning of this for the patients, but it may relate to humiliation, loss of control or fear of a more ‘powerful’ other; the angry dentist may be subconsciously representing the critical and/or angry parent (Linehan, 1993).
Intrusions often result from humiliation, sometimes as result of an unhelpful attempt at the use of humour, by the dentist, to lighten the atmosphere. This is reflected in items in Table 1.
The possible, differing interpretations of these items may be reflected in a change in importance of particular items in cross-sectional study. For example, ‘Dentist laughs while he looks in your mouth’ was found to be highly anxiety provoking by Gale (1972) but much less so in a later study (Stouthard and Hoogstraten, 1987). However, it is consistent with the development of gelotophobia as a result of intrusive parenting (Proyer et al., 2012).
The literature considering the effectiveness of the dental team behaviour on child anxiety relies largely on behavioural measures which are effectively measuring non/cooperation that may be associated with fear or dental non-compliance (DBMP), (Klingberg, 2008) but are often deemed to represent the absence of fear. Without understanding the meaning of the observed events for the children concerned, we propose that the following observations may reflect the impact of psychological intrusion by the dentist or team on child patients; putdowns, coaxing, coercion, (Weinstein et al., 1982) and punishment and criticism (Melamed et al., 1983). Zhou et al. (2012b) found that extended duty nurses (EDDNs) were more successful at completing fluoride applications when they used praise, instruction, and information-giving to guide the children’s behaviour compared to permission seeking, offering alternative tasks, information seeking and reassurance. However, a review of the literature suggests that findings from earlier research were inconsistent (Zhou et al., 2011). Children with externalizing behaviour (possibly reflected in the dental clinic as non-compliant DBMPs) may elicit intrusive mothering as a way of helping the children learn to self-regulate behaviour (Eisenberg et al., 2015). The detailed research examining clinician-child interactions (Weinstein et al., 1982; ten Berge et al., 1999; Zhou et al., 2012a) could be extended to examine the tripartite dentist-parent-child relationship for potentially intrusive adult behaviour.
In a study of treatment of highly fearful children, they were treated in a more authoritative and controlling way than lower fear children (ten Berge et al., 1999). Children who were more fearful were subject to significantly more ‘put downs,’ had their expressed feelings denied or ignored and were subject to significantly more physical restraint. They were also subject to more (non-significant) levels of coercion and coaxing. If an element of these children’s fears was based on intrusive parenting, this study suggests that fear may elicit intrusive behaviours from the dentists treating them. This would represent a vicious circle. The more fearful children improved more in the course of treatment than the non-compliant. However, given the relationship between externalising disorders and psychological intrusion, it is theoretically possible that fear of intrusion may also have been active in the non-compliant children with DBMPs. Traditional measures of child fearful behaviour are unlikely to identify the child who is afraid of intrusion by the dentist.
In a review, all identified self-report dental fear/anxiety questionnaires for children were found to rely on fear of situations/treatment (Al-Namankany et al., 2012b). The Abeer Children Dental Anxiety Scale (Al-Namankany et al., 2012a) was developed to contain a cognitive element, with questions apparently relating to embarrassment/shame – ‘Do you feel shy because of the way your teeth look?’ – and a need for control, but which might relate to intrusion. A word of caution is needed regarding the item, ‘Are you worried about losing control at the dentist?’ the meaning of this is ambiguous; does the child fear panicking or does the child fear not being able to control what is happening to him/her? Also, it is doubtful that many 6-year-olds would comprehend either meaning of this question. However, the questionnaire is validated with primary school children age 6–11. Another, untitled questionnaire (Welly et al., 2012), contains several items which may well represent intrusion (Table 1).
The boundaries between positive hypnotic suggestion and intrusive behaviour by the dentist are not at all obvious. Peretz (1996) gives a detailed description of the treatment of an anxious 11 year old boy. He describes structuring part of the conversation to end with four statements
“to which I was sure the boy would agree. (1) ‘I understand that you were in a few doctor’s offices before.’ (2) ‘I know you are afraid now.’ (3) ‘I understand that you are having pain in your teeth.’ And (4) ‘I see you want your teeth to be treated, but also, not to be so afraid”’ (p. 206).
Most children would accept these statements in the spirit in which they were intended; to convey understanding of his fear, predicament and wishes. For an individual who has been subject to psychological intrusion, these statements may have been interpreted very differently; as telling him how he is feeling and what he is thinking, thus removing any control of his own thought processes. This can be unsettling or frankly traumatic.
It raises the issue as to whether an individual who is vulnerable to psychological intrusion would actually present as hypnotisable or whether the fear of losing control over one’s own beliefs and thought processes might render them ‘unhypnotisable’ as a form of self-protection.
Implications for Dental Care
We have previously suggested that it is difficult to directly treat dental fear based in a fear of intrusion and that the problem has to be tackled by addressing other elements of the Chapman and Kirby-Turner model of dental fear (Chapman and Kirby-Turner, 1999, 2005). Children who are currently, and adults who have been, subject to psychological intrusion, may seize any opportunity to take whatever control of a situation they are offered or can take advantage of. This is probably the most important aspect of the model to address, though fear of betrayal, pain and the unknown are also important.
Control is the ability to personally influence events and outcomes in one’s environment, principally those related to positive or negative reinforcement (Chorpita and Barlow, 1998). When working with children, the degree of control shared with the child must be age appropriate. Control can be achieved through: behaviour (direct action on the environment), regulated administration, stimulus modification, cognitive, information gain, appraisal, and decisional control (having a choice among alternative courses of action) (Averill, 1973). There is a difference to be highlighted between experienced and objective control, both of which are achieved through decisional control (Law et al., 1994). Age appropriate objective control for a 3- year-old might be the choice between different coloured protective glasses, or whether to have the upper right teeth or the upper left teeth cleaned first with the electric toothbrush. For an adult, experienced control and objective control should be equivalent. In between there should be a sliding continuum along which experienced and objective control approximate.
A case we treated involved a needle phobic teenage girl who was subject to significant psychological control at home. She had previously, aged 8, had treatment under general anaesthetic and had been offered desensitisation immediately afterward. Despite being told that this was a routine procedure for children at this age, her mother had refused on the grounds that she was not old enough to manage it. (This was interpreted as over-protection and infantilization to maintain intrusive control.) Seven years later she needed a restoration replaced and she, herself, refused another general anaesthetic or sedation. HC took her through a CBT-based desensitization programme. At each stage, she initially refused to do the task which had previously been agreed upon; at each stage HC worked through the situation with her and pointed out that, on every previous occasion, she had eventually managed to complete the task. Eventually this stopped being effective and the girl explained that she felt that HC was over-riding her sense of control and acting rather like a ‘snake charmer’ and manipulating her to do things against her better judgement. Most young people would have seen such persuasion as a demonstration of faith in their ability to cope and complete the task, but, for this girl, it was an act of profound psychological intrusion. The impasse was eventually broken by HC giving her supervised control of a dental probe (explorer) to prod herself, eventually quite hard, to check, for herself, that the topical anaesthetic had worked.
Intrusive relationships are particularly difficult to deal with within the surgery. If subject to intrusive parenting, young children will have reduced self-efficacy. The child is likely to avoid situations of enforced separation from parents as they do not believe they can manage alone. Because they are not used to coping and problem solving on their own, they may be far more likely to catastrophically misinterpret ambiguous situations so care needs to be taken to shift at a slow enough pace, with sufficient explanations, to alleviate the child’s anxiety. On the other hand, the presence of the parent provides safety and reassurance thereby reducing child anxiety and negatively reinforcing the child (Bowlby, 1988). (Negatively reinforcing because of the removal of anxiety.) Thus, the child is likely to want to avoid a situation of enforced separation from parents and refusal to allow an intrusive parent to accompany their child, or prompt removal of an intrusive parent, is likely to provoke heightened child anxiety (see below).
We have found that the way to deal with this is to build a relationship with the child over several visits, during which the parent can witness that everything is explained to the child and that their own perceived ability to cope is monitored very carefully using a rating scale (Chapman and Kirby-Turner, 2002). During this induction phase of overtly non-threating treatment, such as a prophylaxis brush on the finger and then the teeth, the parent may well keep interrupting to check that the child is all right; “Are you sure you’re alright?” the implicit message to the child is, “Maybe you’re not OK.” However, it can then be pointed out to the parent that the child has a stop signal and hasn’t used it. The child can be asked if they needed to use the signal and ‘forgot’ to do so. Once a good relationship with the child is established, one of two outcomes are possible. Either the parent has relaxed and is far less anxious about the situation, is no longer trying to control it and is a help in the surgery – s/he has learned some coping skills, or the parent is still ‘interfering.’ In the latter situation, the dental nurse, at the next visit, requests the child to come by name from the waiting room, the child gets up spontaneously and makes no gesture to request the parent to accompany them, the parent can be encouraged to remain, with the caveat that if the child changes his/her mind, or the treatment plan changes, the parent will be invited into the surgery. The child may need to be prompted by a simple enquiry as to whether they would like to come on their own. The same caveats apply. This represents a confident child making age appropriate choices and who is separated from the parent without offence.
