- 1Child and Adolescent Psychiatry, Department of Psychiatry, Western Michigan University Homer Stryker M.D. School of Medicine, Kalamazoo, MI, USA
- 2Department of Psychiatry, Western Michigan University Homer Stryker M.D. School of Medicine, Kalamazoo, MI, USA
- 3Clinical Research, Department of Psychiatry, Western Michigan University Homer Stryker M.D. School of Medicine, Kalamazoo, MI, USA
Attention-deficit hyperactivity disorder (ADHD) is a common neurodevelopmental disorder that affects the child and adolescent population. It is characterized by impairment in attention/concentration, hyperactivity, and impulsivity, all of which can impact performance of athletes. ADHD treatment within the athletic population is a unique challenge. The research in this field has been relatively limited. The National Collegiate Athletic Association and International Olympic Committee both regulate the use of psychostimulants for treatment of ADHD due to their performance-enhancing effects. In this article, authors have discussed the screening methods, pharmacological treatment, side effects, and behavioral approaches for the treatment of ADHD in adolescent athletes.
Introduction
Attention-deficit hyperactivity disorder (ADHD) is a neurodevelopmental disorder that affects about 6–7% of the child and adolescent population (1). Reports suggest that the prevalence of this disorder is higher in athletes at both the collegiate and professional levels. Overall, ADHD is more prevalent in boys (13.2%) than in girls (5.6%), which may explain the above-mentioned discrepancy (2, 3). Literature is limited on how ADHD affects adolescents during sports-related activities. As a result, there is a paucity of literature on the treatment and management of athletes dealing with this disorder. Due to increasing awareness, researchers have started looking closely at the deleterious effects of ADHD in adolescent and adult athletes.
Search Strategies
For this article, we searched the following databases for the period of January 1985, to December 2013: Medline, PsychINFO, Ovid, PubMed, and Cochrane Library. We used the following search terms: “ADHD,” “adolescents,” “athletes,” and “sports.” Key articles were selected on the basis of topic covered, and emphasis was placed on articles published after 2000. Reference sections of identified publications were also searched for relevant information. The current article is supplemented with the authors’ clinical knowledge, and the references list was modified on the basis of suggestions from peer reviewers.
Attention-Deficit Hyperactivity Disorder
Descriptions of ADHD in the literature go back to the beginning of the twentieth century. This disorder was further conceptualized and refined at the time that the Diagnostic and Statistical Manual of Mental Disorders-III (DSM-III) was introduced. ADHD is a chronic disorder that affects multiple areas of life including education, work, family, and social functioning. If left untreated, ADHD can have long-lasting detrimental effects on the individual’s development and psychosocial functioning.
Signs and Symptoms
The Diagnostic and Statistical Manual of Mental Disorders-IV-TR identifies inattention, hyperactivity, and impulsivity as the three cardinal symptoms of this disorder (4). DSM-IV-TR also requires onset of these symptoms to be before 7 years of age. Inattentive symptoms include paying poor attention to detail, difficulty sustaining attention, poor follow-through on instructions, poor organization, avoiding homework, losing things, being distractible, and being forgetful. Hyperactivity symptoms include difficulty sitting still, inappropriately leaving one’s seat, fidgeting, running, climbing, being unusually active, and talking excessively. Impulsive behaviors usually present as an individual’s inability to wait for his turn in activities or blurting out answers before being called on in class. Children with a predominance of hyperactive and impulsive behaviors tend to present to clinical care earlier than the ones dealing primarily with inattention (5). Literature has also shown that a significant majority of children continue to deal with this disorder in their late adolescent years and that they do not “outgrow” ADHD (6). This disorder also is associated with significant comorbidity, including mood, anxiety, and oppositional disorders, which further complicates the presentation and treatment (7).
The Diagnostic and Statistical Manual of Mental Disorders-5 continues to include the inattention group criteria as well as the hyperactivity and impulsivity criteria. According to the DSM-5, ADHD symptoms must be present prior to the age of 12 years, in contrast to the age of 7 years as required in the DSM-IV. DSM-5 does not exclude children with autism spectrum disorder (8). ADHD symptoms must not occur during the course of other mental disorders such as schizophrenia, bipolar disorder, anxiety disorder, dissociative identity disorder, personality disorder, and substance intoxication or withdrawal. Such changes to the DSM-5 ensure that children with ADHD continue to receive care throughout their lives as needed.
Diagnosis of ADHD
In the majority of cases, a thorough clinical interview is sufficient to clearly establish this diagnosis. DSM-5 requires certain criteria to be met before the diagnosis is finalized, including onset of the symptoms before 12 years of age, presence of symptoms in more than one setting, and psychosocial dysfunction (8).
Certain tests can be reviewed to further clarify the diagnosis, including the Continuous Performance Test as well as the Connors and the Vanderbilt parent and teacher rating scales. It is important to remember that none of these tests are diagnostic, but they can be used as supporting evidence, especially when the clinical history is equivocal and insufficient by itself to make the diagnosis. On occasion, thorough neuropsychological testing is also warranted. A complete physical examination and laboratory testing are necessary to rule out any medical problems that may be mimicking ADHD symptoms (9).
Psychosocial Development of ADHD Adolescents
The adolescent years are marked by rapid psychosocial development with an emphasis on successfully forming an individual identity. During this stage, adolescents face numerous challenges and tend to focus mostly on themselves and their present circumstances. They struggle to improve their self-esteem, which is largely dependent upon their physical attractiveness to others and the role they play in their peer group (10). Adolescents who are successful in this stage grow to be confident and self-assured and go on to find a role in life in which they feel comfortable. Friends and peers tend to play a significant role during this phase of life, and learning to be a part of the team is an important developmental task (11).
