Abstract
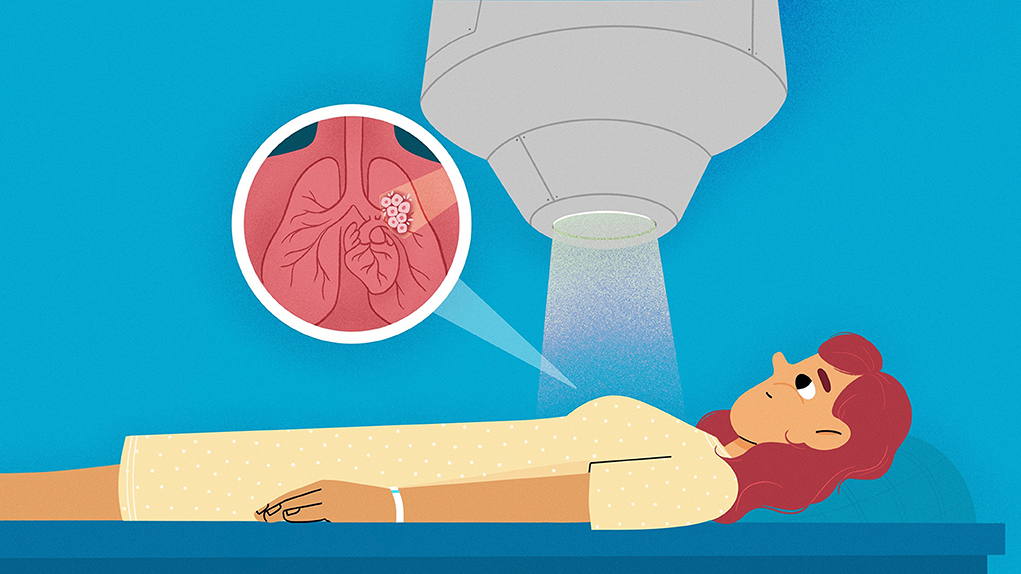
In this article, we will explore the way radiation can be used to treat cancer. Radiation for cancer therapy consists of high-energy particles or light that can damage living cells, including cancer cells. Radiation beams can be generated using a special machine, called a linear accelerator, and they are precisely aimed at a patient’s cancer. When cancer is located near the patient’s lungs, the cancer moves around as the patient breathes in and out. Hitting the cancer with the radiation beam can be hard when the cancer does not stay still. It is a little like trying to hit a moving target in a video game. In that case, there are some tricks that patients and radiation therapy workers can use to make sure that the radiation beam hits the cancer and misses healthy organs.
What is Cancer?
When a person has cancer, they have cells in their body that can increase in number quickly and make them sick. One way that cancer can be slowed down or stopped is by using a kind of radiation. Radiation is energy, in the form of particles or light, that can travel from one place to another. One form of radiation we see every day is light from the sun. Other kinds of radiation have enough energy that they can travel through solid objects, like a person’s body. This type of radiation is called x-ray radiation, and it can be used by dentists to take pictures of teeth. The radiation used for treating cancer is even higher energy. This high-energy radiation can cause a lot of damage to the body’s cells, so scientists aim radiation beams at cancer cells to damage the cancer cells and keep them from growing and spreading. Radiation can hurt both healthy cells and cancer cells, so it is important to be careful to aim the radiation at the cancer cells while avoiding the patient’s healthy cells and organs as much as possible [1].
Where Does Radiation Come From?
Scientists use a machine called a linear accelerator to create radiation beams that are used to treat cancer. This machine speeds up tiny particles called electrons very fast—close to the speed of light! These speedy electrons crash into a piece of metal, which causes the release of large amounts of the radiation used for cancer therapy [2]. You can learn more about linear accelerators from another article in Frontiers for Young Minds. Figure 1 shows a picture of a linear accelerator in a hospital.
