Consider the Risk of Vesicouterine Fistula in the Event of Intermittent Fluid Vaginal Discharge after a Cesarean Section
- 1Department of Gynecology and Obstetrics, Neuchâtel Cantonal Hospital, Fribourg, Switzerland
- 2Department of Gynecology and Obstetrics, Fribourg Cantonal Hospital, Fribourg, Switzerland
Though the number of Vesicouterine Fistulas is steadily increasing in association with the increasing number of cesarean sections, clinical presentation can be subtle and not easily identified. In this case study, we will review the presenting symptoms of this complication and suggest an updated management protocol.
Introduction
Vesicouterine fistula (VUF) represents 2–9% of all urogenital fistulae. The increasing rate of cesarean sections is associated with a growing number of cases reported in medical literature. In developed countries, most cases occur as a complication of Cesarean section, whereas in developing countries, VUF is mainly a complication following prolonged labor or vaginal obstetric procedures (1).
Youssef first described “Menouria” secondary to a VUF complicating a cesarean extraction in 1957. Menstruation is evacuated through the bladder via the VUF (may even cause amenorrhea). The flow can also be inverted, with urine leaking through the cervix into the vagina imitating urinary incontinence or causing persistent unexplained vaginal discharge following a cesarean section.
In 1999, Maciej Jozwik introduced a classification of VUF based on the routes of menstrual flow:
Type I: amenorrhea (absence of vaginal menstrual bleeding), menouria, and absence of urine leakage (the so-called Youssef syndrome),
Type II: menouria, normal menses, and intermittent urine leakage and
Type III: absence of menouria, normal menses, and intermittent urine leakage.
We will present the case of a patient with prolonged and intermittent vaginal discharge resulting from a VUF following a cesarean section. Note the prolonged delay of 6 months before to establish the diagnosis.
Case Report
The patient has given written consent for the publication of this case study.
A 30-year-old primigravida woman in labor was admitted to the labor ward at term.
The presenting fetal pole failed to descend into the pelvis after 2 h of full cervical dilation and the fetal heart rate monitoring was deemed pathological. An emergency cesarean section was performed according to the “Misgav Lagash technique.” The surgeons encountered no difficulties during the operation and the patient was discharged home on the fourth post operatory day without complications.
One month after the operation, the patient consulted her physician for intermittent vaginal discharge. The vaginal examination was normal: The vaginal mucosa was not irritated; there was a limited presence of vaginal fluid with normal wet mount microscopy. An empirical local antiseptic treatment was prescribed.
The patient continued to report persistent intermittent vaginal discharge. She was referred to our department 6 months after the cesarean section. Upon questioning, she specified that the vaginal discharge was present every day and increased after micturition. The amount of the liquid discharge required one to two sanitary towels per day.
A tampon test (the bladder is filled with methylene blue dye after vaginal tampon insertion, transfer of the dye to the tampon proves the presence of a fistula) confirmed the diagnosis of a urogenital fistula.
We were able to locate the fistula using combined cystoscopy and hysteroscopy (Figures 1 and 2).
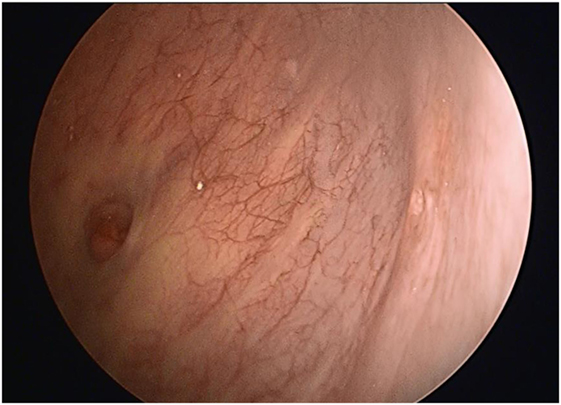
Figure 1. Cystoscopic view of the vesicouterine fistula on the right and the left ureteral ostium on the left.
After discussion, the patient chose to have the fistula surgically repaired. The surgeon selected a laparotomy access via Pfannenstiel to approach the fistula site.
The bladder was completely separated from the uterine scar and the fistula tissue excised. The bladder was closed in two layers with a running suture using PDS 2.O. The uterine wall was closed with a polyglactin1 X-stitch. An omental flap was placed between the vesical and uterine sutures to obliterate dead space and fixed.
An indwelling urinary catheter was left in place for 10 days.
The 3-month postoperative cystoscopy showed a normal vesical mucosa and the tampon test was negative.
