- 1Department of Psychiatry, University of Michigan, Ann Arbor, MI, United States
- 2Center for Research on Ethnicity, Culture and Health, School of Public Health, University of Michigan, Ann Arbor, MI, United States
- 3Division of Community Health Sciences, School of Public Health, University of Illinois at Chicago, Chicago, IL, United States
- 4HIV/AIDS, Substance Abuse and Trauma Training Program, University of California, Los Angeles, Los Angeles, CA, United States
Background: Although male partners' socioeconomic status (SES) and substance use is associated with worse health of female partners, the mechanism behind this link is still unknown.
Objectives: To investigate whether intimate partner violence (IPV) is a mechanism by which male partners' SES and substance use influence female partners' self-rated health (SRH) as victims and survivors of IPV.
Materials and Methods: Fragile Families and Child Wellbeing Study (FFCWS) is an ongoing population-based cohort. Male and female partners' SES, anxiety, depression, and substance use, and their relationship status were measured at baseline. IPV victimization was also asked among female partners' at baseline. Female partners' subjective health was measured 3 times (baseline−1998, 3 years later−2001, and 5 years later−2003). Using AMOS, we fitted two structural equation models (SEM) for data analysis. In Model 1 we tested direct paths from male partners' SES and mental health to female partners' SRH, in the absence of IPV. In the Model 2 we conceptualized female partners' IPV victimization between male partners' SES and mental health and female partners' SRH. In both models we controlled for the effect of female partners' SES and mental health.
Results: In Model 1, male partners' poor SES and substance use were associated with worse trajectory of SRH of female partner. In Model 2, male to female IPV was the mechanism by which male partners' SES and substance use were associated with female partners' SRH.
Conclusions: IPV is one of the mechanisms by which male partners' SES and substance use can influence female partners' health. That is, IPV may operate as a vehicle by which male partners' social and psychological risk factors impact female partners' health. Thus, this study demonstrates how male partners' socio-ecological risk factors such as low SES and substance use impact female partners' health. Therefore, there is a need for broader socio-ecological approach to IPV prevention and intervention that recognizes the relationship between male partners' risk factors and their female partners' health outcomes. Such approach can inform prevention and treatment of IPV and enhance partner wellbeing.
Background
Intimate Partner Violence (IPV) is a serious public health problem (1). Although both males and females may use violence against their partners, male to female IPV is more common than female to male IPV (2). Based on the World Report on Violence and Health, up to 69% of women experience physical abuse during their lifetime (3). In the United States, 29% of women experience physical violence, rape, and/or stalking by an intimate partner, 24% experience severe physical violence by an intimate partner, and 15% become injured as a result of IPV (4–6).
Exposure to IPV is associated with poor psychological and physical health (7). IPV victims also report worse overall health and sense of well-being, which hinders their ability to live a life without pain and suffering. In a study, quality of life was worse across physical health, social relationship, environment, and psychological health domains in women who had experienced IPV (8). Other studies have also documented poor quality of life of victims of physical, psychological and sexual IPV (9–11).
Most of the research on male to female IPV has focused on either the perpetrator or the victim (12–14), with minimum research on if male to female IPV is the actual mechanism by which male SES influence females' sense of well-being. The role of male to female IPV as a mechanism by which male partner socio-economic status (SES) factors and mental health influences female partner health is not fully investigated (15). The well-established associations identified during the last 30 years include a link between SES and IPV (16). Research has shown that separated or divorced women, those with unemployed partners, and people with low household income experience more abuse (17). Analysis of the National Crime Victimization Survey data showed that young women (age 19–29) in low-income families (under $10,000) are more likely than other women to experience IPV (18).
Another segment of IPV research that has not been fully investigated is whether IPV is a mechanism by which male partner mental health impacts female partner well-being. A few studies have shown that early-onset of mental disorders may increase risk of IPV perpetration among men (19–21). In one study, premarital Major Depressive Disorder (MDD), Generalized Anxiety Disorder (GAD), antisocial behavior, and non-affective psychosis predicted IPV perpetration among married or cohabiting men in the United States general population (19). Substance use increases risk of IPV perpetration (22), while alcohol misuse is one of the most established risk factors for IPV perpetration (22–25). Several female IPV victims report that their male partners had consumed alcohol in the episode of violence (26). Involvement in illicit drug use also increases the risks of IPV perpetration (27). As a result, World Health Organization (WHO) has used the term drug-related IPV (27). Again, it is still unknown whether IPV can operate as one of the potential mechanisms by which male partners' mental health problems impact female partners' health and sense of well-being.
The current study tested the role of IPV as a mechanism by which male partners' poor SES and substance use affect poor well-being of female partner. We conceptualized male to female's IPV as a bridge connecting male partners' SES and substance use to well-being of female partner.
Methods
Design and Setting
Fragile Families and Child Wellbeing Study (FFCWS) is an ongoing population-based cohort of 4,898 male and female partners, started in 1998. Participants were male and female partners who had a newborn in 20 U.S. cities with populations of 200,000 or more. Baseline data were collected in 75 hospitals across 20 cities. From all participants, 3,712 couples were unmarried and 1,186 couples were married at baseline. A detailed description of the FFCWS sampling strategy and interview protocol is available (28).
Ethics
The study protocol was approved by Institutional Review Board Committees at Princeton University and Columbia University. Verbal and written informed consent was obtained from participants at each interview, and all participants were compensated for their involvement in the study.
