- 1Department of Psychiatry and Psychotherapy, University of Lübeck, Lübeck, Germany
- 2Institute for Cardiogenetics, University of Lübeck, Lübeck, Germany
- 3Partner Site Hamburg and Lübeck and Kiel, German Research Centre for Cardiovascular Research (DZHK), Lübeck, Germany
- 4University Heart Center Lübeck, Lübeck, Germany
- 5German Heart Center Munich, Technical University Munich, Munich, Germany
- 6Partner Site Munich Heart Alliance, German Centre for Cardiovascular Research (DZHK), Munich, Germany
Background: Comorbid mental disorders in patients with coronary artery disease (CAD) are common and associated with adverse somatic outcomes. However, data on utilization rates of mental health care and treatment efficiency are scarce and inconsistent, which we tried to remedy with the present preliminary study on Northern German CAD patients.
Method: A total of 514 German CAD patients, as diagnosed by cardiac catheterization, were assessed using the Mini International Neuropsychiatric Interview and the Global Assessment of Functioning (GAF) scale.
Results: Global utilization of mental health care since onset of CAD was 21.0%. Depressive disorders, younger age, and lower GAF at onset of CAD were associated with higher utilization rates, while anxiety disorders and gender were not. Lower GAF at onset of CAD, female gender, and psychotherapy was positively associated with higher gains in GAF, while younger age and anxiety disorders were negatively associated.
Conclusion: The majority of CAD patients with comorbid depression reported to have received mental health treatment and seemed to have benefited from it. However, we found preliminary evidence of insufficiencies in the diagnosis and treatment of anxiety disorders in CAD patients. Further studies, preferably prospective and with representative samples, are needed to corroborate or falsify these findings and explore possible further mediators of health-care utilization by CAD patients such as race, ethnicity, and socioeconomic status.
Introduction
Comorbid mental disorders, especially depression and anxiety disorders, are common in patients with coronary artery disease (CAD) and are consistently associated with lower quality of life, poorer somatic outcomes, higher mortality, and higher medical costs (1–8). However, contrary to acute coronary syndrome and myocardial infarction (MI), data on the effectiveness of mental health treatment are inconsistent. There is some data on the effectiveness of SSRIs sertraline and citalopram on depressive symptoms in patients with CAD (9, 10), but several studies found no benefit of add-on psychotherapy (PT) such as interpersonal PT or cognitive behavior therapy (10–13).
Although anxiety disorders are as common in CAD patients as depressive disorders (unpublished data), research on their treatment is even scarcer (14). Panic disorder was successfully treated in CAD patients in the small PATCHD trial (15) and additional CBT reduced somatic anxiety in the SUPRIM trial (12, 13). In addition, little is known about the utilization rates of mental health-care services by patients with CAD and comorbid affective or anxiety disorders, as well as about effectiveness of general mental health care in CAD patients outside of the research setting. As the associations between mental health, well-being and CAD have consistently been shown to be moderated by race, ethnicity and socioeconomic factors (16, 17), data from various countries have to be collected to gain a comprehensive overview. Therefore, the aim of this preliminary descriptive study was to provide data on utilization rates of mental health care and treatment efficiency in CAD patients in Northern Germany to inform researchers, local policy makers and developers of mental health programs.
Materials and Methods
Participants
This study constitutes a full survey of patients diagnosed with CAD by cardiac catheterization at the University Hospital Schleswig-Holstein in Lübeck, Germany, between February 2004 and December 2012. Being one of only two University Hospitals in the federal state of Schleswig-Holstein, the University Hospital in Lübeck has a big catchment area extending into the neighboring states of Mecklenburg-Vorpommern and Hamburg. A total of 1,182 patients (74.4% male, mean age = 62.2 years, SD = 11.1) gave written informed consent to the use of their data and to be contacted for research purposes, in accordance with the Declaration of Helsinki. The study protocol was approved by the ethics committee of the University of Lübeck (ID 04/041). When contacted between March 2013 and January 2015, 511 patients agreed to participate in the telephone survey described in this paper. Exclusion criteria were a lack of informed consent, exclusion of CAD during cardiac catheterization and inability to participate (e.g., due to hearing impairment, aphasia, cognitive deficits, or insufficient language skills).
Assessment
Onset of CAD
Onset of CAD was defined as the year in which one of the following criteria was met for the first time: (a) specific symptoms of CAD (e.g., angina pectoris) not otherwise explicable, (b) cardiac catheterization showing CAD or a diminished cardiac function, and (c) formal diagnosis of MI.