One year later, the patient gave birth to her second child by a programmed cesarean section at term. The omentum was easily separated from its vesicouterine adhesion and the bladder was easily manipulated to enable a large exposure of the lower uterine segment. The operation was without complications, and the long-term follow-up was without fistula recurrence.
Discussion
Urogenital fistula is an abnormal communication between the vesical bladder and the female genital tract. In developed countries, most of the cases occur as a complication of cesarean section or other gynecological operations and, less often, after obstetrical complications or different pelvic diseases or irradiation (2–4). In developing countries, urogenital fistulae occur mostly after a prolonged obstructed labor (1).
The World Health organization estimates 130,000 new cases of urogenital fistula occur per year. VUF represent only 2–9% of all urogenital fistulae (5, 6). Described for the first time in 1935, their prevalence was rare until 1947. Since then, their number has increased following the increasing number of cesarean sections and vaginal births following a previous caesarian section (7). A thin lower uterine segment and the presence of scar tissue between the uterus and the bladder related to a previous cesarean section may lead to a VUF as shearing forces are transmitted during labor.
An inadequate reflection of the bladder from the lower uterine segment during cesarean section is the main cause of injury of the bladder either during uterotomy or uterine closure. The devitalization of the posterior wall of the bladder with the presence of hematoma or infection could be the reason for a delayed presentation of the fistula (8).
Other less frequent causes of VUF reported in literature are the manual removal of the placenta, abnormal implantation of the placenta, uterine perforation, and migration of intrauterine device (9) cervical cerclage (10), endometriosis, uterine arteries embolization, necrobiosis of uterine fibroids, inflammatory bowel disease, and pelvic irradiation (11, 12).
A particularity of this type of fistula is that urinary leakage is not always present (see VUF classification in the introduction). Patients with a fistula situated above the internal os of a competent cervix, with the intrauterine pressure higher than intravesical, are continent (13). The VUF often manifests with cyclic hematuria (termed menouria by Youssef) as menses leak into the bladder through the fistulous track. The result is called “Yousseff Syndrome” described for the first time in 1957 and is associated with amenorrhea (absence of vaginal menstrual bleeding), cyclic menouria, and absence of urinary leakage.
The intermittent urine leakage can be explained by the presence of small fistulae, which are permeable during certain phases of the menstrual cycle.
Other presenting complaints can include perineal irritation, vaginal fungal infections, and recurrent urinary tract infections. Infertility and first trimester abortion are also associated. The diagnostic procedure of choice is the tampon test in cases of clinical suspicion of urine leakage through the uterine cervix. The instillation of methylene blue dye or indigo carmine is easily done with limited discomfort. Cystoscopy is usually performed to determine the size and location of fistula tract and its relation with the ureteral meatus (14).
Other imaging procedures can be useful to fully characterize the fistulous tract. There is no clear consensus on the best modality (15) and often more than one technique is required (16). Cystography, hysterography, excretory urography but also ultrasonography with or without intrauterine saline infusion (17, 18) can complete the diagnosis workup. False negatives can occur when sciagraphic pressure is not sufficient to cross the fistulous orifice (19). Helical computer tomography and MRI can be helpful for a patient when several other tests were inconclusive but should not be used as a first line imaging.
Conservative management by the placement of a bladder catheter for 4–6 weeks has been reported for small early diagnosed fistulae (<6 weeks from the causative surgery) (20) with a complete recovery in 5% of the cases. Simultaneous hormonal manipulation with induction of amenorrhea seems to promote spontaneous healing, as histological examination of fistulous tracts showed epithelial and stroma cells that contain sex hormone receptors as in the endometrium (21). There is no consensus for the length of the treatment, but most authors propose a duration of 6 months. Endoscopic fulguration of the fistula with induction of amenorrhea has also been reported (22, 23).
For most patients, VUF surgery is the definitive treatment. Upon the optimal timing of corrective surgery, some authors await the complete uterine involution as well as tissue healing (24). For fistulae post cesarean section, delaying the operation by up to 3 months seems to be preferred when possible. Different approaches have been reported for surgical closure of VUF including vaginal, extra peritoneal or trans peritoneal laparotomies, laparoscopic and robotic procedures (25–27).
The surgical technique usually used is based on the O’Connor’s technique applied for the treatment of VUF. The bladder is mobilized with the dissection of the fistulous tract and the opening of the uterus cavity. The bladder is repaired with two layers of stitches and the uterus is closed with a one layer suture. A vascularized tissue interposition like an omental flap is usually placed to obliterate dead space and prevent hematoma formation (28). The use of a parietal peritoneum flap has also been reported (28).
