- 1Robert Stempel College of Public Health and Social Work, Florida International University, Miami, FL, USA
- 2College of Business, Florida Atlantic University, Boca Raton, FL, USA
Introduction
Nearly a century ago, Charles-Edward Amory Winslow, defined public health as “the science and art of preventing disease, prolonging life, and promoting health and efficiency through organized community effort” (1). From health policy reforms to scientific advances with many technological innovations, a range of forces are converging to cause a seismic shift in how public health is practiced. We think that in the twenty-first century, global public health system will be completely restructured. Reliance on complex technologies like nanotechnology and artificial intelligence (AI), which were previously only used in fields like computer science and physics, will become the new trend. Using such advanced technologies would become megatrends of public health in new and exciting ways. Historically, public health, in comparison to other scientific disciplines, has been behind the curve in terms of using advanced technologies (2). This article highlights the current trends in public health in terms of use of advanced technologies like nanotechnology and AI and how they can impact the future of public health in the twenty-first century.
Nanotechnology and Public Health
What is Nanotechnology?
Nanotechnology is the science, which involves the design, synthesis and application of materials and devices, which have smallest functional organization on the nanometer scale in at least one dimension (3). According to Pautler and Brenner, “the most widely accepted definition of scale for nanotechnology is 1–100 nm” (4). For the purposes of advancing public health, there are several advantages to engineering materials on such a small scale. For example, using “nanomedicine” approaches allows researchers to apply drug therapies to human cancer cells with previously unachievable accuracy and fewer treatment related adverse effects (4). Other examples include biomedical technology that can monitor patient’s metabolic systems from inside the body, and nano-engineered bone prostheses that could be implanted with the highest achievable precision (5). Thus, the use of such complex medical technologies with individual based approaches could significantly improve population health over time with indirect advantages to public health.
Nanotechnology in Public Health
Protecting the Human Right to Clean Water
One specific use of nanotechnology, which can improve public health, is environmental nanotechnology, which can produce clean and safe drinking water for human consumption and use. In the modern world, availability of water continues to be a problem on an international level due to factors like global warming, drought, and unprecedented population growth (6). For example, nanotechnology can be used to make water-testing sensors to purify water for safe consumption (5–7). This can improve public health on a global level by reducing the numbers of people harmed or killed by health problems associated with unsanitary water (7). Furthermore, safe drinking water can help primary education in several developing countries in Africa, Asia, and Latin America, where children are often unable to attend schools due to the lack of clean water sources (7).
Reducing the Global Disease Burden
Nanotechnology could also improve public health through advanced drug administration strategies. For example, there are many cancer-fighting drugs such as Abraxane® (for breast cancer) and Doxil® (for ovarian cancer), which are “nanoenabled” and have already been approved by the Food and Drug Administration (FDA) (4). Nanotechnology is also being used to manufacture single dose regimens of hepatitis B vaccine with better penetrance and immune activation profiles compared to the currently administrated four dose regimen. This can be considered a major advance in public health because many more vaccines can be derived with single dose options thereby increasing compliance and effectiveness (4).
Safety concerns
Nanotechnology is already being used for manufacturing thousands of consumer products marketed globally. For example, nanoparticles are used in popular sunscreen brands such as Burt’s Bees® and Coppertone® (4). However, there are still questions about the long-term effects of nanotechnology on general health and environment. There are no FDA regulations within the U.S. that govern the use of such materials in consumer products. Many researchers have expressed concerns because safety controls and monitoring systems are lacking for nanotechnological products both within the U.S., and globally (5, 6, 8, 9).
Artificial Intelligence and Public Health
What is Artificial Intelligence?
Artificial intelligence, often abbreviated as “AI,” is defined as “the science and engineering of making intelligent machines, especially intelligent computer programs. It is related to the task of using computers to understand human intelligence, but AI does not have to confine itself to methods that are biologically observable” (10). Broadly speaking, AI involves the creation of “intelligent” systems capable of performing complex data analyses, which are superior to the ones performed by existing data systems without the use of AI.
