- 1Health Policy and Management, School of Public Health, University of Minnesota, Minneapolis, MN, United States
- 2Office of Health Information Technology, Minnesota Department of Health, St. Paul, MN, United States
- 3Courage Kenny Rehabilitation Institute, AllinaHealth, Minneapolis, MN, United States
- 4Environmental Health Sciences, School of Public Health, University of Minnesota, Minneapolis, MN, United States
- 5Minnesota Department of Health, St Paul, MN, United States
We describe a master’s level public health informatics (PHI) curriculum to support workforce development. Public health decision-making requires intensive information management to organize responses to health threats and develop effective health education and promotion. PHI competencies prepare the public health workforce to design and implement these information systems. The objective for a Master’s and Certificate in PHI is to prepare public health informaticians with the competencies to work collaboratively with colleagues in public health and other health professions to design and develop information systems that support population health improvement. The PHI competencies are drawn from computer, information, and organizational sciences. A curriculum is proposed to deliver the competencies and result of a pilot PHI program is presented. Since the public health workforce needs to use information technology effectively to improve population health, it is essential for public health academic institutions to develop and implement PHI workforce training programs.
Introduction
With the increasing use of electronic data collection and storage, there is an increasing focus on information and knowledge management systems (1). This results in public health workforce needs for public health informatics (PHI) professionals skilled in designing and implementing these systems. PHI professionals are those who “work in practice, research, or academia and whose primary work function is to use informatics to improve the health of populations” (2). Recent studies highlight the need for informatics training in the public health workforce (3, 4). Similarly, the Council on Education for Public Health (CEPH) includes informatics as a foundational competency for accreditation of public health programs (5, 6). We build on the literature for developing informatics’ savvy public health departments (7–10) and PHI core competency descriptions (11, 12) to design a curriculum for a Master’s in Public Health (MPH) and certificate in PHI. The proposed curriculum differs from many existing health informatics programs by emphasizing the public health informatician’s architectural role as a systems analyst linking public health users and information technology specialists by guiding the analysis and design of information systems. The focus is on: (a) problem definition for public health information systems (PHInfSys); (b) analyzing, designing, and implementing effective PHInfSys, such as surveillance, community health assessment, and population health management systems (11, 13), (c) encoding, collecting, curating, storing, retrieving, and analyzing data to create information, (c) assuring system and data governance, management, integration, confidentiality, and security, (e) creating and managing information technologies, and (f) collaborating in and leading inter-disciplinary and cross-cutting teams.
The foundation of public health is information, collected across a variety of sources with the goal of generating and disseminating new knowledge and instituting actions to improve the public’s health. The need for public health education programs to be informed by current public health needs and employment opportunities has been long noted (14), as has the importance of establishing academic-practice links with public health agencies and training students in practice situations. In 2001, the need for PHI training was noted in an American Medical Informatics Association (AMIA) conference on developing a PHI agenda (15). In 2012, AMIA revisited and updated these recommendations (16). Both reports covered technical topics, such as information architecture and standards, governance and policy, including confidentiality and privacy, and workforce training. These needs are addressed by the PHI training program we describe.
The 2012 AMIA reported noted that the “The public health value chain is composed of business processes and use cases that describe the flow of data and information. Business processes describe how data, information, and knowledge are used by creating a framework that relates work activities to domains of public health function” (16). PHI is a foundation for modernizing public health value chains, including public health department business processes (17), public health surveillance (18, 19), public health emergency response, population health science (20), population health management (21), learning health systems (22), and public health research. PHI is an essential specialization that bridges the digital gap public health agencies face given growing expectations of service and preparedness. PHI integrates knowledge and skills from the information sciences (computer, information, organizational, and systems sciences) with public health expertise and “includes the conceptualization, design, development, deployment, refinement, maintenance, and evaluation of communication, surveillance, and information systems relevant to public health” (23).
While PHI shares some core skills with other health informatics domains, such as bioinformatics or clinical and nursing informatics, it is distinct in necessitating integration of core informatics skills with public health systems, such as surveillance systems, community health assessment, disease/condition registries, and prevention programs in an overall framework of population health science. Public health informaticians (PHInf) differ from information technologists (ITs) because “The focus of IT is to implement and operate information systems (hardware and software) that meet programmatic needs. In contrast, PHInf have a strategic and systems view of how information systems and technology can impact public health, such as how information systems can support public health decision-making. Unlike IT specialists, PHInf work within the larger context of how information systems function within the political, cultural, economic, and social environment and evaluate their impact within the broad sphere of public health. Thus, PHInf are in the unique position to understand how information systems can improve the practice and science of public health while contributing to the evidence-based practice of public health informatics” (11).
Our paper focuses on training PHInf through MPH and certificate programs to provide them a foundation for a PHI professional career. The professional role is one of four related PHI roles identified by the PHI Institute, the Association of State and Territorial Health Officials, and the National Association of County and City Health Officials (NACCHO): executive; manager; professional; and clinical (24). The curriculum design highlighted here focuses on the professional role because it is a frontline position that is the foundation for a career path through management to executive leadership (25).
Our paper describes program design objectives and assumptions, design challenges, and core competencies. This overview provides context and prioritization for the program design.
PHI Program Design Objectives and Assumptions
The objective of PHI training is to educate PHInf with public health and PHI knowledge and skills that enable them to design and implement effective PHInfSys and have a successful PHI career. The design assumes that PHInf require competencies in (a) public health core competencies (26), functions, and systems [e.g., disease and environmental surveillance (19), population health management (21), and community health assessment (21, 27, 28)], (b) design thinking and systems analysis (29–31), (c) computer, information, organizational, and systems sciences (23, 32), (d) evaluating information systems effectiveness (33), and (e) teamwork and project management.
