- 1Department of Neuroscience, Rehabilitation, Ophthalmology, Genetics and Maternal and Child Health, Section of Psychiatry, University of Genoa, Genoa, Italy
- 2Department of Neurosciences, Mental Health and Sensory Organs, Suicide Prevention Center, Sant’Andrea Hospital, Sapienza University of Rome, Rome, Italy
- 3Department of Psychiatry, University of Naples SUN, Naples, Italy
- 4Department of Psychology and Human Development, UCL Institute of Education, University College London, London, United Kingdom
Introduction: Childhood maltreatment (CM) has been associated with an increased risk of non-suicidal self-injury (NSSI) and suicidal behaviors. However, the exact nature of the association between CM and NSSI is currently unclear. The present review aimed to systematically investigate the association between CM and NSSI in adolescence and early adulthood.
Methods: A systematic search of four major electronic databases covering both medical and social science research (PubMed, Scopus, Science Direct, and PsycINFO) was conducted.
Results: Overall, 20 cross-sectional studies including a total of 22,517 individuals, 3 longitudinal follow-up studies including 1,728 individuals, and 3 retrospective studies including 62,089 individuals were selected. It appears that CM is a significant risk factor for both NSSI and suicide attempts. The increased vulnerability to NSSI seems to be related to experiences of CM, particularly sexual abuse. Gender differences were also found. Generally, when compared to males, females who experienced CM seem to be more vulnerable to presenting with NSSI and suicidal behaviors.
Conclusion: There is a positive association between CM and NSSI. The importance of early detection and risk reduction of self-injurious behavior for adolescents is discussed.
Introduction
Non-suicidal self-injury (NSSI) may be defined as the direct, deliberate destruction of one’s own body without suicidal intent (1), and it has been described as a serious public health concern for adolescents and young adults (2). Using data from community and psychiatric samples, Grandclerc and colleagues (3) reported that the prevalence of adolescent NSSI is between 10 and 35%. Individuals experiencing NSSI thoughts and those engaging in NSSI behaviors report poorer social relationships and greater psychosocial impairment, compared with their counterparts (4). Importantly, NSSI is associated with an increased risk of psychopathological conditions (5, 6). In adolescence, a significant percentage of both community self-injurers and inpatients reporting NSSI attempt suicide (7, 8).
Self-harming behavior rates in those with a history of childhood maltreatment (CM) are higher than in the general population (9), in line with much evidence showing that the psychopathological potential and consequences of CM are quite broad (10). CM can be subdivided into the following domains (11): (1) physical abuse, i.e., deliberate physical harm; (2) emotional abuse such as verbal aggression significantly affecting the child’s wellbeing, or behaviors that may humiliate, embarrass, or seriously threaten the child; (3) sexual abuse, i.e., any type of sexual contact/behavior between a child and an adult; (4) emotional neglect, i.e., the failure to satisfy vital emotional and psychological needs such as love and support; and (5) physical neglect, i.e., the failure to meet basic physical needs such as food and shelter.
Small-to-medium associations have been reported between CM and the presence of a recent history of NSSI (12). Maltreatment has also been associated with an increased risk of adolescent suicidal behaviors, particularly in females (13). Some recent evidence suggests specificity in both CM and injury behaviors in adolescence (14), with a history of physical/sexual abuse being associated with an increased risk of suicide attempts and a history of neglect with an increased risk of NSSI. However, the exact nature of the association between CM and NSSI in adolescence and early adulthood is currently unclear (15). The consequences for prolonged, chronic engagement in NSSI, or for intermittent versus repetitive NSSI represent additional aspects that need to be explored.
Thus, given this background, the present review aims to systematically investigate the association between CM and NSSI in adolescence and early adulthood. We hypothesized that CM is associated with an increased vulnerability to NSSI, although we postulated that this association may be moderated or mediated by other factors, not necessarily linked to the characteristics of CM. Therefore, the present review seeks to add to the literature on the link between CM and NSSI, while providing a more in depth analysis of the paths leading to NSSI following an experience of CM.
Methods
Eligibility Criteria
We adopted the “Preferred Reporting Items for Systematic Reviews and Meta-Analyses” guidelines (16). We included studies that explicitly mentioned the association between child maltreatment (OR child abuse OR child neglect) AND NSSI in childhood, adolescence, or adulthood. When a title or abstract seemed to describe a study suitable for inclusion, the full-text article was obtained and carefully examined to evaluate its relevance for our work. Our exclusion criteria were as follows: (1) studies published before 1980; (2) studies without abstracts or with abstracts that did not explicitly mention the association between CM and NSSI or self-harm in childhood, adolescence, or adulthood; (3) studies that were not published in English; (4) systematic reviews or meta-analytic studies on the topic; and (5) studies in which maltreatment was perpetrated by other children.