Some children with ADHD struggle with these challenges of normal development. Their abilities to deal with the world are somewhat limited in comparison to their non-ADHD peers (12). They grow up having to deal with inattention, disorganization, and limited ability to follow through on instructions. These deficiencies are more pronounced if the ADHD remains undiagnosed and, as a result, untreated. Children with ADHD tend to get more negative feedback from their parents and teachers (13, 14). This in turn affects their self-esteem and negatively impacts their drive to achieve certain goals in life (15). They often feel criticized, yet know that they have limited control over their symptoms (16, 17). Research also has suggested that children with ADHD who feel less able to control their behaviors tend to experience more persistence of these behaviors (18–20).
ADHD Adolescents and Sports
Participation in sports is an important part of school and college life. This participation requires individuals to be attentive, organized, and calm and also to have the ability to wait for their turn. These abilities are naturally lacking in children with attention-deficit ADHD. Adolescents with ADHD also tend to struggle with impaired motor coordination, anticipation, and planning (21).
Despite these challenges, adolescents are encouraged to participate in sports, as it is widely accepted that this participation improves on-task behaviors, self-confidence, and social status within the peer group. In one study, authors examined the effects of outdoor activities on ADHD symptoms and concluded that activities in “green” outdoor spaces appear to improve ADHD symptoms the most (22). In another study, a regular exercise program for 5 out of 7 days over 6 weeks significantly improved ADHD-related behaviors in young children and adolescents (23). Other authors have found improved academic performance and overall attitude in children with a regular schedule of physical activity (24). A more recent study examining parental perceptions of the effects of regular physical activity on ADHD showed a positive impact on symptoms, with a greater benefit for symptoms of inattention and hyperactivity compared to symptoms of impulsivity (25).
Adolescents with a hyperactivity disorder report being shy and lonely and are unsure about themselves in a variety of different situations. Social skills training is one of the types of therapy that is used in the treatment of ADHD. Basic techniques in this type of therapy include role playing, modeling, and coaching (26). As with social skills training, participation in sports improves social deficits and also elevates mood and motivation level (27). Adolescents learn social cues and how to trust peers, adhere to rules, and effectively participate in structured activities. This also leads to improved relationships with peers which ultimately improves self-esteem. Participation in sports also affects the neurochemical signals in the brain. Regular exercise increases levels of dopamine and norepinephrine, two vital neurotransmitters that are deficient in individuals with ADHD (28). Elevated levels improve the ability to stay on-task and reduce impulsive behaviors. Regular exercise and other structured activities lead to improved communication between neurons and further neurogenesis (29). Brain-derived neurotrophic factor (BDNF) is the most abundant neurotrophin in the brain (30). BDNF promotes normal brain development, enhances learning and improves neuronal plasticity (31). Reductions in hippocampal BDNF levels are known to impair memory and learning in laboratory animals (32). Exercise is shown to markedly increase levels of BDNF expression in ADHD rat models (33, 34). Exercise has shown improvements in functional, regional, and bio-marker deficits and in hypothalamic pituitary adrenal disruptions (35).
Management of ADHD
Treatment of ADHD depends upon multiple factors, including the extent of dysfunction in the home, school, or workplace. The age and gender of the individual and the severity of the symptoms also play major roles in the treatment decision-making process. Both medication- and non-medication-related treatments are available, with multiple studies suggesting superior results with medication management. In reality, most adolescents with ADHD require a combination of medication management, academic support with individualized education or 504 plans, and behavioral therapies. Parent training and parent-child interaction therapy are other associated therapies that are available (36).
Stimulant medications for the treatment of ADHD
Stimulant medications are usually the first line of treatment for ADHD and are relatively safe (37). These medications have proven efficacy in treating the core symptoms of ADHD, including inattentive, hyperactive, and impulsive behaviors, and numerous studies over the last three decades have validated the safety and effectiveness of these medications (38–43).
Broadly, these medications can be divided into methylphenidate and amphetamine compounds. These compounds enhance activity in both the dopaminergic and noradrenergic systems (44) and thereby improve attention and concentration (45). By affecting dopamine, these medications also have the tendency to increase the heart rate and blood pressure, which is a consideration when prescribing these medications to athletes with ADHD (46). Other noted side effects include abdominal pain, headache, anorexia, sleep impairment, growth problems, weight loss, jitteriness, and constipation (47).
Stimulants medications have profound effects on individuals with and without ADHD and as a result, can be abused in a variety of settings. In non-ADHD adolescents, stimulants improve on-task behaviors, improve concentration, increase the ability to learn more information in limited time, minimize fatigue, and improve the performance level (48–50).
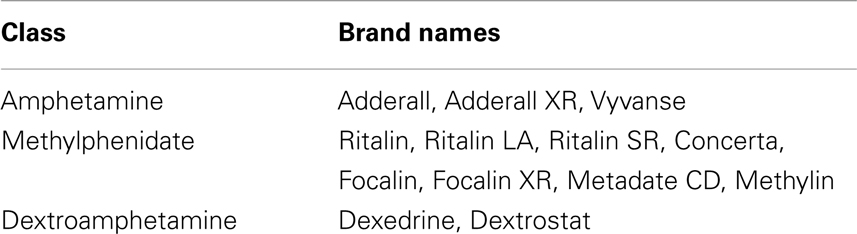
Table 1 is a simplified list of the available stimulant medications and the groups to which they belong.