Artificial Intelligence in Public Health
The use of AI for public health spans back to the 1960s, when professionals from disciplines like computer science, chemistry, and biology began using AI programs in complex medical researches (11). Several researchers convened at the conference Artificial Intelligence in Medicine in Europe (AIME) in 2007 to discuss the role of AI in modern medicine, and their opinions were collectively published in the year 2009 (11). In our opinion, AI can best serve the goals of public health only with cross-disciplinary expansions and collaborations. This entails not only the development of computer science but also incorporating advancements from fields like epidemiology, biology, genetics, modern medicine, and public health policy.
Artificial Intelligence in Disease Surveillance
According to Neill (12), public health surveillance may be defined as “the process of detecting, characterizing, tracking, and responding to disease outbreaks, other health threats (such as a bioterrorist attack, radiation leak, or contamination of the food or water supply), and other patterns relevant to the health of populations (such as obesity, drug abuse, mental health, or malnutrition).” This type of surveillance is conducted at multiple levels, ranging from local community levels all the way up to global community health settings (12, 13). It also spans across several types of public and private entities such as government agencies, healthcare clinics, hospitals, pharmacies, and health corporations (13).
National Institutes of Health in the U.S. has several ongoing studies targeting the use of AI for improving surveillance of both communicable and non-communicable diseases (13). Modern disease surveillance systems use AI to help automate the process of disease surveillance so that there is less reliance on human labor; to make the process more expedited so that real-time and predictive surveillance can occur; to allow for data to come from a much wider variety of sources than traditional systems; and to allow the results of such data to be disseminated to public health officials and the general public on a wider and faster basis (14). A new type of system has emerged specifically for using digital data to improve public health surveillance. This has been referred to as “digital surveillance” and it “attempts to provide knowledge of public health issues by analysis of health information stored digitally, and the distribution and patterns governing access to these data” (15). Data gathered from Internet sources used to feed a digital surveillance system is one such advancement. Milinovich et al. (15) offer many examples of such Internet-based health surveillance systems. These include tracking communicable and non-communicable diseases, mental health trends, illegal drug use trends, and the impact of health policies. Disease surveillance systems using AI can help in tracking health issues as they occur and predict health issues in the future. For example, one such system was able to predict a rise in U.S. flu cases approximately 1–3 weeks before they occurred and was based on Yahoo search queries for related health information variables (16). In addition to data from search engines, data from social media have also been used to feed digital surveillance systems. For example, Lee et al. (17) built a flu and cancer surveillance system, which relies on Twitter data to give real time estimates of trends such as severity of disease, progression, symptoms being experienced, and treatments being implemented.
There is significant evidence to state that Internet-based disease surveillance systems offer advantages over traditional disease surveillance systems. Traditional disease surveillance systems are typically fed by data from public health officials working in hospitals and agency settings, whereas Internet-based systems can offer more data over different, and oftentimes larger population segments (16). Systems such as “Google Flu Trends” have predicted flu outbreaks earlier than traditional disease surveillance systems. However, there are some disadvantages to these systems as well because it relies on data provided by people who have access to Internet and use it for health information. In spite of advanced web delivery options, Internet use continues to be low in many underdeveloped and developing nations. Also, there are privacy concerns over the use of data within these systems (16). While such systems may offer advancements to modern day disease surveillance, Polgreen et al. (16) argues that “they do not have the capacity to replace traditional surveillance systems and they should not be viewed as an alternative, but rather an extension” to traditional disease surveillance systems. Our opinion is that these systems should be integrated into traditional systems in the coming years.
When opining about the future of AI for disease surveillance, Neill states that this field is now experiencing a “major paradigm shift” because compared to the past, today’s surveillance systems are relying on ever increasing volumes of data and data from non-traditional sources like online news feeds and Twitter feeds (12, 15).
Other Technologies
There are several other technologies that hold promise for advancing the public health in the twenty-first century. Some of the major ones include mHealth (mobilehealth), virtual reality, biosensors for healthcare, disappearing technology, etc. mHealth is defined as, “the practice of medicine and public health, supported by mobile communication devices for health services and information” (18). mHealth and e-health are widely used in interventions for adult and pediatric obesity (18, 19). Another promising technology includes virtual reality, where a computer generated advanced interface could simulate a real word scenario and communicate the healthcare advice. For example, virtual reality enhanced cognitive behavioral therapy was more effective in weight reduction strategies when compared to other strategies like inpatient multimodal treatment and standard cognitive behavior therapy (20). The use of biosensors could revolutionize public health delivery in the twenty-first century. Micro-miniaturized sensors could be permanently implanted in biological fluids for continuous evaluations of biomedical parameters in diabetes, cancers, and cardiovascular diseases (21). Through the use of yet another modern application known as disappearing technology, public health could expand to dimensions hither to unknown. This technology uses bio/eco-resorbable chips implanted into the body. Though majority of the applications of this technology are currently limited to clinical medicine, public health prospects could be subsequently researched (22).