Despite being in obvious distress, some children are so reluctant to use a stop signal and make a control request, that they fail to use it. In these circumstances they have to be coached in its use. They can be instructed to request something ‘silly’ like needing to scratch their noses. Having practised this, they can then rehearse asking for a rest, before they need it. We hypothesis that this may be associated with a history of psychological control and/or behavioural inhibition.
The parent may behave in other unhelpful ways, but rather than ask them to leave, a tripartite system of working with the parent which fosters child independence and encourages the parent to ‘leave the child alone.’ For example, if the parent is touching too much toward the trunk, hands and face, they can be asked to sit at the foot of the dental chair and hold/stroke the child’s ankle. This tends to move the parent out of the child’s most intimate personal space and de-escalates the overprotectiveness of the physical contact.
The parent who keeps telling the child, presumably as a way to reassure, “It’s nearly finished,” when one has only just started, can be contained by explaining, in detail, with a guided tour of the cavity (including, via a mirror, the child if s/he would like to be), exactly why the filling is not nearly finished. The parent then can then be encouraged to look regularly and learns to give accurate feedback on how much better things are looking and sounding (a way of differentiating healthy from unhealthy dentine). They can become excited as progress occurs and this positive message of progress is helpful.
Because they are not used to coping and problem solving on their own, children who are psychologically controlled may be far more likely to catastrophically misinterpret ambiguous situations. False reassurance such as solicitous inquiries such as, “Are you OK?” “Are you sure it’s not hurting?” which occur despite a structured stop signal-fear thermometer combination being in place and not being used by the child, (Chapman and Kirby-Turner, 2002) only serve to increase fear. This can be gently addressed by acknowledging that the parent (usually mother) is only trying to ensure that the child is OK, but that her child’s experiences are different from those she had; that the child has had every opportunity to let the dentist know that s/he is not coping and has chosen not to do so. The child is than asked to confirm that s/he really would let the dentist know if there were a problem. This defuses the situation and allows the parent to stay with the child to provide a secure base; the presence of the parent provides safety and reassurance thereby reducing child anxiety and negatively reinforcing the child by of removal of anxiety (Bowlby, 1988).
Including the parent, wherever possible, in cognitive-behavioural type treatment of dental fear is consistent with the involvement of parent in the treatment of children with anxiety disorders (FCBT) and can lead to better outcomes (Creswell and Cartwright-Hatton, 2010; Hudson et al., 2014; Manassis et al., 2014). Indeed, there is some evidence that effectiveness of FCBT in treating anxiety disorders in children is mediated by a reduction in parental intrusiveness (Wood et al., 2006, 2009).
Some teenagers may feel that their parents are ‘interfering’ and may be heartily relieved to accede to a suggestion that they might like to come into the surgery alone. It is, however, essential that, as with younger children, the parent does not feel completely excluded or alienated.
Adults who have been subject to intrusive parenting are going to be particularly vulnerable to any situation in which they perceive that they are being laughed at, even if they are not diagnosed with gelotophobia. It behoves dentists, when using humour, to ensure that they are not perceived to be laughing at their patients. They are likely to need a high degree of control over their treatment and to be vulnerable to fear of betrayal. Recent reviews found that CBT and behaviour therapy had the most evidence of efficacy in the treatment of dental fear in adults (Gordon et al., 2013; Heaton, 2013), though even with this, care needs to be taken in the way patients are encouraged to challenge their negative thinking patterns as too great an enthusiasm in ‘helping’ with challenging negative automatic thoughts on the part of the dentist or therapist is open to interpretation as intrusion.
Finally, and no doubt controversially, we have to consider what is possibly the ultimate intrusion by dentists on child patients. A large variety of ‘child behaviour management’ techniques have been researched for effectiveness in helping children accept treatment, be that in terms of over-coming non-compliance or fear, the two often being confused (Klingberg, 2008). One of these is ‘escape and reward’ or contingent escape. There are variations of this procedure. The ‘poorly behaving’ child patient may be told that a procedure, be that in an introductory session (Allen and Stokes, 1987; Allen et al., 1988) or active treatment such as a prophylaxis or drilling (Allen et al., 1992), will continue until s/he behaves properly and then s/he will be given a rest. In another variation, the child is given regular breaks from treatment on a fixed time-schedule, independent of the child’s behaviour (O’Callaghan et al., 2006). This technique appears to be well accepted by parents (Elango et al., 2012). A more recent version of the technique is parental presence/absence or PPA; poorly behaved, uncooperative children are ‘empathically offered’ parental presence if they are cooperative (Molinari and DeYoung, 2004; Kotsanos et al., 2005, 2009). These techniques do appear to allow dentists to complete more clinical work, but at what price to the child’s mental well-being?
Conclusion
We believe that psychological intrusion plays an important role in the aetiology of some children’s dental fear and continues to affect individuals into adulthood. Belittlement and shaming experiences may be particularly salient. However, the relationships between child dental anxiety, child temperament (behavioural inhibition), parental (particularly maternal) dental anxiety and general anxiety, parenting style and intrusive parenting are complex.
Dentists may inadvertently act intrusively toward patients with negative consequences.
There is a need for detailed, good quality research to explore the extent and exact nature of these problems. The development of a simple, non-threatening means of helping dentists identify patients for whom psychological intrusion is a problem would be helpful.
Author Contributions
HC wrote the first draft and constructed the diagrams. NK-T was responsible for the original clinical observations and development of the idea. He contributed to and reviewed the content of the article and illustrations.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
Aartman, I. H., and Hoogstraten, J. (1999). Reliability and validity of the Dutch version of the social attributes of dental anxiety scale. Eur. J. Oral Sci. 107, 322–327. doi: 10.1046/j.0909-8836.1999.eos107502.x
Abrahamsson, K. H., Berggren, U., Hallberg, L., and Carlsson, S. G. (2002). Dental phobic patients’ view of dental anxiety and experiences in dental care: a qualitative study. Scand. J. Caring Sci. 16, 188–196. doi: 10.1046/j.1471-6712.2002.00083.x
Affrunti, N. W., and Ginsburg, G. S. (2012). Maternal overcontrol and child anxiety: the mediating role of perceived competence. Child Psychiatry Hum. Dev. 43, 102–112. doi: 10.1007/s10578-011-0248-z
Allen, K. D., Loiben, T., Allen, S. J., and Stanley, R. T. (1992). Dentist-implemented contingent escape for management of disruptive child behavior. J. Appl. Behav. Anal. 25, 629–636. doi: 10.1901/jaba.1992.25-629
Allen, K. D., Stark, L. J., Rigney, B. A., Nash, D. A., and Stokes, T. F. (1988). Reinforced practice of children’s cooperative behavior during restorative dental treatment. ASDC J. Dent. Child. 55, 273–277.
Allen, K. D., and Stokes, T. F. (1987). Use of escape and reward in the management of young children during dental treatment. J. Appl. Behav. Anal. 20, 381–390. doi: 10.1901/jaba.1987.20-381
Allen, K. D., and Wallace, D. P. (2013). Effectiveness of using noncontingent escape for general behavior management in a pediatric dental clinic. J. Appl. Behav. Anal. 46, 723–737. doi: 10.1002/jaba.82
Al-Namankany, A., Ashley, P., and Petrie, A. (2012a). The development of a dental anxiety scale with a cognitive component for children and adolescents. Pediatr. Dent. 34, 219–224.
Al-Namankany, A., De, S. M., and Ashley, P. (2012b). Evidence-based dentistry: analysis of dental anxiety scales for children. Br. Dent. J. 212, 219–222. doi: 10.1038/sj.bdj.2012.174
Aminabadi, N. A., Deljavan, A. S., Jamali, Z., Azar, F. P., and Oskouei, S. G. (2015). The influence of parenting style and child temperament on child-parent-dentist interactions. Pediatr. Dent. 37, 342–347.