Information Sources
We conducted a systematic search of four major electronic databases including medical and social science studies (PubMed, Scopus, Science Direct, and PsycINFO) for titles and abstracts relevant to our research questions. We also examined the bibliographies of the retrieved articles for additional papers that might be relevant. Overall, the papers we examined covered the period between 1996 and 2016.
Search Terms
The following search query was used in all databases: “child maltreatment” AND “non-suicidal self-injury” OR “child abuse” AND “non-suicidal self-injury” OR “child neglect” AND “non-suicidal self-injury.”
Selection of Studies
Articles were screened and selected in a two-step process to minimize bias. First, three independent researchers (Giovanna Canepa, Giulia Adavastro, and Jacopo Nebbia) conducted the literature search. Any discrepancies between the three reviewers who examined the studies independently for possible inclusion were resolved by consultation with the senior reviewers (Gianluca Serafini and Mario Amore). In the second phase, full-text articles that met our inclusion criteria were retrieved and independently reviewed by Gianluca Serafini and Mario Amore, who discussed the design and characteristics of the studies to decide whether they could be included in the review. If there were doubts about a particular study, then that study was put on the list of those awaiting assessment, pending acquisition of more information, and was then carefully reanalyzed for possible inclusion. Any disagreements in this step were solved by discussion between reviewers.
Data Collection Process
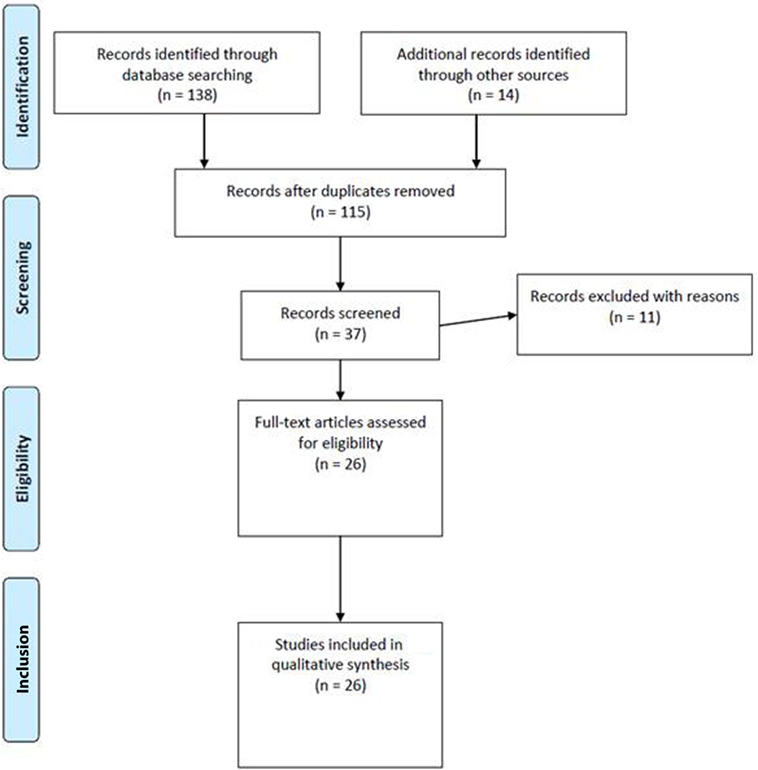
Giovanna Canepa, Giulia Adavastro, and Jacopo Nebbia extracted the following data elements from the 37 studies screened for this review (see “Study Sample” below): author/s and publication year, presence/absence of control group, psychiatric diagnosis, study design, sample size, physical or biological assessment, psychometric instruments, sample characteristics, limitations, and main conclusions (for more details, see Table 1). Reviewers acquired the full-text of all 37 articles.