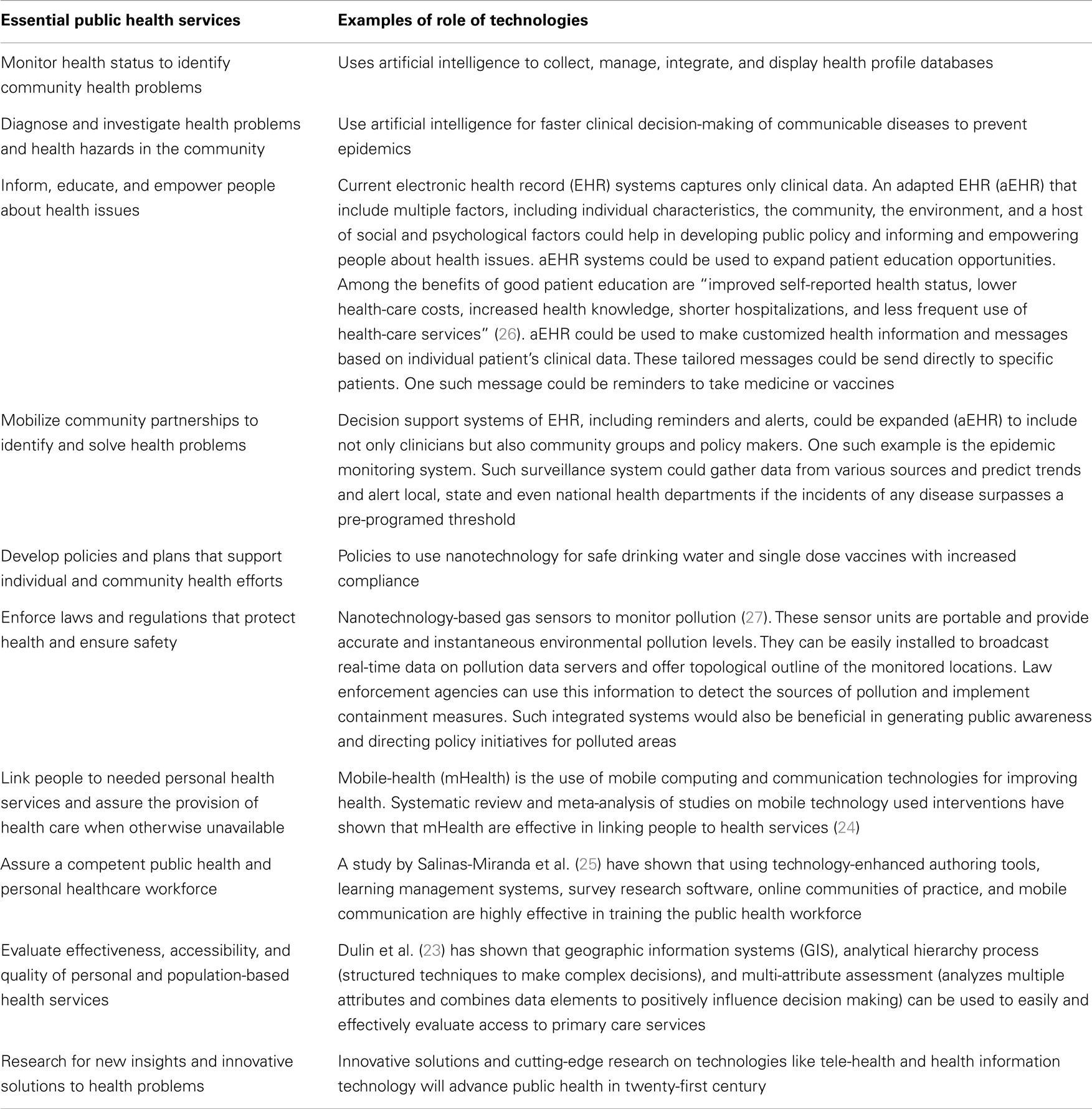
Table 1 shows how advanced technologies can impact essential public health services.