Aminabadi, N. A., and Farahani, R. M. (2008). Correlation of parenting style and pediatric behavior guidance strategies in the dental setting: preliminary findings. Acta Odontol. Scand. 66, 99–104. doi: 10.1080/00016350802001322
Armfield, J. (2011). Australian population norms for the index of dental anxiety and fear (IDAF-4C). Aust. Dent. J. 56, 16–22. doi: 10.1111/j.1834-7819.2010.01279.x
Armfield, J. M. (2010). Development and psychometric evaluation of the index of dental anxiety and fear (IDAF-4C+). Psychol. Assess. 22, 279–287. doi: 10.1037/a0018678
Armfield, J. M., and Ketting, M. (2015). Predictors of dental avoidance among Australian adults with different levels of dental anxiety. Health Psychol. 34, 929–940. doi: 10.1037/hea0000186
Arnrup, K., Berggren, U., Broberg, A. G., and Bodin, L. (2004). A short-term follow-up of treatment outcome in groups of uncooperative child dental patients. Eur. J. Paediatr. Dent. 5, 216–224.
Arnrup, K., Broberg, A. G., Berggren, U., and Bodin, L. (2002). Lack of cooperation in pediatric dentistry–the role of child personality characteristics. Pediatr. Dent. 24, 119–128.
Arnrup, K., Broberg, A. G., Berggren, U., and Bodin, L. (2007). Temperamental reactivity and negative emotionality in uncooperative children referred to specialized paediatric dentistry compared to children in ordinary dental care. Int. J. Paediatr. Dent. 17, 419–429. doi: 10.1111/j.1365-263X.2007.00868.x
Arrindell, W. A., Emmelkamp, P. M., Monsma, A., and Brilman, E. (1983). The role of perceived parental rearing practices in the aetiology of phobic disorders: a controlled study. Br. J. Psychiatry 143, 183–187. doi: 10.1192/bjp.143.2.183
Aunola, K., and Nurmi, J.-E. (2005). The role of parenting styles in children’s problem behavior. Child Dev. 76, 1144–1159. doi: 10.1111/j.1467-8624.2005.00840.x-i1
Averill, J. R. (1973). Personal control over aversive stimuli and its relationship to stress. Psychol. Bull. 80, 286–303. doi: 10.1037/h0034845
Barber, B. K. (1996). Parental psychological control: Revisiting a neglected construct. Child Dev. 67, 3296–3319. doi: 10.2307/1131780
Barber, B. K. (2002). Intrusive Parenting: How Psychological Control Affects Children and Adolescents. Washington, DC: American Psychological Association. doi: 10.1037/10422-000
Barber, B. K., Bean, R. L., and Erickson, L. D. (2002). “Expanding the study and understanding of psychological control,” in Intrusive Parenting - How pychological Control Affects Children and Adolescents, ed. B. K. Barber (Washington, DC: American Psychological Association).
Barber, B. K., and Buehler, C. (1996). Family cohesion and enmeshment: different constructs, different effects. J. Marriage Fam. 58, 433–441. doi: 10.2307/353507
Barber, B. K., and Harmon, E. L. (2002). “Violating the self: Parental psychological control of children and adolescents,” in Intrusive Parenting - How Psychological Control Affects Children and Adolescents, ed. B. K. Barber (Washington, DC: American Psychological Association).
Barber, B. K., Olsen, J. E., and Shagle, S. C. (1994). Associations between parental psychological and behavioral control and youth internalized and externalized behaviors. Child Dev. 65, 1120–1136. doi: 10.2307/1131309
Barnett, M. A., and Scaramella, L. V. (2017). Supportive and intrusive parenting during early childhood: relations with children’s fear temperament and sex. J. Fam. Psychol. 31, 553–562. doi: 10.1037/fam0000304
Barnett, M. A., Shanahan, L., Deng, M., Haskett, M. E., and Cox, M. J. (2010). Independent and interactive contributions of parenting behaviors and beliefs in the prediction of early childhood behavior problems. Parent. Sci. Pract. 10, 43–59. doi: 10.1080/15295190903014604
Barrett, P. M., Dadds, M. R., and Rapee, R. M. (1996). Family treatment of childhood anxiety: a controlled trial. J. Consult. Clin. Psychol. 64, 333–342. doi: 10.1037/0022-006X.64.2.333
Baumrind, D. (1966). Effects of authoritative parental control on child behavior. Child Dev. 37, 887–907. doi: 10.2307/1126611
Baumrind, D. (2012). Differentiating between confrontive and coercive kinds of parental power-assertive disciplinary practices. Hum. Dev. 55, 35–51. doi: 10.1159/000337962
Beck, A. T., Rush, A. J., Shaw, B. F., and Emery, G. (1979). Cognitive Therapy of Depression. New York, NY: Guilford.
Bell, K. M., and Higgins, L. (2015). The impact of childhood emotional abuse and experiential avoidance on maladaptive problem solving and intimate partner violence. Behav. Sci. 5, 154–175. doi: 10.3390/bs5020154
Bennetts, S. K., Mensah, F. K., Westrupp, E. M., Hackworth, N. J., and Reilly, S. (2016). The agreement between parent-reported and directly measured child language and parenting behaviors. Front. Psychol. 7:1710. doi: 10.3389/fpsyg.2016.01710
Benoit Allen, K., Silk, J. S., Meller, S., Tan, P. Z., Ladouceur, C. D., Sheeber, L. B., et al. (2016). Parental autonomy granting and child perceived control: effects on the everyday emotional experience of anxious youth. J. Child Psychol. Psychiatry 57, 835–842. doi: 10.1111/jcpp.12482
Berg-Nielsen, T. S., Vikan, A., and Dahl, A. A. (2002). Parenting related to child and parental psychopathology: a descriptive review of the literature. Clin. Child Psychol. Psychiatry 7, 529–552. doi: 10.1177/1359104502007004006
Berryhill, M. B., Hayes, A., and Lloyd, K. (2018). Chaotic-enmeshment and anxiety: the mediating role of psychological flexibility and self-compassion. Contemp. Fam. Ther. 1–12. doi: 10.1007/S10591-018-9461-2
Blount, R. L., Bunke, V., Cohen, L. L., and Forbes, C. J. (2001). The child-adult medical procedure interaction scale-short form (CAMPIS-SF): validation of a rating scale for children’s and adults’ behaviors during painful medical procedures. J. Pain Symptom Manage. 22, 591–599. doi: 10.1016/S0885-3924(01)00303-7
Bowlby, J. (1988). A Secure Base: Parent-Child Attachment and Healthy Human Development. New York, NY: Basic Books.
Busato, P., Garbin, R. R., Santos, C. N., Paranhos, L. R., and Rigo, L. (2017). Influence of maternal anxiety on child anxiety during dental care: cross-sectional study. Sao Paulo Med. J. 135, 116–122. doi: 10.1590/1516-3180.2016.027728102016
Buss, K. A., and Kiel, E. J. (2011). Do maternal protective behaviors alleviate toddlers’ fearful distress? Int. J. Behav. Dev. 35, 136–143. doi: 10.1177/0165025410375922
Carrillo-Diaz, M., Crego, A., Armfield, J. M., and Romero, M. (2012). Self-assessed oral health, cognitive vulnerability and dental anxiety in children: testing a mediational model. Community Dent. Oral Epidemiol. 40, 8–16. doi: 10.1111/j.1600-0528.2011.00646.x
Carter, A. E., Carter, G., Boschen, M., Alshwaimi, E., and George, R. (2014). Pathways of fear and anxiety in dentistry: a review. World J. Clin. Cases 2, 642–653. doi: 10.12998/wjcc.v2.i11.642
Chapman, H. R., Chipchase, S. Y., and Bretherton, R. (2015). Understanding emotionally relevant situations in primary care dental practice: 1. Clinical situations and emotional responses. Br. Dent. J. 219, 401–409. doi: 10.1038/sj.bdj.2015.817
Chapman, H. R., and Kirby-Turner, N. (2002). Visual/verbal analogue scales: examples of brief assessment methods to aid management of child and adult patients in clinical practice. Br. Dent. J. 193, 447–450. doi: 10.1038/sj.bdj.4801593
Chapman, H. R., and Kirby-Turner, N. C. (1999). Dental fear in children–a proposed model. Br. Dent. J. 187, 408–412. doi: 10.1038/sj.bdj.4800293
Chapman, H. R., and Kirby-Turner, N. C. (2005). “The treatment of dental fear in children and adolescents - A cognitive-behavioural approach to the development of coping skills and their clinical application,” in New Research on the Psychology of Fear, ed. P. L. Gower (Hauppauge, NY: Nova Science Publishers).