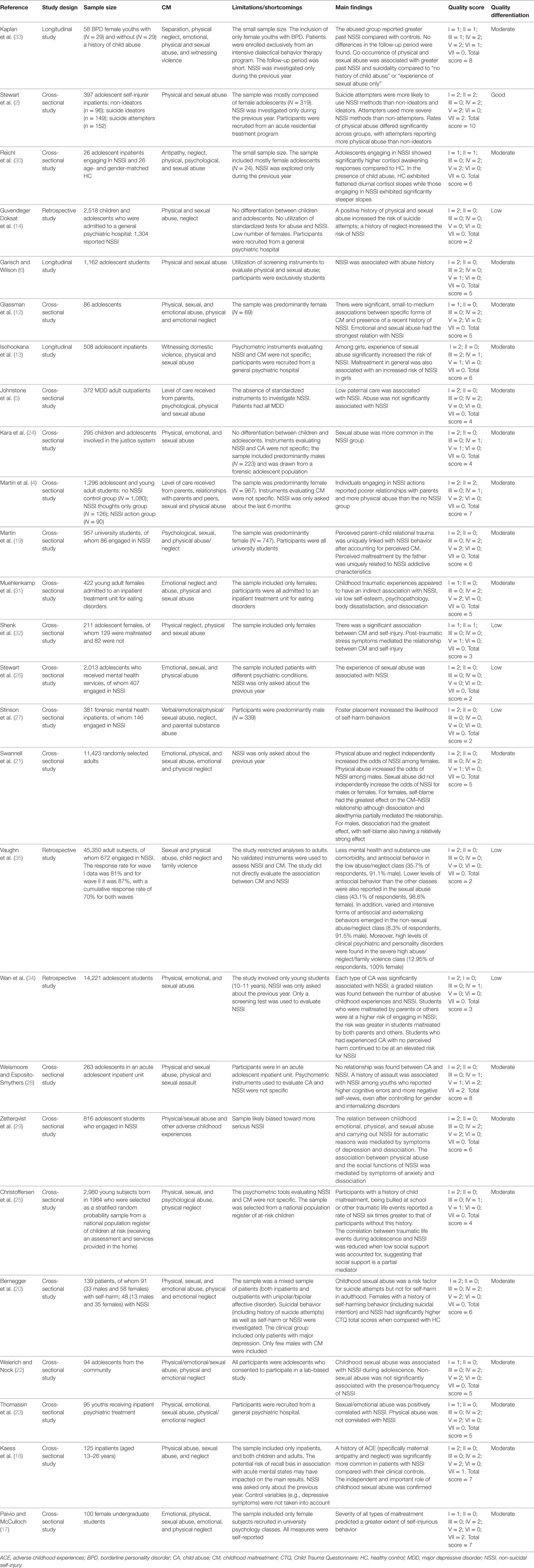
Table 1. Summary information about all the studies on the association between CM and NSSI included in this review.
Summary Measures
The quality of the 26 studies eventually used for this review was evaluated using the following criteria: (1) representativeness of the sample (0–2 points); (2) presence and representativeness of control group (0–2 points); (3) presence of follow-up (0–2 points); (4) evidence-based measures of CM [e.g., Childhood Experiences of Care and Abuse Interview, Child Trauma Questionnaire (CTQ), Childhood Maltreatment Interview Schedule-Short Form, Comprehensive Trauma Interview, Christchurch Trauma Assessment, Abuse and Perpetration Inventory, Childhood Trauma Interview, Comprehensive Childhood Maltreatment Scale, Traumatic Experiences Checklist, or other psychometric evaluation (0–2 points)]; (5) evidence-based measures of NSSI [e.g., NSSI Checklist, Self-Injurious Thoughts and Behaviors Interview, Deliberate Self-Harm Inventory, Comprehensive Trauma Interview, Lifetime Parasuicidal Count, Suicidal Behaviour Questionnaire, Viennese Suicide Risk Assessment Scale, Ottawa Self-Injury Inventory, Self-Injury Questionnaire, Self-Injurious Behavior Questionnaire, or other psychometric evaluation (0–2 points)]; (6) presence of raters who identified independently the presence of CM (0–2 points); and (7) statistical evaluation of interrater reliability (0–2 points).
Quality scores ranged from 0 to 14. Studies were differentiated according to their quality, as follows: (1) good quality (10–14 points), if most or all the criteria were fulfilled or, where they were not met, the study conclusions were deemed very robust; (2) moderate quality (4–9 points), if some criteria were fulfilled or, where they were not met, the study conclusions were deemed robust; and (3) low quality (0–3 points), where few criteria were fulfilled or the conclusions were not deemed robust.
Results
Study Sample
The searches in PubMed, Scopus, Science Direct, and PsycInfo revealed, after the removal of duplicates, a total of 26 potentially relevant articles about CM and NSSI. Overall, the search in PubMed generated 34 articles for maltreatment, 32 for abuse, and 33 for neglect; the search in Scopus generated 7 articles for maltreatment, 19 for abuse, and 2 for neglect; the search in Science Direct generated 5 articles for maltreatment, 4 for abuse, and 2 for neglect, whereas the search in PsycInfo did not provide any article. Moreover, we extracted another 14 studies from the reference lists of these articles. Of all these, 115 were excluded because they were duplicates, or they were without an abstract, or they had an abstract that did not explicitly mention NSSI and a form of CM, or they were not written in English. Then, 11 articles were excluded because they were on self-mutilation or self-harm and did not mention NSSI. Thus, 26 met our inclusion criteria and were therefore used for the present review. Figure 1 summarizes the main results of the search strategy (i.e., the identification, screening, eligibility, and inclusion process) used for selecting studies.
Study Types and Sample Characteristics
Overall, 20 cross-sectional studies—including a total of 22,517 individuals—3 longitudinal follow-up studies—including 1,728 individuals—and 3 retrospective studies—including 62,089 individuals—were considered. Clinical samples included predominantly patients with NSSI and one of the following psychiatric diagnoses: major depressive disorder (MDD), bipolar disorder, substance use disorder, eating disorders, personality disorders or other psychiatric disorders.