Other medications sometimes used to treat ADHD include atomoxetine, guanfacine, clonidine, bupropion, and the tricyclic antidepressants. These belong to the category of non-stimulant drugs and can be a good alternative in case of concerning side effects from stimulant medications (51).
Stimulant medications and effects on athletes
As mentioned above, ADHD causes numerous limitations in the performance ability of adolescent athletes. Limited research is available on the role and effects of stimulant medications in this unique population, but certain reports have suggested that the side effect profile is somewhat different in this population in comparison to non-athletic ADHD adolescents. In one survey, athletes reported lack of creativity, lack of spontaneity, palpitations, sweating, and irritability (52). Overall, it has been noticed that the treated ADHD adolescent athletes have better participation and outcome in sports as compared to their non-treated peers. Stimulants also help them achieve the level of concentration that is necessary for adequate class participation (53).
As stimulants improve concentration and boost performance, some professional athletes in competitive sports consider them beneficial and sometimes use them to gain an advantage over others (54). There is a varied literature about the effects of stimulants on non-ADHD athletes’ sports performance. Research has suggested that these medications do not specifically improve athletic performance but instead improve the perception that one is doing well (55). Other studies that have reviewed the effects of these medications on sports have noted improved performance through increased attention to task, improved balance, and enhanced acceleration (56, 57). In a study of college students, amphetamines improved measures of acceleration, although speed and power were not consistently increased (58). Studies have also shown that athletes taking stimulants can exercise at higher core temperatures and heart rates without a perception of increased effort or stress (59, 60). One downside of using stimulants is therefore a potentially increased risk of developing heat-related illness during exercise. On the other hand, the untreated condition of ADHD may offer certain advantages also; for example, impulsivity may translate to spontaneity and quick decision-making.
It is because of the sense of euphoria, perception of slight improvement in certain aspects of performance, and improved concentration that these medications are considered to be performance enhancing and are strictly regulated by the National Collegiate Athletic Association (NCAA) and International Olympic Committee (IOC). The NCAA updated their drug testing medical exception procedures in 2008 and now requires more stringent documentation for ADHD diagnosed athletes. It allows for stimulant use by athletes with adequate documentation of ADHD diagnosis and evidence of continued follow up (53, 61). The drug may be present at the time of competition.
In 1992, the IOC introduced the therapeutic use exemption (TUE). Stimulant use by Olympic athletes for ADHD and narcolepsy has been approved recently under the TUE. Stringent rules apply and approval by two independent consultants is required.
Athletes on continued stimulant use must obtain a TUE from the World Anti-Doping Agency (WADA) prior to competing internationally (62). Athletes maintained on continued therapy must undergo annual review. In the case of a well-documented, long-standing diagnosis, a TUE can be granted for up to 4 years; however, yearly reviews by an experienced clinician are still recommended (63).
The true prevalence of ADHD in athletes is not known, as among the athletes who have this condition, few are open about it. Despite the risks, a few athletes have come forward and discussed their condition openly: Michael Phelps, the multiple Olympic gold medalist, was diagnosed with ADHD at 9 years of age; Terry Bradshaw is a pro football Hall-of-Famer who quarterbacked the Pittsburgh Steelers to four Super Bowl victories in the 1970s; Pete Rose became a World Series MVP in 1975; Cammi Granato scored more goals than any other player in the history of U.S. women’s hockey and led her team to a gold medal at the 1998 Winter Olympics in Nagano, Japan. These are just a few examples of the many professional athletes who have excelled despite their disabilities related to ADHD (64).
Stimulant medications and cardiac effects
As noted above, stimulant medications have the tendency to increase heart rate and blood pressure (65). Exercise itself has varied effects on the cardiovascular system. During exercise, there is an increased demand for oxygen by other parts of the body, including the brain and muscles. This leads to an increased workload on the heart and a resulting increase in heart rate to meet the demands of the body.
During the last few years, concerns have been raised about the effects of stimulant medications on the cardiovascular system. In 2005, Health Canada suspended the sale of Adderall XR following reports of sudden deaths in children taking this medication. The U.S. Food and Drug Administration (FDA) later issued a warning about the use of these medications in children with pre-existing heart disease. The effects of stimulants on the heart and their association with sudden cardiac death are still being debated, but in 2008, the American Heart Association (AHA) published monitoring guidelines that are currently being followed by most physicians (66).