Chorpita, B. F., and Barlow, D. H. (1998). The development of anxiety: the role of control in the early environment. Psychol. Bull. 124, 3–21. doi: 10.1037/0033-2909.124.1.3
Chronis-Tuscano, A., Rubin, K. H., O’brien, K. A., Coplan, R. J., Thomas, S. R., Dougherty, L. R., et al. (2015). Preliminary evaluation of a multimodal early intervention program for behaviorally inhibited preschoolers. J. Consult. Clin. Psychol. 83, 534–540. doi: 10.1037/a0039043
Cobham, V. E., and Rapee, R. M. (1999). Accuracy of predicting a child’s response to potential threat: a comparison of children and their mothers. Aust. J. Psychol. 51, 25–28. doi: 10.1080/00049539908255331
Coolidge, T., Heima, M., Coldwell, S. E., Weinstein, P., and Milgrom, P. (2005). Psychometric properties of the revised dental beliefs survey. Community Dent. Oral Epidemiol. 33, 289–297. doi: 10.1111/j.1600-0528.2005.00214.x
Cox, I. C., Krikken, J. B., and Veerkamp, J. S. (2011). Influence of parental presence on the child’s perception of, and behaviour, during dental treatment. Eur. Arch. Paediatr. Dent. 12, 200–204. doi: 10.1007/BF03262807
Crego, A., Carrillo-Diaz, M., Armfield, J. M., and Romero, M. (2013). Applying the cognitive vulnerability model to the analysis of cognitive and family influences on children’s dental fear. Eur. J. Oral Sci. 121, 194–203. doi: 10.1111/eos.12041
Creswell, C., and Cartwright-Hatton, S. (2010). Family treatment of child anxiety: outcomes, limitations and future directions. Clin. Child Fam. Psychol. Rev. 10, 232–252. doi: 10.1007/s10567-007-0019-3
Crossley, M. L., and Joshi, G. (2002). An investigation of paediatric dentists’ attitudes towards parental accompaniment and behavioural management techniques in the UK. Br. Dent. J. 192, 517–521. doi: 10.1038/sj.bdj.4801416
Dadds, M. R., and Barrett, P. M. (1996). Family processes in child and adolescent anxiety and depression. Behav. Change 13, 231–239. doi: 10.1017/S0813483900004836
Dagnan, D., Trower, P., and Gilbert, P. (2002). Measuring vulnerability to threats to self-construction: the self and other scale. Psychol. Psychother. 75, 279–293. doi: 10.1348/147608302320365271
Dagnan, D., Trower, P., and Smith, R. (1998). Care staff responses to people with learning disabilities and challenging behaviour: a cognitive-emotional analysis. Br. J. Clin. Psychol. 37, 59–68. doi: 10.1111/j.2044-8260.1998.tb01279.x
Darlow, V., Norvilitis, J. M., and Schuetze, P. (2017). The relationship between helicopter parenting and adjustment to college. J. Child Fam. Stud. 26, 2291–2298. doi: 10.1007/s10826-017-0751-3
de Jongh, A., Muris, P., Schoenmakers, N., and Ter, H. G. (1995). Negative cognitions of dental phobics: reliability and validity of the dental cognitions questionnaire. Behav. Res. Ther. 33, 507–515. doi: 10.1016/0005-7967(94)00081-T
de Jongh, A., and Stouthard, M. E. (1993). Anxiety about dental hygienist treatment. Community Dent. Oral Epidemiol. 21, 91–95. doi: 10.1111/j.1600-0528.1993.tb00728.x
de Oliveira, V., Da Costa, L. R., Marcelo, V. C., and Lima, A. R. (2006). Mothers’ perceptions of children’s refusal to undergo dental treatment: an exploratory qualitative study. Eur. J. Oral Sci. 114, 471–477. doi: 10.1111/j.1600-0722.2006.00405.x
Desjardins, T., and Leadbeater, B. J. (2017). Changes in parental emotional support and psychological control in early adulthood: direct and indirect associations with educational and occupational adjustment. Emerg. Adulthood 5, 177–190.
Dexter-Smith, S., Trower, P., Oyebode, J., and Dagnan, D. (2003). Psychometric evaluation and standardization of the self and other scale. J. Ration. Emot. Cogn. Behav. Ther. 21, 89–104. doi: 10.1023/A:1025047331048
Eisenberg, N., Taylor, Z. E., Widaman, K. F., and Spinrad, T. L. (2015). Externalizing symptoms, effortful control, and intrusive parenting: a test of bidirectional longitudinal relations during early childhood. Dev. Psychopathol. 27, 953–968. doi: 10.1017/S0954579415000620
Elango, I., Baweja, D. K., and Shivaprakash, P. K. (2012). Parental acceptance of pediatric behavior management techniques: a comparative study. J. Indian Soc. Pedod. Prev. Dent. 30, 195–200. doi: 10.4103/0970-4388.105010
Eley, T. C., Napolitano, M., Lau, J. Y., and Gregory, A. M. (2010). Does childhood anxiety evoke maternal control? A genetically informed study. J. Child Psychol. Psychiatry 51, 772–779. doi: 10.1111/j.1469-7610.2010.02227.x
Enns, M. W., Cox, B. J., and Clara, I. (2002). Parental bonding and adult psychopathology: results from the Us National Comorbidity Survey. Psychol. Med. 32, 997–1008. doi: 10.1017/S0033291702005937
Fenlon, W. L., Dabbs, A. R., and Curzon, M. E. (1993). Parental presence during treatment of the child patient: a study with British parents. Br. Dent. J. 174, 23–28. doi: 10.1038/sj.bdj.4808062
Gale, E. N. (1972). Fears of the dental situation. J. Dent. Res. 51, 964–966. doi: 10.1177/00220345720510044001
Gallitto, E. (2015). Temperament as a moderator of the effects of parenting on children’s behavior. Dev. Psychopathol. 27, 757–773. doi: 10.1017/S0954579414000753
Gar, N. S., and Hudson, J. L. (2008). An examination of the interactions between mothers and children with anxiety disorders. Behav. Res. Ther. 46, 1266–1274. doi: 10.1016/j.brat.2008.08.006
Geanellos, R. (2003). Understanding the need for personal space boundary restoration in women-client survivors of intrafamilial childhood sexual abuse. Int. J. Ment. Health Nurs. 12, 186–193. doi: 10.1046/j.1440-0979.2003.00288.x
Gerlsma, C., Emmelkamp, P. M., and Arrindell, W. A. (1990). Anxiety, depression, and perception of early parenting: a meta-analysis. Clin. Psychol. Rev. 10, 251–277. doi: 10.1016/0272-7358(90)90062-F
Gifford, S., Reynolds, S., Bell, S., and Wilson, C. (2008). Threat interpretation bias in anxious children and their mothers. Cogn. Emot. 22, 497–508. doi: 10.1080/02699930801886649
Givertz, M., and Segrin, C. (2014). The association between overinvolved parenting and young adults’ self-efficacy, psychological entitlement, and family communication. Commun. Res. 41, 1111–1136. doi: 10.1177/0093650212456392
Gordon, D., Heimberg, R. G., Tellez, M., and Ismail, A. I. (2013). A critical review of approaches to the treatment of dental anxiety in adults. J. Anxiety Disord. 27, 365–378. doi: 10.1016/j.janxdis.2013.04.002
Gruhn, M. A., Dunbar, J. P., Watson, K. H., Reising, M. M., Mckee, L., Forehand, R., et al. (2016). Testing specificity among parents’ depressive symptoms, parenting, and child internalizing and externalizing symptoms. J. Fam. Psychol. 30, 309–319. doi: 10.1037/fam0000183
Hadwin, J. A., Garner, M., and Perez-Olivas, G. (2006). The development of information processing biases in childhood anxiety: a review and exploration of its origins in parenting. Clin. Psychol. Rev. 26, 876–894. doi: 10.1016/j.cpr.2005.09.004
Hammock, S. J. (1999). Dental Anxiety and Behavioral Inhibition in Young Children. Dissertation Abstracts International: Section B: The Sciences and Engineering, Vol. 59. Available at: https://search-proquest-com.proxy.library.lincoln.ac.uk/pqdtglobal/results/152D72613CA425EPQ/1?accountid=16461
Heaton, L. J. (2013). Behavioral interventions may reduce dental anxiety and increase acceptance of dental treatment in dentally fearful adults. J. Evid. Based Dent. Pract. 13, 160–162. doi: 10.1016/j.jebdp.2013.10.008
Howenstein, J., Kumar, A., Casamassimo, P. S., Mctigue, D., Coury, D., and Yin, H. (2015). Correlating parenting styles with child behavior and caries. Pediatr. Dent. 37, 59–64.