Anxiety and Depressive Disorders
Participants were assessed for mental disorders with the Mini International Neuropsychiatric Interview (M.I.N.I. 5.0.0), a short, structured diagnostic interview for DSM-IV (18) and ICD-10 (19) psychiatric disorders with good psychometric qualities. The interview was conducted with regard to the years after onset of the CAD. Mental disorders were grouped in depressive disorders (Major Depressive Episode and Dysthymia) and anxiety disorders (Agoraphobia, Panic Disorder, Social Phobia, Generalized Anxiety Disorder, Posttraumatic Stress Disorder, Obsessive Compulsive Disorder, and Hypochondria). Other severe mental disorders were assessed but excluded from further analyses due to low frequency: of the participants who did not meet criteria for a depressive or anxiety disorder, only eight met criteria for another severe mental disorder, e.g., bipolar, substance related, eating or somatoform disorder. Mild and moderate depressive episodes as well as adjustment disorders were not assessed.
Psychosocial Functioning
The Global Assessment of Functioning (GAF) of the DSM-IV was used to estimate psychosocial functioning on a scale from 1 to 100 (e.g., 1–10: severe impairment; 90–100 superior functioning) (20). This standard method of judgment of a participant’s current level of psychological, social, and occupational functioning has shown good psychometric properties (21, 22).
Utilization of Mental Health Care
As this was a preliminary, fact-finding study, we operationalized mental health care very broadly as any care by a certified professional meant to alleviate mental troubles. Accordingly, participants were asked if they had ever consulted a psychiatrist, been prescribed a drug for mental troubles, underwent outpatient PT (>4 sessions) or been hospitalized for mental disorders. In the case of an answer in the affirmative, timing of mental health care was assessed with regard to onset of the CAD. We did not collect data on the identities of the mental health professionals that provided care for the participants of our study. Of note, one particularity of the German mental health-care system is a high rate of voluntary hospitalizations for dosing of antidepressants and/or inpatient PT. None of the participants of our study reported an involuntary admission to a psychiatric hospital.
Procedure
Trained and regularly supervised interviewers of the psychological and medical staff of the University Hospital Schleswig-Holstein, Lübeck, Germany, contacted participants to inform them about the content and purpose of the survey. When consent was renewed, onset of CAD was determined, and the M.I.N.I. was conducted with regard to years before and after the onset of CAD as well as to the present. After scoring the GAF, the interviewers informed participants about access to treatment (if necessary). In the example of acute suicidality, which did not occur, study protocol specified alerting the psychiatrist on duty. At the end of the interview, participants were offered a summary of the research findings in layman’s terms upon completion of the study, in which case contact details were noted.
Statistical Analysis
SPSS 23 for Windows (SPSS Inc., USA) was used for all statistical analyses. To test for influence of the length of the interval between onset of CAD and the telephone interview on the prevalence rates of mental disorders and the utilization rates of mental health care, we performed point-biserial correlations. In χ2 tests, Cramér’s V was used to measure effect size, and z-test and standardized residuals to breakdown significant χ2 tests. Interactions in ANOVA were followed-up with t-tests and Games–Howell-post hoc tests as appropriate. To compensate for violations of assumptions regarding sampling distributions, resampling was applied where necessary using bias corrected and accelerated (BCa) bootstrapping with a significance level of 0.05. Due to the exploratory nature of the present study, we refrained from correction for multiple comparisons to prevent accumulation of β error.
Results
Sample Characteristics
Of the 1,182 participants who were contacted for the telephone survey, 269 could not be reached, 207 were known to be deceased, 138 declined consent, 26 suffered from communication problems such as insufficient language skills or hardness of hearing, 18 could not participate due to impairment of cognitive functions, and 13 participants were excluded for other reasons. Thus, response rate was 43.2%. The final sample consisted of 511 participants (75.9% male, mean age = 60.1 years, SD = 10.11). Mean onset of CAD was at 55.3 years (SD = 10.8).
Psychiatric Morbidity
In the years between CAD onset and the telephone interview (M = 10.9 years, SD = 8.2), 10.5% of participants met the criteria for an anxiety disorder, 11.3% for a depressive disorder, and 6.0% for both an anxiety and depressive disorder. 72.2% did not meet criteria for any depressive or anxiety disorder (unpublished data). These prevalence rates did not correlate with the length of the interval between CAD onset and the telephone interview (all rs ε [−0.05; 0.05], all ps ≥ 0.180).