The core public health functions are assurance, assessment, and advocacy, which are used to maximize population health (34). The PHI program design focuses on understanding how information systems achieve these functions rather than having a sub-goal focus on technological, computer science, or data mining aspects of PHI. Because PHI focuses on designing PHInfSys it has a foundation in design thinking (29–31). Design thinking focuses on identifying problems as gaps in population health that information systems can help reduce by determining the root causes of those gaps and designing and implementing information systems to reduce population health gaps. Systems analysts are the architects who bridge the gap between users and technologies by understanding and translating user needs to system specifications and collaborating with technologists to implement those systems. The goal of systems analysis is to minimize the frequent disconnects between information system development and the usefulness of the resulting information systems (35, 36) by avoiding simply automating existing inefficient information pathways.
To address these disconnects, effective systems analysis requires that PHInf are “well grounded in the fundamentals of organization theory, decision-making, teamwork and leadership, and research methods as well as current and emerging information systems technologies” (37). PHInf also need the ability to design, implement, and evaluate information systems in multiple contexts, using approaches such as realistic evaluation and context-mechanism-outcome configurations (CMOc) (33).
Finally, PHInf need strong teamwork and project management skills because “PHI is cross-cutting. … Informaticians see the ‘big picture’ and ‘connects the dots’ across all of the other fields related to public health” (13). Because information systems span diverse domains, the public health informatician requires the knowledge and skills to collaborate with diverse clients, lead systems analysis and development, and coordinate the diverse specialists implementing information systems, data use and privacy agreements, data and vocabulary standards, evaluation, training, and more.
In sum, PHInf require competencies in (a) public health core concepts and systems, (b) systems thinking and systems analysis, (c) computer, information, organizational, and systems sciences, (d) evaluating information systems effectiveness, and (e) the ability to work in and lead teams. These competencies provide the foundation for successfully progressing from being a PHI professional to PHI leadership positions.
PHI Program Design Challenges
Public health informatics requires many different competencies. This can result in a laundry list of competencies that are not feasible to implement in a credit-constrained curriculum. Implementing a constrained educational program requires competency prioritization and trade-offs. There are three major challenges.
(1) Content: PHI requires competencies in distinct domains—public health, health informatics, computer, information, and organizational sciences (2, 12, 32). These include required core competencies for public health practice (38). Health informatics and computer science focus on technical competencies. Information, systems, and organizational science competencies support solving population health problems because they provide systems analysis and design competencies needed to: (1) understand and translate user needs into system requirements and (2) create designs that can be implemented by ITs. Computer science competencies, such as modular decomposition, data structures, algorithms, programming languages, database theories, and system architectures are necessary to provide PHInf the knowledge and skills to communicate and collaborate effectively with ITs implementing PHInfSys.
(2) Curricular independence vs integration: Siloed, independent courses maximize covering competency breadth, but rely on students to integrate across competencies. Courses integrating competencies develop the skills to apply informatics in public health. Examples of integrating competencies include using population health management and surveillance examples in technical courses, such as systems analysis, database, or health information exchange.
(3) Declarative vs procedural competencies: Declarative competencies are familiarity with analysis tools, such as requirements analysis, business process modeling, use cases, data flow diagrams, and entity relationship diagrams. Procedural competencies are being able to develop requirements, business process models, use cases, data flow diagrams, and entity relationship diagrams. Training in procedural competencies requires experiential practicums in which students apply declarative competencies. Increasing the emphasis on procedural competencies limits the breadth of declarative competencies that can be covered. The PHI design focuses on developing strong procedural competencies in system analysis because it is the core competency used to design and implement effective PHInf.
In sum, design challenges include decisions about content, integration (independent/integrated), and competency type (declarative/procedural) tradeoffs.
The proposed PHI design focuses on public health core competencies and organization/systems/information sciences related to analyzing, designing, implementing, and disseminating effective information systems in public health. Integrating competencies across courses maximizes the ability to apply skills in public health settings. For declarative and procedural learning, experiential practicums assure the ability to apply declarative knowledge. Elective credits support students in developing deeper skills in areas they are interested in, such as data management, analytics/data mining, GIS, visualization/communication, health information exchange (39), leading community health information exchange, or surveillance systems (19).
PHI Competencies
A PHI competency is a measurable and demonstrable knowledge related to the role “of developing innovative applications of technology and systems that address public health priorities by analyzing how information is organized and used and evaluating how this work contributes to the scientific field” (11). The master’s level competencies for PHI professionals build on earlier work (11, 12). Not all competencies listed in earlier work are included for three reasons. First, the selected competencies need to fit into a typical MPH curriculum. While there are many desirable and important competencies, there is limited curriculum time. Second, some competencies reflect work in a practice setting that are not directly measurable (e.g., collaborating with others in program development, offering insights, contributing to decision-making, leading knowledge management). Third, some competencies are more managerial/executive competencies than professional competencies.
Core Competencies
Core competencies include both public health and PHI. Public health core competencies (6, 26) are addressed through the required MPH curriculum courses. This material is extended by integrating competencies related to public health systems, surveillance systems, population health management, community health assessment, eHealth, program monitoring, and evaluation in the PHI courses. For example, using electronic disease surveillance, population health management, community health assessment, and other public health systems as examples in the systems analysis courses educates students in the use of systems analysis to address common public health systems (17, 40).
Public health informatics competencies focus on systems analysis and data modeling. These include computer science and health informatics competencies related to nomenclature, standards, platforms, information architecture, inter-operability, and systems analysis and data modeling which require integration of material from organization/information systems/systems sciences, public health, and computer sciences. This integration builds the overall competency to design PHInfSys to solve problems in the public health domain. These competencies are noted as central to PHI. For example, “Redesigning Public Health Surveillance in an eHealth World” demonstrates the importance of systems analysis when it points out that “Defining requirements is a critical step in developing or acquiring an information system that will effectively support the work of the organization” (40). Similarly, system selection depends “on the clarity and applicability of the use cases you define, and on determining prior to the demonstration how—based on what criteria—the use-case demonstrations will be judged” (40) as well as business process definitions (40). The description of an informatics savvy health department states that “Information systems managers and staff require competency in creating formal system requirements” (7). Requirements, use cases, and business process definitions are produced by systems analysis and require expertise in the system development life cycles (SDLC), national standards, and public policy related to informatics (e.g., meaningful use) (8). Complementary competencies are those that support systems analysis and data modeling (41), such as standards (e.g., HL7), nomenclature (e.g., ICD, CPT) (42), data flow diagrams, relational database theory, and query languages that inform system analysis and are used during implementation.
