The Split Second Effect: The Mechanism of How Equinus Can Damage the Human Foot and Ankle
- Department of Orthopaedic Surgery, University of Cincinnati, Cincinnati, OH, USA
We are currently in the process of discovering that many, if not the majority, of the non-traumatic acquired adult foot and ankle problems are caused by a singular etiology: non-neuromuscular equinus or the isolated gastrocnemius contracture. There is no question that this biomechanical association exists and in time much more will be uncovered. There are three basic questions that must be answered: why would our calves tighten as we normally age, how does a tight calf, or equinus, actually cause problems remotely in the foot and ankle, and how do the forces produced by equinus cause so many seemingly unrelated pathologies in the foot and ankle? The purpose of this paper is to address the second question: how does a tight calf mechanically cause problems remotely in the foot and ankle? There has been little evidence in the literature addressing the biomechanical mechanisms by which equinus creates damaging forces upon the foot and ankle, and as a result, a precise, convincing mechanism is still lacking. Thus, the mere concept that equinus has anything to do with foot pathology is generally unknown or disregarded. The split second effect, described here, defines exactly how the silent equinus contracture creates incremental and significant damage and injury to the human foot and ankle resulting in a wide variety of pathological conditions. The split second effect is a dissenting theory based on 30 years of clinical and academic orthopedic foot and ankle experience, keen clinical observation along the way, and review of the developing literature, culminating in examination of many hours of slow motion video of normal and abnormal human gait. To my knowledge, no one has ever described the mechanism in detail this precise.
Introduction
Foot and ankle problems account for significant percentage of visits to physicians every year, particularly primary care physicians, orthopedic surgeons, and podiatrists. The cost of treating these problems is no doubt an economic strain on all of us (1, 2).
The equinus or isolated gastrocnemius contracture deformity referred to herein is of the non-neuromuscular/non-paralytic type in otherwise healthy individuals. This is why it is often referred to as subtle or silent.
There has been an increasing amount of literature in the last several decades suggesting a link between equinus and many foot and ankle conditions (1, 3–53). Despite this association, little if any evidence concentrating on a mechanism of how the tight calf might actually produce problems in the foot and ankle (3, 4, 11, 15, 18, 31, 32, 44, 54–56).
While we are busy discovering the cause and effect associations between equinus and certain foot and ankle conditions, there has been little interest in determining or explaining how equinus might actually cause damage to the foot and ankle. Two authors have indeed shed light on the cause and effect that equinus exerts on the human foot and ankle. In 1913, Nutt (57) shed considerable light on this subject only to be lost until now. In 2014, Cazeau and Stiglitz (14) described causality to some extent as equinus relates to increased forefoot pressures describing the critical area of the gait cycle as the C-zone when the ankle dorsiflexion is less than 5° and the maximal point of forefoot pressure as the X point and just after.
The incidence of non-neuromuscular equinus in otherwise normal, healthy people (5, 11, 13, 14, 18, 23, 25, 57–59) is not known; however, it is likely far more common than currently perceived. While most would consider a calf that is too tight to be trivial, this could not be further from the truth. The long-term strain produced by equinus, which is usually silent, ultimately leads to progressive, incremental damage in the foot and ankle until it finally becomes symptomatic. Directing treatment toward the most obvious problem, the presenting foot or ankle condition, has traditionally been the main, if not the only, objective; however, emerging data will hopefully point us in a different direction, i.e., the correct direction.
The purpose of this paper is to describe the exact mechanism, the split second effect, by which a seemingly innocuous, subtle equinus contracture causes so much cumulative damage and deformity in the human foot and ankle over time as we age.
The source of the isolated gastrocnemius contracture or equinus has recently been recently addressed by this author (5). The four common categories described in this article: activity changes, physiologic changes in muscles and tendons, genetics, and reverse evolution. An additional fifth source of the acquired isolated gastrocnemius contracture is discussed here in Appendix B.
Finally, considering this knowledge, I assert, if not challenge, that the calf is the singular source of the majority of acquired, non-traumatic adult foot and ankle problems, such as plantar fasciitis, non-traumatic midfoot osteoarthritis, diabetic Charcot arthropathy, insertional Achilles tendinosis, and Achilles tendinitis (Appendix A).
The Perfect Human Foot
To understand the forces projected upon the human foot and ankle by an isolated gastrocnemius contracture, one must first understand the “perfect foot” (5). The perfect foot, from a mechanical and theoretical standpoint, is the foot that evolution left behind long ago, as humans moved away from being quadrupeds. In understanding the structure of the perfect foot, we are better able to understand, by contrast, the damaging forces equinus places upon the two imperfect feet that we have been entrusted.
Structurally speaking, the equinus foot of a horse or dog is better suited for wear and abuse than the human foot, especially for the long haul. It would be correct to argue that this might be the case because quadrupeds ambulate on four legs distributing the weight on four instead of two feet. However, when considering the foot as a biomechanical structure unto itself and the forces humans put on each of theirs through every day, it is apparent that the construction of the quadruped foot is much more suited for the task required.
Of course, the weight-bearing platform of an equinus foot is too small for prolonged maintenance of a bipedal gait, considering balance and ground force distribution. So, the human foot wisely evolved and rotated upward through the ankle joint about 70° to permanently place the heel on the ground (Figure 1). This adaptation provided a much larger plantar surface area for improved force distribution, balance, and necessary leverage for bipedal locomotion. However, this new foot position placed the human foot in a biomechanically disadvantaged position due to the leveraged forces placed upon it by ground reaction forces.
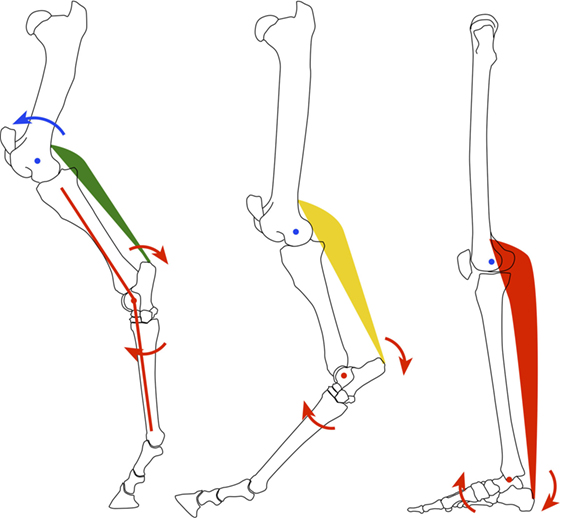
Figure 1. Diagrammatic representation of the evolution of the equine quadruped (left) to human biped (right).