Utilization of Mental Health Treatment
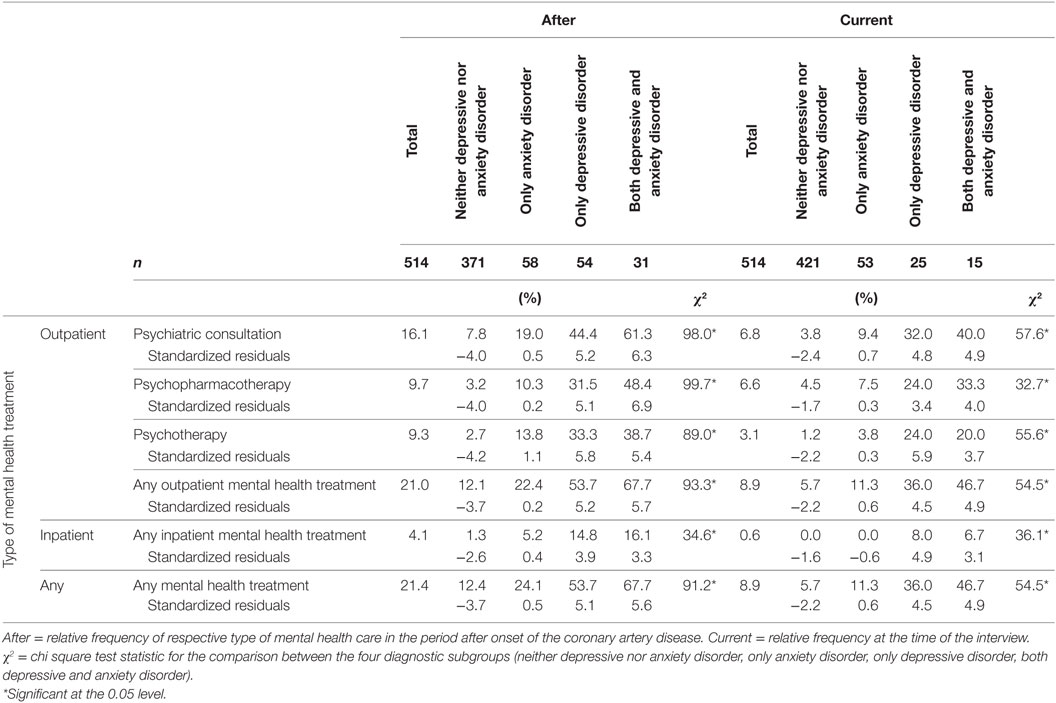
The global utilization rate of mental health care was 20.1% and was highest in participants with comorbid depressive and anxiety disorders (67.7%, see also Table 1), followed by participants with depressive disorders (53.7%). In comparison, participants with anxiety disorders (22.4%) and participants with neither depressive nor anxiety disorders (12.1%) were significantly less likely to have received mental health care [χ2(3) = 93.27, p < 0.001]. Utilization of all types of mental health treatment (psychopharmacologic, psychotherapeutic, or combination) was highest in participants with depressive disorders, regardless of comorbidity with anxiety disorders [all χ2(3) ≥ 24.9, p < 0.001]. The same overall utilization pattern emerged regarding the utilization of outpatient mental health treatment at the time of the interview, only with lower frequencies (McNemar p < 0.001). None of the rates of utilization of mental health care correlated with the length of the interval between CAD onset and the telephone interview (all rs ε [−0.08; 0.07], all ps ≥ 0.073).
Utilization of inpatient mental health treatment was highest in participants with comorbid depressive and anxiety disorders (16.1%), followed by participants with depressive disorders (14.8%). Participants with anxiety disorders (5.2%) and participants with neither depressive nor anxiety disorders (1.3%) again were significantly less likely to have received inpatient mental health care [χ2(3) = 34.61, p < 0.001]. Overall utilization of inpatient mental health treatment was lower (McNemar’s p < 0.001) with only participants with depressive disorders (with or without comorbid anxiety disorders, 3.7 or 3.2%, respectively) currently in inpatient mental health care.
Psychopharmacotherapy without specialist (namely, psychiatric) consultation was uncommon (22% of participants receiving medication) and occurred mainly among participants meeting criteria for neither depressive nor anxiety disorders (61.5%).
There was no significant gender difference in the global utilization of mental health care or for any specific type of mental health treatment.
Binary logistic regression was performed to identify predictors of receiving mental health care after onset of CAD. A model including age at onset of CAD, gender, utilization of mental health treatment before onset of CAD, GAF after onset of CAD, depressive disorders and anxiety disorders after onset of CAD was a significant fit for the data [χ2(6) = 117.70, p < 0.001, R2 = 0.22 (Cox and Snell), =0.33 (Nagelkerke’s), Hosmer–Lemeshow Test: χ2(8) = 6.69, p = 0.57]. Participants with younger age at onset of CAD as well as low GAF after onset of CAD were more likely to receive any kind of mental health treatment [Wald (1) = 5.94, p = 0.02; Wald (1) = 27.36, p < 0.001]. Participants with depressive disorder were 2.7 times more likely to receive any kind of mental health treatment [Wald (1) = 8.1, p = 0.004], whereas meeting criteria for an anxiety disorder did not significantly predict the utilization of mental health care (OR = 1.3). Likewise, neither gender nor previous utilization of mental health treatment was predictors of utilization of mental health treatment after onset of the CAD.