Process
Data were collected during core interviews and the add-on in-home interviews (more in-depth interviews that collected additional data). Male and female partners were interviewed at baseline-1998 (near the time of the target child's birth), 1 year later (Wave 2), 3 years later (Wave 3) and 5 years later.
The Fragile Families and Child Wellbeing Study has oversampled non-married couples (28). As non-marital unions are at greater risk for relationship instability, a large number of male partners were not living with female partners in Waves 2 or 3. For instance, by the time the study target child was 3 years old, fewer than half of male partners were residing in the home.
Measures
Most variables were based on paternal self-report. Male to female IPV was based on female partners' self-report.
Outcomes
Male to Female Physical IPV
Physical IPV was assessed by asking female partners four questions, on a 3-point scale (“never,” “sometimes,” or “often”), regarding how often the male partner carried out behaviors toward the female partner, (e.g., slapping, kicking, hitting with fist, hitting with an object). Items were adapted from the Conflict Tactics Scale (CTS-2) for adults (29, 30). The original and revised Conflict Tactics Scales (29, 30) have been the most common research measures of domestic violence, and the 1996 version includes separate measures of psychological dimensions, physical violence, sexual violence and financial control. The physical violence items of the CTS are still the most widely used approach to assessing levels of domestic violence (31).
Predictors
Major Depressive Disorder (MDD) and Generalized Anxiety Disorder (GAD)
The Composite International Diagnostic Interview - Short Form (CIDI - SF), Section A (32) was used to measure MDD and GAD. The CIDI-SF is a standardized instrument that is consistent with the criteria set forth in the Diagnostic and Statistical Manual of Mental Disorders – Third Edition – Revised (DSM-III-R) (33). This instrument has good reliability and validity for measurement of MDD and GAD (32). The CIDI-SF uses the criteria set forth in the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) to determine the probability that the respondent would be diagnosed with MDD, GAD, and other psychiatric disorders if given the full CIDI interview. MDD is indicated by feelings of depression or anhedonia experienced for most of the day, every day, for at least 2 weeks. Participants were classified as likely to have MDD if they endorsed the screening items and 3 or more depressive symptoms (e.g., losing interest, feeling tired, change in weight) (0 = no, 1 = yes). GAD is indicated by a period of 6 months or more when an individual feels excessively worried or anxious about more than one thing, more days than not, and has difficulty controlling their worries. Common symptoms of GAD include being keyed up or on edge, irritability, restlessness, having trouble falling asleep, tiring easily, difficulty concentrating and tense or aching muscles. Subjects were classified as having GAD if they met full diagnostic criteria based on the CIDI-SF (0 = no, 1 = yes).
Substance Use
Tobacco use, alcohol use and illicit drug use were measured. This measure was operationalized as a latent factor in this study. All of the drug and alcohol abuse data used in this analysis are drawn from female partner's reports. This is because of considerable proportion of missing data in male partners' report data (primarily due to attrition and/or refusal to participate among male partners who do not live with their child). Thus, we relied only on female partners' reports.
Self-Rated Health (SRH)
Female respondents were asked to classify their self-rated health as excellent, very good, good, fair, or poor. We treated SRH as a continuous score. SRH is coded from 1 (excellent) to 5 (poor), with higher values indicative of worse SRH. Poor SRH is a strong predictor of mortality (34–36).
Socioeconomic Status (SES)
All following SES variables were measured at the baseline interview (Wave 1): age, education level, income, minority status, and relationship status. Partners' demographic factors included household income, age at the time of the child's birth, education level (1 = less than high school, 2 = high school degree or GED, 3 = some college/technical school or higher), and relationship status (1 = married, 2 = cohabiting, 3 = not married or cohabiting).
Analysis Plan
We used SPSS 20 for our univariate and bivariate analysis. The Pearson correlation test was used for bivariate associations between male partners' SES, and male partners' mental health, female partners' SES, IPV, and female partners' SRH. We used AMOS for multivariable analysis. We fitted two structural equation models (SEM) for data analysis.
Model 1 included direct paths from male partners' SES (a latent factor) and male partners' substance use to female partners' baseline and trajectory of SRH, while the effect of female partners' SES and mental health is controlled.
In Model 2, we hypothesized that male partners' SES and male partners' substance use would be associated with IPV victimization among female partners, and that female partners' IPV victimization would be in turn associated with female partners' trajectory of SRH. In both models, female partners' SES and mental health (i.e., depression, anxiety, and substance use) were control variables.
The chi-square test, comparative fit index (CFI), root mean square error of approximation (RMSEA), and chi-square to degree of freedom ratio were considered as fit indices. A CFI of higher than 0.90, RMSEA of lower than 0.08 and chi-square test to degree of freedom ratio less than 4 were indicative of good fit (37). Although variables measured at baseline data did not have considerable missing values, variables measured at other waves had more missing values. We did not impute the data.
Missing Data
AMOS uses the Full Information Maximum Likelihood (FIML) method to handle missing data. So, all available data from all participants contribute to SEM models, even in the presence of missing data due to loss to follow up. This approach reduces selection bias due to complete data analysis. This approach is in contrast to Listwise or case deletion (deleting any case that has any missing value), as it preserves all cases that enter to the original study (38).