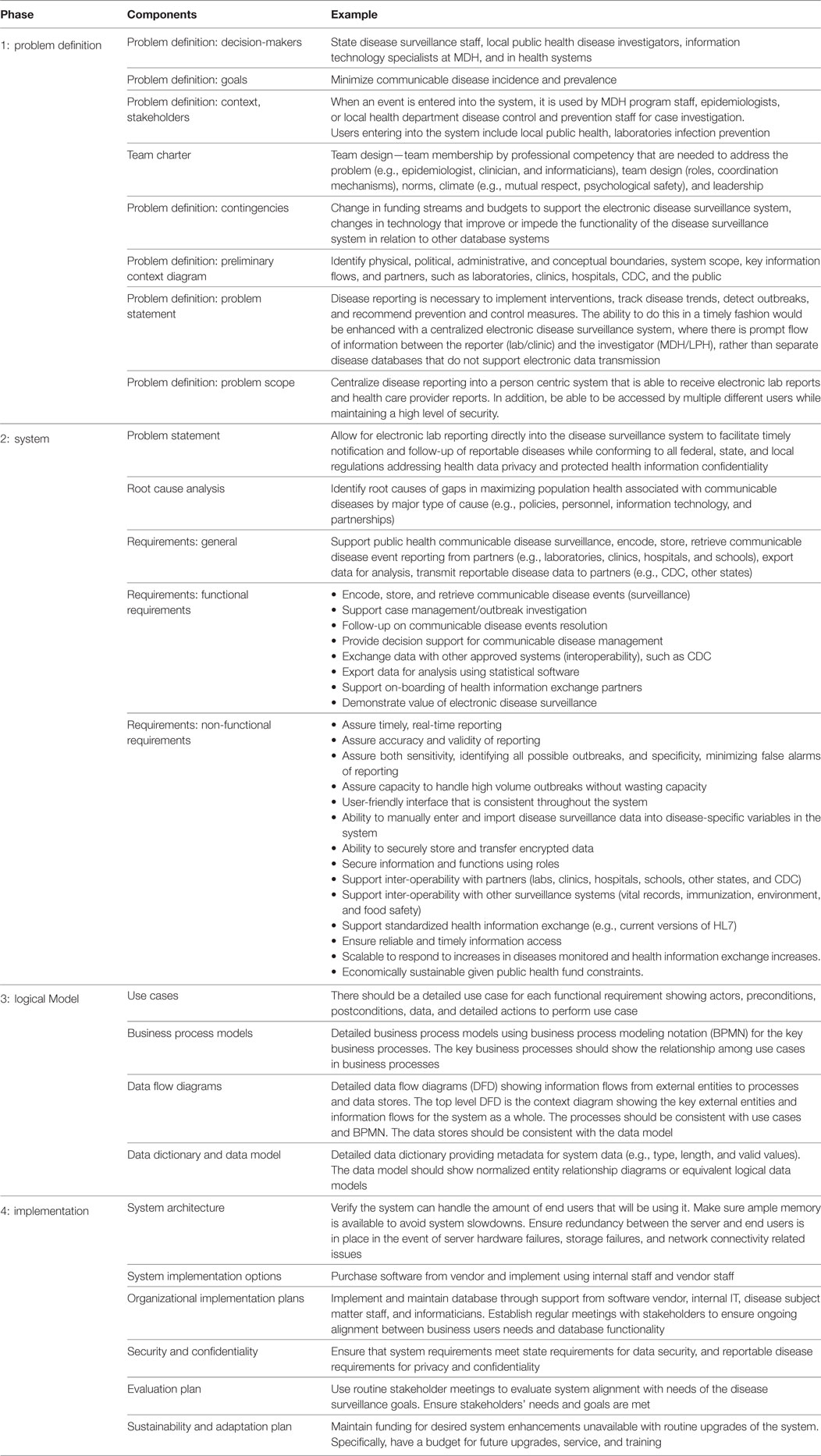
As an example, Table 1 illustrates systems analysis competencies for electronic disease surveillance. The goal of the system is to maximize population health by minimizing transmission of communicable diseases, which is done “through early identification, treatment, and resolution of health conditions” (17). Systems analysis requires integrating competency in systems analysis with expertise in the system’s public health domain (e.g., electronic disease surveillance). The first analysis phase defines the problem, its decision-makers, context, and stakeholders. The second phase does a root cause analysis of gaps in population health related to communicable disease surveillance or system productivity and describes functional requirements, what tasks the communicable disease surveillance system supports, and nonfunctional requirements, criteria that the system has to meet. The third phase describes the logical model, the use cases corresponding to each functional requirement, business processes, data flows, and data model. Design and implementation is the final phase and builds on the analysis in the earlier phases to design and implement the information system that supports communicable disease surveillance staff in their activities.