Participants with depressive disorders were as likely to receive psychopharmacotherapy (37.6%) as PT (35.3%; McNemar’s χ2 = 0.04, p = 0.85).
Interaction between Treatment Patterns and Course of Psychosocial Functioning
To quantify proxy markers of effectiveness of mental health treatment in CAD patients, we conducted an ANCOVA with gender, depressive disorder, anxiety disorder, medication, and PT (all after onset of the CAD) as fixed factors, age at onset and lowest GAF after onset of the CAD as covariates and difference between lowest GAF after onset of CAD and GAF at the time of the interview (Δ GAF) as criterion. There was a main effect for age [F(1, 450) = 8.38, p = 0.004, partial η2 = 0.02] with participants younger than 55 years of age at onset of their CAD gaining 3.78 GAF points fewer than older participants [T(547.10) = 3.96, BCa 95% CI = [1.95; 5.66], p = 0.001].
There was a main effect for minimum GAF after onset of the CAD [F(1, 450) = 90.64, p < 0.001, partial η2 = 0.17]. Participants whose GAF sank below 70 after onset of their CAD gained on average 9.63 GAF points more than those whose GAF never fell below 70 [T(264.79) = 9.96, BCa 95% CI = [7.84; 11.56], p = 0.001].
There was a main effect for gender [F(1, 450) = 5.42, p = 0.020, partial η2 = 0.01], with women gaining 5.1 GAF points (SE = 2.0) more than men.
There was a main effect for anxiety disorders [F(3, 450) = 8.48, p = 0.004, partial η2 = 0.02]. Participants with anxiety disorders gained 7.8 GAF points less than those without (SE = 1.9, p < 0.001). There was no main effect for depressive disorders [F(1, 450) = 0.31, p = 0.577, Δ GAF gain = 0.92 points].
There was a main effect for PT [F(3, 450) = 7.77, p = 0.006, partial η2 = 0.02]. Participants who underwent PT after onset of their CAD gained 5.51 GAF points more than those who did not (SE = 1.97, p = 0.005). This pattern held true when only subjects without depressive or anxiety disorders were included in the analysis [F(1, 336) = 17.81, p < 0.001, partial η2 = 0.05, Δ GAF gain = 16.16 points, BCa 95% SE = 2.33, CI = [10.43; 20.35], p < 0.001].
There was a three-way interaction between PT, anxiety disorders (AD), and gender [F(3, 450) = 8.05, p = 0.005, partial η2 = 0.02, see also Figure 1]. In women with anxiety disorders, PT was associated with higher GAF gain (MAD with PT = 10.58, SE = 4.06 vs. MAD without PT = 4.02, SE = 3.31), but this was not true in men (MAD with PT = 3.71, SE = 2.46 vs. MAD without PT = 3.57, SE = 2.27).
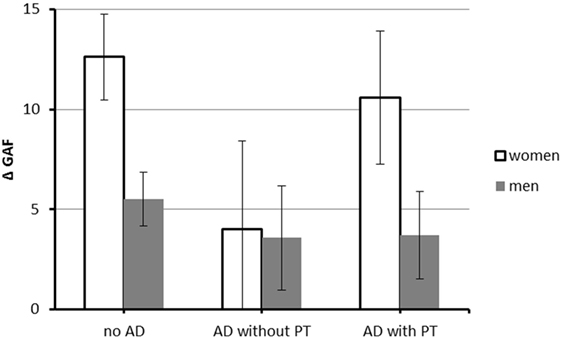
Figure 1. Interaction between anxiety disorders, PT, and gender on difference between minimum GAF after onset of coronary artery disease (CAD) and GAF at interview. N = 481 (117 women and 364 men). Abbreviations: GAF, Global Assessment of Functioning; AD, anxiety disorder; PT, psychotherapy. Values are corrected for the effect of covariates [age at onset of CAD, minimum GAF after onset of CAD]. Error bars indicate SE.
There was no main effect for medication [F(3, 450) = 0.10, p = 0.756, Δ GAF gain = 2.59 points], but a two-way medication × depressive disorders interaction was found [F(3, 450) = 6.10, p = 0.014, partial η2 = 0.01]; in participants with depressive disorders, medication was associated with higher GAF gain (Δ GAF gain = 7.53, BCa 95% SE 3.71, p = 0.040, CI = [0.28; 14.74]).
There was an interaction between PT and medication [F(3, 450) = 8.15, p = 0.004, partial η2 = 0.02]. PT and combination treatment were associated with higher GAF gain than no treatment (both M ≥ 11.24, both Games–Howell ps < 0.001), but no type of treatment was superior to another (all ps ≥ 0.48). There was also a three-way interaction between PT, medication, and gender [F(3, 450) = 22.05, p < 0.000, partial η2 = 0.05, see also Figure 2]. In women, PT (PT) was associated with the highest GAF gain (MPT = 24.07, SE 4.54 vs. MMED = 18.79, SE = 2.94 and MCOMB = 7.34, SE 3.89), whereas in men, combination therapy (COMB) was associated with the highest GAF gain (MCOMB = 12.74, SE = 2.81 vs. MMED = 4.72, SE = 2.34 and MPT = 6.06, SE 2.24).