Results
Bivariate Analysis
Based on bivariate analysis, female SES, GAD, MDD, and substance use were significantly associated with female SRH. Education, relationship, marriage status, and cohabitation status all had marginally significant association with baseline SRH. Female partners' poverty index, Black race, and GAD were significantly associated with change of SRH over time. Age, employment, MDD and substance use all had marginally significant association with SRH over time.
Unconditional Model of the Outcome
Unconditional model of baseline and slope of female partners SRH showed an excellent fit to the data. There was a strong and negative correlation between baseline and trajectory of SRH among female partners (B = 0.67, P < 0.001), suggesting that female partners who started with a higher SRH at baseline were those who experienced a better trajectory of SRH over time. Baseline (variance = 12.36, SE = 0.97, P < 0.001) and slope (variance = 1.84, SE = 0.20, P < 0.001) of SRH of the female partners showed significant variance, suggesting that their variance can be used as an outcome in the models. Thus, we considered baseline and slope as outcomes in the following two models (Model 1 and Model 2).
Model 1
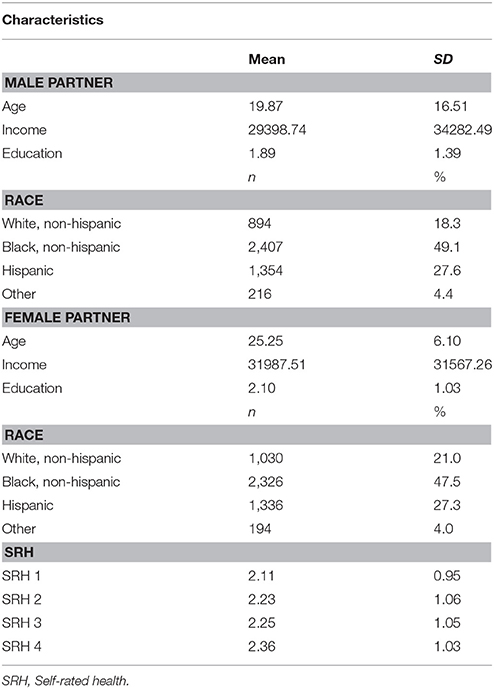
In Model I, we tested direct paths from male partners' SES, MDD, GAD, and substance use to baseline and slope of female partners' SRH. The model showed a good fit [Chi-square = 14437.514, Probability level < 0.001, Degrees of freedom = 348, CFI = 0.936, RMSEA = 0.090]. Our findings suggested that while the effect of female partners' SES and mental health are controlled, male partners' MDD and GAD do not have any association with baseline or slope of SRH among female partners. However, male partner SES and SU were directly associated with both baseline and slope of SRH among female partners in this model (Table 1).
Model 2
In Model 2, we tested the full model in which female partner IPV victimization was conceptualized as an intermediate mechanism that links male partners' predictors to female partners' SRH. The model showed a good fit (Probability level = 0.000, Degrees of freedom = 474, CFI = 0.954, RMSEA = 0.080). Based on this model, there were significant paths from male partners' MDD and GAD (in addition to SES and substance use) to female partners' IPV victimization. Female partner IPV victimization was also associated with SRH among female partners (Table 2).
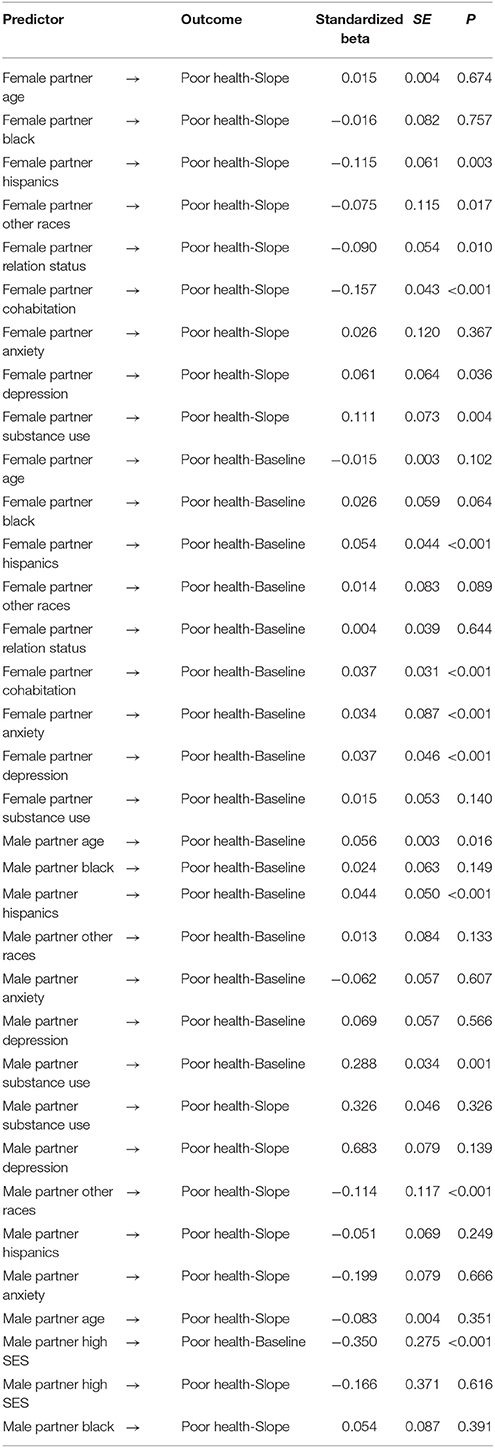
Table 2. Summary of Model 1 that tests the associations between male and female partners' SES, mental health and female partners' self-rated health in the absence of female IPV victimization in the model.