Declarative and Procedural Competencies
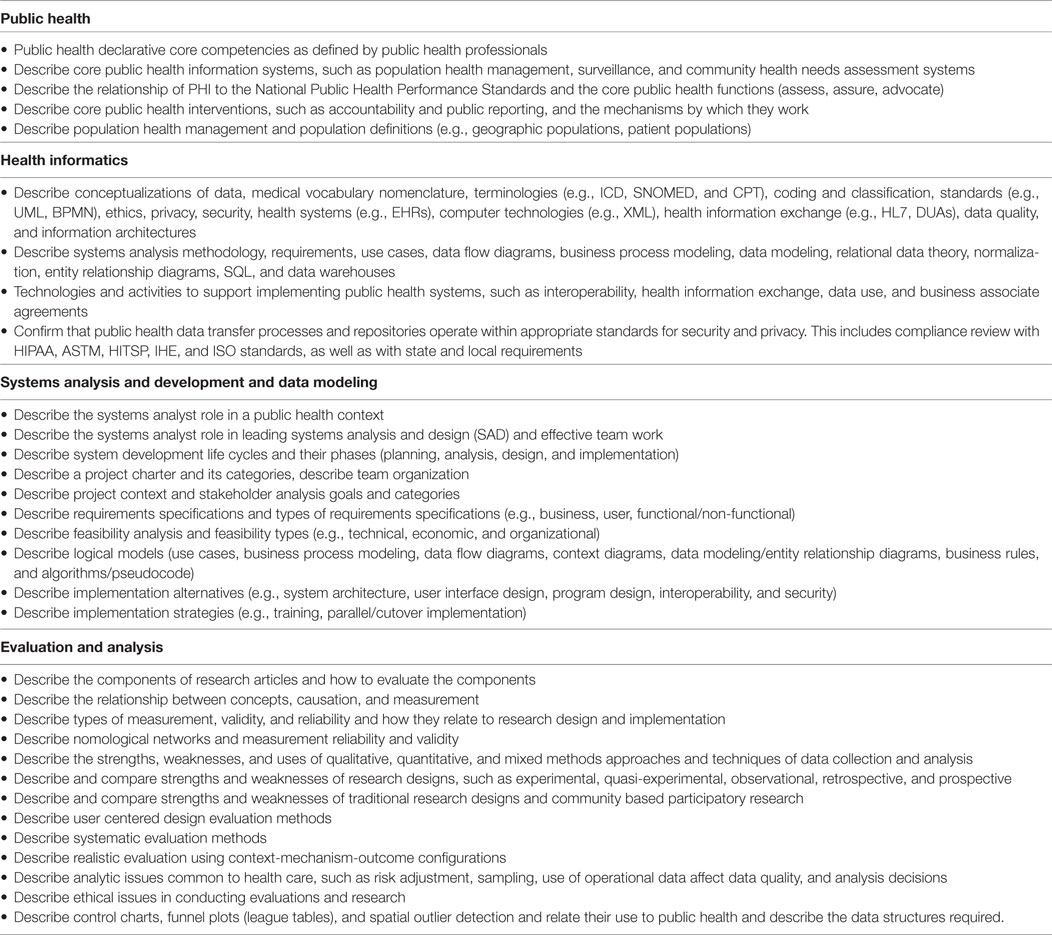
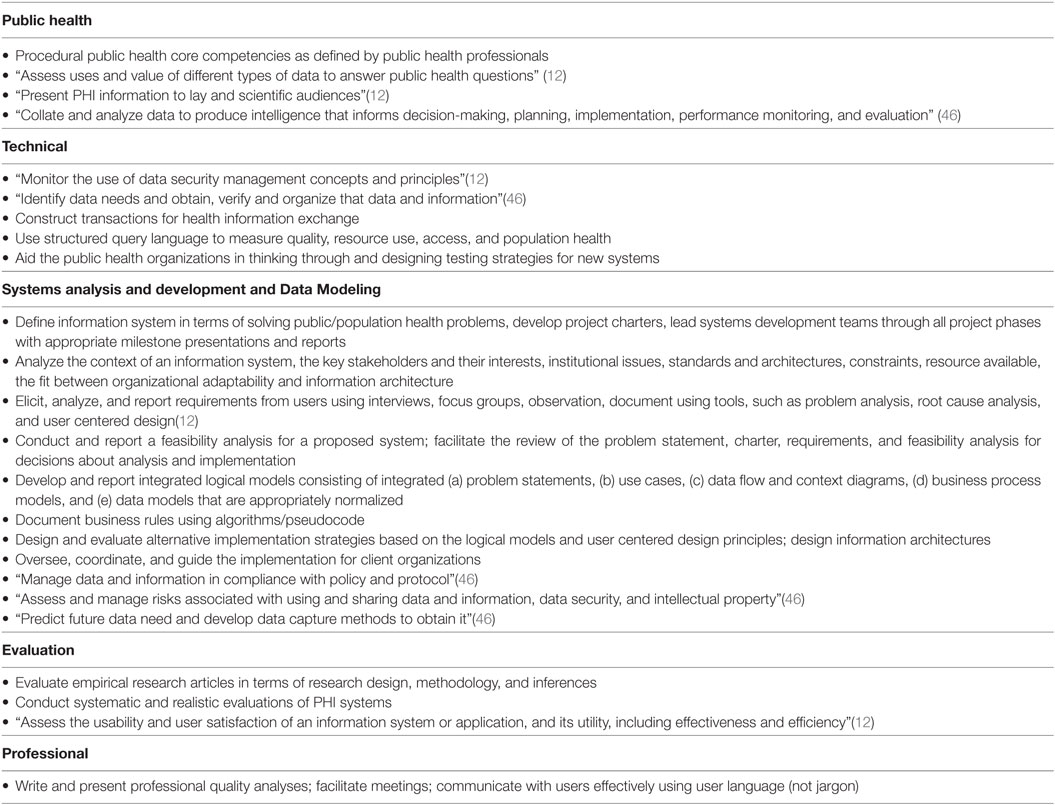
Tables 2 and 3 show the MPH PHI declarative and procedural competencies, which have a strong focus on those competencies also used in systems analysis and data modeling. These competencies reflect the informaticians’ architect role, which focuses on the problem definition and solving skills associated with defining problems, identifying requirements, building logical models, describing core features of information systems (use cases, data flows, data models, business processes), designing implementation alternatives, overseeing implementation, and facilitating user centered design and choice.
The declarative and procedural competencies also include a significant focus on research analysis and evaluation methods because PHInfSys are interventions designed to improve population health by improving quality, reducing costs, or both. Given the intervention aspect, a PHInf should have the competencies to be able to evaluate whether the public health information system accomplished its goals and how the information system functions in different contexts [realistic evaluation (33)]. Effective evaluation requires enough expertise in public health systems, such as disease surveillance (18), quality improvement (43), public reporting, such as control charts, funnel plots (league tables) (44), and spatial outlier detection (45), to be able to assess how well they are implemented as well as their effectiveness. Competencies in assessing measurement validity and reliability are central to measuring population health.