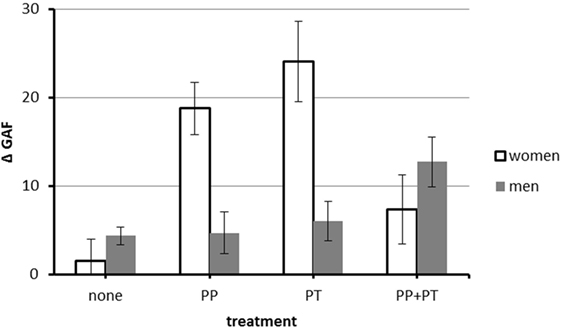
Figure 2. Interaction between PT, medication, and gender on difference between minimum GAF after onset of the coronary artery disease (CAD) and GAF at the interview. N = 481 (117 women and 364 men). Abbreviations: GAF, Global Assessment of Functioning; PP, psychopharmacotherapy; PT, psychotherapy. Values are corrected for the effect of covariates (age at onset of CAD, minimum GAF after onset of CAD). Error bars indicate SE.
Re-running this model with the length of the interval between onset of CAD and the telephone interview as additional covariate did not yield qualitatively different results and there was no main effect for the length of the interval [F(1, 449) = 0.38, p = 0.54, partial η2 = 0.00].
Discussion
In our sample, one in five participants had received mental health care after onset of their CAD, and one in two participants met criteria for an anxiety and/or depressive disorder. Apart from diagnoses, other predictors of mental health-care utilization were young age at onset of the CAD and low psychosocial functioning after onset of the CAD. PT was associated with higher gains in psychosocial functioning in all diagnostic groups, whereas medication was associated with higher gains only in participants with depressive disorders. On the contrary, male gender and anxiety disorders were associated with fewer gains in psychosocial functioning.
The utilization rates of general mental health care in our study of CAD patients were comparable to data from the respective age cohort of the general German population (23, 24), to data from a nationally representative sample of elderly persons with depressive symptoms and chronic somatic diseases (25) and to data from another chronically somatically ill sample in Germany, cancer patients (26). Some participants reported previous mental health treatment without meeting criteria for a depressive or anxiety disorder. They possibly suffered from mild mental disorders such as adjustment disorder (not taken into account in this study) or were prescribed medication in absence of a mental disorder (27–29).
Younger participants and participants with greater psychosocial impairment were more likely to seek mental health care, which is in agreement with data from the German general population (23) and U.S. patients with chronic somatic diseases and depression (30). Higher utilization of mental health care by younger patients may be attributable to higher distress (due to more severe practical consequences of psychological impairment, e.g., at work) or fewer barriers to seeking mental health treatment: younger CAD patients may have greater knowledge of mental health and be less prone to self-stigmatization.
One in two participants with a depressive episode reported to have received any mental health treatment (e.g., psychopharmacotherapy, PT, or a combination of both), which is comparable to data from the Medical Expenditure Panel Survey on depressed CAD patients in the U.S. (30). However, the patterns of treatment modality were strikingly different. Whereas participants in our study were as likely to receive PT as psychopharmacotherapy, the vast majority of participants in the U.S. received psychopharmacotherapy. This finding probably reflects differences in health insurance: for the vast majority of residents, costs for PT are reimbursed by German statutory health insurance. Therefore, roughly 10% of the German general population consulted a psychologist or psychotherapist in 2014, nearly twice the European average (31).
Participants with anxiety disorders were less likely to receive any mental health care than participants with depressive disorders, which is surprising as anxious cardiac patients are known to consult their general practitioners more frequently (32, 33). We hypothesize that patients and/or GPs have trouble recognizing anxiety disorders, which could be ameliorated by specific public education or psychological liaison services in cardiology.
Also, mental health care was not associated with higher gains in psychosocial functioning in participants with anxiety disorders. This finding may be due to a variety of reasons. Efficacy of psychopharmacotherapy for anxiety in CAD patients is uncertain as there is no evidence to date. Evidence-based PT is also not available as standard CBT for anxiety disorders (including exposure therapy) can have adverse somatic effects in CAD patients (34–37), and no adaptation for this patient population has yet been implemented. However, the PATCHD trial recently proved feasibility of such an adaption (15).
Surprisingly, in women, the combination of psychopharmacotherapy and PT was not associated with higher GAF gains compared with psychopharmacotherapy or PT alone.