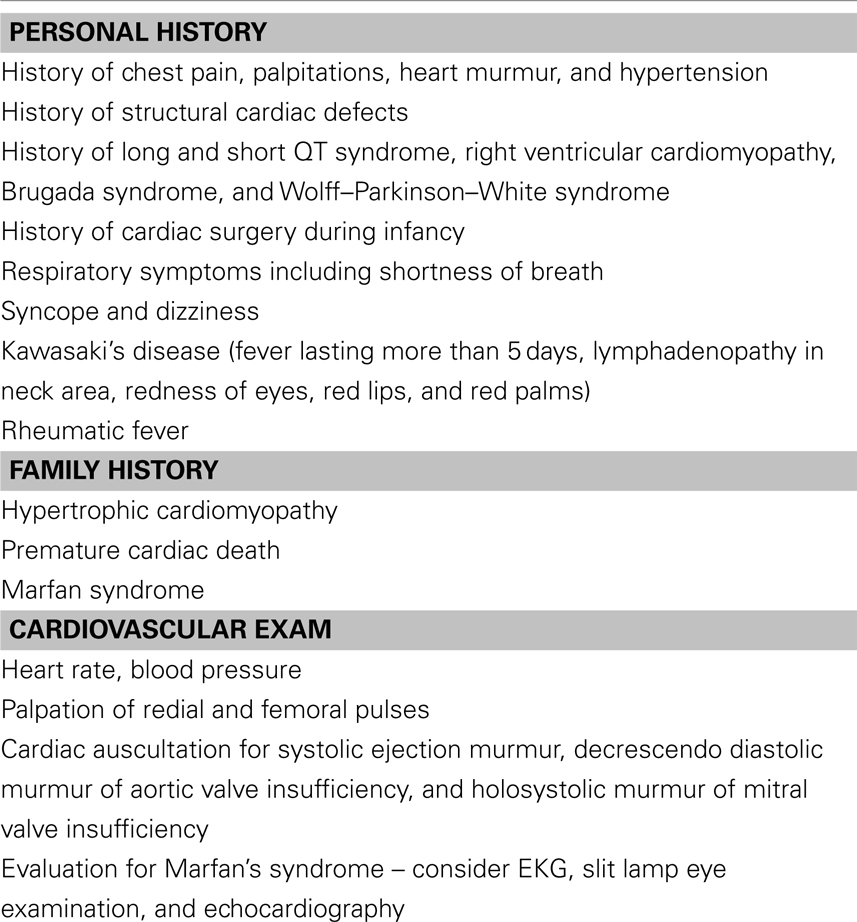
For varied reasons, the use of stimulant medications in athletes has been an area of concern. It is known that ADHD diagnosed athletes can benefit from these medications, but because of the above-mentioned concerns, a thorough cardiac evaluation needs to be done before the start of medications and before participation in sports (67, 68). Table 2 is a template for an adequate cardiovascular screening before the start of stimulant medications.
Non-stimulant medications for the treatment of ADHD (69)
Atomoxetine (Strattera). Atomoxetine is a non-stimulant medication that is approved by the FDA for the treatment of ADHD in children. It can be an alternative medication in competitive sports where stimulants are completely banned despite the clinical necessity. Strattera’s side effect profile does not increase the chance of cardiac problems. On the other hand, in 2005, the FDA issued a boxed warning for this drug because of reports of increased suicidality in individuals taking this medication (70). Atomoxetine has also been associated with elevated serum aminotransferase levels (>20 times of normal limit) and acute liver injury in a small percentage (<0.5%) of individuals. The onset of injury was between 3 and 12 weeks of the start of medication. Although most cases were self-limited, a few progressed to acute hepatic failure, requiring liver transplantation (71, 72).
Alpha-2 agonists. Clonidine and guanfacine are two other alternatives to stimulants for the treatment of ADHD. Clonidine is the more sedating of the two, but both can cause this undesirable side effect for athletes. Cardiovascular parameters including blood pressure, heart rate, and EKG need to be evaluated before the start of these medications (73). These medications are also available in extended-release (ER) preparations under the brand names Intuniv (long-acting guanfacine) and Kapvay (long-acting clonidine) (74, 75).
Behavioral treatment strategies for ADHD athletes
For one reason or an other, neither stimulant nor non-stimulant medications may be the initial choice for adolescent athletes. This is especially true for adolescents with aspirations to compete on the national or international level. In these individuals, implementation of a dedicated behavioral program can help to improve mental capabilities and to overcome ADHD symptoms, namely inattention and impulsivity (76). Problem focused therapies including social skills training, self-control, the stop and think technique, and using positive reinforcements while being consistent and maintaining clear expectations about behaviors are some of the proven strategies (77). The home environment plays a major role in the expression of symptoms of ADHD (78). Homes which provide stability, security, calmness, and structure enable children with ADHD to perform at their best capacity (79).
Mild brain stimulation techniques and neurofeedback (NF) improve brain wave imbalances, facilitating a calmer mental state and therefore better communication throughout the brain (80). NF, which uses signals from the brain’s electrical activity as feedback, has been studied in the last few years for treatment of children with ADHD. In one study, NF was shown to improve the performance of expert rifle shooters (81). Studies have shown that over time, brain stimulation techniques can improve brain development through neuroplasticity. NF is a valid option for treatment, but further studies are needed to determine guidelines for use (80, 82).
Conclusion
Attention-deficit hyperactivity disorder is a common disorder that affects millions of children all over the world. These children suffer from inattention, hyperactivity, impulsivity, poor self-esteem, and academic and social problems. Because of these symptoms and deficits in motor control, their performance in sports is also impaired (83). Stimulant medications have an extensive literature supporting their safety and effectiveness in the treatment of ADHD. By improving the core symptoms, these medications improve the overall functioning of ADHD adolescents. Recently raised concerns about cardiac problems are debatable (84, 85), but a thorough evaluation by the physician is usually an adequate safeguard against any unwanted side effects. Research is equivocal on whether these medications provide an extra benefit to pro-level athletes. Overall, adequate treatment of ADHD improves the adolescent’s quality of life (86).