With weight bearing, the human foot is oriented such that forces shift from a vertical, mostly compressive load (perfect equinus foot) to leveraged/bending or vector forces resulting in higher compressive (dorsal foot, anterior ankle) and tensile forces (plantar foot, posterior ankle). Understanding the difference between the quadruped, equinus foot and the biped, plantigrade foot is critical to understand the damaging effects of equinus and thus the split second effect.
Basic Human Gait
Human gait, or the act of bipedal walking, is divided into two basic periods: stance and swing. During the stance phase of gait, the foot is on the ground. The stance phase is divided into five parts: initial contact, loading response, mid-stance, terminal stance, and pre-swing. Furthermore, Perry (60), in her classic book, Gait Analysis: Normal and Abnormal Function, looks at the center of stance phase of gait as “progression over the supporting foot,” divided into the heel rocker, the ankle rocker, and the forefoot rocker. For ease of use, the purpose of this theory, and particularly for future discussion applying additional rockers, these rockers will be renamed R1 (heel), R2 (ankle), and R3 (forefoot). The ankle rocker, or R2, is the critical time during gait when the split second effect occurs.
Once the forefoot has fully contacted the ground, R1 is completed and R3 has yet to occur. The body weight is now fully on the stance foot and R2 is engaged as the tibia rotates forward to carry the passenger (body) forward over the ankle joint. In order for humans to progress forward using our unique bipedal gait pattern, the passenger must and will move forward over the planted or stance foot. If the gait is to remain smooth and proceed normally, the calf must have enough flexibility to allow the tibia to adequately rotate over the talus in synchrony with the body above, yet have enough strength to eccentrically control the deceleration at the end of R2. In order for unimpeded completion of R2, the tibia must be allowed to rotate forward upon the ankle or dorsiflex fully. In the normal state, the calf lengthens enough to allow the necessary ankle rotation producing a smooth transition reducing bending vector forces onto the foot and ankle at the end of R2.
The Split Second Effect
The split second effect is a theory describing how an equinus contracture mechanically damages the human lower leg, ankle, and foot.
There are two types of forces created by the split second effect. Direct tension forces are more obvious, occurring at the gastrocnemius muscle, musculotendinous junction, the Achilles tendon, the Achilles insertion at the calcaneus, the calcaneus, and finally the plantar fascia. Indirect forces are leveraged upon the foot and ankle and the more esoteric component of this theory.
If the calf becomes too tight, thus limiting its ultimate available length, the rotation of the ankle (R2) is hindered and stopped too early. Yet, the body continues to progress forward over the planted foot, which will produce increased leveraged forces in the foot and ankle. Of course, the ground reaction forces are unavoidable and provide the balance of this equation. The tighter the calf becomes, the higher and earlier the leveraged forces that result.
Early on, these forces generally are not visibly evident as pathologic motion in the foot, and they are undetectable, but the magnified forces are there nonetheless. In other words, the effect is invisible to the casual observer, likely the trained observer, as well as to the person with the tight calves. All the while, the silent, unknown equinus contracture, even in early stages, creates incremental exaggerated leveraged or bending forces upon the tension and compression sides of the foot and ankle. In time, these repetitive forces take their toll, especially as the isolated gastrocnemius contracture increases.
The split second effect describes a critical 120 ms span of time during terminal midstance (R2), just before the heel lifts off the ground, where damaging forces are produced along the whole tension chain, both direct and indirect. These forces are created and magnified by the equinus contracture impeding the forward progress of the tibia or passenger over the ankle. The indirect leveraged forces are exponentially magnified, creating abnormal, pathologic bending or vector stress to the foot and ankle, thus resulting in stress and strain to the joints and supporting ligaments and tendons in a variety of ways ultimately creating an array of non-traumatic acquired foot and ankle pathology (Appendix A).
When we are younger, a normal length gastrocnemius allows the necessary ankle dorsiflexion and smoother near-end-point deceleration as the ankle progresses forward late in R2 just before R3 begins. The ultimate length of the gastrosoleus complex is likely not reached, and the end transition forces are dampened by the compulsory contracture of both the gastrocnemius and soleus (and less end point tension) gradually producing a softer end point. There is room to spare when it comes to the amount of gastrocsoleus complex length that is necessary. This creates an easier, more cushioned force transfer upon the foot and ankle below. However, even when the calf is supple and the ankle has “adequate” dorsiflexion, there is still a transfer of progressive leveraged stress to the foot and ankle even under the most “normal” of conditions. This is the burden we as humans must bear in order to have a bipedal gait.
The split second effect is divided into two separate mechanical components: ankle dorsiflexion and knee extension.
Ankle Dorsiflexion Component
The last half of midstance, R2, is exactly where the split second effect occurs. It begins when the swing phase foot starts to pass by the stance phase foot and ends just as the stance heel lifts from the ground to the earliest part of R3. For most of us, walking at a normal pace, this usually lasts about 120 ms, or just over 1/10th of a second. This timing was derived from video at 250 frames per second (FPS) and limited motion analysis. Figure 2 is a 57-year-old individual with a history of plantar fasciitis on the right and no history of foot or ankle problems on the left. At test time, the plantar fasciitis is asymptomatic. Frame C to D is when the split second effect occurs and ankle dorsiflexion fails to progress. This occurs at approximately 28–45% of the gait cycle.