Electives
Electives allow students to pursue specializations in related public health and PHI competencies such as:
• PHI management: project management, health information management, public health leadership, and leading change for regional and community information systems.
• PHI tools: ePublic health, using the web and mobile apps for health promotion, GIS for public health, health care operations research and analytics, public health decision support systems, eHealth, health information exchange, and surveillance systems in depth.
• PHI evaluation: decision analysis for policy analysis, cost-effective analysis, program evaluation, usability engineering, and realistic evaluation.
• Environmental health systems: Complex systems modeling for population health, infectious diseases, environmental health risk assessment, surveillance of foodborne diseases and food safety hazards.
• Analytics and data mining: Advanced statistical computing, statistical learning and data mining, survival analysis, statistics for surveillance and quality improvement.
• Computer science: Algorithms and data structures, principles and practice of database systems, data marts and warehouse management, NoSQL and alternatives to relational data models.
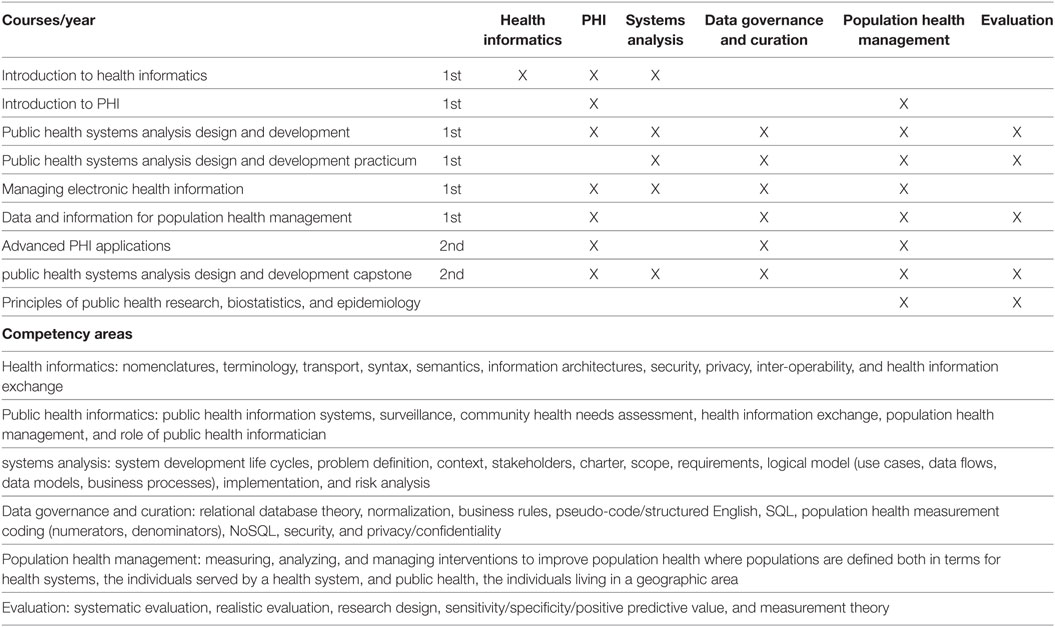
Organizing Competencies into Courses
The design addresses siloing vs. integration in two ways (Table 4). First, given that the application of informatics competencies is conditional on public health context, informatics and public health competencies are strongly integrated. Students need the expertise to apply the informatics concepts in the domain they will practice. Second, a practice-based practicum in the introductory systems analysis course and a practice-based capstone systems analysis course integrate practice and academics.
As an example, informatics competencies in systems analysis courses (introduction and capstone) are illustrated using PHInfSys. The relational database course (managing electronic health information) uses population health measurement for SQL assignments. Data and information for population health management, which focuses on substantive issues related to population health management uses relational database theory and SQL for assignments in population health management and frames the evaluation of public health interventions using realistic evaluation. In sum, the design emphasizes the integration of systems analysis, database, and evaluation competencies with public health systems and population health management. The objective is to train students in informatics competencies, public health competencies, and the use of informatics skills in public health settings. A separate course addresses competencies that are general and applicable to many areas, such as standards, nomenclature, health information exchange layers, and technical issues.
Implications for Policy and Practice
This paper proposes a master’s level public health curriculum to support workforce development in PHI competencies. The competencies are similar to those described for public health core competencies (6) and in the Advanced Health Informatics Certification (47) with the goal of preparing PHInf who “Practice health informatics with an operational focus on information and knowledge problems that directly impacts the practice of health care, public health, and personal health” (47). Edward Baker and his colleagues recently made a strong business case for PHI (48) arguing that public health is an information intensive business and that health information systems are transforming the way that information management speeds responses to health threats, promote health, and supports public health decision-making. The foundation of these systems are the essential public health services, a focus on population health, and core informatics competencies, such as system analysis, database theory, and health informatics. The implementation of effective PHInfSys requires individuals with the competencies described in this paper.