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Boyle CA, Boulet S, Schieve LA, Cohen RA, Blumberg SJ, Yeargin-Allsopp M, et al. Trends in the prevalence of developmental disabilities in US children, 1997–2008. Pediatrics (2011) 127:1034–42. doi: 10.1542/peds.2010-2989
2. Kaufman KR, Bajaj A, Schiltz JF. Attention-deficit/hyperactivity disorder (ADHD) in gymnastics: preliminary findings. Apunts Med de l’Esport (2011) 46:89–95. doi:10.1016/j.apunts.2011.01.002
3. Sauver JLS, Barbaresi WJ, Katusic SK, Colligan RC, Weaver AL, Jacobsen SJ. Early life risk factors for attention-deficit/hyperactivity disorder: a population-based cohort study. Mayo Clin Proc (2004) 79:1124–31. doi:10.1016/S0025-6196(11)62594-9
4. Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR). 4th ed. Washington, DC: American Psychiatric Publishing (2000).
5. Biederman J, Mick E, Faraone SV, Braaten E, Doyle A, Spencer T, et al. Influence of gender on attention deficit hyperactivity disorder in children referred to a psychiatric clinic. Am J Psychiatry (2002) 159:36–42. doi:10.1176/appi.ajp.159.1.36
6. Patukian M, Kreher JB, Coppel DB, Glazer JL, McKeag DB, White RD. Attention deficit hyperactivity disorder and the athlete: an American Medical Society for Sports Medicine Position Statement. Clin J Sport Med (2011) 5:392–401. doi:10.1097/JSM.0b013e3182262eb1
7. Kouichi Y, Barbaresi WJ, Colligan RC, Voigt RG, Killian JM, Weaver AL, et al. Childhood ADHD is strongly associated with a broad range of psychiatric disorders during adolescence: a population-based birth cohort study. J Child Psychol Psychiatry (2012) 10:1036–43. doi:10.1111/j.1469-7610.2012.02567.x
8. Diagnostic and Statistical Manual of Mental Disorders-5th ed. (DSM-5). Washington, DC: American Psychiatric Publishing (2013).
9. Pliszka S. AACAP Work Group on Quality Issues. Practice parameter for the assessment and treatment of children and adolescents with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry (2007) 46(7):894–921. doi:10.1097/chi.0b013e318054e724
10. Bagwell CL, Molina BS, Pelham WE. ADHD and problems in peer relations: predictions from childhood to adolescence. J Am Acad Child Adolesc Psychiatry (2001) 40:1285–92. doi:10.1097/00004583-200111000-00008
11. Chronis AM, Heather AJ, Veronica LR. Evidence-based psychosocial treatments for children and adolescents with attention-deficit/hyperactivity disorder. Clin Psychol Rev (2006) 26(4):486–502. doi:10.1016/j.cpr.2006.01.002
12. DuPaul GJ, McGoey KE, Eckert TL. Preschool children with attention deficit/hyperactivity disorder: impairments in behavioural, social, and school functioning. J Am Acad Child Adolesc Psychiatry (2001) 40:508–15. doi:10.1097/00004583-200105000-00009
13. Johnston C, Mash EJ. Families of children with ADHD: review and recommendations for future research. Clin Child Fam Psychol Rev (2001) 4:183–207. doi:10.1023/A:1017592030434
14. Podolski CL, Nigg JT. Parent stress and coping in relation to child ADHD severity and associated child disruptive behaviour problems. J Clin Child Psychol (2001) 30:503–13. doi:10.1207/S15374424JCCP3004_07
15. Frame K, Kelly L, Bayley E. Increasing perceptions of self-worth in preadolescents diagnosed with ADHD. J Nurs Scholarsh (2003) 35:225–9. doi:10.1111/j.1547-5069.2003.00225.x
17. Harpin VA. The effect of ADHD on the life of an individual, their family, and community from preschool to adult life. Arch Dis Child (2005) 90(Suppl 1):i2–7. doi:10.1136/adc.2004.059006
18. Muraven M, Baumeister RF. Self-regulation and depletion of limited resources: does self-control resemble a muscle? Psychol Bull (2000) 126(2):247–59. doi:10.1037/0033-2909.126.2.247
19. Barkley RA. Behavioral inhibition, sustained attention, and executive functions: constructing a unifying theory of ADHD. Psychol Bull (1997) 121:65–94. doi:10.1037/0033-2909.121.1.65
20. Loge DV, Staton RD, Beatty W. Performance of children with ADHD on tests sensitive to frontal lobe dysfunction. J Am Acad Child Adolesc Psychiatry (1989) 29:540–5. doi:10.1097/00004583-199007000-00006
21. Hickey G, Fricker P. Attention deficit hyperactivity disorder, CNS stimulants and sport. Sports Med (1999) 27(1):11–21. doi:10.2165/00007256-199927010-00002
22. Kuo FE, Taylor AF. A potential natural treatment for attention-deficit/hyperactivity disorder: evidence from a national study. Am J Public Health (2004) 94(9):1580–6. doi:10.2105/AJPH.94.9.1580
23. Archer T, Kostrzewa RM. Physical exercise alleviates ADHD symptoms: regional deficits and development trajectory. Neurotox Res (2012) 21(2):195–209. doi:10.1007/s12640-011-9260-0