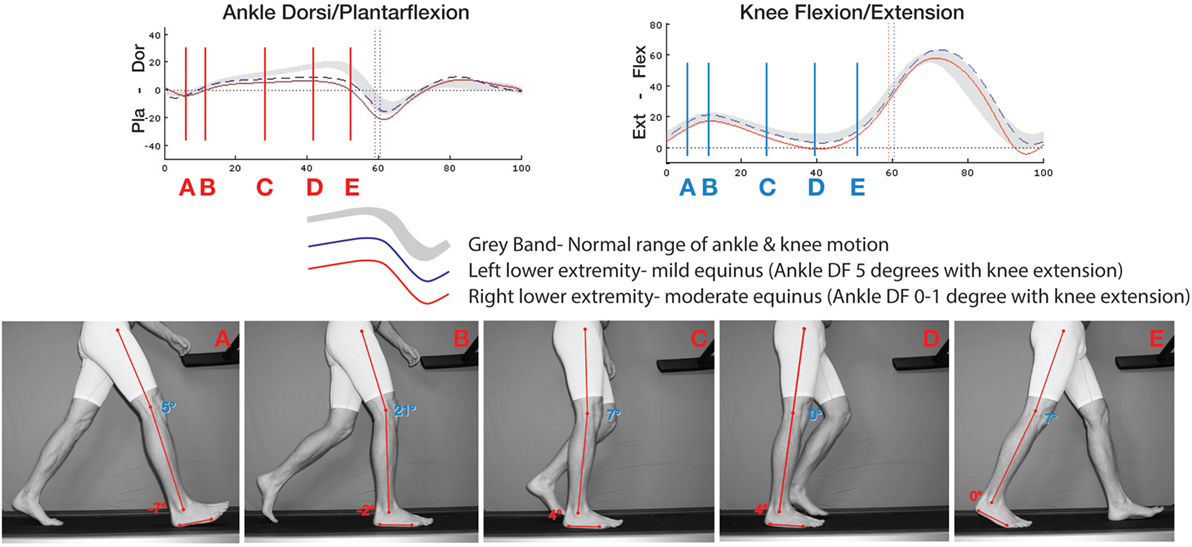
Figure 2. Motion analysis compared to same subject on treadmill shot at 250 FPS of subject with bilateral equinus and history right plantar fasciitis who is asymptomatic at time of testing. At 28–45%, frames C–D depict the timing of the split second effect. There is accentuated knee extension and a failure of ankle dorsiflexion. This lack of normal ankle dorsiflexion motion gives rise to leveraged forces upon the foot and ankle.
With equinus, the leveraged forces transmitted to the foot and ankle during this split second become exponentially worse as the gastrocnemius prematurely reaches its endpoint. The tighter the calf, the sooner and more abrupt the endpoint is reached. This in turn makes the foot and ankle directed forces higher, peak faster, and last longer. These forces can of course be mitigated by the characteristic compensatory “start up” gait alteration such as seen in plantar fasciitis and many other related problems. The start-up limp creates the characteristic gait that compensates for an even tighter gastrocnemius created by rest and lack of calf tension created by the Law of Davis (57). Just as the higher tension is reached, R2 is not completed, and the tibia does not complete its rotation over the talus. It is only after this temporary additional contracture is slightly re-lengthened by walking does the gait return to “normal,” at least as perceived by the patient.
Over time, and as a result of taking thousands of steps per day, the foot and ankle succumb to an occult, unrecognized “overuse of imbalance,” which ultimately leads to damage. This damage can create defined pathology, such as plantar fasciitis, midfoot arthritis, insertional Achilles tendonosis (Haglund’s deformity), and posterior tibialis tendon dysfunction, to name just a few (appendix A).
Knee Extension Component
In the course of looking through hours of slow motion video of many different people walking, both normal and pathologic, a second consistent component critical to the split second effect was noticed. It was observed that, at the exact same time, the ankle was prematurely ceasing to rotate due to the isolated gastrocnemius contracture, the ipsilateral knee abruptly comes to terminal extension or straightens out fully. This might seem unimportant until one considers that the gastrocnemius crosses three joints: the subtalar joint (negligible in this model except for posterior tibialis dysfunction), the ankle, and the knee. With this simultaneous knee extension, the gastrocnemius is pulled even tighter at just the wrong time, when the ankle has ceased to progress forward and ankle dorsiflexion has stopped. This knee extension produces two perfectly timed and simultaneous opposing forces, both of which only increases the direct tension force and indirect leveraged force placed on the foot and ankle below, by causing a further abrupt tension.
In the case of where equinus is present, there is likely an associated increased knee extension or even knee hyperextension occurs secondary to the restricted ankle dorsiflexion. Note in Figure 2 how both knees extend outside the normal gray band and the right (plantar fasciitis side) knee extends fully to 0°.
To be perfectly clear, the ankle dorsiflexion or R2 is distally halted by the calf contracture too early, while the knee abruptly straightens to full extension pulling a now inflexible, tensioned calf even tighter over a very short period of time. The result is the tension in the calf exponentially rises over a split second creating indirect damaging compressive and tensile forces onto the foot and ankle, direct tensile forces along the posterior/plantar tension chain, and likely the knee as well. It would be like two people with the same rope tied around each other’s waists running away from each other in opposite directions until they reach the end of the line. Twice the force in half the time: a split second.
There is a second damaging mechanical force produced by the knee extending at this time adding to the amount of tension produced. The short arc Class II lever at the extending knee (fulcrum) produces high tensile forces through the calf because the fulcrum is short (distance from axis of knee motion to insertion of gastrocnemius) compared to the long lever of the femur (the lever). This is the finishing blow, so to speak, producing a very high tensile, leveraged force over a very short time (Figure 3).
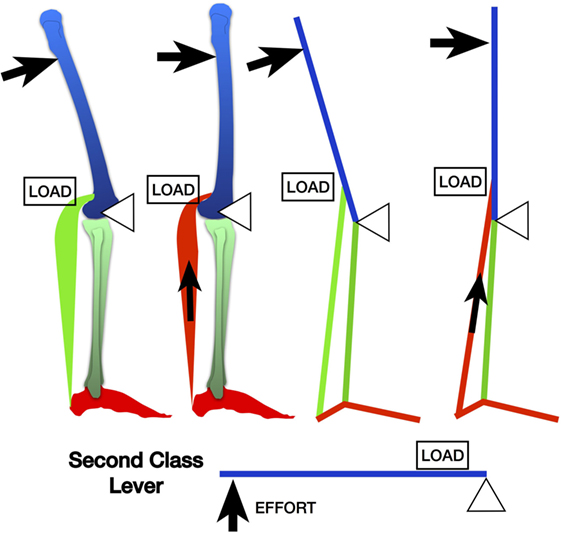
Figure 3. The leveraged forces produced from terminal knee extension during the split second effect via the gastrocnemius by a second class lever mechanism.
Clinical Example: The Split Second Effect and Midfoot Strain
Examples of direct tension forces are simple and easy to comprehend. Too much tension produced by the split second effect anywhere along the posterior/plantar tension chain can cause damage producing the likes of insertional Achilles tendinosis or plantar fasciitis, for example.