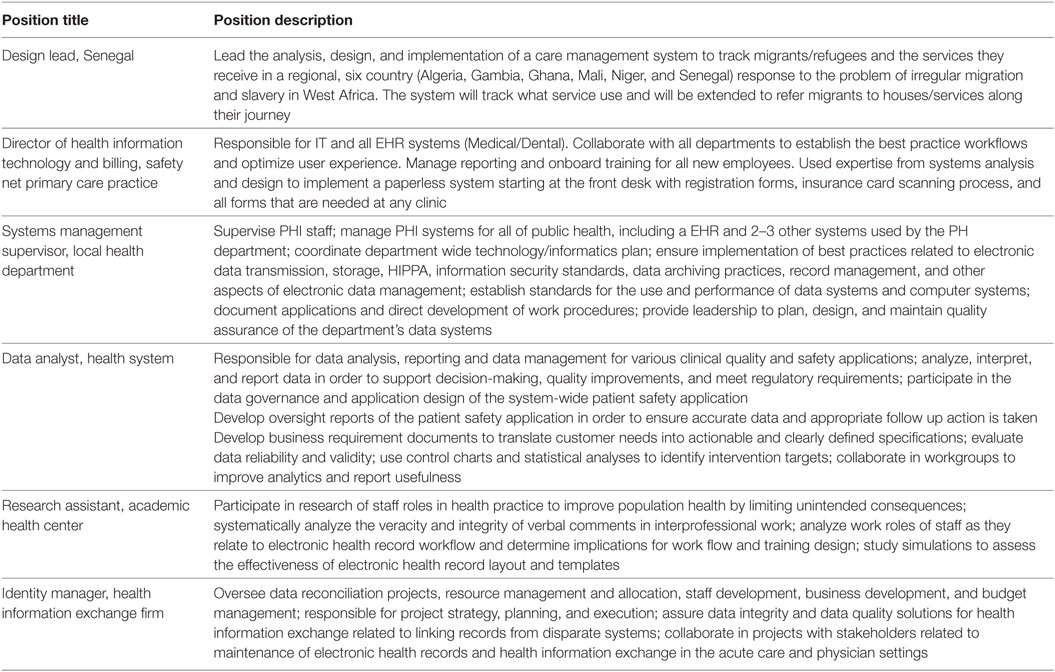
This program design was based on Carnegie Mellon’s highly successful information systems program which focus on systems analysis and information technology skills to “design and implement effective solutions to meet organizational and management needs for information and decision support ” (37). The program was implemented in the School of Public Health at the University of Minnesota in the Fall of 2013. The first year courses have been offered, evaluated, and refined five times and the second year courses have been offered and refined four times. Thus far, 19 students have earned PHI certificates signifying completion of PHI core courses; 15 will have completed the MPH in PHI by May 2018. The certificate attracted diverse students, including students from health informatics, pharmacy, environmental health, and epidemiology. Applicants have expressed interest in PHI because they feel that data and information is critical to public health research and practice and they feel that learning informatics and analytics in a public health context will help them to identify opportunities for improving population health. Students in the PHI program have had internships supporting quality improvement and population health management with a safety net clinic network, database administration in health care systems and professional organizations, and supporting standards implementation in electronic disease surveillance systems in state health departments. Graduates of the PHI program have been successful in securing positions across private and public health sectors and some have pursued further degrees in health informatics. Seven of the 10 MPH-PHI graduates are employed in positions related to PHI. Table 5 provides a sample of their job descriptions. The job responsibilities span the spectrum from leading projects in PHI and population health management to offering technical support in data management and research coordination. Future program evaluation should measure the degree to which graduates are engaged in public health related activities, are engaged in PHI related activities, initial placement, and career growth.
There are development and sustainability issues that occur because PHI is a new field. First, program development requires collaborating with faculty and stakeholders to communicate what PHI is and a vision of its value (13). Second, marketing and social media programs that convey PHI’s contribution to new and existing public health students need to be developed. Third, partnerships with stakeholders for course based projects and integrating practice with academics have to be developed. Fourth, PHI program development requires funding commitment from schools of public health until enrollment reaches a break-even point. Finally, PHI faculty who have competency in both public health and informatics need to be developed. Until PHI as a field is more institutionalized, a potential tactic for doing this is recruiting post-doctoral staff from fields within public health (e.g., epidemiology, environmental health) and have them develop PHI competencies while developing PHI related research and/or recruiting post-doctoral staff from related informatics disciplines (49) and have them develop public health competencies while developing PHI related research and teaching. While these barriers appear substantial, PHI should be sustainable because of the growth in informatics related disciplines and because of skilled PHInf being in high demand as valuable team members in both research and practice.
Conclusion
The effective and efficient collection of quality public health data and information is intensive. It is the foundation of public health functions, such as surveillance, community health assessment, evaluation, and research. PHI is a profession that focuses on the design of governance, analysis, development, and management of information systems that acquire and integrate data that is used in public health functions, such as disease and environmental surveillance, program evaluation, policy analysis, and research. PHI provides the foundation for organizing and collecting data that is used in performing public health functions. PHI is an emerging, distinct, and needed profession in public health that uses knowledge and skills drawn from computer, information, and organizational sciences and public health to develop critical information systems that provide the data and information that other public health professionals use in their work. PHInf provide the expertise in public health, information, and information technology to take advantage of technology advances to improve the PHInf.
This paper proposes a PHI curriculum for schools of public health that can be implemented through MPH and certificate programs. The curriculum provides core competencies in public health and in computer, information, and organizational sciences that are needed by PHInf. The proposed curriculum addresses the challenges of integrating PHI in public health functions, developing declarative knowledge and procedural skills in PHI through a balance of lecture and practicum courses, and allowing the pursuit of specializations. A key focus of the proposed curriculum is its user centered design through systems analysis and systems thinking. This provides PHInf the competencies necessary to lead, design, and implement PHInfSys that take advantage of technology advances.
The proposed program is a starting point. Given the rapidity of change in public health practice, public health research, informatics, and information technology, the curriculum will need to evolve to meet changing needs. This evolution should be guided by partnerships with stakeholders in practice, other public health disciplines, and public health researchers to assure that PHInf are effectively designed and developed to meet the needs of those working to improve population health. This development can be guided by the continued evaluation of PHInf to assure they meet user needs and the continued evaluation of PHI programs to assure they are training the workforce that can lead developments in PHInfSys.
There is a clear need to develop a PHI workforce. It is imperative that public health institutions, both practice and academic, take action and support the development of a strong PHI workforce. This can be achieved through on-the-job training, fellowships, internships, and academic training. The educational program we propose addresses schools of public health, and provides guidelines for implementing PHI training programs. However, support is also needed from public health practitioners to ensure that PHI training is prioritized to meet the evolving demands of the practice environment. With these tools we can continue to develop an effective and relevant workforce that can navigate the changing trends of public health to improve population health.