24. Halperin JM, Healey DM. The influences of environmental enrichment, cognitive enhancement, and physical exercise on brain development: can we alter the developmental trajectory of ADHD? Neurosci Biobehav Rev (2011) 35(3):621–34. doi:10.1016/j.neubiorev.2010.07.006
25. Gapin JI, Etnier JL. Parental perceptions of the effects of exercise on behavior in children and adolescents with ADHD. J Sport Health Sci (2013). doi:10.1016/j.jshs.2013.03.002
26. Storebø OJ, Skoog M, Damm D, Thomsen PH, Simonsen E, Gluud C. Social skills training for Attention Deficit Hyperactivity Disorder (ADHD) in children aged 5 to 18 years. Cochrane Database Syst Rev (2011) 12:CD008223. doi:10.1002/14651858.CD008223.pub2
27. Azrin NH, Ehle CT, Beaumont AL. Physical exercise as a reinforcer to promote calmness of an ADHD child. Behav Modif (2006) 30:564–70. doi:10.1177/0145445504267952
28. Trevor A, Kostrzewa RM. Physical exercise alleviates ADHD symptoms: regional deficits and development trajectory. Neurotox Res (2012) 21(2):195–209. doi:10.1007/s12640-011-9260-0
29. Pereira AC, Huddleston DE, Brickman AM, Sosunov AA, Hen R, McKhann GM, et al. An in vivo correlate of exercise-induced neurogenesis in the adult dentate gyrus. Proc Natl Acad Sci USA (2007) 104(13):5638–43. doi:10.1073/pnas.0611721104
30. Barbacid M. Neurotrophic factors and their receptors. Curr Opin Cell Biol (1995) 7(2):148–55. doi:10.1016/0955-0674(95)80022-0
31. Thoenen H. Neurotrophins and neuronal plasticity. Science (1995) 270(5236):593–8. doi:10.1126/science.270.5236.593
32. Monteggia LM, Barrot M, Powell CM, Berton O, Galanis V, Gemelli T, et al. Essential role of brain-derived neurotrophic factor in adult hippocampal function. Proc Natl Acad Sci USA (2004) 101(29):10827–32. doi:10.1073/pnas.0402141101
33. Kristel K, Goekint M, Heyman EM, Meeusen R. Neuroplasticity-exercise-induced response of peripheral brain-derived neurotrophic factor. Sports Med (2010) 40(9):765–801. doi:10.2165/11534530-000000000-00000
34. Hong K, Heo HI, Kim DH, Ko G, Lee SS, Kim SE, et al. Treadmill exercise and methylphenidate ameliorate symptoms of attention deficit/hyperactivity disorder through enhancing dopamine synthesis and brain-derived neurotrophic factor expression in spontaneous hypertensive rats. Neurosci Lett (2011) 504:35–9. doi:10.1016/j.neulet.2011.08.052
35. Wigal SB, Nemet D, Swanson JM, Regino R, Trampush J, Ziegler MJ, et al. Catecholamine response to exercise in children with attention deficit hyperactivity disorder. Pediatr Res (2003) 53(5):756–61. doi:10.1203/01.PDR.0000061750.71168.23
36. van den Hoofdakker BJ, van der Veen-Mulders L, Sytema S, Emmelkamp PM, Minderaa RB, Nauta MH. Effectiveness of behavioral parent training for children with ADHD in routine clinical practice: a randomized controlled study. J Am Acad Child Adolesc Psychiatry (2007) 46(10):1263–71. doi:10.1097/chi.0b013e3181354bc2
37. Greydanus DE, Pratt HD, Patel DR. Attention deficit hyperactivity disorder across the lifespan: the child, adolescent, and adult. Dis Mon (2007) 53(2):70–131. doi:10.1016/j.disamonth.2007.01.001
38. Schachar R, Jadad AR, Gauld M, Boyle M, Booker L, et al. Attention-deficit hyperactivity disorder: critical appraisal of extended treatment studies. Can J Psychiatry (2002) 47(4):337–48.
39. Prasad V, Brogan E, Mulvaney C, Grainge M, Stanton W, Sayal K. How effective are drug treatments for children with ADHD at improving on-task behaviour and academic achievement in the school classroom? A systematic review and meta-analysis. Eur Child Adolesc Psychiatry (2013) 22(4):203–16. doi:10.1007/s00787-012-0346-x
40. Volkow ND. Long-term safety of stimulant use for ADHD: findings from nonhuman primates. Neuropsychopharmacology (2012) 37(12):2551–2. doi:10.1038/npp.2012.127
41. Zuvekas SH, Vitiello B. Stimulant medication use in children: a 12-year perspective. Am J Psychiatry (2012) 169:160–6. doi:10.1176/appi.ajp.2011.11030387
42. Cooper WO, Habel LA, Sox CM, Chan KA. ADHD drugs and serious cardiovascular events in children and young adults. N Engl J Med (2011) 365(20):1896–904. doi:10.1056/NEJMoa1110212
43. Graham J, Banaschewski T, Buitelaar J, Coghill D, Danckaerts M, Dittmann RW, et al. European guidelines on managing adverse effects of medication for ADHD. Eur Child Adolesc Psychiatry (2011) 20(1):17–37. doi:10.1007/s00787-010-0140-6
44. del Campo N, Chamberlain SR, Sahakian BJ, Robbins TW. The roles of dopamine and noradrenaline in the pathophysiology and treatment of attention-deficit/hyperactivity disorder. Biol Psychiatry (2011) 69(12):e145–57. doi:10.1016/j.biopsych.2011.02.036
45. Volkow ND, Fowler JS, Wang G, Ding Y, Gatley SJ. Mechanism of action of methylphenidate: insights from PET imaging studies. J Atten Disord (2001) 6:S31–43.