As a clinical example of the more elusive indirect forces produced, one of the many areas of stress placed onto the foot due to the split second effect is at the midfoot, defined here as R4. Because the ankle rotation (R2) is reduced or stopped, either the gait adapts with early heel raise or the foot starts to create a “new ankle” or point of rotation, R4. In a normal foot setting, the stresses thrust upon the midfoot cannot actually be seen per se; however, this abnormal motion is well illustrated in this asymptomatic 23-year-old with congenital flexible flatfeet (Figure 4).
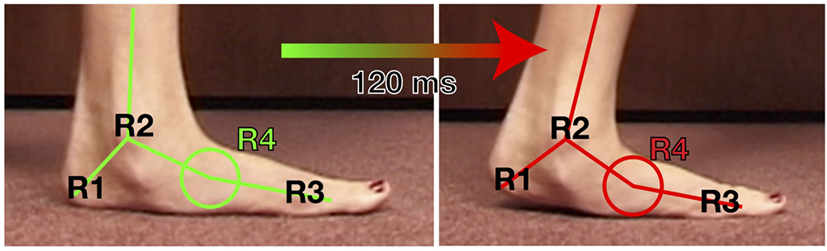
Figure 4. Video still capture from video shot at 250 FPS of a 23-year-old asymptomatic female with painless flexible flatfeet. This visibly exhibits the motion transfer from the ankle (R2) to the midfoot/transverse tarsal joint (R4) when there is equinus. If this flexibility at R4 seen here visibly is not present, such as a normal, less flexible midfoot, the motion is replaced by leveraged forces to the midfoot joints or to the posterior tibialis tendon/spring ligament at the transverse tarsal joint.
Two very common problems we see, non-traumatic midfoot arthritis (4, 9, 13, 18, 61) and Brodsky type 1 and 2 Charcot arthropathy (4, 13, 18, 20, 29, 42), do not just appear by magic. There is no doubt that both of these very common deformities result in part, if not completely from inevitable calf contractures, mediated by the split second effect and R4 bending forces through the midfoot (Figure 4).
An equinus contracture, with associated hamstring contractures (12) and the split second effect could possibly have implications upon the knee and idiopathic knee osteoarthritis. Additionally, this all compounds up the chain right to the hips and back. However, the purpose here is to look at the effect on the foot and ankle.
Discussion
Evidence of the association between the isolated gastrocnemius contracture or equinus and the majority of non-traumatic acquired foot and ankle pathology abounds (1, 3–53). We are awakening to a new era of understanding the mechanics and function of the human foot and ankle. There is a simple, singular, usually silent, and remote cause for the majority of non-traumatic acquired foot and ankle pathology, and mechanically, it creates cumulative damage to the foot and ankle through leveraged forces. In short and in this author’s opinion, equinus is the primary mechanical common denominator that leads to the majority of acquired non-traumatic foot and ankle problems by indirect leveraged means as well as direct forces along the posterior/plantar chain. There can be no more room for the standard thinking that these resultant foot and ankle problems arise just because we are getting older or we are obese or they are just random, or that an equinus contracture is only a part of the equation. Equinus is the equation.
These non-traumatic acquired foot and ankle problems are mechanical in nature, an “overuse syndrome of mechanical imbalance” of sorts, and the end result is a chronic inflammatory process. As a result, traditional non-operative treatment generally fails because it is misdirected at the obvious problem, the foot and ankle inflammatory issue. Treating the resulting inflammatory process can no doubt temporarily alleviate symptoms; however, it is still at best palliative and fails to treat the underlying cause. No wonder mentions and anecdotal evidence pointing out the failure of conservative treatment of these resulting problems [Appendix A] dominates in our literature (11, 21, 23, 62–64).
Why is there such a resistance to the possibility that an equinus contracture is central to so many foot and ankle problems as we age? Much of our literature can certainly be interpreted as doubtful if not ignoring it altogether. Most importantly, the methods of foot and ankle care and treatment probably unlike any other sector of medicine are fueled by urban myth, conflicting research, quick fix society, and a medical industry concerned with palliative-directed treatment.
The concept of the subtle, non-neuromuscular acquired equinus contracture is not new. Nutt (57) described “Shaffer’s foot” over 100 years ago. He stated, “…this condition is a shortening of the gastrocnemius and of the soleus. This shortening is not enough to produce the deformity of equinous but limits [ankle] dorsal flexion.” In this forgotten, but landmark 1913 book Diseases and Deformities of the Foot, Nutt described the abnormal stresses place upon the foot by the contracted gastrocnemius.
In 1995, Hill (23) stated “equinus reflects ‘acquired deformity’ related to factors of lifestyle that leave the posterior muscles at a physiologic disadvantage toward maintaining flexibility.” Furthermore, he went on to state, “Gastrosoleal stretching is an important treatment modality that can lead to a higher success rate of conservative treatment. It can decrease the need for foot surgery, and significantly reduce the number of failed or serial surgical procedures.”
In 2002, DiGiovanni et al. (18) coined the term “isolated gastrocnemius contracture” and rekindled the idea of the gastrocnemius producing foot and ankle pathology with out any proposed mechanism. The sheer importance of this seminal article has been mostly overlooked by the great majority of the orthopedic and podiatric community, even today. They stated, “Our experience has suggested that the gastrocnemius muscle in particular is the predominant deforming force in people with structural breakdown or chronic pathological changes related to the foot and ankle. We suspect that contracture of this muscle is not only common but often partially responsible for many of the chronic forefoot and midfoot symptoms identified in non-neurologically impaired patients.”
I would disagree with two critical assumptions they made. First, I would disagree with their comment “We suspect that contracture of this muscle is not only common but often partially responsible for many of the chronic forefoot and midfoot symptoms identified in non-neurologically impaired patients.” I believe that the contribution of the isolated gastrocnemius contracture is the singular cause of the many associated pathological conditions described in the literature, and is partially responsible much less often. These authors also stated, “We further postulated that the difference would be present whether the knee was extended or flexed.” It is my hypothesis that the previously unknown simultaneous extension of the knee is critical to the synergistic damage delivered to the foot and ankle by the isolated gastrocnemius contracture and is described here as the split second effect.