The results suggest that in the absence of considering IPV as an intermediate mechanism, male partners' MDD and GAD do not show an association with female partners' SRH. However, when we take into account IPV as a possible mechanism, male partners' MDD and GAD influence female partners' SRH through IPV victimization of the female partner. In contrast, to document the association between male partners' SES and substance use and female partners' SRH, there is no need to consider IPV as an intermediate factor.
Discussion
The current study showed two findings. First, male partners' poor SES and alcohol abuse were associated with worse trajectory of SRH among female partner. Second, IPV may be a mechanism by which male partners' psychosocial factors such as SES and substance can influence female partners' mental health outcomes.
These findings emphasize the relevance of socioecological models for predicting and contextualizing the risks, occurrence and impact of IPV (39). Our finding reinforces the basis of the social ecological model (SEM) of health promotion that emphasizes a broader understanding of among the individual, relationship, community and societal factors that enable violence. Our study establishes a clear understanding that contextual factors male perpetrator such as his SES and substance use increase the health consequences among female IPV victims and survivors (40–43). From such vantage point, we are able to assess that IPV is more than just an act of violence but can be situated with multi-factoral reasons that influences a person's health and wellbeing. SEM approach to IPV demonstrares how IPV is manifested and sustained beyond physical abuse and toward the mental health outcomes observed in our study. Therefore, it is important to consider the prevention and intervention of intimate partner violence have to conceptualized from multi-level approach to reduce the public health consequences (44).
Our study also reinforces ample evidence that substance use and substance use disorders are proven associations among male perpetrated IPV (45–47). Bennett and Williams (48) assert that “intimate partner violence cannot be well explained as a simple sequela of substance use” (p. 560); however, they identify that there is an apparent relationship between the two, and a number of studies point to how substance use can shape violence. For instance, cocaine and marijuana use are associated with increased odds of aggression perpetration (45), as is alcohol use (49). Furthermore, Stuart et al. (52) found 31% of men arrested for domestic violence met criteria for a drug use disorder and 53% met criteria for an alcohol use disorder. Substance use and abuse with IPV enables a degree of trauma for both perpetrators and victims that have consequences on their health outcomes. The risk of domestic violence among men is also linked to mental health symptomatology. Research has shown that antisocial personality disorder (ASPD) and borderline personality disorder (BPD) traits are associated with the perpetration of IPV (47, 50) Additionally, Holtzworth-Munroe and Stuart's (51) typologies of IPV perpetrators were defined, in part, by borderline/dysphoric (BD) and generally violent/antisocial (GVA) features, both of which are associated with increased rates of perpetration (38). Studies have shown that these are often predictive of who recidivates after participating in batterer intervention programs (BIP) (52, 53). Our finding shows that IPV is one reason why poor SES and substance abuse transcend beyond the male perpetrator and become a health issue for IPV-exposed female.
Our finding shows male partners' SES and substance abuse are associated with the trajectory of the female partners' SRH. Such finding provides additional context to the existing literature about the interplay between SES, substance use, IPV, and health (16, 54, 55). Perpetrator's SES does impact female partner health status. Such finding suggests that the effects of low SES and poor mental health of one partner stress to traumatize and impact the health of another partner. There is a call for evaluation of IPV in families and couples where male partner has low SES and substance use problem. Male partner SES and substance use may have implications for well-being of the other partner.
This research also supports the literature that suggests low SES and substance abuse increase risk of IPV within families (56–58). In our analysis, IPV is a mechanism by which low SES and substance use in male partner impacts female partners' health (See Table 3). This study proposes that female partners well-being should be seen in a relational view, and promotion of female partner well-being may require IPV prevention, particularly in the presence of substance use and low SES.
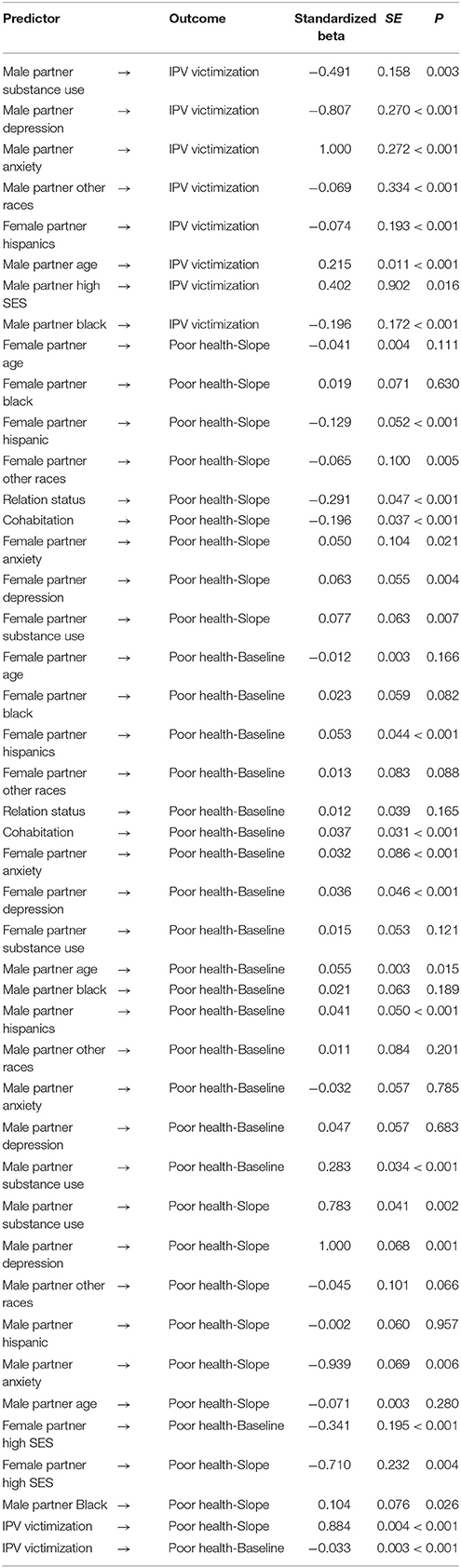
Table 3. Summary of Model 2 that tests the associations between male and female partners' SES, mental health, IPV, and female partners' self-rated health conceptualizing female IPV victimization as an intermediate variable.