Conclusion
We think that there should be increased awareness among public health professionals and policy makers about the use of advanced technologies to improve health care and address newer health challenges. This would also lead to improved and widespread implementation of modern technologies. The continued use and advancement of such technologies cannot be isolated within the dimensions of abstract science. It should be directed toward public awareness for increased support and funding. The researchers and practitioners of these technologies rely on the public support, and therefore, these technologies should be oriented toward the public whom they intend to serve. Indeed, Currall et al. (28) have shown that public perceptions about tools, such as nanotechnology, play a vital role in how these technologies progress. They argue that “understanding public sentiment toward any new innovation is pivotal because, historically, public perceptions, and attitudes have shaped the direction and pace of scientific activity in a number of fields.” Today’s populace is very supportive for scientific and technological progress. Thus, we predict that public health will continue to advance into the twenty-first century and take full advantage of today’s popular support. It is clear that dedicated research efforts, driven by public education will establish a megatrends of highest use of technology for improved public health outcomes.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
Authors would like to thank Dr. William W. Darrow for his valuable comments and suggestions.
References
1. Winslow CE. The untilled fields of public health. Science (1920) 51(1306):23–33. doi: 10.1126/science.51.1306.23
2. Riegelman R, Persily NA. Health information systems and health communications: narrowband and broadband technologies as core public health competencies. Am J Public Health (2001) 91(8):1179–83. doi:10.2105/AJPH.91.8.1179
3. Emerich DF, Thanos CG. Nanotechnology and medicine. Expert Opin Biol Ther (2003) 3(4):655–63. doi:10.1517/14712598.3.4.655
4. Pautler M, Brenner S. Nanomedicine: promises and challenges for the future of public health. Int J Nanomedicine (2010) 5:803–9. doi:10.2147/IJN.S13816
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
6. Savage N, Diallo MS. Nanomaterials and water purification: opportunities and challenges. J Nanopart Res (2005) 7(4–5):331–42. doi:10.1007/s11051-005-7523-5
7. Hillie T, Hlophe M. Nanotechnology and the challenge of clean water. Nat Nanotechnol (2007) 2(11):663–4. doi:10.1038/nnano.2007.350
8. Geiser K. Nanotechnology and environmental and public health considerations. New Solut (2004) 14(1):9–18. doi:10.2190/G05Y-WGRK-WN8U-AAB4
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
9. Sahoo S, Parveen S, Panda J. The present and future of nanotechnology in human health care. Nanomedicine (2007) 3(1):20–31. doi:10.1016/j.nano.2006.11.008
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
10. McCarthy J. What is Artificial Intelligence? (2002) [cited 2014 August 22]. Available from: http://www-formal.stanford.edu/jmc/whatisai/whatisai.html
11. Patel VL, Shortliffe EH, Stefanelli M, Szolovits P, Berthold MR, Bellazzi R, et al. The coming of age of artificial intelligence in medicine. Artif Intell Med (2009) 46(1):5–17. doi:10.1016/j.artmed.2008.07.017
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
12. Neill DB. New directions in artificial intelligence for public health surveillance. Intell Syst (2012) 15217(15218):15101. doi:10.1109/MIS.2012.18
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
13. Linford L. Artificial Intelligence and Public Health Implications in 2013 and Beyond (2013) [cited 2014 September 23]. Available from: http://usuphi.blogspot.com/2013/04/artificial-intelligence-and-public.html
14. Yan P, Zeng D, Chen H. A review of public health syndromic surveillance systems. In: Sharad M; Zeng DD, Hisnchun C, Bhavani T, Fei-Yue W, editors. Intelligence and Security Informatics. San Diego, USA: Springer (2006). p. 249–60.