In 2002, Porter et al. (56) reported on isolated calf stretching for plantar fasciitis demonstrating a measurable and excellent improvement in ankle dorsiflexion and pain relief. The dorsiflexion gained over 4 months went from average ankle dorsiflexion of 5.1–13.5°. Foot and ankle scores (pain relief) improved on average 56–90%. They stated “The increase in flexibility correlated with a decrease in foot and ankle pain, and an increase in foot and ankle function. This correlation should be emphasized to physicians and patients alike.”
Cazeau and Stiglitz (14) provided additional insight into this biomechanical aberration describing the mechanism of equinus leading to increased forces placed upon the forefoot. They termed this timing of forefoot overload resulting from equinus as the “C-zone,” defining it as “the lack of EMG activity points out the passive nature of gastrocnemius stretching.” They also described the “X point” in the middle of the C-zone as the point the gastrocnemius reaches its maximal stretching and just after. While no force plate analysis was provided, it can be safely assumed that the forefoot pressures increase significantly at the X point. Their work endorsed addressing the calf, but by surgical lengthening and characteristically denounced calf stretching as minimally effective stating, “various clinical presentations and pathologies are described in which stretching as a single treatment is probably insufficient.” While more work appears to be necessary, the evidence would disagree with the ongoing inference that calf stretching is generally ineffective (12, 23, 56, 59, 65).
In the last two decades, the evidence has been mounting supporting that the gastrocnemius is associated with many foot and ankle problems, but little, if any, reason as to the cause and effect has been offered until now. The split second effect concept is like a key to open the lock few even knew existed; here is the problem explained simply. No doubt many more studies will and should emerge to both qualify and quantify equinus and its role on the demise of the human foot and ankle. It is likely that high resolution, ultra high-speed gait lab motion analysis coupled with force plate analysis should and will show this theory to be correct, as well as provide more defined details.
Misperception and conventional wisdom has pervaded our literature in regard to etiology of the majority of non-traumatic acquired foot and ankle pathology. Much of the current thought and evidence on the epidemiology of these non-traumatic acquired foot and ankle pathologies is by association and subjective (3, 29, 33, 44, 55). The generally accepted factors cited in the literature and on the internet, such as obesity, sedentary life style, medical co-morbidities, shoe wear, concrete floors, overuse, etc., likely have a common pathway to these associated foot and ankle problems via an equinus contracture. In other words, these factors, while they may indeed be commonly present, contribute minimally if at all in a direct manner to the resulting problems or pathology in the foot and ankle. Each of these factors at best creates an additional accelerated avenue to equinus, which in turn causes the foot and ankle pathology by way of the split second effect.
For instance, it is more or less thought by many that the acquired flatfoot deformity is somehow a random, unknown problem or due to obesity and that calf contractures might come about secondarily. In this scenario, acquired equinus might at most be considered to only contribute to an acquired flatfoot deformity usually after the fact (22). The studies done commenting on the epidemiology of this problem, as well as many other foot problems, point to other collateral or associated factors noted above and that is where they stop. The calf contracture indeed worsens as the flatfoot deformity progresses via vicious cycle, but it is still likely the inciting underlying cause.
The singular and real cause of these problems is a contracture of the gastrocnemius muscle, which is camouflaged in this large list of collateral, minimally contributory risk factors. Every other factor cited as a cause of foot and ankle problems is mediated by contributing to the degree and/or rate of an already contracting human gastrocnemius (5). In other words, these co-morbidities promote gastrocnemius tightness, which in time causes incremental damage to the foot and/or ankle. This concept cannot be overstated or we will continue to aim our treatment efforts at the wrong target.
To put it very frankly, obese people have calf lengthening and resolve their recalcitrant Achilles tendinosis and yet they are still overweight. Employees who work on concrete have a calf lengthening procedure, resolve their midfoot arthritis pain, and return to work pain free on the concrete. A runner with plantar fasciitis definitively stretches their calves and moves on, pain free back to running.
There are still questions that must be answered. Is calf stretching effective? The evidence seems to support it, yet as a definitive treatment, it is very poorly embraced and the current momentum in this area is unfortunately toward surgical lengthening. Poor compliance with calf stretching would certainly lead to failure as seen in so many areas of medical care (66–68). More importantly, can gastrocnemius stretching be preventative? While there is little if any evidence to support this, further work in this area would be prudent.
Certainly, not everyone will develop significant damage producing isolated gastrocnemius contracture in their lifetime. What is the incidence of equinus? And who is prone to develop it and can we identify them and apply preventative stretching before pathology develops? Are there recognizable subtle gait variances that produce equinus?
Certainly, in most cases, equinus develops bilaterally and approximately equally. Then why are resulting problems often present on just one side or the other? One very tangible and very common cause of unilateral equinus is one limb that is left fallow for a period of time due to injury, or elective limb surgery, or recovery from a total knee only to develop plantar fasciitis in the ensuing months.
Given that we as a culture finally embrace subtle equinus as a significant problem, should we stretch calves or have them surgically lengthened? What guidelines for stretching versus surgically lengthening might there be developed? The current guidelines for considering surgery after 6 months of failed non-operative treatment is likely incorrect. The 6-month time frame is adequate; however, what defines the failed non-operative treatment? Traditionally speaking as well as today, non-operative treatment for these issues includes a random inconsistent mixture of palliative conservative measures directed at the obvious Achilles, foot or ankle problem and does not address the equinus (23). Certainly, the current trend is toward surgical correction of which this author disagrees.
Conclusion
It appears that merely being human places us at risk of developing acquired non-traumatic foot and ankle problems. This damage is mediated through our unique anatomy and the gastrocnemius that tightens for a number of reasons (5). The split second effect explains exactly how a silent equinus contracture, that seemingly has little to do with the foot and ankle below, can gradually cause significant harm when left undetected and unattended.
The isolated gastrocnemius contracture must be addressed as the definitive treatment for many if not the majority of non-traumatic acquired foot and ankle pathology (Appendix A). While treating the obvious foot or ankle problem is advisable and can be of great benefit to the patient, it must be considered only as adjunctive and palliative.
This crucial concept must be vetted and passed on to as many people as possible and as fast as possible. We have already waited over a century since first described by Nutt (57); let us not wait too much longer. Better yet, going forward, we must promote prevention in the form of proactive daily calf stretching before the damage occurs.
Author Contributions
This article in its entirety considering originality, views, concept form, authorship and future communication is the sole responsibility of JA, MD.