More inquiries are needed to better understand the complex links between SES, substance use, IPV, and well-being of the partners. More efforts are needed to understand how coping, communication, and conflict explain the effect of IPV on male partner characteristics on female partner well-being. Well-being of a partner should be seen as interdependent with the SES and behavioral profile of her partner, and the presence of violence in the relationship.
This work draws attention to male partners' psychosocial factors (e.g., SES and substance use) (57, 59, 60) as risk factors of IPV that in turn impacts the health and wellbeing of women. There is a need to consider SES and behaviors of men as perpetrators to improve the health outcomes and coping strategies of women. We have learned that though these elements may or may not impact the lives of women in the absence of IPV, when IPV is present, the linkage to a woman's health and wellbeing is impactful (41).
Our finding suggests that when considering ways to promote well-being of women, male partners' SES and substance use and associated male to female IPV should be considered. It is imperative that IPV prevention is delivered to low SES families with the history of substance use problems. In addition, programs should integrate ways to screen and treat anxiety, depression, and substance abuse of the male perpetrators.
A more careful consideration must be given into how IPV prevention should be regarded as a core element of programs that wish to enhance well-being of low SES families that have low SES and substance use problem. IPV victims should receive health evaluation.
Limitations
The current study had several limitations. First, it only used a few items from CTS to measure IPV. Second, it only measured physical not psychological or sexual IPV. There are a number of unmeasured confounders such as physical health problems in female partner. In addition, the study was exclusively limited to heterosexual couples. Finally, we used female partners' reports of independent variables (See Figure 1). This decision was based on several reasons. First, we were only interested in male to female IPV, In addition, in the FFCWS, male and female partners' reports of the same variables do not have high concordance. As the FFCWS has enrolled an economically disadvantaged population which is composed of mostly unmarried couples, many households are headed by the female partner (single headed households), thus the female partners' reports may be considered more reliable and accurate than male partners' reports of the same constructs (14).
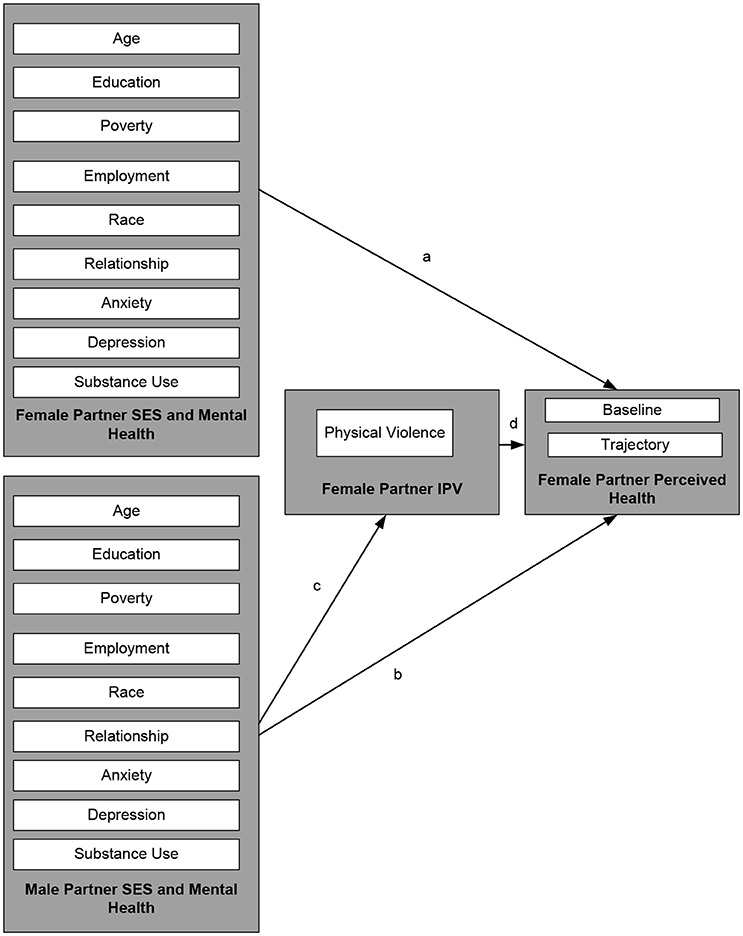
Figure 1. Conceptual model and modeling approach: In Model I, paths c and d were absent. In Model II, paths a, b, c, and d were tested.