Study Quality Assessment
According to our quality score system, the mean quality score of the 20 cross-sectional studies was 5; the mean score of the 3 longitudinal studies was 6.3; and the mean score of the 3 retrospective studies was 2.3. Most of the studies (N = 19) were of moderate quality, one was of good quality, and six of low quality. The most relevant findings derived from the 26 studies we used are reported below.
Cross-Sectional Studies on the Association between CM and NSSI
Most of the studies (N = 20) were cross-sectional in nature. Overall, only one study (quality score 10) was considered good quality, 16 studies were of moderate quality (mean quality score 5.6), and three studies were of low quality (mean quality score 2.3). All documented a positive association between NSSI and CM.
In the study of Martin and colleagues (4), NSSI thoughts were distinguished from NSSI actions, but both NSSI thoughts and NSSI actions were correlated with physical abuse. Paivio and McCulloch (17) highlighted the importance of severity of CM for NSSI. Kaess et al. (18) showed that a history of adverse childhood experiences (in particular maternal antipathy/neglect, and sexual abuse) was significantly more common in patients with NSSI than in those without. Similar results were documented by Martin and colleagues in a more recent study (19) in which NSSI behavior was linked with perceived CM. Bernegger et al. (20) analyzed a sample of adults with unipolar or bipolar affective disorder and found that childhood sexual abuse was a risk factor for suicide attempts but not for self-harm in adulthood. In that study, females who engaged in self-harming behavior (including suicidal intention) or NSSI had significantly higher CTQ scores than controls. Small-to-medium associations between specific forms of CM (in particular, sexual abuse) and the presence of a recent NSSI were also found in the study of Glassman and colleagues (12). Conversely, Swannell et al. (21) did not find evidence for the predictive role of sexual abuse for NSSI. In the study of Weierich and Nock (22), only childhood sexual abuse was positively associated with NSSI during adolescence.
On the other hand, Thomassin and colleagues (23) found that sexual and emotional abuse—but not physical abuse—were both positively correlated with NSSI. More recently, Kara et al. (24) reported that, in their sample from a forensic adolescent population, those who engaged in NSSI showed higher rates of sexual abuse and were more frequently involved in multiple crimes. In a large (N = 2,980) study carried out by Christoffersen and colleagues in 2015 (25), individuals with a history of CM, peer victimization at school, or other adverse experiences were six times more likely to report NSSI than participants without this history. Stewart et al. (26) confirmed that sexual abuse was associated with NSSI in a sample of adolescents who accessed mental health services. Finally, in the study of Stinson and colleagues (27) in a sample of 381 forensic mental health inpatients, traumatic experiences enhanced the likelihood of self-harm and suicide attempts.
Studies Demonstrating the Existence of Mediators/Moderators in the Association between CM and NSSI
Overall, six studies [of which one was of good quality (quality score 10), four of moderate quality (mean quality score 6.25), and one of low quality (quality score 3)] did not find a direct correlation between CM and NSSI. In the study by Weismoore and Esposito-Smythers (28), there was no relation between childhood abuse and NSSI, but the association between assault and NSSI was significant in youth who reported more cognitive errors and more negative self-views. The retrospective study of Zetterqvist and colleagues (29) with 816 adolescents found an indirect association (mediated by depressive symptoms and dissociation) between childhood emotional or physical/sexual abuse and NSSI (see Table 1). Reichl et al. (30) showed that childhood adversity was associated with a steeper diurnal cortisol slope in the NSSI group and a flattened slope in the healthy control group. Analyzing a cohort of 422 young adult females with eating disorders, Muehlenkamp et al. (31) reported that CM likely shows an indirect association with self-harm behavior through low self-esteem, psychopathology, body dissatisfaction, and dissociation symptoms. Shenk and colleagues (32) reported that there was a significant association between CM and NSSI in females, but this relation was mediated by post-traumatic stress symptoms. Stewart et al. (2) also reported indirect links (between NSSI and physical abuse).
Studies Not Demonstrating the Existence of an Association between CM and NSSI
Only the study of Johnstone and colleagues (5), conducted in a sample of adult outpatients with MDD, did not demonstrate the existence of a correlation between CM and NSSI. In that study, abuse was not significantly associated with NSSI or suicide attempts. The authors, however, reported a correlation between low maternal care and suicide attempts and between low paternal care and NSSI.
Longitudinal Follow-up Studies on the Association between CM and NSSI
Overall, three studies [all of moderate quality (mean quality score 6.3)] prospectively investigated the association between CM and NSSI. Kaplan and colleagues (33) reported that abused individuals were at increased risk of NSSI at baseline. Isohookana and colleagues (13) found, in their study with 508 adolescent inpatients, that maltreatment, and specifically sexual abuse, was associated with an increased risk of NSSI and suicide attempts, although only in females. Finally, Garisch and Wilson (6) conducted a prospective study of 1,162 adolescent students and confirmed that NSSI was associated with abuse history.