Conflict of Interest Statement
The author declares a potential conflict of interest with respect to the publication of this article and the One Stretch®, but not to this original research or authorship.
The reviewer, KO, and handling Editor declared their shared affiliation, and the handling Editor states that the process nevertheless met the standards of a fair and objective review.
References
1. Patel A, DiGiovanni B. Association between plantar fasciitis and isolated contracture of the gastrocnemius. Foot Ankle Int (2011) 32:5–8. doi: 10.3113/FAI.2011.0005
2. Tong KB, Furia J. Economic burden of plantar fasciitis treatment in the United States. Am J Orthop (Belle Mead NJ) (2010) 39:227–31. doi:10.1185/030079907X199790
3. Abbassian A, Kohls-Gatzoulis J, Solan MC. Proximal medial gastrocnemius release in the treatment of recalcitrant plantar fasciitis. Foot Ankle Int (2012) 33:14–9. doi:10.3113/FAI.2012.0014
4. Abdulmassih S, Phisitkul P, Femino JE, Amendola A. Triceps surae contracture: implications for foot and ankle surgery. J Am Acad Orthop Surg (2013) 21:398–407. doi:10.5435/JAAOS-21-07-398
5. Amis J. The gastrocnemius: a new paradigm for the human foot and ankle. Foot Ankle Clin (2014) 19:637–47. doi:10.1016/j.fcl.2014.08.001
6. Anderson JG, Bohay DR, Eller EB, Witt BL. Gastrocnemius recession. Foot Ankle Clin (2014) 19:767–86. doi:10.1016/j.fcl.2014.09.001
7. Armstrong DG, Stacpoole-Shea S, Nguyen H, Harkless LB. Lengthening of the Achilles tendon in diabetic patients who are at high risk for ulceration of the foot. J Bone Joint Surg Am (1999) 81:535–8.
8. Aronow MS, Diaz-Doran V, Sullivan RJ, Adams DJ. The effect of triceps surae contracture force on plantar foot pressure distribution. Foot Ankle Int (2006) 27:43–52.
9. Aronow M. Triceps surae contractures associated with posterior tibial tendon dysfunction. Tech Orthop (2000) 15:164–73. doi:10.1097/00013611-200015030-00002
10. Barouk LS. The effect of gastrocnemius tightness on the pathogenesis of juvenile hallux valgus: a preliminary study. Foot Ankle Clin (2014) 19:807–22. doi:10.1016/j.fcl.2014.08.005
11. Barske HL, DiGiovanni BF, Douglass M, Nawoczenski DA. Current concepts review: isolated gastrocnemius contracture and gastrocnemius recession. Foot Ankle Int (2012) 33:915–21. doi:10.3113/FAI.2012.0915
12. Bolívar YA, Munuera PV, Padillo JP. Relationship between tightness of the posterior muscles of the lower limb and plantar fasciitis. Foot Ankle Int (2013) 34:42–8. doi:10.1177/1071100712459173
13. Bowers AL, Castro MD. The mechanics behind the image: foot and ankle pathology associated with gastrocnemius contracture. Semin Musculoskelet Radiol (2007) 11:83–90. doi:10.1055/s-2007-984418
14. Cazeau C, Stiglitz Y. Effects of gastrocnemius tightness on forefoot during gait. Foot Ankle Clin (2014) 19:649–57. doi:10.1016/j.fcl.2014.08.003
15. Chen WM, Park J, Park SB, Shim VPW, Lee T. Role of gastrocnemius-soleus muscle in forefoot force transmission at heel rise – a 3D finite element analysis. J Biomech (2012) 45:1783–9. doi:10.1016/j.jbiomech.2012.04.024
16. Crawford F, Thomson C. Interventions for treating plantar heel pain. Cochrane Database Syst Rev (2003) 3:CD000416.
17. Cychosz CC, Phisitkul P, Belatti DA, Glazebrook MA, DiGiovanni CW. Gastrocnemius recession for foot and ankle conditions in adults: Evidence-based recommendations. Foot Ankle Surg (2015) 21:77–85. doi:10.1016/j.fas.2015.06.001
18. DiGiovanni CW, Kuo R, Tejwani N, Price R, Hansen ST Jr, Cziernecki J, et al. Isolated gastrocnemius tightness. J Bone Joint Surg (2002) 84:962–70.
19. DiGiovanni CW, Langer P. The role of isolated gastrocnemius and combined Achilles contractures in the flatfoot. Foot Ankle Clin (2007) 12:363–79. doi:10.1016/j.fcl.2007.03.005
20. Frykberg RG, Bowen J, Hall J, Tallis A, Tierney E, Freeman D. Prevalence of equinus in diabetic versus nondiabetic patients. J Am Podiatr Med Assoc (2012) 102:84–8. doi:10.7547/1020084
21. Gentchos CE, Bohay DR, Anderson JG. Gastrocnemius recession as treatment for refractory achilles tendinopathy: a case report. Foot Ankle Int (2008) 29:620–3. doi:10.3113/FAI.2008.0620
22. Harris RI, Beath T. Hypermobile flat-foot with short tendo achillis. J Bone Joint Surg (1948) 30:116–50.
23. Hill RS. Ankle equinus. prevalence and linkage to common foot pathology. J Am Podiatr Med Assoc (1995) 85:295–300. doi:10.7547/87507315-85-6-295
24. Hoke M. An operation for the correction of extremely relaxed flat feet. J Bone Joint Surg (1931) 13:773–83.
25. Johnson E, Bradley B, Witkowski K, McKee R, Telesmanic C, Chavez A, et al. Effect of a static calf muscle-tendon unit stretching program on ankle dorsiflexion range of motion of older women. J Geriatr Phys Ther (2007) 30:49–52. doi:10.1519/00139143-200708000-00003
26. Kibler WB, Goldberg C, Chandler TJ. Functional biomechanical deficits in running athletes with plantar fasciitis. Am J Sports Med (1991) 19:66–71. doi:10.1177/036354659101900111
27. Kiewiet NJ, Holthusen SM, Bohay DR, Anderson JG. Gastrocnemius recession for chronic noninsertional Achilles tendinopathy. Foot Ankle Int (2013) 34:481–5. doi:10.1177/1071100713477620
28. Laborde JM. Bilateral proximal fifth metatarsal nonunion treated with gastrocnemius-soleus recession. JBJS Case Connect (2013) 3:e68. doi:10.2106/JBJS.CC.M.00021
29. Lavery LA, Armstrong DG, Boulton AJM, Diabetex Research Group. Ankle equinus deformity and its relationship to high plantar pressure in a large population with diabetes mellitus. J Am Podiatr Med Assoc (2002) 92:479–82. doi:10.7547/87507315-92-9-479
30. Lin SS, Lee TH, Wapner KL. Plantar forefoot ulceration with equinus deformity of the ankle in diabetic patients: the effect of tendo-Achilles lengthening and total contact casting. Orthopedics (1996) 19:465–75.