Vaginal approach is mostly used for VUF when an adequate mobilization is not possible for fistulae situated higher in the posterior wall of the bladder (29, 30). Hysterectomy can also be offered to patients with no desire to keep their uterus.
Concerning the future fertility after the correction of the VUF, Rajamaheswari and Chhikara report a spontaneous pregnancy for every seven patients who had not completed their family (29).
Conclusion
Vesicouterine fistula is a rare type of urogenital fistula. The major risk factor is a previous cesarean section, which explains the growing number of reported cases in literature. Clinical manifestations vary and can be discrete and misleading. The diagnosis of VUF should be considered when there is a history of previous cesarean section. The vaginal tampon dye test is an easy diagnostic test. Treatment of VUF is mostly surgical with the surgical approach depending on the skills of the surgeon. The limited results are reassuring with no apparent effect on patient’s future fertility. An elective cesarean section is preferred after surgical VUF repair.
Ethics Statement
Clinical ethics committee of the Cantonal Hospital of Fribourg. Written consent procedure.
Author Contributions
PT: operator of the surgery. ME: review of the literature. NA: redaction of the article, affiliation to the HFR hospital. JJ, YB, and AF: lecture and correction. BF: correction of the English language redaction.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Vangeenderhuysen C, Prual A, Ould el Joud D. Obstetric fistulae: incidence estimates for sub-Saharan Africa. Int J Gynaecol Obstet (2001) 73:65–6. doi:10.1016/S0020-7292(00)00374-X
2. Setubal A, Clode N, Bruno-Paiva JL, Roncon I, Graca LM. Vesicouterine fistula after manual removal of placenta in a woman with previous cesarean section. Eur J Obstet Gynecol Reprod Biol (1999) 84:75–6. doi:10.1016/S0301-2115(98)00305-4
3. Nariculam J, Aggarwal D, Kapadia S, Walker R, Croucher C. Spontaneous vesico-uterine fistula at the time of miscarriage: a case report. Br J Med Surg Urol (2009) 2(3):124–6. doi:10.1016/j.bjmsu.2008.11.011
4. Furbetta A, Fagioli A, Cristini C, Michetti PM, Trucchi A, Signore S, et al. Vesicouterine fistulae as complications of repeated cesarean section. Int Urogynecol J (1994) 5:240–6. doi:10.1007/BF00460318
5. Hadzi-Djokic JB, Pejcie TP, Colovic VC. Vesico-uterine fistula: report of 14 cases. BJU Int (2007) 53:1361–3. doi:10.1111/j.1464-410X.2007.07067.x
6. El-Lamie I. Urogenital fistulae: changing trends and personal experience of 46 cases. Int Urogynecol J Pelvic Floor Dysfunct (2008) 19:267–72. doi:10.1007/s00192-007-0426-5
7. Bettez M, Breault G, Carr L, Tu LM. Early versus delayed repair of vesicouterine fistula. Can Urol Assoc J (2011) 5:e52–5. doi:10.5489/cuaj.10065
8. Porcaro AB, Zicari M, Zecchini Antoniolli S, Pianon R, Monaco C, Migliorini F, et al. Vesicouterine fistulas following cesarean section: report on a case, review and update of the literature. Int Urol Nephrol (2002) 34:335–44. doi:10.1023/A:1024443822378
9. El-Hefnawy AS, El-Nahas AR, Osman Y, Bazeed MA. Urinary complications of migrated intrauterine contraceptive device. Int Urogynecol J Pelvic Floor Dysfunct (2008) 19:241–5. doi:10.1007/s00192-007-0413-x
10. McKay HA, Hanlon K. Vesicovaginal fistula after cervical cerclage repair by transurethral suture cystorraphy. J Urol (2003) 169:1086–7. doi:10.1097/01.ju.0000047516.32699.aa
11. Krysiewicz S, Auh YH, Kazam E. Vesico-uterine fistula associated with placenta percreta. Urol Radiol (1985) 57:438–9.