Retrospective Studies on the Association between CM and NSSI
Three retrospective studies [all of low quality (mean quality score 2.3)] analyzed the direct association between CM and NSSI. Wan and colleagues (34) demonstrated that a continuous experience of abuse was significantly associated with NSSI, independently of gender. More recently, Guvendeger Doksat et al. (14) found that a history of neglect significantly increased the risk of NSSI, whereas physical/sexual abuse increased the odds of suicide attempts. Finally, Vaughn et al. (35) found that, in a nationally representative sample including subjects who engaged in NSSI, the severity of CM was related to clinical psychiatric and personality disorders.
Discussion and Conclusion
Summary of Main Findings
This review was carried out to explore the association between CM and NSSI in adolescence and early adulthood. We reviewed 26 studies that investigated the association between CM and NSSI. Generally, it appears that experience of CM can increase the risk of adverse outcomes later on, in line with much evidence not reviewed here (36, 37). In addition, sexual abuse in childhood and other factors such as emotional inexpressivity, and affect intensity/reactivity can be particularly significant for both suicidal behaviors and NSSI, in line with previous findings (38–43). Only one study (5) reviewed here did not find a correlation between CM and NSSI.
There were some noteworthy gender differences. Generally, when compared to males, females who experienced childhood traumatic experiences (particularly sexual abuse) (13, 21) were more vulnerable to NSSI and suicidal behaviors. However, when physical and sexual abuse co-occurred (37) or when the experience of abuse was continuous (14), both males and females were at risk of NSSI and suicidal behaviors.
Some of the studies reviewed also tested or suggested potential mechanisms underlying the association between NSSI and CM, such as via post-traumatic stress disorder (22), depression (44), and emotion dysregulation (45). For instance, Weierich and Nock (22) found that re-experiencing and avoidance symptoms can mediate the relation between childhood sexual abuse and self-injury, even when controlling for major depression. Glassman et al. (12) suggested that self-criticism and cognitive dysregulation could mediate the relation between emotional abuse and self-injury, in line with much evidence that cognitive styles can be directly related to NSSI and suicidal behaviors (46, 47). The association between CM and NSSI was also mediated by post-traumatic stress symptoms in that of Shenk and colleagues (32), and low self-esteem, psychopathology, body dissatisfaction, and dissociation symptoms in that of Muehlenkamp et al. (31). These findings are in line with the suggestion that suicidal behaviors and NSSI may represent attempts to cope with dissociative symptoms or to reach a dissociative state (1, 48–50). For example, a recent meta-analysis (49) on the link between dissociation and NSSI/suicide attempts showed that those with dissociative disorders were more likely to report both previous suicide attempts and NSSI, compared to those without.
The association between CM and NSSI or suicidal behaviors was not confirmed in all studies as already suggested in the meta-analysis of Klonsky and Moyer (51). The absence of a direct association between CM and NSSI may be explained by the existence of mediators, as mentioned above. Some studies (5, 19) also suggest that high-risk family contexts rather than the experience of maltreatment may play a significant role in suicidal behaviors and NSSI.
In conclusion, therefore, CM and childhood traumatic experiences appear to increase the odds of NSSI and suicidal behaviors either directly or via other risk factors.
Main Strengths and Limitations/Shortcomings
To the best of our knowledge, this is the first review to systematically evaluate the relation between CM and NSSI. However, our findings should be considered in the light of several limitations. First, we could not carry out a meta-analysis because the studies identified measured CM and NSSI differently. Importantly, we selected studies that did not exclude self-harm, suicide attempts, and other suicidal behaviors; this may have introduced confounding. In addition, although this review aimed to summarize the most relevant studies on the topic, the inclusion/exclusion of specific studies may reflect our individual point of view or expertise and training. Moreover, some studies included may have been underpowered (some had only small sample sizes and small numbers of subjects who engaged in NSSI). Another limitation is that findings may have been hampered by recall bias. In addition, the severity, duration, intensity, and age at occurrence of CM were not taken into account in all studies; these aspects of CM, potentially very important, should perhaps be considered routinely in future studies. Finally, some of the included studies were heterogeneous and/or did not include control groups.
Implications and Future Directions
In conclusion, the findings of this systematic review support the positive association between CM and NSSI. This information may help to early detect and rapidly recognize those who experienced CM as a specific group at risk for NSSI and suicidal behaviors. Future research should explore systematically the role of vulnerability and protective factors, i.e., factors that may act to increase or attenuate, respectively, the association between CM and NSSI.