Author Contributions
All authors contributed to the conceptualization of this paper. DW, RK, and SR led the curriculum conceptualization and development. ML, SR, and DW led the focus on public health informatics (e.g., the informatics savvy health department, immunization systems), CH, SR, and CK led the focus on applications of PHI in electronic disease surveillance system. DW and ML did the first draft. RK, SR, CH, and CK edited and provided components (e.g., description of electronic disease support systems, contents of systems analysis competencies). All read the final version, edited it, and approved it for submission.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We thank Pat Larkey, Sara Kiesler, Serge Taylor, Bill Hefley, Kathleen Carley, and the Information Systems program at Carnegie Mellon University for foundational ideas. We thank Julie Jacko, Daniel Chan, and Matteo Convertino for their ideas and help in implementing the PHI program at Minnesota. We thank Rochelle Martin, Raul Noriega, Megan Pruente, Cole Schluchter, Nicholas Solberg, Herong Song, and Patrick Williams for information on their current job responsibilities and comments about the PHI program. We thank MPH and certificate PHI students for working with us to develop the program. We thank Ira Moscovice the Health Policy & Management Department, and the School of Public Health at the University of Minnesota for supporting PHI program development.
References
1. Freed J, Kyffin R, Rashbass J, Organ S, Boseley P, Haworth A, et al. Knowledge Strategy: Harnessing the Power of Information to Improve the Public’s Health. London: Public Health England (2014).
2. US Department of Health and Human Services (HHS) and Centers for Disease Control and Prevention (CDC) and University of Washington School of Public Health and Community Medicine’s Center for Public Health Informatics. Competencies for Public Health Informaticians 2009. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention (2009).
3. Massoudi BL, Chester K, Shah GH. Public health staff development needs in informatics: findings from a national survey of local health departments. J Public Health Manag Pract (2016) 22:S58–62. doi:10.1097/PHH.0000000000000450
4. Beck AJ, Leider JP, Coronado F, Harper E. State health agency and local health department workforce: identifying top development needs. Am J Public Health (2017) 107:1418–24. doi:10.2105/AJPH.2017.303875
5. Calhoun JG, Ramiah K, Weist EM, Shortell SM. Development of a core competency model for the master of public health degree. Am J Public Health (2008) 98:1598–607. doi:10.2105/AJPH.2007.117978
6. Council on Education for Public Health. Accreditation Criteria Schools of Public Health & Public Health Programs. Silver Spring, MD: Council on Education for Public Health (2016).
7. LaVenture M, Brand B, Ross DA, Baker EL. Building an informatics-savvy health department: part I, vision and core strategies. J Public Health Manag Pract (2014) 20:667–9. doi:10.1097/PHH.0000000000000149
8. LaVenture M, Brand B, Ross DA, Baker EL. Building an informatics-savvy health department II: operations and tactics. J Public Health Manag Pract (2015) 21(1):96–9. doi:10.1097/PHH.0000000000000179
9. LaVenture M, Brand B, Baker EL. Developing an informatics-savvy health department: from discrete projects to a coordinating program. Part I: assessment and governance. J Public Health Manag Pract (2017) 23:325–7. doi:10.1097/PHH.0000000000000551
10. Brand B, Laventure M, Baker E. Developing an informatics-savvy health department: from discrete projects to a coordinating program-part III, ensuring well-designed and effectively used information systems. J Public Health Manag Pract (2018) 24:181–4. doi:10.1097/PHH.0000000000000756
11. Office of Workforce and Career Development and University of Washington School of Public Health and Community Medicine’s Center for Public Health Informatics. Competencies for Public Health Informaticians 2009. Atlanta, GA: Centers for Disease Control and Prevention (2009).
12. Miner K, Alperin M, Brogan CW, Buchanan N, Brand B. Applied Public Health Informatics Curriculum. Decatur, GA: Public Health Informatics Institute (2011).
13. Fond M, Volmert A, Kendall-Taylor N. Making Public Health Informatics Visible: Communicating an Emerging Field. Washington, DC: The FrameWorks Institute (2015).
14. Institute of Medicine. The Future of Public Health. Washington, DC: The National Academies Press (1988).
15. Yasnoff WA, Overhage JM, Humphreys BL, Laventure M. A national agenda for public health informatics: summarized recommendations from the 2001 AMIA spring congress. J Am Med Inform Assoc (2001) 8:535–45. doi:10.1136/jamia.2001.0080535
16. Massoudi BL, Goodman KW, Gotham IJ, Holmes JH, Lang L, Miner K, et al. An informatics agenda for public health: summarized recommendations from the 2011 AMIA PHI conference. J Am Med Inform Assoc (2012) 19:688–95. doi:10.1136/amiajnl-2011-000507
17. Public Health Informatics Institute and National Association of County and City Health Officials. Taking Care of Business: A Collaboration to Define Local Health Department Business Processes. Second Printing. Decatur, GA: Public Health Informatics Institute (2008).
18. McNabb SJ, Conde JM, Ferland L, Macwright W, Okutani S, Park MM, et al., editors. Transforming Public Health Surveillance: Proactive Measures for Prevention, Detection, and Response. Amman, Jordan: Elsevier (2016).
19. McNabb SJ, Ryland P, Sylvester J, Shaikh A. Informatics enables public health surveillance. J Health Spec (2017) 5:55. doi:10.4103/jhs.JHS_28_17
20. Bachrach CA, Daley DM. Shaping a new field: three key challenges for population health science. Am J Public Health (2017) 107:251–2. doi:10.2105/AJPH.2016.303580
21. Kindig DA. Understanding population health terminology. Milbank Q (2007) 85:139–61. doi:10.1111/j.1468-0009.2007.00479.x
22. Friedman C, Rubin J, Brown J, Buntin M, Corn M, Etheredge L, et al. Toward a science of learning systems: a research agenda for the high-functioning learning health system. J Am Med Inform Assoc (2015) 22:43–50. doi:10.1136/amiajnl-2014-002977
23. Yasnoff WA, O’Carroll PW, Koo D, Linkins RW, Kilbourne EM. Public health informatics: improving and transforming public health in the information age. J Public Health Manag Pract (2000) 6:67–75. doi:10.1097/00124784-200006060-00010
24. The Public Health Informatics Institute. Workforce Position Classifications and Description. (2014). Available from: https://www.phii.org/resources/view/6423/workforce-position-classifications-and-descriptions (Accessed: September 15, 2017).