A strength of the present study is its setting in routine health care as opposed to research centers, pointing to high ecologic validity of the results. The sample is also large and representative for Northern Germany. A high level of training for the interviewers, including regular supervision as well as assessment with two intensely validated, semi-structured interviews, the MINI and the GAF, allow for the assumption of good reliability of the findings.
However, our study is based on a convenience sample, which limits generalizability of the findings. The retrospective study design could have led to underestimation of utilization rates due to compromised recall and clearly reduced the reliability of GAF ratings. Using self-reported onset of CAD as a reference point without standardization of the time point of contacting by the study team led to different survey periods for each participant, which complicated the comparison of our findings with existing data on utilization rates of mental health care (while improving ecological validity). The assessment by telephone may have led to misunderstandings due to lack of nonverbal communication (reducing sensitivity) and selection bias, as critically ill and/or hospitalized patients are less likely to answer the telephone. Our operationalization of mental health care also did not consider length of treatment, increasing the risk of overestimation of participants receiving mental health treatment.
Outlook
As the associations between mental health, well-being and CAD have consistently been shown to be moderated by race, ethnicity and socioeconomic factors (16, 17), future studies should compare mental health-care utilization rates of CAD patients across countries and social environments.
Conclusion
To the best of our knowledge, this is the first study on utilization rates of mental health care in CAD patients in Northern Germany. One in five of all participants in our preliminary study and one in two participants who met criteria for major mental disorder reported to have received mental health care after onset of their CAD. The majority of CAD patients with comorbid depression reported to have received mental health treatment and seemed to have benefited from it. However, we found preliminary evidence for insufficiencies in the diagnosis and treatment of anxiety disorders in CAD patients in Germany. Further studies, preferably prospective and with representative samples, are needed to corroborate or falsify these findings and explore possible further mediators of health-care utilization by CAD patients such as race, ethnicity, and socioeconomic status.
Ethics Statement
This study was carried out in accordance with the recommendations of the ethics committee of the University of Lübeck, Germany, with written informed consent from all subjects. All subjects gave written informed consent in accordance with the Declaration of Helsinki. The protocol was approved by the ethics committee of the University of Lübeck, Germany (ID 04/041).
Author Contributions
BW, CW, HS, JE, and US contributed to the conception and design of the study; AW, AS, BW, and SN acquired the data and organized the database; AW, AS, and US performed the statistical analysis; AW and AS wrote the first draft of the manuscript. All the authors contributed to manuscript revision, read and approved the submitted version.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors thank all patients, research assistants, and students who participated in this study.
Funding
The study was funded by the University of Lübeck.
References
1. Chauvet-Gélinier J-C, Trojak B, Vergès-Patois B, Cottin Y, Bonin B. Review on depression and coronary heart disease. Arch Cardiovasc Dis (2013) 106(2):103–10. doi:10.1016/j.acvd.2012.12.004
2. Baumeister H, Haschke A, Munzinger M, Hutter N, Tully PJ. Inpatient and outpatient costs in patients with coronary artery disease and mental disorders: a systematic review. Biopsychosoc Med (2015) 9:11. doi:10.1186/s13030-015-0039-z
3. de Jager TA, Dulfer K, Pieters K, Utens EM, Daemen J, Lenzen MJ, et al. The association between subjective health status and 14-year mortality in post-PCI patients. Int J Cardiol (2017) 229:108–12. doi:10.1016/j.ijcard.2016.11.218
4. Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B. Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet (2007) 370(9590):851–8. doi:10.1016/S0140-6736(07)61415-9
5. Vogelzangs N, Seldenrijk A, Beekman AT, van Hout HP, de Jonge P, Penninx BW. Cardiovascular disease in persons with depressive and anxiety disorders. J Affect Disord (2010) 125(1–3):241–8. doi:10.1016/j.jad.2010.02.112
6. Van Dijk MR, Utens EM, Dulfer K, Al-Qezweny MN, van Geuns R-J, Daemen J, et al. Depression and anxiety symptoms as predictors of mortality in PCI patients at 10 years of follow-up. Eur J Prev Cardiol (2016) 23(5):552–8. doi:10.1177/2047487315571889
7. Szpakowski N, Bennell MC, Qiu F, Ko DT, Tu JV, Kurdyak P, et al. Clinical impact of subsequent depression in patients with a new diagnosis of stable angina. Circ Cardiovasc Qual Outcomes (2016) 9(6):731–9. doi:10.1161/CIRCOUTCOMES.116.002904
8. Assari S, Lankarani MM, Ahmadi K. Comorbidity influences multiple aspects of well-being of patients with ischemic heart disease. Int Cardiovasc Res J (2013) 7(4):118–23.