46. Hamilton RM, Rosenthal E, Hulpke-Wette M, Graham JG, Sergeant J. Cardiovascular considerations of attention deficit hyperactivity disorder medications: a report of the European Network on Hyperactivity Disorders work group, European Attention Deficit Hyperactivity Disorder Guidelines Group on attention deficit. Cardiol Young (2012) 22(1):63–70. doi:10.1017/S1047951111000928
47. Bezchlibnyk-Butler KZ, Jeffries JJ, Procyshyn RM. Clinical Handbook of Psychotropic Drugs. Hogrefe Publishing (2012).
48. Smith ME, Farah MJ. Are prescription stimulants smart pills? The epidemiology and cognitive neuroscience of prescription stimulant use by normal healthy individuals. Psychol Bull (2011) 137(5):717–41. doi:10.1037/a0023825
49. Swanson J, Baler RD, Volkow ND. Understanding the effects of stimulant medications on cognition in individuals with attention-deficit hyperactivity disorder: a decade of progress. Neuropsychopharmacology (2011) 36(1):207–26. doi:10.1038/npp.2010.160
50. Swanson JM, Wigal TL, Volkow ND. Contrast of medical and nonmedical use of stimulant drugs, basis for the distinction, and risk of addiction: comment on Smith and Farah (2011). Psychol Bull (2011) 5:742–8. doi:10.1037/a0024898
51. Santosh PJ, Sattar S, Canagaratnam M. Efficacy and tolerability of pharmacotherapies for attention-deficit hyperactivity disorder in adults. CNS Drugs (2011) 25(9):737–63. doi:10.2165/11593070-000000000-00000
52. Conant-Norville DO, Tofler IR. Attention deficit/hyperactivity disorder and psychopharmacologic treatments in the athlete. Clin Sports Med (2005) 24(4):829–43. doi:10.1016/j.csm.2005.05.007
53. Putukian M, Kreher JB, Coppel DB, Glazer JL, McKeag DB, White RD. Attention deficit hyperactivity disorder and the athlete: an American Medical Society for Sports Medicine position statement. Clin J Sport Med (2011) 21(5):392–400. doi:10.1097/JSM.0b013e3182262eb1
54. Veliz P, Boyd C, McCabe SE. Adolescent athletic participation and nonmedical Adderall use: an exploratory analysis of a performance-enhancing drug. J Stud Alcohol Drugs (2013) 74(5):714–9.
55. Greydanus DE, Patel DR. Sports doping in the adolescent athlete: the hope, hype, and hyperbole. Pediatr Clin North Am (2002) 49(4):829–55. doi:10.1016/S0031-3955(02)00021-4
56. Pelham WE, McBurnett K, Harper GW, Milich R, Murphy DA, Clinton J, et al. Methylphenidate and baseball playing in ADHD children: who’s on first? J Consult Clin Psychol (1990) 58:130–3. doi:10.1037/0022-006X.58.1.130
57. Wade MG. Effects of methylphenidate on motor skills acquisition of hyperactive children. J Learn Disabil (1976) 9:48–52. doi:10.1177/002221947600900711
58. Chandler JV, Blair SN. The effect of amphetamines on selected physiological components related to athletic success. Med Sci Sports Exerc (1980) 12:65–9. doi:10.1249/00005768-198021000-00013
59. Watson P, Hasegawa H, Roelands B, Piacentini MF, Looverie R, Meeusen R. Acute dopamine/noradrenaline reuptake inhibition enhances human exercise performance in warm, but not temperate conditions. J Physiol (2005) 565:873–83. doi:10.1113/jphysiol.2004.079202
60. Roelands B, Hasegawa H, Watson P. The effects of acute dopamine reuptake inhibition on performance. Med Sci Sports Exerc (2008) 40:879–85. doi:10.1249/MSS.0b013e3181659c4d
62. Medical Information to Support the Decisions of TUEC’s ADHD. Available from: http://www.wada-ama.org/Documents/Science_Medicine/Medical_info_to_support_TUECs/WADA_Medical_info_ADHD_2.0_EN.pdf
63. Fitch K. Proscribed drugs at the Olympic Games: permitted use and misuse (doping) by athletes. Clin Med (2012) 12(3):257–60. doi:10.7861/clinmedicine.12-3-257
64. Judy D. (0000). ADHD Athletes: Inspiring Sports Stars with Attention Deficit. Available from: http://www.additudemag.com/adhd/article/989.html
65. Safer DJ. Relative cardiovascular safety of psychostimulants used to treat attention-deficit hyperactivity disorder. J Child Adolesc Psychopharmacol (1992) 2(4):279–90. doi:10.1089/cap.1992.2.279
66. Vetter VL, Elia J, Erickson C. Cardiovascular monitoring of children and adolescents with heart disease receiving medications for attention deficit/hyperactivity disorder: a Scientific Statement From the American Heart Association Council on Cardiovascular Disease in the Young Congenital Cardiac Defects Committee and the Council on Cardiovascular Nursing. Circulation (2008) 117(18):2407–23. doi:10.1161/CIRCULATIONAHA.107.189473
67. Perrin JM, Friedman RA, Knilans TK, Black Box Working Group, Section on Cardiology and Cardiac Surgery. Cardiovascular monitoring and stimulant drugs for attention deficit/hyperactivity disorder. Pediatrics (2008) 122:451–3. doi:10.1542/peds.2008-1573
68. Bille K, Figueiras D, Schamasch P, Kappenberger L, Brenner JI, Meijboom FJ, et al. Sudden cardiac death in athletes: the Lausanne Recommendations. Eur J Cardiovasc Prev Rehabil (2006) 13(6):859–75. doi:10.1097/01.hjr.0000238397.50341.4a
69. Staufer WB, Greydanus DE. Attention-deficit/hyperactivity disorder psychopharmacology for college students. Pediatr Clin North Am (2005) 52(1):71–84. doi:10.1016/j.pcl.2004.10.007
70. Bushe CJ, Nicola CS. Systematic review of atomoxetine data in childhood and adolescent attention-deficit hyperactivity disorder 2009–2011: focus on clinical efficacy and safety. J Psychopharmacol (2014) 28(3):204–11. doi:10.1177/0269881113478475
71. Atomoxetine (StratteraTM) Prescribing Information. Eli Lilly and Company (2014). Available from: http://pi.lilly.com/us/strattera-pi.pdf
72. Kohn MR, Tsang TW, Clarke SD. Efficacy and safety of atomoxetine in the treatment of children and adolescents with attention deficit hyperactivity disorder. Clinical Medicine Insights. Pediatrics (2012) 6:95–162. doi:10.4137/CMPed.S7868
73. Hirota T, Schwartz S, Correll CU. Alpha-2 agonists for attention-deficit/hyperactivity disorder in youth: a systematic review and meta-analysis of monotherapy and add-on trials to stimulant therapy. J Am Acad Child Adolesc Psychiatry (2014) 53(2):153–73. doi:10.1016/j.jaac.2013.11.009
74. Cruz MP. Guanfacine extended-release tablets (Intuniv), a non-stimulant selective alpha2A-adrenergic receptor agonist for attention-deficit/hyperactivity disorder. P T (2010) 35(8):448–51.