Implication for Health Policy Makers/Practice/Research/Medical Education
The study suggests that intimate partner violence may be a bridge between male partners' mental health to female partners' perceived health. The study highlights a need for multi-dimensional approach to the prevention of intimate partner violence as a strategy for health promotion of women who's male partner/spouse has poor mental health.
Conclusion
While more than 30 years of IPV research has shown that SES and mental health problems increase risk of IPV, and IPV reduces sense of well-being, it was not known whether male to female IPV is the mechanism by which male SES and mental health problems influence female partner health and wellbeing. This study suggests that IPV, a public health challenge, is one reason why male partners' characteristics influence female partners' well-being. More research is needed to understand how these findings can inform prevention and treatment of IPV and to enhance wellbeing of partners. Screening and treatment of substance use among male partners may be an important component of prevention and treatment of IPV and enhancing female partners' partner wellbeing.
Authors Contributions
SA: design, analysis, early draft and also revision of the manuscript; RJ: literature review and discussion, early draft and revision of the manuscript draft.
Funding
The project was supported by the Eunice Kennedy Shriver National Institute of Child Health & Human Development Award Numbers R01HD066054 (to IG), R01HD036916 (to IG), and P2CHD058486 (to IG). The content is solely the responsibility of the authors and does not necessarily represent the official views of the Eunice Kennedy Shriver National Institute of Child Health & Human Development or the National Institutes of Health. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. Agencies that provided funding support: Eunice Kennedy Shriver National Institute of Child Health & Human Development, Eunice Kennedy Shriver National Institute of Child Health & Human Development through the Office of Population Research, Princeton University, National Science Foundation, U.S. Department of Health and Human Services (ASPE and ACF), California HealthCare Foundation, The Center for Research on Religion and Urban Civil Society at the University of Pennsylvania, Commonwealth Fund, Ford Foundation, Foundation for Child Development, Fund for New Jersey, William T. Grant Foundation, Healthcare Foundation of New Jersey, William and Flora Hewlett Foundation, Hogg Foundation, Christian A. Johnson Endeavor Foundation, Kronkosky Charitable Foundation, Leon Lowenstein Foundation, John D. and Catherine T. MacArthur Foundation, A.L. Mailman Family Foundation, Charles Stewart Mott Foundation, David and Lucile Packard Foundation, Public Policy Institute of California, Robert Wood Johnson Foundation, St. David's Hospital Foundation, St. Vincent Hospital and Health Services.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
With special thanks to the other members of the Fragile Families Working Group at Princeton and Columbia University. We also acknowledge the role of the summer workshop on Fragile Families data. SA is supported by the Heinz C. Prechter bipolar research fund and the Richard Tam foundation at the University of Michigan Depression Center.
References
1. Garcia-Moreno C, Jansen HA, Ellsberg M, Heise L, Watts CH. WHO multi-country study on women's health and domestic violence against women study team. Prevalence of intimate partner violence: findings from the WHO multi-country study on women's health and domestic violence. Lancet (2006) 368:1260–9. doi: 10.1016/S0140-6736(06)69523-8
2. Archer J. Sex differences in aggression between heterosexual partners. A meta-analytic review. Psychol Bull. (2000) 126:651–80. doi: 10.1037/0033-2909.126.5.651
3. Krug EG, Mercy JA, Dahlberg LL, Zwi AB. The world report on violence and health. Lancet (2002) 360:1083–8. doi: 10.1016/S0140-6736(02)11133-0
4. Basile KC, Hall JE. Intimate partner violence perpetration by court-ordered men: distinctions and intersections among physical violence, sexual violence, psychological abuse, and stalking. J Interpers Violence (2011) 26:230–53. doi: 10.1177/0886260510362896
5. Black MC. Intimate partner violence and adverse health consequences: implications for clinicians. Am J Lifestyle Med. (2011) 5:428–39. doi: 10.1177/1559827611410265
6. Black MC, Basile KC, Breiding MJ, Smith SG, Walters ML, Merrick MT, et al. The National Intimate Partner and Sexual Violence Survey (NISVS): 2010 Summary Report. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention (2011).
7. Coker AL, Davis KE, Arias I, Desai S, Sanderson M, Brandt HM, et al. Physical and mental health effects of intimate partner violence for men and women. Am J Prev Med. (2002) 23:260–8. doi: 10.1016/S0749-3797(02)00514-7
8. Leung TW, Leung WC, Ng EH, Ho PC. Quality of life of victims of intimate partner violence. Int J Gynaecol Obstet. (2005) 90:258–62. doi: 10.1016/j.ijgo.2005.05.010
9. Gielen AC, McDonnell KA, Wu AW, O'Campo P, Faden R. Quality of life among women living with HIV: the importance violence, social support, and self care behaviors. Soc Sci Med. (2001) 52:315–22. doi: 10.1016/S0277-9536(00)00135-0
10. Sadler AG, Booth BM, Nielson D, Doebbeling BN. Health-related consequences of physical and sexual violence: women in the military. Obstet Gynecol. (2000) 96:473–80. doi: 10.1097/00006250-200009000-00027
11. Mohammadkhani P, Khooshabi KS, Forouzan AS, Azadmehr H, Assari S, Lankarani MM. Associations between coerced anal sex and psychopathology, marital distress and non-sexual violence. J Sex Med. (2009) 6:1938–46. doi: 10.1111/j.1743-6109.2009.01273.x
12. Mohammadkhani P, Forouzan AS, Khooshabi KS, Assari S, Lankarani MM. Are the predictors of sexual violence the same as those of nonsexual violence? A gender analysis. J Sex Med. (2009) 6:2215–23. doi: 10.1111/j.1743-6109.2009.01338.x
13. Gleason WJ. Mental disorders in battered women: an empirical study. Violence Victims (1993) 8:53–68.
14. Preiser B, Assari S. Psychological predictors of sexual intimate partner violence against black and hispanic women. Behav Sci. (2017) 8:E3. doi: 10.3390/bs8010003
15. Cronholm PF. Intimate partner violence and men's health. Prim Care (2006) 33:199–209. doi: 10.1016/j.pop.2005.11.005
16. European Commission. Special Eurobarometer 344 Domestic Violence Against Women. Brussels: European Commission (2010).