31. Maceira E, Monteagudo M. Functional hallux rigidus and the Achilles-calcaneus-plantar system. Foot Ankle Clin (2014) 19:669–99. doi:10.1016/j.fcl.2014.08.006
32. Macklin K, Healy A, Chockalingam N. The effect of calf muscle stretching exercises on ankle joint dorsiflexion and dynamic foot pressures, force and related temporal parameters. Foot (Edinb) (2012) 22:10–7. doi:10.1016/j.foot.2011.09.001
33. Martin RL, Irrgang JJ, Conti SF. Outcome study of subjects with insertional plantar fasciitis. Foot Ankle Int (1998) 19:803–11. doi:10.1177/107110079801901203
34. Maskill JD, Bohay DR, Anderson JG. Gastrocnemius recession to treat isolated foot pain. Foot Ankle Int (2010) 31:19–23. doi:10.3113/FAI.2010.0019
35. McGlamry ED, Kitting RW. Aquinus foot. An analysis of the etiology, pathology and treatment techniques. J Am Podiatry Assoc (1973) 63:165–84. doi:10.7547/87507315-63-5-165
36. Monteagudo M, Maceira E, Garcia-Virto V, Canosa R. Chronic plantar fasciitis: plantar fasciotomy versus gastrocnemius recession. Int Orthop (2013) 37:1845–50. doi:10.1007/s00264-013-2022-2
37. Norregaard J, Larsen CC, Bieler T, Langberg H. Eccentric exercise in treatment of Achilles tendinopathy. Scand J Med Sci Sports (2007) 17:133–8.
38. Park DY, Rubenson J, Carr A, Mattson J, Besier T, Chou LB. Influence of stretching and warm-up on Achilles tendon material properties. Foot Ankle Int (2011) 32:407–13. doi:10.3113/FAI.2011.0407
39. Pascual-Huerta J. The effect of the gastrocnemius on the plantar fascia. Foot Ankle Clin (2014) 19:701–18. doi:10.1016/j.fcl.2014.08.011
40. Pratt K, Bohannon R. Effects of a 3-minute standing stretch on ankle-dorsiflexion range of motion. J Sport Rehabil (2003) 12:162–73.
41. Radford JA, Burns J, Buchbinder R, Landorf KB, Cook C. Does stretching increase ankle dorsiflexion range of motion? A systematic review. Br J Sports Med (2006) 40:870–5. doi:10.1136/bjsm.2006.029348
42. Rao SR, Saltzman CL, Wilken J, Yak J. Increased passive ankle stiffness and reduced dorsiflexion range of motion in individuals with diabetes mellitus. Foot Ankle Int (2006) 27:617–22.
43. Reimers J, Pedersen B, Brodersen A. Foot deformity and the length of the triceps surae in Danish children between 3 and 17 years old. J Pediatr Orthop B (1995) 4:71–3. doi:10.1097/01202412-199504010-00011
44. Riddle DL, Pulisic M, Pidcoe P, Johnson RE. Risk factors for plantar fasciitis: a matched case-control study. J Bone Joint Surg (2003) 85:872–7.
45. Roos EM, Engstrom M, Lagerquist A, Soderberg B. Clinical improvement after 6 weeks of eccentric exercise in patients with mid-portion Achilles tendinopathy – a randomized trial with 1-year follow-up. Scand J Med Sci Sports (2004) 14:286–95. doi:10.1111/j.1600-0838.2004.378.x
46. Sgarlato TE, Morgan J, Shane HS, Frenkenberg A. Tendo achillis lengthening and its effect on foot disorders. J Am Podiatry Assoc (1975) 65:849–71. doi:10.7547/87507315-65-9-849
47. Solan MC, Carne A, Davies MS. Gastrocnemius shortening and heel pain. Foot Ankle Clin (2014) 19:719–38. doi:10.1016/j.fcl.2014.08.010
48. Subotnick SI. Equinus deformity as it affects the forefoot. J Am Podiatry Assoc (1971) 61:423–7. doi:10.7547/87507315-61-11-423
49. Szames SE, Forman WM, Oster J, Eleff JC, Woodward P. Sever’s disease and its relationship to equinus: a statistical analysis. Clin Podiatr Med Surg (1990) 7:377–84.
50. Tabrizi P, McIntyre WM, Quesnel MB, Howard AW. Limited dorsiflexion predisposes to injuries of the ankle in children. J Bone Joint Surg Br (2000) 82:1103–6. doi:10.1302/0301-620X.82B8.10134
51. Verrall G, Schofield S, Brustad T. Chronic Achilles tendinopathy treated with eccentric stretching program. Foot Ankle Int (2011) 32:843–9. doi:10.3113/FAI.2011.0843
52. Wapner KL, Sharkey PF. The use of night splints for treatment of recalcitrant plantar fasciitis. Foot Ankle Int (1991) 12:135–7. doi:10.1177/107110079101200301
53. Zimny S, Schatz H, Pfohl M. The role of limited joint mobility in diabetic patients with an at-risk foot. Diabetes Care (2004) 27:942–6. doi:10.2337/diacare.27.4.942
54. Duthon VB, Lubbeke A, Duc SR, Stern R, Assal M. Noninsertional Achilles tendinopathy treated with gastrocnemius lengthening. Foot Ankle Int (2011) 32:375–9. doi:10.3113/FAI.2011.0375
55. Klein SE, Dale AM, Hayes MH, Johnson JE, McCormick JJ, Racette BA. Clinical presentation and self-reported patterns of pain and function in patients with plantar heel pain. Foot Ankle Int (2012) 33:693–8. doi:10.3113/FAI.2012.0693
56. Porter D, Barrill E, Oneacre K, May BD. The effects of duration and frequency of achilles tendon stretching on dorsiflexion and outcome in painful heel syndrome: a randomized, blinded, control study. Foot Ankle Int (2002) 7:619–24. doi:10.1177/107110070202300706
57. Nutt J. Diseases and Deformities of the Foot (E. B. Treat & Co.). Google Digital Copy (1913). Available from: http://books.google.com/books?id=UWgQAAAAYAAJ
58. Silfverskiöld N. Reduction of the uncrossed two-joints muscles of the leg to one-joint muscles in spastic conditions. Acta Chir Scand (1924) 56:315–30.