Author Contributions
Each author consistently contributed to the paper. GS discussed and conceived the study hypothesis and wrote the main body of the paper. DE, GC, and BP performed the methodological search on the research topic and provided help in selecting papers on the main topic. GA, JN, and MBM contributed to reviewing the literature. MP, AF, and EF reviewed the paper adding contributions to the applied methodology and the discussion section. MA provided the intellectual impetuous and supervised the writing of the manuscript.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Nock MK, Prinstein MJ. A functional approach to the assessment of self-mutilative behavior. J Consult Clin Psychol (2004) 72:885–90. doi:10.1037/0022-006X.72.5.885
2. Stewart JG, Esposito EC, Glenn CR, Gilman SE, Pridgen B, Gold J, et al. Adolescent self-injurers: comparing non-ideators, suicide ideators, and suicide attempters. J Psychiatr Res (2017) 84:105–12. doi:10.1016/j.jpsychires.2016.09.031
3. Grandclerc S, De Labrouhe D, Spodenkiewicz M, Lachal J, Moro MR. Relations between nonsuicidal self-injury and suicidal behavior in adolescence: a systematic review. PLoS One (2016) 11:e0153760. doi:10.1371/journal.pone.0153760
4. Martin J, Bureau JF, Cloutier P, Lafontaine MF. A comparison of invalidating family environment characteristics between university students engaging in self-injurious thoughts & actions and non-self-injuring university students. J Youth Adolesc (2011) 40:1477–88. doi:10.1007/s10964-011-9643-9
5. Johnstone JM, Carter JD, Luty SE, Mulder RT, Frampton CM, Joyce PR. Childhood predictors of lifetime suicide attempts and non-suicidal self-injury in depressed adults. Aust N Z J Psychiatry (2016) 50:135–44. doi:10.1177/0004867415585581
6. Garisch JA, Wilson MS. Prevalence, correlates, and prospective predictors of non-suicidal self-injury among New Zealand adolescents: cross-sectional and longitudinal survey data. Child Adolesc Psychiatry Ment Health (2015) 9:28. doi:10.1186/s13034-015-0055-6
7. Brausch AM, Gutierrez PM. Differences in non-suicidal self-injury and suicide attempts in adolescents. J Youth Adolesc (2010) 39:233–42. doi:10.1007/s10964-009-9482-0
8. Nock MK, Joiner TE Jr, Gordon KH, Lloyd-Richardson E, Prinstein MJ. Non-suicidal self-injury among adolescents: diagnostic correlates and relation to suicide attempts. Psychiatry Res (2006) 144:65–72. doi:10.1016/j.psychres.2006.05.010
9. Santa Mina EE, Gallop RM. Childhood sexual and physical abuse and adult self-harm and suicidal behaviour: a literature review. Can J Psychiatry (1998) 43:793–800. doi:10.1177/070674379804300803
10. Shonkoff JP, Garner AS; Committee on Psychosocial Aspects of Child and Family Health; Committee on Early Childhood, Adoption, and Dependent Care; Section on Developmental and Behavioral Pediatrics. The lifelong effects of early childhood adversity and toxic stress. Pediatrics (2012) 129:e232–46. doi:10.1542/peds.2011-2663
11. Bernstein DP, Fink L, Handelsman L, Foote J, Lovejoy M, Wenzel K, et al. Initial reliability and validity of a new retrospective measure of child abuse and neglect. Am J Psychiatry (1994) 151:1132–6. doi:10.1176/ajp.151.8.1132
12. Glassman LH, Weierich MR, Hooley JM, Deliberto TL, Nock MK. Child maltreatment, non-suicidal self-injury, and the mediating role of self-criticism. Behav Res Ther (2007) 45:2483–90. doi:10.1016/j.brat.2007.04.002
13. Isohookana R, Riala K, Hakko H, Räsänen P. Adverse childhood experiences and suicidal behavior of adolescent psychiatric inpatients. Eur Child Adolesc Psychiatry (2013) 22:13–22. doi:10.1007/s00787-012-0311-8
14. Guvendeger Doksat N, Zahmacioglu O, Demirci AC, Kocaman GM, Erdogan A. Association of suicide attempts and non-suicidal self-injury behaviors with substance use and family characteristics among children and adolescents seeking treatment for substance use disorder. Subst Use Misuse (2017) 52:604–13. doi:10.1080/10826084.2016.1245745
15. Oldershaw A, Richards C, Simic M, Schmidt U. Parents’ perspectives on adolescent self-harm: qualitative study. Br J Psychiatry (2008) 193:140–4. doi:10.1192/bjp.bp.107.045930
16. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med (2009) 151:W65–94. doi:10.7326/0003-4819-151-4-200908180-00136
17. Paivio SC, McCulloch CR. Alexithymia as a mediator between childhood trauma and self-injurious behaviors. Child Abuse Negl (2004) 28:339–54. doi:10.1016/j.chiabu.2003.11.018
18. Kaess M, Parzer P, Mattern M, Plener PL, Bifulco A, Resch F, et al. Adverse childhood experiences and their impact on frequency, severity, and the individual function of nonsuicidal self-injury in youth. Psychiatry Res (2013) 206:265–72. doi:10.1016/j.psychres.2012.10.012
19. Martin J, Bureau JF, Yurkowski K, Fournier TR, Lafontaine MF, Cloutier P. Family-based risk factors for non-suicidal self-injury: considering influences of maltreatment, adverse family-life experiences, and parent-child relational risk. J Adolesc (2016) 49:170–80. doi:10.1016/j.adolescence.2016.03.015
20. Bernegger A, Kienesberger K, Carlberg L, Swoboda P, Ludwig B, Koller R, et al. Influence of sex on suicidal phenotypes in affective disorder patients with traumatic childhood experiences. PLoS One (2015) 10:e0137763. doi:10.1371/journal.pone.0137763
21. Swannell S, Martin G, Page A, Hasking P, Hazell P, Taylor A, et al. Child maltreatment, subsequent non-suicidal self-injury and the mediating roles of dissociation, alexithymia and self-blame. Child Abuse Negl (2012) 36:572–84. doi:10.1016/j.chiabu.2012.05.005
22. Weierich MR, Nock MK. Posttraumatic stress symptoms mediate the relation between childhood sexual abuse and nonsuicidal self-injury. J Consult Clin Psychol (2008) 76:39–44. doi:10.1037/0022-006X.76.1.39
23. Thomassin K, Shaffer A, Madden A, Londino DL. Specificity of childhood maltreatment and emotion deficit in nonsuicidal self-injury in an inpatient sample of youth. Psychiatry Res (2016) 244:103–8. doi:10.1016/j.psychres.2016.07.050
24. Kara K, Ozsoy S, Teke H, Congologlu MA, Turker T, Renklidag T, et al. Non-suicidal self-injurious behavior in forensic child and adolescent populations. Clinical features and relationship with depression. Neurosciences (Riyadh) (2015) 20:31–6.
25. Christoffersen MN, Møhl B, DePanfilis D, Vammen KS. Non-suicidal self-injury – does social support make a difference? An epidemiological investigation of a Danish national sample. Child Abuse Negl (2015) 44:106–16. doi:10.1016/j.chiabu.2014.10.023
26. Stewart SL, Baiden P, Theall-Honey L. Examining non-suicidal self-injury among adolescents with mental health needs, in Ontario, Canada. Arch Suicide Res (2014) 18:392–409. doi:10.1080/13811118.2013.824838
27. Stinson JD, Quinn MA, Levenson JS. The impact of trauma on the onset of mental health symptoms, aggression, and criminal behavior in an inpatient psychiatric sample. Child Abuse Negl (2016) 61:13–22. doi:10.1016/j.chiabu.2016.09.005
28. Weismoore JT, Esposito-Smythers C. The role of cognitive distortion in the relationship between abuse, assault, and non-suicidal self-injury. J Youth Adolesc (2010) 39:281–90. doi:10.1007/s10964-009-9452-6
29. Zetterqvist M, Lundh LG, Svedin CG. A cross-sectional study of adolescent non-suicidal self-injury: support for a specific distress-function relationship. Child Adolesc Psychiatry Ment Health (2014) 8:23. doi:10.1186/1753-2000-8-23
30. Reichl C, Heyer A, Brunner R, Parzer P, Völker JM, Resch F, et al. Hypothalamic-pituitary-adrenal axis, childhood adversity and adolescent nonsuicidal self-injury. Psychoneuroendocrinology (2016) 74:203–11. doi:10.1016/j.psyneuen.2016.09.011
31. Muehlenkamp JJ, Claes L, Smits D, Peat CM, Vandereycken W. Non-suicidal self-injury in eating disordered patients: a test of a conceptual model. Psychiatry Res (2011) 188:102–8. doi:10.1016/j.psychres.2010.12.023
32. Shenk CE, Noll JG, Cassarly JA. A multiple mediational test of the relationship between childhood maltreatment and non-suicidal self-injury. J Youth Adolesc (2010) 39:335–42. doi:10.1007/s10964-009-9456-2
33. Kaplan C, Tarlow N, Stewart JG, Aguirre B, Galen G, Auerbach RP. Borderline personality disorder in youth: The prospective impact of child abuse on non-suicidal self-injury and suicidality. Compr Psychiatry (2016) 71:86–94. doi:10.1016/j.comppsych.2016.08.016