15. Milinovich GJ, Williams GM, Clements AC, Hu W. Internet-based surveillance systems for monitoring emerging infectious diseases. Lancet Infect Dis (2014) 14(2):160–8. doi:10.1016/S1473-3099(13)70244-5
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
16. Polgreen PM, Chen Y, Pennock DM, Nelson FD, Weinstein RA. Using Internet searches for influenza surveillance. Clin Infect Dis (2008) 47(11):1443–8. doi:10.1086/593098
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
17. Lee K, Agrawal A, Choudhary A, editors. Real-time disease surveillance using twitter data: demonstration on flu and cancer. Proceedings of the 19th ACM SIGKDD International Conference on Knowledge Discovery and Data Mining. New York, USA: ACM (2013).
18. Castelnuovo G, Manzoni GM, Pietrabissa G, Corti S, Giusti E, Molinari E, et al. Obesity and outpatient rehabilitation using mobile technologies: the potential mHealth approach. Psychol Clin Settings (2014) 5:559. doi:10.3389/fpsyg.2014.00559
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
19. Castelnuovo G, Simpson S. Ebesity-E-health for obesity – new technologies for the treatment of obesity in clinical psychology and medicine. Clin Pract Epidemiol Ment Health (2011) 7:5. doi:10.2174/1745017901107010005
20. Cesa GL, Manzoni GM, Bacchetta M, Castelnuovo G, Conti S, Gaggioli A, et al. Virtual reality for enhancing the cognitive behavioral treatment of obesity with binge eating disorder: randomized controlled study with one-year follow-up. J Med Internet Res (2013) 15(6):e113. doi:10.2196/jmir.2441
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
21. Baldini F. New trends in biosensors for health care. Anal Bioanal Chem (2005) 381(5):1003. doi:10.1007/s00216-005-3100-0
22. Hwang S-W, Tao H, Kim D-H, Cheng H, Song J-K, Rill E, et al. A physically transient form of silicon electronics. Science (2012) 337(6102):1640–4. doi:10.1126/science.1226325
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
23. Dulin MF, Ludden TM, Tapp H, Blackwell J, de Hernandez BU, Smith HA, et al. Using geographic information systems (GIS) to understand a community’s primary care needs. J Am Board Fam Med (2010) 23(1):13–21. doi:10.3122/jabfm.2010.01.090135
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
24. Free C, Phillips G, Watson L, Galli L, Felix L, Edwards P, et al. The effectiveness of mobile-health technologies to improve health care service delivery processes: a systematic review and meta-analysis. PLoS Med (2013) 10(1):e1001363. doi:10.1371/journal.pmed.1001363
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
25. Salinas-Miranda AA, Nash MC, Salemi JL, Mbah AK, Salihu HM. Cutting-edge technology for public health workforce training in comparative effectiveness research. Health Informatics J (2013) 19(2):101–15. doi:10.1177/1460458212461366
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
26. Speros C. Health literacy: concept analysis. J Adv Nurs (2005) 50(6):633–40. doi:10.1111/j.1365-2648.2005.03448.x
27. Vaseashta A, Vaclavikova M, Vaseashta S, Gallios G, Roy P, Pummakarnchana O. Nanostructures in environmental pollution detection, monitoring, and remediation. Sci Tech Adv Mat (2007) 8(1):47–59. doi:10.1016/j.stam.2006.11.003
Keywords: public health, megatrend, twenty-first century, nanotechnology, artificial intelligence
Citation: Rubens M, Ramamoorthy V, Saxena A and Shehadeh N (2014) Public health in the twenty-first century: the role of advanced technologies. Front. Public Health 2:224. doi: 10.3389/fpubh.2014.00224
Received: 28 September 2014; Accepted: 21 October 2014;
Published online: 10 November 2014.
Edited by:
Roger A. Harrison, The University of Manchester, UKReviewed by:
Milka Dančević-Gojković, Public Health Institute of Federation of Bosnia and Herzegovina, Bosnia and HerzegovinaGianluca Castelnuovo, Università Cattolica del Sacro Cuore, Italy
Copyright: © 2014 Rubens, Ramamoorthy, Saxena and Shehadeh. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: mrube001@fiu.edu
 Muni Rubens
Muni Rubens Venkataraghavan Ramamoorthy
Venkataraghavan Ramamoorthy Anshul Saxena
Anshul Saxena Nancy Shehadeh
Nancy Shehadeh