17. Duke MR, Cunradi CB. Measuring intimate partner violence among male and female farmworkers in San Diego County, CA. Cultur Divers Ethnic Minor Psychol. (2011) 17:59–67. doi: 10.1037/a0021826
18. Bachman R, Saltzman LE. Violence Against Women: Estimates from the Redesigned Survey. US Department of Justice Statistical Clearinghouse (1995).
19. Kessler RC, Molnar BE, Feurer ID, Appelbaum M. Patterns and mental health predictors of domestic violence in the United States. Results from the National Comorbidity Survey. Int. J. Law Psychiatry (2001) 24:487–508. doi: 10.1016/S0160-2527(01)00080-2
20. O'Leary KD, Tintle N, Bromet EJ, Gluzman SF. Descriptive epidemiology of intimate partner aggression in Ukraine. Soc Psychiatry Psychiatr Epidemiolol. (2008) 43:619–26. doi: 10.1007/s00127-008-0339-8
21. Dahlberg LL, Krug EG. Violence-a global public health problem. In: Krug E, Dahlberg LL, Mercy JA, Zwi AB, Lozano R, editors. World Report on Violence and Health. World Health Organization (2002), p. 1–56.
22. Foran HM, O'Leary KD. Alcohol and intimate partner violence: a meta-analytic review. Clin Psychol Rev. (2008) 28:1222–34. doi: 10.1016/j.cpr.2008.05.001
23. Lipsky S, Caetano R, Field CA, Bazargan S. The role of alcohol use and depression in intimate partner violence among black and Hispanic patients in an urban emergency department. Am J Drug Alcohol Abuse (2005) 31:225–42. doi: 10.1081/ADA-47923
24. Lipsky S, Caetano R, Field CA, Larkin GL. Psychosocial and substance-use risk factors for intimate partner violence. Drug Alcohol Depend. (2005) 78:39–47. doi: 10.1016/j.drugalcdep.2004.08.028
25. Ansara DL, Hindin MJ. Perpetration of intimate partner aggression by men and women in the Philippines: prevalence and associated factors. J Interpers Violence (2009) 24:1579–90. doi: 10.1177/0886260508323660
26. Zaleski M, Pinsky I, Laranjeira R, Ramisetty-Mikler S, Caetano R. Intimate partner violence and alcohol consumption. Rev Saude Publica (2010) 44:53–9. doi: 10.1590/S0034-89102010000100006
27. Atkinson A, Anderson Z, Hughes K, Bellis MA, Sumnall H, Syed Q. Interpersonal Violence Illicit Drugs. Available online at: http://www.who.int/violenceprevention/interpersonal_violence_and_illicit_drug_use.pdf (2009).
28. Reichman N, Teitler J, Garfinkel I, McLanahan S. Fragile families: sample and design. Child Youth Serv Rev. (2001) 32:303–26. doi: 10.1016/S0190-7409(01)00141-4
29. Straus MA. Measuring intrafamily conflict and violence: the Conflict Tactics (CS) Scale. J Marriage Fam. (1979) 41:75–88. doi: 10.2307/351733
30. Straus MA, Hamby SL, Boney-McCoy S, Sugarman DB. The revised Conflict Tactics Scale (CTS2): development and preliminary psychometric data. J Fam Issues (1996) 17:283–316. doi: 10.1177/019251396017003001
31. Kelly J, Johnson M. Differentiation among types of intimate partner violence: research update & implications for interventions. Fam Court Rev. (2008) 46:476–99. doi: 10.1111/j.1744-1617.2008.00215.x
32. Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equat Model. (1999) 6:1–55. doi: 10.1080/10705519909540118
33. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 3rd ed. Washington, DC: American Psychiatric Association (1994).
34. Singh-Manoux A, Martikainen P, Ferrie J, Zins M, Marmot M, Goldberg M. What does self rated health measure? Results from the British Whitehall II and French Gazel cohort studies. J Epidemiol Community Health (2006) 60:364–72. doi: 10.1136/jech.2005.039883
35. IOM. State of the USA Health Indicators: Letter Report. (2009). Available online at: http://www.nationalacademies.org/hmd/Activities/Research/USHealthIndicators.aspx
36. Assari S. Synergistic effects of depression and poor impulse control on physical partner violence; a national longitudinal study in United States. Int J Epidemiol Res. (2017) 4:232–9. doi: 10.15171/ijer.2017.09
37. Fine CG. The cognitive sequelae of incest. In: Kluft RP editor. Incest-Related Syndromes of Adult Psychopathology. Washington DC: American Psychiatric Press (1990). p. 161–82.