25. The Public Health Informatics Institute. Professional Level Public Health Informatician, Sample Position Description and Sample Career Ladder. (2014). Available from: https://www.phii.org/sites/www.phii.org/files/resource/pdfs/Professional%20Sample%20Position%20AND%20Career%20Ladder.pdf (Accessed: October 5, 2017).
26. The Council on Linkages between Academia and Public Health Practice. Core Competencies for Public Health Professionals. Council on Linkages, editor. Washington, DC: Public Health Foundation (2014). p. 1–24.
27. Berndt DJ, Hevner AR, Studnicki J. The catch data warehouse: support for community health care decision-making. Decis Support Syst (2003) 35:367–84. doi:10.1016/S0167-9236(02)00114-8
28. Kindig D, Stoddart G. What is population health? Am J Public Health (2003) 93:380–3. doi:10.2105/AJPH.93.3.380
30. Dym CL, Agogino AM, Eris O, Frey DD, Leifer LJ. Engineering design thinking, teaching, and learning. J Eng Educ (2005) 94:103–20. doi:10.1002/j.2168-9830.2005.tb00832.x
31. Johansson-Sköldberg U, Woodilla J, Çetinkaya M. Design thinking: past, present and possible futures. Creat Innov Manag (2013) 22:121–46. doi:10.1111/caim.12023
32. Friedman CP. What informatics is and isn’t. J Am Med Inform Assoc (2013) 20:224–6. doi:10.1136/amiajnl-2012-001206
33. Pawson R, Manzano-Santaella A. A realist diagnostic workshop. Evaluation (2012) 18:176–91. doi:10.1177/1356389012440912
34. Centers for Disease Control and Prevention. National Public Health Performance Standards: The Public Health System and the 10 Essential Public Health Services. Atlanta, GA: Centers for Disease Control and Prevention (2014). Available from: https://www.cdc.gov/nphpsp/essentialservices.html (Accessed: May 8, 2017).
35. Harrison MI, Koppel R, Bar-Lev S. Unintended consequences of information technologies in health care – an interactive sociotechnical analysis. J Am Med Inform Assoc (2007) 14:542–9. doi:10.1197/jamia.M2384
36. Pentland BT, Feldman MS. Designing routines: on the folly of designing artifacts, while hoping for patterns of action. Info Organ (2008) 18:235–50. doi:10.1016/j.infoandorg.2008.08.001
37. Carnegie Mellon University. Information Systems. Pittsburgh, PA: Carnegie Mellon University (2016). Available from: https://www.cmu.edu/information-systems/ (Accessed: January 29, 2018).
38. Council on Linkages between Academia and Public Health Practice. Core Competencies for Public Health Professionals. Washington, DC: Public Health Foundation (2014).
39. Dixon B, editor. Health Information Exchange: Navigating and Managing a Network of Health Information Systems. Amsterdam: Elsevier, Academic Press (2016).
40. Public Health Informatics Institute. Redesigning Public Health Surveillance in an eHealth World. Decatur, GA: Public Health Informatics Institute (2012).
42. Hammond WE, Jaffe C, Cimino JJ, Huff SM. Standards in biomedical informatics. 4th ed. In: Edward HS, Cimino JJ, editors. Biomedical Informatics. London: Springer (2014). p. 211–53.
43. Woodall WH. The use of control charts in health-care and public-health surveillance. J Qual Technol (2006) 38:89–104. doi:10.1080/00224065.2006.11918593
44. Dover DC, Schopflocher DP. Using funnel plots in public health surveillance. Popul Health Metr (2011) 9:1–11. doi:10.1186/1478-7954-9-58
45. Sherman RL, Henry KA, Tannenbaum SL, Feaster DJ, Kobetz E, Lee DJ. Applying spatial analysis tools in public health: an example using SaTScan to detect geographic targets for colorectal cancer screening interventions. Prev Chronic Dis (2014) 11:E41. doi:10.5888/pcd11.130264
46. Public Health England. The Public Health Skills and Knowledge Framework (PHSKF). London: Public Health England (2016).
47. Gadd CS, Williamson JJ, Steen EB, Andriole KP, Delaney C, Gumpper K, et al. Eligibility requirements for advanced health informatics certification. J Am Med Inform Assoc (2016) 23:851–4. doi:10.1093/jamia/ocw090
48. Baker EL, Brand W, Davidson A, Laventure M, Singletary V, Smith P. Building the business case for public health information systems. J Public Health Manag Pract (2016) 22:603–6. doi:10.1097/PHH.0000000000000495
Keywords: public health informatics, public health practice, public health workforce, systems analysis, systems design
Citation: Wholey DR, LaVenture M, Rajamani S, Kreiger R, Hedberg C and Kenyon C (2018) Developing Workforce Capacity in Public Health Informatics: Core Competencies and Curriculum Design. Front. Public Health 6:124. doi: 10.3389/fpubh.2018.00124
Received: 14 February 2018; Accepted: 16 April 2018;
Published: 02 May 2018
Edited by:
Rosemary M. Caron, University of New Hampshire, United StatesReviewed by:
Pradeep Nair, Central University of Himachal Pradesh, IndiaMargo Bergman, University of Washington Tacoma, United States
Copyright: © 2018 Wholey, LaVenture, Rajamani, Kreiger, Hedberg and Kenyon. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Douglas R. Wholey, whole001@umn.edu
 Douglas R. Wholey
Douglas R. Wholey Martin LaVenture
Martin LaVenture Sripriya Rajamani
Sripriya Rajamani Rob Kreiger
Rob Kreiger Craig Hedberg
Craig Hedberg Cynthia Kenyon
Cynthia Kenyon