75. Thomas C. Extended release alpha-2 agonists for ADHD. Child Adolesc Psychopharmacol News (2013) 18:7–9. doi:10.1521/capn.2013.18.2.7
76. Hodgson K, Hutchinson AD, Denson L. Nonpharmacological treatments for ADHD: a meta-analytic review. J Atten Disord (2014) 18(4):275–82. doi:10.1177/1087054712444732
77. Young S, Myanthi Amarasinghe J. Practitioner review: non-pharmacological treatments for ADHD: a lifespan approach. J Child Psychol Psychiatry (2010) 51(2):116–33. doi:10.1111/j.1469-7610.2009.02191.x
78. Mokrova I, O’Brien M, Calkins S, Keane S. Parental ADHD symptomology and ineffective parenting: the connecting link of home chaos. Parent Sci Pract (2010) 10(2):119–35. doi:10.1080/15295190903212844
79. Mulligan A, Anney R, Butler L, O’Regan M, Richardson T, Tulewicz EM, et al. Home environment: association with hyperactivity/impulsivity in children with ADHD and their non-ADHD siblings. Child Care Health Dev (2013) 39(2):202–12. doi:10.1111/j.1365-2214.2011.01345.x
80. Moriyama TS, Polanczyk G, Caye A, Banaschewski T, Brandeis D, Rohde LA. Evidence-based information on the clinical use of neurofeedback for ADHD. Neurotherapeutics (2012) 9(3):588–98. doi:10.1007/s13311-012-0136-7
81. Rostami R, Sadeghi H, Karami KA, Abadi MN, Salamati P. The effects of neurofeedback on the improvement of rifle shooters’ performance. J Neurother (2012) 16(4):264–9. doi:10.1080/10874208.2012.730388
82. Arnold LE, Lofthouse N, Hersch S, Pan X, Hurt E, Bates B, et al. EEG neurofeedback for ADHD double-blind sham-controlled randomized pilot feasibility trial. J Atten Disord (2013) 17(5):410–9. doi:10.1177/1087054712446173
83. Demers MM, McNevin N, Azar NR. ADHD and motor control: a review of the motor control deficiencies associated with attention deficit/hyperactivity disorder and current treatment options. Crit Rev Phys Rehabil Med (2013) 25:231–9. doi:10.1615/CritRevPhysRehabilMed.2013009763
84. Martinez-Raga J, Knecht C, Szerman N, Martinez MI. Risk of serious cardiovascular problems with medications for attention-deficit hyperactivity disorder. CNS Drugs (2013) 27(1):15–30. doi:10.1007/s40263-012-0019-9
85. Winterstein AG. Cardiovascular safety of stimulants in children: findings from recent population-based cohort studies. Curr Psychiatry Rep (2013) 15(8):1–5. doi:10.1007/s11920-013-0379-y
Keywords: attention-deficit hyperactivity disorder, adolescents, athletes, sports, stimulants, pharmacotherapies
Citation: Nazeer A, Mansour M and Gross KA (2014) ADHD and adolescent athletes. Front. Public Health 2:46. doi: 10.3389/fpubh.2014.00046
Received: 25 November 2013; Accepted: 02 May 2014;
Published online: 17 June 2014.
Edited by:
Udo Rolle, Goethe University Frankfurt am Main, GermanyReviewed by:
Mladen Jasic, General Hospital Pula, CroatiaDaniel Rossignol, Rossignol Medical Center, USA
Copyright: © 2014 Nazeer, Mansour and Gross. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ahsan Nazeer, Department of Psychiatry, Western Michigan University Homer Stryker M.D. School of Medicine, 1717 Shaffer Road, Suite 010, Kalamazoo, MI 49048, USA e-mail: ahsan.nazeer@med.wmich.edu
 Ahsan Nazeer
Ahsan Nazeer Miriam Mansour
Miriam Mansour Kathleen A. Gross
Kathleen A. Gross