Hudson, J. L., Newall, C., Rapee, R. M., Lyneham, H. J., Schniering, C. C., Wuthrich, V. M., et al. (2014). The impact of brief parental anxiety management on child anxiety treatment outcomes: a controlled trial. J. Clin. Child Adolesc. Psychol. 43, 370–380. doi: 10.1080/15374416.2013.807734
Hudson, J. L., and Rapee, R. M. (2001). Parent–child interactions and anxiety disorders: an observational study. Behav. Res. Ther. 39, 1411–1427. doi: 10.1016/S0005-7967(00)00107-8
Hudson, J. L., and Rapee, R. M. (2002). Parent-child interactions in clinically anxious children and their siblings. J. Clin. Child Adolesc. Psychol. 31, 548–555. doi: 10.1207/S15374424JCCP3104_13
Humphris, G., Crawford, J. R., Hill, K., Gilbert, A., and Freeman, R. (2013). UK population norms for the modified dental anxiety scale with percentile calculator: adult dental health survey 2009 results. BMC Oral Health 13:29. doi: 10.1186/1472-6831-13-29
Janssen, I. (2015). Hyper-parenting is negatively associated with physical activity among 7–12 year olds. Prev. Med. 73, 55–59. doi: 10.1016/j.ypmed.2015.01.015
Johansson, P., and Berggren, U. (1992). Assessment of dental fear. A comparison of two psychometric instruments. Acta Odontol. Scand. 50, 43–49. doi: 10.3109/00016359209012745
Kagan, J. (1997). Conceptualizing psychopathology: the importance of developmental profiles. Dev. Psychopathol. 9, 321–334. doi: 10.1017/S0954579497002071
Kagan, J., Snidman, N., Arcus, D., and Reznick, J. S. (1994). Galen’s Prophecy: Temperament in Human Nature. New York, NY: Basic Books.
Kagan, J., Snidman, N., Kahn, V., and Towsley, S. (2007). The preservation of two infant temperaments into adolescence. Monogr. Soc. Res. Child Dev. 72, 1–75.
Kakudate, N., Morita, M., Fukuhara, S., Sugai, M., Nagayama, M., Kawanami, M., et al. (2010). Application of self-efficacy theory in dental clinical practice. Oral Dis. 16, 747–752. doi: 10.1111/j.1601-0825.2010.01703.x
Kent, G., and Gibbons, R. (1987). Self-efficacy and the control of anxious cognitions. J. Behav. Ther. Exp. Psychiatry 18, 33–40. doi: 10.1016/0005-7916(87)90069-3
Ketisch, T., Jones, R., Mirsalimi, H., Casey, R., and Milton, T. (2014). Boundary disturbances and eating disorder symptoms. Am. J. Fam. Ther. 42, 438–451. doi: 10.1080/01926187.2014.912103
Kiel, E. J., and Buss, K. A. (2010). Maternal accuracy and behavior in anticipating children’s responses to novelty: relations to fearful temperament and implications for anxiety development. Soc. Dev. 19, 304–325. doi: 10.1111/j.1467-9507.2009.00538.x
Kiel, E. J., and Buss, K. A. (2013). Toddler inhibited temperament, maternal cortisol reactivity and embarrassment, and intrusive parenting. J. Fam. Psychol. 27, 512–517. doi: 10.1037/a0032892
Kiel, E. J., and Maack, D. J. (2012). Maternal BIS sensitivity, overprotective parenting, and children’s internalizing behaviors. Pers. Individ. Differ. 53, 257–262. doi: 10.1016/j.paid.2012.03.026
Kim, J. S., Boynton, J. R., and Inglehart, M. R. (2012). Parents’ presence in the operatory during their child’s dental visit: a person-environmental fit analysis of parents’ responses. Pediatr. Dent. 34, 407–413.
Kivisto, K. L., Welsh, D. P., Darling, N., and Culpepper, C. L. (2015). Family enmeshment, adolescent emotional dysregulation, and the moderating role of gender. J. Fam. Psychol. 29, 604–613. doi: 10.1037/fam0000118
Klingberg, G. (2008). Dental anxiety and behaviour management problems in paediatric dentistry — a review of background factors and diagnostics. Eur. Arch. Paediatr. Dent. 9, 11–15. doi: 10.1007/BF03262650
Klingberg, G., and Broberg, A. G. (1998). Temperament and child dental fear. Pediatr. Dent. 20, 237–243.
Klingberg, G., and Broberg, A. G. (2007). Dental fear/anxiety and dental behaviour management problems in children and adolescents: a review of prevalence and concomitant psychological factors. Int. J Paediatr. Dent. 17, 391–406. doi: 10.1111/j.1365-263X.2007.00872.x
Kotsanos, N., Arhakis, A., and Coolidge, T. (2005). Parental presence versus absence in the dental operatory: a technique to manage the uncooperative child dental patient. Eur. J. Paediatr. Dent. 6, 144–148.
Kotsanos, N., Coolidge, T., Velonis, D., and Arapostathis, K. N. (2009). A form of ’parental presence/absence’ (PPA) technique for the child patient with dental behaviour management problems. Eur. Arch. Paediatr. Dent. 10, 90–92. doi: 10.1007/BF03321607
Krikken, J. B., Van Wijk, A. J., Ten Cate, J. M., and Veerkamp, J. S. J. (2012a). Child dental anxiety, parental rearing style and referral status of children. Community Dent. Health 29, 289–292.
Krikken, J. B., Van Wijk, A. J., Ten Cate, J. M., and Veerkamp, J. S. J. (2012b). Measuring dental fear using the CFSS-DS. Do children and parents agree? Int. J. Paediatr. Dent. 23, 94–100. doi: 10.1111/j.1365-263X.2012.01228.x
Krikken, J. B., Vanwijk, A. J., Tencate, J. M., and Veerkamp, J. S. (2013). Child dental anxiety, parental rearing style and dental history reported by parents. Eur. J. Paediatr. Dent. 14, 258–262.
Krikken, J. B., and Veerkamp, J. S. J. (2008). Child rearing styles, dental anxiety and disruptive behaviour; an exploratory study. Eur. Arch. Paediatr. Dent. 9(Suppl. 1), 23–28. doi: 10.1007/BF03262652
Kvale, G., Raadal, M., Vika, M., Johnsen, B. H., Skaret, E., Vatnelid, H., et al. (2002). Treatment of dental anxiety disorders. Outcome related to DSM-IV diagnoses. Eur. J. Oral Sci. 110, 69–74. doi: 10.1034/j.1600-0722.2002.11204.x
Law, A., Logan, H., and Baron, R. S. (1994). Desire for control, felt control, and stress inoculation training during dental treatment. J. Pers. Soc. Psychol. 67, 926–936. doi: 10.1037/0022-3514.67.5.926
LeMoyne, T., and Buchanan, T. (2011). Does “hovering” matter? Helicopter paretning and its effect on well-being. Sociol. Spect. 31, 399–418. doi: 10.1080/02732173.2011.574038
Lester, K. J., Seal, K., Nightingale, Z. C., and Field, A. P. (2010). Are children’s own interpretations of ambiguous situations based on how they perceive their mothers have interpreted ambiguous situations for them in the past? J. Anxiety Disord. 24, 102–108. doi: 10.1016/j.janxdis.2009.09.004
Lindell, A. K., Campione-Barr, N., and Killoren, S. E. (2017). Implications of parent–child relationships for emerging adults’ subjective feelings about adulthood. J. Fam. Psychol. 31, 810–820. doi: 10.1037/fam0000328
Linehan, M. M. (1993). Skills Training Manual for Treating Borderline Personality Disorder. New York, NY: Guilford Press.
Locker, D. (2003). Psychosocial consequences of dental fear and anxiety. Community Dent. Oral Epidemiol. 31, 144–151. doi: 10.1034/j.1600-0528.2003.00028.x
Lundgren, J., Elfstrom, M. L., and Berggren, U. (2007). The relationship between temperament and fearfulness in adult dental phobic patients. Int. J. Paediatr. Dent. 17, 460–468. doi: 10.1111/j.1365-263X.2007.00880.x
Luoto, A., Tolvanen, M., Rantavuori, K., Pohjola, V., and Lahti, S. (2010). Can parents and children evaluate each other’s dental fear? Eur. J. Oral Sci. 118, 254–258. doi: 10.1111/j.1600-0722.2010.00727.x
Maccoby, E. E., and Martin, J. A. (1983). “Socialization in the context of the family: parent-child interaction,” in Handbook of Child Psychology: Vol. 4. Socialization, Personality, and Social Development, eds P. H. Mussen and E. M. Hetherington (New York, NY: Wiley).