12. Fridman D, Chakraborty S, Khulpateea N. Fistula between degenerated uterine leiomyoma and the bladder: case report. Int Urogynecol J (2011) 22(10):1329–31. doi:10.1007/s00192-011-1414-3
14. Park OR, Kim TS, Kim HJ. Sonographic diagnosis of vesicouterine fistula. Ultrasound Obstet Gynecol (2003) 22:82–4. doi:10.1002/uog.161
15. Moon SG, Kim SH, Lee HJ, Moon MH, Myung JS. Pelvic fistulas complicating pelvic surgery or diseases: spectrum of imaging findings. Korean J Radiol (2001) 2:97–104. doi:10.3348/kjr.2001.2.2.97
16. Smayra T, Ghossain MA, Buy JN, Moukarzel M, Jacob D, Truc JB. Vesicouterine fistulas: imaging findings in three cases. AJR Am J Roentgenol (2005) 184:139–42. doi:10.2214/ajr.184.1.01840139
17. Ali-El-Dein B, El-Tabey N, El-Hefnawy A, Osman Y, Soliman S, Shaaban AA. Diagnosis, treatment and need for hysterectomy in management of postcaesarean section vesicouterine fistula. Scand J Urol (2014) 48:460–5. doi:10.3109/21681805.2014.903511
18. Tancer ML. Observations on prevention and management of vesicovaginal fistula after total hysterectomy. Surg Gynecol Obstet (1992) 175:501–6.
19. Alkatib M, Ferano AV, Fynes MM. Vesicouterine fistula following cesarean delivery-ultrasound diagnosis and surgical management. Ultrasound Obstet Gynecol (2005) 26:183–5. doi:10.1002/uog.1925
20. Jozwik M, Jozwik M. Spontaneous closure of vesicouterine fistula: account for effective hormonal treatment. Urol Int (1999) 62:183–7. doi:10.1159/000030388
21. Yokoyama M, Arisawa C, Ando M. Successful management of vesicouterine fistula by luteinizing hormone-releasing hormone analog. Int J Urol (2006) 13:457–9. doi:10.1111/j.1442-2042.2006.01325.x
22. Mathieu B, Breault G, Carr L, Mai Tu L. Early versus delayed repair of vesicouterine fistula. Can Urol Assoc J (2011) 5(2):c52–5. doi:10.5489/cuaj.10065
23. Molina LR, Lynne CM, Politano VA. Treatment of vesicouterine fistula by fulguration. J Urol (1989) 141:1422–3. doi:10.1016/S0022-5347(17)41333-4
24. Wong MJ, Wong K, Rezvan A, Tate A, Bhatia NN, Yazdany T. Urogenital fistula. Female Pelvic Med Reconstr Surg (2012) 18:71–8. doi:10.1097/SPV.0b013e318249bd20
25. Falk HC, Tancer ML. Management of vesical fistulas after cesarean section. Am J Obstet Gynecol (1956) 71:97–106. doi:10.1016/0002-9378(56)90683-4
26. Willson-Pepper JK. Vesico-uterine fistula. Br J Urol (1965) 37:433–6. doi:10.1111/j.1464-410X.1965.tb09621.x
27. Hemal AK, Sharma N, Mukherjee S. Robotic repair of complex vesicouterine fistula with and without hysterectomy. Urol Int (2009) 82:411–5. doi:10.1159/000218529
28. Kilhl B, Nilson AE, Pettersson S. Postcesarean vesicouterine fistula. Acta Obstet Gynecol Scand (1980) 59:277–80. doi:10.3109/00016348009155412
29. Rajamaheswari N, Chhikara AB. Vesicouterine fistulae: our experience of 17 cases and literature review. Int Urogynecol J (2013) 24:275–9. doi:10.1007/s00192-012-1798-8
Keywords: caesarean section, vesicouterine fistula, vaginal discharge, caesarean complication, bladder lesion
Citation: Talla P, Ekotomati M, Brünisholz Y, Bouquet de la Jolinière J, Fagan B, Feki A and Ben Ali N (2017) Consider the Risk of Vesicouterine Fistula in the Event of Intermittent Fluid Vaginal Discharge after a Cesarean Section. Front. Surg. 4:58. doi: 10.3389/fsurg.2017.00058
Received: 05 June 2017; Accepted: 25 September 2017;
Published: 17 October 2017
Edited by:
Evanguelos Nicolas Xylinas, Paris Descartes University, FranceReviewed by:
Marianne Schmid, University Medical Center Goettingen, GermanyChristian Paul Meyer, Brigham and Women’s Hospital, United States
Copyright: © 2017 Talla, Ekotomati, Brünisholz, Bouquet de la Jolinière, Fagan, Feki and Ben Ali. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nordine Ben Ali, docnordine@gmail.com
 Pascal Talla1
Pascal Talla1
 Jean Bouquet de la Jolinière
Jean Bouquet de la Jolinière Anis Feki
Anis Feki Nordine Ben Ali
Nordine Ben Ali