59. Gajdosik R, Vander Linden D, McNair P, Williams A, Riggin T. Effects of an eight-week stretching program on the passive-elastic properties and function of the calf muscles of older women. Clin Biomech (Bristol, Avon) (2005) 20:973–83. doi:10.1016/j.clinbiomech.2005.05.011
60. Perry J. Gait Analysis: Normal and Abnormal Function. Thorofare, NJ: SLACK International (1992).
61. Phisitkul P, Rungprai C, Femino JE, Arunakul M, Amendola A. Endoscopic gastrocnemius recession for the treatment of isolated gastrocnemius contracture: a prospective study on 320 consecutive patients. Foot Ankle Int (2014) 35:747–56. doi:10.1177/1071100714534215
62. Gill LH, Kiebzak GM. Outcome of nonsurgical treatment for plantar fasciitis. Foot Ankle Int (1996) 17:527–32. doi:10.1177/107110079601700903
63. Gurdezi S, Kohls-Gatzoulis J, Solan MC. Results of proximal medial gastrocnemius release for Achilles tendinopathy. Foot Ankle Int (2013) 34:1364–9. doi:10.1177/1071100713488763
64. Riddle DL, Schappert SM. Volume of ambulatory care visits and patterns of care for patients diagnosed with plantar fasciitis: a national study of medical doctors. Foot Ankle Int (2004) 25:303–10.
65. Trent V. An Investigation into the Effect of Stretching Frequency on Range of Motion at the Ankle Joint. Masters Thesis. Auckland: Auckland University of Technology (2002).
66. Faber F, Anderson M, Sevel C, Thorbozrg K, Bandholm T, Rathleff M. The majority are not performing home-exercises correctly two weeks after their initial instruction–an assessor-blinded study. PeerJ (2015) 3:e1102. doi:10.7717/peerj.1102
67. Sciberras N, Gregori A, Holt G. The ethical and practical challenges of patient noncompliance in orthopaedic surgery. J Bone Joint Surg Am (2013) 95:e61. doi:10.2106/JBJS.L.00483
68. Atkins D, Crawford F, Edwards J, Lambert M. A systematic review of treatments for the painful heel. Rheumatology (Oxford) (1999) 38:968–73. doi:10.1093/rheumatology/38.10.968
69. Becerro de Bengoa Vallejo R, Losa Iglesias ME, Rodriguez Sanz D, Prados Frutos JC, Salvadores Fuentes P, Chicharro JL. Plantar pressures in children with and without Sever’s disease. J Am Podiatr Med Assoc (2011) 101:17–24. doi:10.7547/1010017
Appendix A
List of non-traumatic acquired foot and ankle pathology associated with an equinus contracture is described below.
Compression/Dorsal/Anterior
Generalized foot pain especially associated with start up pain or stiffness
Shin splints/Medial tibial stress syndrome
Midfoot osteoarthritis
Jones/Fifth MT metadiaphyseal stress fracture
Ankle arthritis/Anterior ankle spurs (prevention)
Navicular stress fracture
Metatarsal stress fractures (prevention)
Sinus tarsi syndrome
Diabetic Charcot arthropathy
Tension/Plantar/Posterior
Plantar fasciitis
Sever’s disease
Posterior Tibialis Tendon Rupture (PTTR)-Acquired flatfoot deformity
Insertional Achilles tendinosis/Haglund’s deformity
Achilles tendinitis/tendinosis
Achilles tendon ruptures (prevention)
Recurrent musculotendinous Achilles ruptures
Calf cramps at night/Charley horse
Second MTP synovitis/plantar plate rupture which leads to hammer toe
Morton’s neuroma
Diabetic malperforans forefoot ulcer formation
Hallux valgus/Bunion
Hallux rigidus
Appendix B
The rationale as to why calf contractures develop in humans as we age was addressed (5) with one omission: adolescents. I will take this opportunity to address and add this fifth category for the shortened gastrocnemius: bone/muscle growth mismatch. In this category, the gastrocnemius may well be “normal” length genetically speaking, but the tibia is too long creating a relative or situational isolated gastrocnemius contracture or equinus.
This mismatch is found in the adolescents with Sever’s disease (50, 51, 65, 69). It is no coincidence that Sever’s disease occurs just after or late in the physiologic growth spurt most adolescents go through. In this case, the longitudinal growth of the tibia and fibula temporarily outpaces the gastrocnemius and one gets a “situational” isolated gastrocnemius contracture. The innocent calcaneal apophysis is pulled from both ends being placed under excessive tension placing the split second effect into action. It is the pediatric form of plantar fasciitis, nothing more, nothing less.
I believe in time we will find in another subset of this category that excessively tall people also have an increase in isolated gastrocnemius contracture-generated foot and ankle pathologies due to this same mismatch. In this case, the skeletal growth end point is too long for the gastrocnemius muscle, which is too short. While there are no published comparison statistics this author can find, all one has to do is notice the preponderance of foot and ankle problems, particularly plantar fasciitis, encountered in the NBA compared to other sports.
Keywords: equinus, isolated gastrocnemius contracture, plantar fasciitis, insertional Achilles tendinosis, Achilles tendinitis, midfoot arthritis, Charcot arthropathy, biomechanics of gait
Citation: Amis J (2016) The Split Second Effect: The Mechanism of How Equinus Can Damage the Human Foot and Ankle. Front. Surg. 3:38. doi: 10.3389/fsurg.2016.00038
Received: 29 March 2016; Accepted: 14 June 2016;
Published: 27 July 2016
Edited by:
Jaimo Ahn, Hospital of the University of Pennsylvania, USAReviewed by:
Kathryn O’Connor, University of Pennsylvania, USAHarish Hosalkar, The Hosalkar Institute for Joint Preservation and Injury Care, USA
Copyright: © 2016 Amis. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: James Amis, jamesamis@mac.com
 James Amis
James Amis