Manassis, K., Lee, T. C., Bennett, K., Zhao, X. Y., Mendlowitz, S., Duda, S., et al. (2014). Types of parental involvement in Cbt with anxious youth: a preliminary meta-analysis. J. Consult. Clin. Psychol. 82, 1163–1172. doi: 10.1037/a0036969
Marcum, B. K., Turner, C., and Courts, F. J. (1995). Pediatric dentists’ attitudes regarding parental presence during dental procedures. Pediatr. Dent. 17, 432–436.
Marzo, G., Campanella, V., Albani, F., and Gallusi, G. (2003). Psychological aspects in paediatric dentistry: parental presence. Eur. J. Paediatr. Dent. 4, 177–180.
McMurtry, C. M., Chambers, C. T., Mcgrath, P. J., and Asp, E. (2010). When “don’t worry” communicates fear: children’s perceptions of parental reassurance and distraction during a painful medical procedure. Pain 150, 52–58. doi: 10.1016/j.pain.2010.02.021
Melamed, B. G., Bennett, C. G., Jerrell, G., Ross, S. L., Bush, J. P., Hill, C., et al. (1983). Dentists’ behavior management as it affects compliance and fear in pediatric patients. J. Am. Dent. Assoc. 106, 324–330. doi: 10.14219/jada.archive.1983.0055
Messman-Moore, T. L., and Coates, A. A. (2007). The impact of childhood psychological abuse on adult interpersonal conflict: the role of early maladaptive schemas and patterns of interpersonal behavior. J. Emot. Abuse 7, 75–92. doi: 10.1300/J135v07n02_05
Milgrom, P., Weinstein, P., and Getz, T. (1995). Treating Fearful Dental Patients - A Patient Management Handbook. Seattle, WA: University of Washington.
Molinari, G. E., and DeYoung, A. (2004). Parental presence and absence as a behavior management technique. J. Mich. Dent. Assoc. 86, 30–33.
Moore, P. S., Whaley, S. E., and Sigman, M. (2004). Interactions between mothers and children: impacts of maternal and child anxiety. J. Abnorm. Psychol. 113, 471–476. doi: 10.1037/0021-843X.113.3.471
Moore, R., Birn, H., Kirkegaard, E., Brodsgaard, I., and Scheutz, F. (1993). Prevalence and characteristics of dental anxiety in Danish adults. Community Dent. Oral Epidemiol. 21, 292–296. doi: 10.1111/j.1600-0528.1993.tb00777.x
Moore, R., Brodsgaard, I., and Rosenberg, N. (2004). The contribution of embarrassment to phobic dental anxiety: a qualitative research study. BMC Psychiatry 4:10. doi: 10.1186/1471-244X-4-10
Moore, R., and Brødsgaard, I. (1995). Differential diagnosis of odontophobic patients using the DSM-IV. Eur. J. Oral Sci. 103, 121–126. doi: 10.1111/j.1600-0722.1995.tb00129.x
Moore, R., Brodsgaard, I., Mao, T. K., Kwan, H. W., Shiau, Y. Y., and Knudsen, R. (1996). Fear of injections and report of negative dentist behavior among Caucasian American and Taiwanese adults from dental school clinics. Community Dent. Oral Epidemiol. 24, 292–295. doi: 10.1111/j.1600-0528.1996.tb00862.x
Muris, P., Steerneman, P., Merckelbach, H., and Meesters, C. (1996). The role of parental fearfulness and modeling in children’s fear. Behav. Res. Ther. 34, 265–268. doi: 10.1016/0005-7967(95)00067-4
Nelson, D. A., and Crick, N. R. (2002). “Parental psychological control: Implications for childhood physical and relational aggression,” in Psychological Control of Children and Adolescents, ed. B. K. Barber (Washington, DC: American Psychological Association).
Nucci, L., and Smetana, J. G. (1996). Mothers’ concept of young children’s areas of personal freedom. Child Dev. 67, 1870–1886. doi: 10.2307/1131737
O’Callaghan, P. M., Allen, K. D., Powell, S., and Salama, F. (2006). The efficacy of noncontingent escape for decreasing children’s disruptive behavior during restorative dental treatment. J. Appl. Behav. Anal. 39, 161–171. doi: 10.1901/jaba.2006.79-05
Olak, J., Saag, M., Honkala, S., Nõmmela, R., Runnel, R., Honkala, E., et al. (2013). Children’s dental fear in relation to dental health and parental dental fear. Stomatologija 15, 26–31.
Ollendick, T. H., and Horsch, L. M. (2007). Fears in clinic-referred children: relations with child anxiety sensitivity, maternal overcontrol, and maternal phobic anxiety. Behav. Ther. 38, 402–411. doi: 10.1016/j.beth.2006.12.001
Olsen, S. F., Yang, C., Hart, C. H., Robinson, C. C., Wu, P., Nelson, D. A., et al. (2002). “Maternal psychological control and preschool children’s behavioral outcomes in China, Russia, and the United States,” in Intrusive Parenting: How Psychological Control Affects Children and Adolescents ed. B. K. Barber (Washington, DC: American Psychological Association).
Ono, Y., Takaesu, Y., Nakai, Y., Ichiki, M., Masuya, J., Kusumi, I., et al. (2017). The influence of parental care and overprotection, neuroticism and adult stressful life events on depressive symptoms in the general adult population. J. Affect. Disord. 217, 66–72. doi: 10.1016/j.jad.2017.03.058
Oosterink, F. M. D., De Jongh, A., and Aartman, I. H. A. (2008). What are people afraid of during dental treatment? Anxiety-provoking capacity of 67 stimuli characteristic of the dental setting. Eur. J. Oral Sci. 116, 44–51. doi: 10.1111/j.1600-0722.2007.00500.x
Overbeek, G., Vollebergh, W., Meeus, W., De Graaf, R., and Engels, R. C. M. E. (2004). Young adults’ recollections of parental bonds: Does satisfaction with partner relationships mediate the longitudinal association with mental disorders? Soc. Psychiatry Psychiatr. Epidemiol. 39, 703–710. doi: 10.1007/s00127-004-0806-9
Padilla-Walker, L. M., and Nelson, L. J. (2012). Black hawk down?: Establishing helicopter parenting as a distinct construct from other forms of parental control during emerging adulthood. J. Adolesc. 35, 1177–1190. doi: 10.1016/j.adolescence.2012.03.007
Parker, G., Tupling, H., and Brown, L. B. (1979). A parental bonding instrument. Br. J. Med. Psychol. 52, 1–10. doi: 10.1111/j.2044-8341.1979.tb02487.x
Paulus, F. W., Backes, A., Sander, C. S., Weber, M., and Von Gontard, A. (2015). Anxiety disorders and behavioral inhibition in preschool children: a population-based study. Child Psychiatry Hum. Dev. 46, 150–157. doi: 10.1007/s10578-014-0460-8
Peretz, B. (1996). Relaxation and hypnosis in pediatric dental patients. J. Clin. Pediatr. Dent. 20, 205–207.
Perez-Olivas, G., Stevenson, J., and Hadwin, J. A. (2008). Do anxiety-related attentional biases mediate the link between maternal over involvement and separation anxiety in children? Cogn. Emot. 22, 509–521. doi: 10.1080/02699930801886656
Pettit, G. S., and Laird, R. D. (2002). “Psychological control and monitoring in early adolescence: the role of parental involvement and earlier child adjustment,” in Intrusive Parenting: How Psychological Control Affects Children and Adolescents, ed. B. K. Barber (Washington, DC: American Psychological Association).
Proyer, R. T., Estoppey, S., and Ruch, W. (2012). An initial study on how families deal with ridicule and being laughed at: parenting styles and parent–child relations with respect to gelotophobia, gelotophilia, and katagelasticism. J. Adult Dev. 19, 228–237. doi: 10.1007/s10804-012-9150-6
Quinonez, R., Santos, R. G., Boyar, R., and Cross, H. (1997). Temperament and trait anxiety as predictors of child behavior prior to general anesthesia for dental surgery. Pediatr. Dent. 19, 427–431.
Radis, F. G., Wilson, S., Griffen, A. L., and Coury, D. L. (1994). Temperament as a predictor of behavior during initial dental examination in children. Pediatr. Dent. 16, 121–127.