38. Kang H. The prevention and handling of the missing data. Kor J Anesthesiol. (2013) 64:402–6. doi: 10.4097/kjae.2013.64.5.402
39. Kumar S, Quinn SC, Kim KH, Musa D, Hilyard KM, Freimuth VS. The social ecological model as a framework for determinants of 2009 H1N1 influenza vaccine uptake in the United States. Health Educ Behav. (2012) 39:229–43. doi: 10.1177/1090198111415105
40. Herman JL, Perry JC. Van der Kolk BA. Childhood trauma in borderline personality disorder. Am J Psychiatry (1989) 146:490–5. doi: 10.1176/ajp.146.4.490
41. Humphreys J, Parker B, Campbell J. Intimate partner violence against women. Annu Rev Nursing Res. (2001) 19:275–306.
42. Bronfenbrenner U. Ecological systems theory. In: R. Vasta, editor. Annals of Child Development, Vol. 6. London: Jessica Kingsley Publishers (1989), p. 187–249.
43. Landecker H. The role of childhood sexual trauma in the etiology of borderline personality disorder: considerations for diagnosis and treatment. Psychotherapy (1992) 29:234. doi: 10.1037/0033-3204.29.2.234
44. Bronfenbrenner U, Friedman SL, Wachs TD, (ed.). Measuring Environment Across the Life Span: Emerging Methods and Concepts. Washington, DC: American Psychological Association Press (1999).
45. Stuart GL, Moore TM, Gordon KC, Ramsey SE, Kahler CW. Psychopathology in women arrested for domestic violence. J Interpers Violence (2006) 21:376–89. doi: 10.1177/0886260505282888
46. Stuart GL, Meehan JC, Moore TM, Morean M, Hellmuth J, Follansbee K. Examining a conceptual framework of intimate partner violence in men and women arrested for domestic violence. J Studies Alcohol (2006) 67:102–12. doi: 10.15288/jsa.2006.67.102
47. Bennett L, Williams OJ. Substance abuse and men who batter: Issues in theory and practice. Violence Against Women (2003) 5:558–75. doi: 10.1177/1077801202250453
48. Keller PS, El-Sheikh M, Keiley M, Liao PJ. Longitudinal relations between marital aggression and alcohol problems. Psychol Addict Behav. (2009) 23:2–13. doi: 10.1037/a0013459
49. Dutton MA, Green BL, Kaltman SI, Roesch DM, Zeffiro TA, Krause ED. Intimate partner violence, PTSD, and adverse health outcomes. J Interpers Violence (2006) 21:955–68. doi: 10.1177/0886260506289178
50. Gondolf EW. A comparison of four batterer intervention systems do court referral, program length, and services matter? J Interpers Violence (1999) 14:41–61. doi: 10.1177/088626099014001003
51. Holtzworth-Munroe A, Stuart GL. Typologies of male batterers: three subtypes and the differences among them. Psychol Bull. (1994) 116:476.
52. Hamberger LK, Lohr JM, Bonge D, Tolin DF. A large sample empirical typology of male spouse abusers and its relationship to dimensions of abuse. Violence Victims (1996) 11:277–92.
53. Holtzworth-Munroe A, Meehan JC, Herron K, Rehman U, Stuart GL. Testing the Holtzworth-Munroe and Stuart (1994) batterer typology. J Consult Clin Psychol. (2000) 68:1000. doi: 10.1037/0022-006X.68.6.1000
54. Klostermann K, Kelley ML, Mignone T, Pusateri L, Fals-Stewart W. Partner violence and substance abuse: treatment interventions. Aggress Violent Behav. (2010) 15:162–6. doi: 10.1016/j.avb.2009.10.002
55. Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav. (1997) 38:21–37.
56. Connelly CD, Hazen, AL, Baker-Ericzén MJ, Landsverk J, Horwitz SM. Is screening for depression in the perinatal period enough? The co-occurrence of depression, substance abuse, and intimate partner violence in culturally diverse pregnant women. J Women's Health (2013) 22:844–52. doi: 10.1089/jwh.2012.4121
57. Caetano R, McGrath C, Ramisetty-Mikler S, Field CA. Drinking, alcohol problems and the five-year recurrence and incidence of male to female and female to male partner violence. Alcohol Clin Exp Res. (2005) 29:98–106. doi: 10.1097/01.ALC.0000150015.84381.63
58. Moore TM, Stuart GL, Meehan JC, Rhatigan DL, Hellmuth JC, Keen SM. Drug abuse and aggression between intimate partners: a meta-analytic review. Clin Psychol Rev. (2008) 28:247–74. doi: 10.1016/j.cpr.2007.05.003
Keywords: intimate partner violence, gender, mental health, self-rated health, socioeconomic status, substance use
Citation: Assari S and Jeremiah RD (2018) Intimate Partner Violence May Be One Mechanism by Which Male Partner Socioeconomic Status and Substance Use Affect Female Partner Health. Front. Psychiatry 9:160. doi: 10.3389/fpsyt.2018.00160
Received: 02 August 2017; Accepted: 09 April 2018;
Published: 08 May 2018.
Edited by:
Jutta Lindert, University of Applied Sciences Emden Leer, GermanyReviewed by:
Antonis A. Kousoulis, Mental Health Foundation, United KingdomStephan T. Egger, Universität Zürich, Switzerland
Copyright © 2018 Assari and Jeremiah. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shervin Assari, assari@umich.edu
 Shervin Assari
Shervin Assari Rohan D. Jeremiah
Rohan D. Jeremiah