9. Pizzi C, Mancini S, Angeloni L, Fontana F, Manzoli L, Costa G. Effects of selective serotonin reuptake inhibitor therapy on endothelial function and inflammatory markers in patients with coronary heart disease. Clin Pharmacol Ther (2009) 86(5):527–32. doi:10.1038/clpt.2009.121
10. Lesperance F, Frasure-Smith N, Koszycki D, Laliberte MA, van Zyl LT, Baker B, et al. Effects of citalopram and interpersonal psychotherapy on depression in patients with coronary artery disease: the Canadian Cardiac Randomized Evaluation of Antidepressant and Psychotherapy Efficacy (CREATE) trial. JAMA (2007) 297(4):367–79. doi:10.1001/jama.297.4.367
11. Herrmann-Lingen C, Beutel ME, Bosbach A, Deter H-C, Fritzsche K, Hellmich M, et al. A stepwise psychotherapy intervention for reducing risk in coronary artery disease (SPIRR-CAD): results of an observer-blinded, multicenter, randomized trial in depressed patients with coronary artery disease. Psychosom Med (2016) 78(6):704–15. doi:10.1097/PSY.0000000000000332
12. Norlund F, Olsson EM, Pingel R, Held C, Svärdsudd K, Gulliksson M, et al. Psychological mediators related to clinical outcome in cognitive behavioural therapy for coronary heart disease: a sub-analysis from the SUPRIM trial. Eur J Prev Cardiol (2017) 24(9):917–25. doi:10.1177/2047487317693131
13. Gulliksson M, Burell G, Vessby B, Lundin L, Toss H, Svärdsudd K. Randomized controlled trial of cognitive behavioral therapy vs standard treatment to prevent recurrent cardiovascular events in patients with coronary heart disease: secondary prevention in Uppsala primary health care project (SUPRIM). Arch Intern Med (2011) 171(2):134–40. doi:10.1001/archinternmed.2010.510
14. Tully PJ, Cosh SM, Baumeister H. The anxious heart in whose mind? A systematic review and meta-regression of factors associated with anxiety disorder diagnosis, treatment and morbidity risk in coronary heart disease. J Psychosom Res (2014) 77(6):439–48. doi:10.1016/j.jpsychores.2014.10.001
15. Tully PJ, Sardinha A, Nardi AE. A new CBT model of panic attack treatment in comorbid heart diseases (PATCHD): how to calm an anxious heart and mind. Cogn Behav Pract (2017) 24(3):329–41. doi:10.1016/j.cbpra.2016.05.008
16. Assari S. Race and ethnic differences in additive and multiplicative effects of depression and anxiety on cardiovascular risk. Int J Prev Med (2016) 7:22. doi:10.4103/2008-7802.173931
17. Assari S, Moghani Lankarani M. Association between heart disease and subjective health in ten north, middle, and South American countries. Int J Travel Med Glob Health (2014) 2(4):141–7.
18. Saß H, Wittchen H-U, Zaudig M. Diagnostisches und Statistisches Manual psychischer Störungen-DSM-IV. Deutsche Bearbeitung u. Einleitung von H. Sass, H.-U. Wittchen, M. Zaudig. Göttingen: Hogrefe (1996).
19. World Health Organization. Internationale Klassifikation psychischer Störungen - ICD 10 Kapitel V (F). 8 ed. Bern: Verlag Hans Huber, Hogrefe AG (2011).
20. American Psychiatric Association. Statistical Manual of Mental Disorders (DSM-IV). Washington, DC: American Psychiatric Association (1994).
21. Hilsenroth MJ, Ackerman SJ, Blagys MD, Baumann BD, Baity MR, Smith SR, et al. Reliability and validity of DSM-IV axis V. Am J Psychiatry (2000) 157(11):1858–63. doi:10.1176/appi.ajp.157.11.1858
22. Sonesson O, Tjus T, Arvidsson H. Reliability of a functioning scale (GAF) among psychiatric ward staff. Nord Psychol (2010) 62(1):53. doi:10.1027/1901-2276/a000005
23. Rattay P, Butschalowsky H, Rommel A, Prutz F, Jordan S, Nowossadeck E, et al. [Utilization of outpatient and inpatient health services in Germany: results of the German Health Interview and Examination Survey for Adults (DEGS1)]. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz (2013) 56(5–6):832–44. doi:10.1007/s00103-013-1665-x
24. Maercker A, Enzler A, Grimm G, Helfenstein E, Ehlert U. [Psychotherapy service utilization and psychotherapy motivation in a representative community sample of the elderly – results of the Zurich older age study]. Psychother Psychosom Med Psychol (2005) 55(3–4):177–82. doi:10.1055/s-2004-828510
25. Rommel A, Bretschneider J, Kroll LE, Prütz F, Thom J. Inanspruchnahme psychiatrischer und psychotherapeutischer Leistungen – Individuelle Determinanten und regionale Unterschiede. Journal of Health Monitoring (2017) 2(4). doi:10.17886/RKI-GBE-2017-111