Rapee, R. M. (2002). The development and modification of temperamental risk for anxiety disorders: prevention of a lifetime of anxiety? Biol. Psychiatry 52, 947–957. doi: 10.1016/S0006-3223(02)01572-X
Raudino, A., Murray, L., Turner, C., Tsampala, E., Lis, A., De Pascalis, L., et al. (2013). Child anxiety and parenting in England and Italy: the moderating role of maternal warmth. J. Child Psychol. Psychiatry 54, 1318–1326. doi: 10.1111/jcpp.12105
Reed, K., Duncan, J. M., Lucier-Greer, M., Fixelle, C., and Ferraro, A. J. (2016). Helicopter parenting and emerging adult self-efficacy: implications for mental and physical health. J. Child Fam. Stud. 25, 3136–3149. doi: 10.1007/s10826-016-0466-x
Reitman, D., and Asseff, J. (2010). Parenting practices and their relation to anxiety in young adulthood. J. Anxiety Disord. 24, 565–572. doi: 10.1016/j.janxdis.2010.03.016
Robinson, C. C., Mandleco, B., Olsen, S. F., and Hart, C. H. (1995). Authoritative, authoritarian, and permissive parenting practices: development of a new measure. Psychol. Rep. 77, 819–830. doi: 10.2466/pr0.1995.77.3.819
Rodgers, B. (1996a). Reported parental behaviour and adult affective symptoms. 1. Associations and moderating factors. Psychol. Med. 26, 51–61. doi: 10.1017/S0033291700033717
Rodgers, B. (1996b). Reported parental behaviour and adult affective symptoms. 2. Mediating factors. Psychol. Med. 26, 63–77. doi: 10.1017/S0033291700033729
Rorty, M., Yager, J., and Rossotto, E. (1994). Childhood sexual, physical, and psychological abuse in bulimia nervosa. Am. J. Psychiatry 151, 1122–1126. doi: 10.1176/ajp.151.8.1122
Rorty, M., Yager, J., Rossotto, E., and Buckwalter, G. (2000). Parental intrusiveness in adolescence recalled by women with a history of bulimia nervosa and comparison women. Int. J. Eat. Disord. 28, 202–208. doi: 10.1002/1098-108X(200009)28:2<202::AID-EAT9>3.0.CO;2-G
Rowsell, M., Doyle, S., and Francis, S. E. (2016). The role of BIS sensitivity in the relationship between family enmeshment and child anxiety. J. Child Fam. Stud. 25, 2585–2596. doi: 10.1007/s10826-016-0415-8
Rubin, K. H., Burgess, K. B., and Hastings, P. D. (2002). Stability and social-behavioral consequences of toddlers’ inhibited temperament and parenting behaviors. Child Dev. 73, 483–495. doi: 10.1111/1467-8624.00419
Salmon, K., and Pereira, J. K. (2002). Predicting children’s response to an invasive medical investigation: the influence of effortful control and parent behavior. J. Pediatr. Psychol. 27, 227–233. doi: 10.1093/jpepsy/27.3.227
Sanders, B., and Becker-Lausen, E. (1995). The measurement of psychological maltreatment: early data on the Child Abuse and Trauma Scale. Child Abuse Negl. 19, 315–323. doi: 10.1016/S0145-2134(94)00131-6
Schiffrin, H. H., Liss, M., Miles-Mclean, H., Geary, K. A., Erchull, M. J., and Tashner, T. (2014). Helping or hovering? The effects of helicopter parenting on college students’ well-being. J. Child Fam. Stud. 23, 548–557. doi: 10.1007/s10826-013-9716-3
Schuurs, A. H., Duivenvoorden, H. J., Makkes, P. C., Thoden, V., and Verhage, F. (1988). Personality traits of patients suffering extreme dental anxiety. Community Dent. Oral Epidemiol. 16, 38–41. doi: 10.1111/j.1600-0528.1988.tb00552.x
Schwartz, C. E., Wright, C. I., Shin, L. M., Kagan, J., and Rauch, S. L. (2003). Inhibited and uninhibited infants “grown up”: adult amygdalar response to novelty. Science 300, 1952–1953. doi: 10.1126/science.1083703
Scott, A. L. (1993). A beginning theory of personal space boundaries. Perspect. Psychiatr. Care 29, 12–21. doi: 10.1111/j.1744-6163.1993.tb00407.x
Scott, D. S., Hirschman, R., and Schroder, K. (1984). Historical antecedents of dental anxiety. J. Am. Dent. Assoc. 108, 42–45. doi: 10.14219/jada.archive.1984.0207
Segrin, C., Woszidlo, A., Givertz, M., Bauer, A., and Murphy, M. T. (2012). The association between overparenting, parent-child communication, and entitlement and adaptive traits in adult children. Fam. Relat. 61, 237–252. doi: 10.1111/j.1741-3729.2011.00689.x
Segrin, C., Woszidlo, A., Givertz, M., and Montgomery, N. (2013). Parent and child traits associated with overparenting. J. Soc. Clin. Psychol. 32, 569–595. doi: 10.1521/jscp.2013.32.6.569
Seligman, L. D., Hovey, J. D., Chacon, K., and Ollendick, T. H. (2017). Dental anxiety: An understudied problem in youth. Clin. Psychol. Rev. 55, 25–40. doi: 10.1016/j.cpr.2017.04.004
Shaw, E. G., and Routh, D. K. (1982). Effect of mother presence on children’s reaction to aversive procedures. J. Pediatr. Psychol. 7, 33–42. doi: 10.1093/jpepsy/7.1.33
Shinde, S. D., and Hegde, R. J. (2017). Evaluation of the influence of parental anxiety on children’s behavior and understanding children’s dental anxiety after sequential dental visits. Indian J. Dent. Res. 28, 22–26. doi: 10.4103/ijdr.IJDR_181_16
Shroff, S., Hughes, C., and Mobley, C. (2015). Attitudes and preferences of parents about being present in the dental operatory. Pediatr. Dent. 37, 51–55.
Silk, J. S., Morris, A. S., Kanaya, T., and Steinberg, L. (2003). Psychological control and autonomy granting: opposite ends of a continuum or distinct constructs? J. Res. Adolesc. 13, 113–28. doi: 10.1111/1532-7795.1301004
Sirin, Y., Yucel, B., Firat, D., and Husseinova-Sen, S. (2011). Assessment of dental fear and anxiety levels in eating disorder patients undergoing minor oral surgery. J. Oral Maxillofac. Surg. 69, 2078–2085. doi: 10.1016/j.joms.2010.12.050
Smetana, J. G., and Daddis, C. (2002). Domain-specific antecedents of parental psychological control and monitoring: the role of parenting beliefs and practices. Child Dev. 73, 563–580. doi: 10.1111/1467-8624.00424
Soenens, B., Vansteenkiste, M., Duriez, B., and Goossens, L. (2006). In search of the sources of psychologically controlling parenting: the role of parental separation anxiety and parental maladaptive perfectionism. J. Res. Adolesc. 16, 539–559. doi: 10.1111/j.1532-7795.2006.00507.x
Soenens, B., Vansteenkiste, M., Vandereycken, W., Luyten, P., Sierens, E., and Goossens, L. (2008). Perceived parental psychological control and eating-disordered symptoms: maladaptive perfectionism as a possible intervening variable. J. Nerv. Ment. Dis. 196, 144–152. doi: 10.1097/NMD.0b013e318162aabf
Sroufe, L. A., Bennett, C., Englund, M., and Urban, J. (1993). The significance of gender boundaries in preadolescence: contemporary correlates and antecedents of boundary violation and maintenance. Child Dev. 64, 455–466. doi: 10.2307/1131262
Stalker, C. A., Russell, B. D., Teram, E., and Schachter, C. L. (2005). Providing dental care to survivors of childhood sexual abuse: treatment considerations for the practitioner. J. Am. Dent. Assoc. 136, 1277–1281. doi: 10.14219/jada.archive.2005.0344
Stenebrand, A., Wide, B. U., and Hakeberg, M. (2013). Dental anxiety and temperament in 15-year olds. Acta Odontol. Scand. 71, 15–21. doi: 10.3109/00016357.2011.645068
Stenman, J., Hallberg, U., Wennstrom, J. L., and Abrahamsson, K. H. (2009). Patients’ attitudes towards oral health and experiences of periodontal treatment: a qualitative interview study. Oral Health Prev. Dent. 7, 393–401.