34. Wan Y, Chen J, Sun Y, Tao F. Impact of childhood abuse on the risk of non-suicidal self-injury in mainland chinese adolescents. PLoS One (2015) 10(6):e0131239. doi:10.1371/journal.pone.0131239
35. Vaughn MG, Salas-Wright CP, Underwood S, Gochez-Kerr T. Subtypes of non-suicidal self-injury based on childhood adversity. Psychiatr Q (2015) 86:137–51. doi:10.1007/s11126-014-9313-7
36. Thabrew H, de Sylva S, Romans SE. Evaluating childhood adversity. Adv Psychosom Med (2012) 32:35–57. doi:10.1159/000330002
37. Gibb BE, Alloy LB. A prospective test of the hopelessness theory of depression in children. J Clin Child Adolesc Psychol (2006) 35:264–74. doi:10.1207/s15374424jccp3502_10
38. Maniglio R. The role of child sexual abuse in the etiology of suicide and non-suicidal self-injury. Acta Psychiatr Scand (2011) 124:30–41. doi:10.1111/j.1600-0447.2010.01612.x
39. Romans SE, Martin JL, Anderson JC, Herbison GP, Mullen PE. Sexual abuse in childhood and deliberate self-harm. Am J Psychiatry (1995) 152(9):1336–42. doi:10.1176/ajp.152.9.1336
40. Ystgaard M, Hestetun I, Loeb M, Mehlum L. Is there a specific relationship between childhood sexual and physical abuse and repeated suicidal behavior? Child Abuse Negl (2004) 28:863–75. doi:10.1016/j.chiabu.2004.01.009
41. Plener PL, Schumacher TS, Munz LM, Groschwitz RC. The longitudinal course of non-suicidal self-injury and deliberate self-harm: a systematic review of the literature. Borderline Personal Disord Emot Dysregul (2015) 2:2. doi:10.1186/s40479-014-0024-3
42. Gratz KL, Conrad SD, Roemer L. Risk factors for deliberate self-harm among college students. Am J Orthopsychiatry (2002) 72:128–40. doi:10.1037/0002-9432.72.1.128
43. Kendall-Tackett KA, Williams LM, Finkelhor D. Impact of sexual abuse on children: a review and synthesis of recent empirical studies. Psychol Bull (1993) 113:164–80. doi:10.1037/0033-2909.113.1.164
44. Cicchetti D, Toth SL. Child maltreatment. Ann Rev Clin Psychol (2005) 1:409–38. doi:10.1146/annurev.clinpsy.1.102803.144029
45. Shipman K, Zeman J, Penza S, Champion K. Emotion management skills in sexually maltreated and nonmaltreated girls: a developmental psychopathology perspective. Dev Psychopathol (2000) 12:47–62. doi:10.1017/S0954579400001036
46. Braquehais MD, Oquendo MA, Baca-García E, Sher L. Is impulsivity a link between childhood abuse and suicide? Compr Psychiatry (2010) 51:121–9. doi:10.1016/j.comppsych.2009.05.003
47. O’Connor RC, Noyce R. Personality and cognitive processes: self-criticism and different types of rumination as predictors of suicidal ideation. Behav Res Ther (2008) 46:392–401. doi:10.1016/j.brat.2008.01.007
48. Connors R. Self-injury in trauma survivors: 1. Functions and meanings. Am J Orthopsychiatry (1996) 66:197–206. doi:10.1037/h0080171
49. Calati R, Bensassi I, Courtet P. The link between dissociation and both suicide attempts and non-suicidal self-injury: meta-analyses. Psychiatry Res (2017) 251:103–14. doi:10.1016/j.psychres.2017.01.035
50. Zanarini MC. Childhood experiences associated with the development of borderline personality disorder. Psychiatr Clin North Am (2000) 23:89–101. doi:10.1016/S0193-953X(05)70145-3
Keywords: childhood maltreatment, physical/sexual abuse, emotional neglect, non-suicidal self-injury, suicidal behaviors
Citation: Serafini G, Canepa G, Adavastro G, Nebbia J, Belvederi Murri M, Erbuto D, Pocai B, Fiorillo A, Pompili M, Flouri E and Amore M (2017) The Relationship between Childhood Maltreatment and Non-Suicidal Self-Injury: A Systematic Review. Front. Psychiatry 8:149. doi: 10.3389/fpsyt.2017.00149
Received: 29 May 2017; Accepted: 28 July 2017;
Published: 24 August 2017
Edited by:
Bruno Etain, Paris Diderot University, FranceReviewed by:
Stephane Richard-Devantoy, McGill University, CanadaJorge Lopez-Castroman, Centre Hospitalier Universitaire De Nîmes, France
Copyright: © 2017 Serafini, Canepa, Adavastro, Nebbia, Belvederi Murri, Erbuto, Pocai, Fiorillo, Pompili, Flouri and Amore. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gianluca Serafini, gianluca.serafini@unige.it
 Gianluca Serafini
Gianluca Serafini Giovanna Canepa
Giovanna Canepa Giulia Adavastro1
Giulia Adavastro1 Jacopo Nebbia
Jacopo Nebbia Maurizio Pompili
Maurizio Pompili Eirini Flouri
Eirini Flouri