26. Faller H, Weis J, Koch U, Brähler E, Härter M, Keller M, et al. Utilization of professional psychological care in a large German sample of cancer patients. Psychooncology (2017) 26(4):537–43. doi:10.1002/pon.4197
27. Aarts N, Noordam R, Hofman A, Tiemeier H, Stricker BH, Visser LE. Utilization patterns of antidepressants between 1991 and 2011 in a population-based cohort of middle-aged and elderly. Eur Psychiatry (2014) 29(6):365–70. doi:10.1016/j.eurpsy.2014.02.001
28. Takayanagi Y, Spira AP, Bienvenu OJ, Hock RS, Carras MC, Eaton WW, et al. Antidepressant use and lifetime history of mental disorders in a community sample: results from the Baltimore Epidemiologic Catchment Area study. J Clin Psychiatry (2015) 76(1):40. doi:10.4088/JCP.13m08824
29. Wiechers IR, Leslie DL, Rosenheck RA. Prescribing of psychotropic medications to patients without a psychiatric diagnosis. Psychiatr Serv (2013) 64(12):1243–8. doi:10.1176/appi.ps.201200557
30. Loeb DF, Ghushchyan V, Huebschmann AG, Lobo IE, Bayliss EA. Association of treatment modality for depression and burden of comorbid chronic illness in a nationally representative sample in the United States. Gen Hosp Psychiatry (2012) 34(6):588–97. doi:10.1016/j.genhosppsych.2012.07.004
31. Eurostat. Eigene Angaben zur Konsultation von Fachpersonen für psychische Gesundheit oder für rehabilitative Pflege, nach Geschlecht, Alter und Bildungsabschluss. (2018). Available from: http://appsso.eurostat.ec.europa.eu/nui/show.do?dataset=hlth_ehis_am2e&lang=de (accessed March 2, 2018).
32. Nielsen TJ, Vestergaard M, Fenger-Grøn M, Christensen B, Larsen KK. Healthcare contacts after myocardial infarction according to mental health and socioeconomic position: a population-based cohort study. PLoS One (2015) 10(7):e0134557. doi:10.1371/journal.pone.0134557
33. Iles-Smith H, McGowan L, Campbell M, Mercer C, Deaton C. A prospective cohort study investigating readmission, symptom attribution and psychological health within six months of primary percutaneous coronary intervention. Eur J Cardiovasc Nurs (2015) 14(6):506–15. doi:10.1177/1474515114543227
34. Rozanski A, Blumenthal JA, Kaplan J. Impact of psychological factors on the pathogenesis of cardiovascular disease and implications for therapy. Circulation (1999) 99(16):2192–217. doi:10.1161/01.CIR.99.16.2192
35. Fleet R, Lespérance F, Arsenault A, Grégoire J, Lavoie K, Laurin C, et al. Myocardial perfusion study of panic attacks in patients with coronary artery disease. Am J Cardiol (2005) 96(8):1064–8. doi:10.1016/j.amjcard.2005.06.035
36. Oldenburg O, Spießhöfer J, Fox H, Bitter T, Horstkotte D. Cheyne-Stokes respiration in heart failure: friend or foe? Hemodynamic effects of hyperventilation in heart failure patients and healthy volunteers. Clin Res Cardiol (2015) 104(4):328–33. doi:10.1007/s00392-014-0784-1
Keywords: coronary artery disease, depressive disorders, anxiety disorders, mental health care, utilization behavior, psychosocial functioning, health services research, treatment outcome
Citation: Westermair AL, Schaich A, Willenborg B, Willenborg C, Nitsche S, Schunkert H, Erdmann J and Schweiger U (2018) Utilization of Mental Health Care, Treatment Patterns, and Course of Psychosocial Functioning in Northern German Coronary Artery Disease Patients with Depressive and/or Anxiety Disorders. Front. Psychiatry 9:75. doi: 10.3389/fpsyt.2018.00075
Received: 19 January 2018; Accepted: 23 February 2018;
Published: 12 March 2018
Edited by:
Michael Noll-Hussong, Universitätsklinikum des Saarlandes, GermanyReviewed by:
Shervin Assari, University of Michigan, United StatesHideki Hashimoto, University Hospital Medical Information Network, Japan
Copyright: © 2018 Westermair, Schaich, Willenborg, Willenborg, Nitsche, Schunkert, Erdmann and Schweiger. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Anna Lisa Westermair, anna.westermair@uksh.de
†These authors share first authorship and contributed equally to this work.
 Anna Lisa Westermair
Anna Lisa Westermair Anja Schaich
Anja Schaich Bastian Willenborg
Bastian Willenborg Christina Willenborg2,3,4
Christina Willenborg2,3,4 Jeanette Erdmann
Jeanette Erdmann Ulrich Schweiger
Ulrich Schweiger