Stone, G., Buehler, C., and Barber, B. K. (2002). “Interparental conflict, parental psychological control, and youth problem behavior,” in Intrusive Parenting - How Psychological Control Affects Children and Adolescents, ed. B. K. Barber (Washington, DC: American Psychological Association).
Stouthard, M. E., Hoogstraten, J., and Mellenbergh, G. J. (1995). A study on the convergent and discriminant validity of the dental anxiety inventory. Behav. Res. Ther. 33, 589–595. doi: 10.1016/0005-7967(94)00096-3
Stouthard, M. E. A., and Hoogstraten, J. (1987). Ratings of fears associated with twelve dental situations. J. Dent. Res. 66, 1175–1178. doi: 10.1177/00220345870660061601
Tanaka, S., Uehara, N., Tsuchihashi, N., and Sugimoto, K. (2016). Emotional relationships between child patients and their mothers during dental treatments. J. Dent. Sci. 11, 287–292. doi: 10.1016/j.jds.2016.03.003
ten Berge, M. (2003). “Dental fear in children: assessment, prevalence and etiology,” in Psychology of Fear, ed. P. L. Gower (New York, NY: Nova Science).
ten Berge, M., Veerkamp, J., and Hoogstraten, J. (1999). Dentists’ behavior in response to child dental fear. ASDC J. Dent. Child 66, 36–40, 12.
ten Berge, M., Veerkamp, J. S., Hoogstraten, J., and Prins, P. J. (2001). Parental beliefs on the origins of child dental fear in The Netherlands. ASDC J. Dent. Child 68, 51–54.
ten Berge, M., Veerkamp, J. S., Hoogstraten, J., and Prins, P. J. (2003). Childhood dental fear in relation to parental child-rearing attitudes. Psychol. Rep. 92, 43–50. doi: 10.2466/pr0.2003.92.1.43
Themessl-Huber, M., Freeman, R., Humphris, G., Macgillivray, S., and Terzi, N. (2010). Empirical evidence of the relationship between parental and child dental fear: a structured review and meta-analysis. Int. J. Paediatr. Dent. 20, 83–101. doi: 10.1111/j.1365-263X.2009.00998.x
Vasiliki, B., Konstantinos, A., Nikolaos, K., Vassilis, K., Cor, V. L., and Jaap, V. (2016). Relationship between child and parental dental anxiety with child’s psychological functioning and behavior during the administration of local anesthesia. J. Clin. Pediatr. Dent. 40, 431–437. doi: 10.17796/1053-4628-40.6.431
Vervoort, L., Wolters, L. H., Hogendoorn, S. M., De Haan, E., Boer, F., and Prins, P. J. M. (2010). Sensitivity of Gray’s behavioral inhibition system in clinically anxious and non-anxious children and adolescents. Pers. Individ. Differ. 48, 629–633. doi: 10.1016/j.paid.2009.12.021
Waller, R., Shaw, D. S., and Hyde, L. W. (2017). Observed fearlessness and positive parenting interact to predict childhood callous-unemotional behaviors among low-income boys. J. Child Psychol. Psychiatry 58, 282–291. doi: 10.1111/jcpp.12666
Walling, B. R., Mills, R. S. L., and Freeman, W. S. (2007). Parenting cognitions associated with the use of psychological control. J. Child Fam. Stud. 16, 642–659. doi: 10.1007/s10826-006-9113-2
Wang, F., Cox, M. J., Mills-Koonce, R., and Snyder, P. (2015). Parental behaviors and beliefs, child temperament, and attachment disorganization. Fam. Relat. 64, 191–204. doi: 10.1111/fare.12120
Weinstein, P., Getz, T., Ratener, P., and Domoto, P. (1982). The effect of dentists’ behaviors on fear-related behaviors in children. J. Am. Dent. Assoc. 104, 32–38. doi: 10.14219/jada.archive.1982.0117
Welly, A., Lang, H., Welly, D., and Kropp, P. (2012). Impact of dental atmosphere and behaviour of the dentist on children’s cooperation. Appl. Psychophysiol. Biofeedback 37, 195–204. doi: 10.1007/s10484-012-9189-y
Wepman, B. J., and Sonnenberg, E. M. (1978). Effective communication with the pedodontic patient. J. Pedod. 2, 316–321.
Williams, S. R., Kertz, S. J., Schrock, M. D., and Woodruff-Borden, J. (2012). A sequential analysis of parent - Child interactions in anxious and nonanxious families. J. Clin. Child Adolesc. Psychol. 41, 64–74. doi: 10.1080/15374416.2012.632347
Willumsen, T. (2001). Dental fear in sexually abused women. Eur. J. Oral Sci. 109, 291–296. doi: 10.1034/j.1600-0722.2001.00069.x
Willumsen, T. (2004). The impact of childhood sexual abuse on dental fear. Community Dent. Oral Epidemiol. 32, 73–79. doi: 10.1111/j.1600-0528.2004.00120.x
Winefield, H. R., Goldney, R. D., Tiggemann, M., and Winefield, A. H. (1990). Parental rearing behaviors: stability of reports over time and relation to adult interpersonal skills. J. Genet. Psychol. 151, 211–219. doi: 10.1080/00221325.1990.9914655
Wood, J. J. (2006). Parental intrusiveness and children’s separation anxiety in a clinical sample. Child Psychiatry Hum. Dev. 37, 73–87. doi: 10.1007/s10578-006-0021-x
Wood, J. J., Kiff, C., Jacobs, J., Ifekwunigwe, M., and Piacentini, J. C. (2007). Dependency on elementary school caregivers: the role of parental intrusiveness and children’s separation anxiety. Psychol. Sch. 44, 823–837. doi: 10.1002/pits.20268
Wood, J. J., Mcleod, B. D., Piacentini, J. C., and Sigman, M. (2009). One-year follow-up of family versus child Cbt for anxiety disorders: exploring the roles of child age and parental intrusiveness. Child Psychiatry Hum. Dev. 40, 301–316. doi: 10.1007/s10578-009-0127-z
Wood, J. J., Piacentini, J. C., Southam-Gerow, M., Chu, B. C., and Sigman, M. (2006). Family cognitive behavioral therapy for child anxiety disorders. J. Am. Acad. Child Adolesc. Psychiatry 45, 314–321. doi: 10.1097/01.chi.0000196425.88341.b0
Young, R., Lennie, S., and Minnis, H. (2011). Children’s perceptions of parental emotional neglect and control and psychopathology. J. Child Psychol. Psychiatry 52, 889–897. doi: 10.1111/j.1469-7610.2011.02390.x
Zelenski, J. M., and Larsen, R. J. (2002). Predicting the future: How affect-related personality traits influence likelihood judgments of future events. Pers. Soc. Psychol. Bull. 28, 1000–1010. doi: 10.1177/014616720202800712
Zhou, Y., Cameron, E., Forbes, G., and Humphris, G. (2011). Systematic review of the effect of dental staff behaviour on child dental patient anxiety and behaviour. Patient Educ. Couns. 85, 4–13. doi: 10.1016/j.pec.2010.08.002
Zhou, Y., Cameron, E., Forbes, G., and Humphris, G. (2012a). Development of a novel coding scheme (Sabics) to record nurse child interactive behaviours in a community dental preventive intervention. Patient Educ. Couns. 88, 268–276. doi: 10.1016/j.pec.2012.01.001
Zhou, Y., Forbes, G. M., Macpherson, L. M., Ball, G. E., and Humphris, G. M. (2012b). The behaviour of extended duties dental nurses and the acceptance of fluoride varnish application in preschool children. Br. Dent. J. 213, 603–609. doi: 10.1038/sj.bdj.2012.1133
Keywords: intrusion, intrusive parenting, psychological control, dental fear, dental anxiety, parenting, temperament
Citation: Chapman HR and Kirby-Turner N (2018) Psychological Intrusion – An Overlooked Aspect of Dental Fear. Front. Psychol. 9:501. doi: 10.3389/fpsyg.2018.00501
Received: 14 July 2017; Accepted: 26 March 2018;
Published: 17 April 2018.
Edited by:
Alexandrina L. Dumitrescu, Independent Researcher, Bucharest, RomaniaReviewed by:
Unai Diaz-Orueta, Maynooth University, IrelandRadwa Khalil, Jacobs University Bremen, Germany
Seth Davin Norrholm, Emory University School of Medicine, United States
Copyright © 2018 Chapman and Kirby-Turner. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Helen R. Chapman, hchapman@lincoln.ac.uk
 Helen R. Chapman
Helen R. Chapman Nick Kirby-Turner
Nick Kirby-Turner