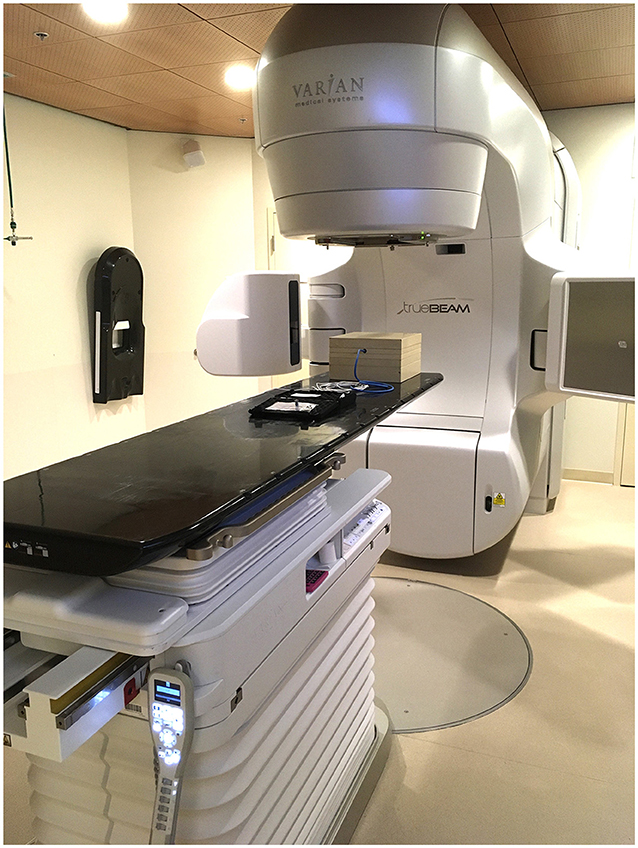
- Figure 1 - Photo of a linear accelerator used to make radiation beams to treat cancer.
Making radiation beams is not the only thing that linear accelerators can do: they can also change the shape of the radiation beam and point it in different directions. You can think of a linear accelerator a little like a flashlight. Just like you can turn on a flashlight, a scientist can turn on a linear accelerator. You can move the flashlight around to change which direction the flashlight beam is headed, and a scientist can change the direction of the radiation beam by moving parts in the linear accelerator. You can also put your hand in front of the flashlight to make shadows of different shapes. Scientists can do the same thing with thick pieces of metal that block part of the radiation beam and change its shape.
What Happens When a Cancer Patient is Treated With Radiation?
Sometimes doctors treat cancer using radiation, sometimes they use drugs called chemotherapy, and sometimes they surgically remove the cancer. Many cancer patients receive radiation therapy as part of their care—in fact, there were about two million new cancer cases in the United States in 2023, and about half of those patients received radiation therapy [3, 4]. When a patient needs radiation therapy, a healthcare team works to deliver the treatment carefully and safely. Before radiation therapy, the patient lies down on a flat surface so their doctor can take a 3D picture of their body, called a CT scan. This scan shows where the cancer is located, and the picture is used by the radiation team to design a treatment that damages the cancer cells and avoids healthy cells.
When it is time for treatment, the patient lies down in the same position they did for their CT scan, and the radiation beam from the linear accelerator is carefully positioned to target the patient’s cancer. The positions of the patient and the radiation beam need to be exactly right because it is important to avoid hitting healthy cells or organs while making sure that the cancer cells are treated with the right amount of radiation.
What Happens When the Target is Moving?
When a patient gets radiation therapy, they must lie very still while their healthcare team gets them into position and aims the radiation beam at just the right spot. But what happens if a patient has cancer in a part of their body that is moving? For example, when you breathe, you can see your chest moving because your lungs are changing shape. When you breathe in, your lungs increase in size and fill with air. When you breathe out, your lungs decrease in size. If a patient has cancer in or near their lungs, this can make aiming the radiation beams trickier than when the target is not moving. You can think of this like a video game in which the player must hit a target with a cannon. In the easy levels, the target stays still. In harder levels, the target moves around. In even harder levels, the target moves around and may also get close to other objects the player is trying not to hit. This is a lot like radiation therapy: the target is the cancer cells, and the cannon is the high-energy radiation.
Sometimes the radiation team can use special tools that help control motion—this is called motion management. Breast cancer is a good example. Breast cancer is a common disease, with about 300,000 new cases in the United States in 2023 [3]. When patients are treated for breast cancer using radiation, the radiation team often wants to treat the whole breast. They need to think about what other healthy cells are near the target so they do not damage those healthy cells. For example, if a patient is being treated for breast cancer on the left side, their heart is near the target. Scientists must also think about what happens to the target when the patient is breathing in and out, which can make the target move around.
We can use some special strategies to hit the target (the breast) while not hitting the object we are trying to avoid (the heart). The patient can be a big help with motion management—they can take a deep breath in and hold it for about 20 s. When they do that, their lungs fill with air, and their chest moves a little farther away from their heart (Figure 2). While the patient is holding their breath, the linear accelerator can be turned on, so radiation is delivered only during the short amount of time that the patient is holding their breath. This allows the radiation beam to irradiate the breast while missing the heart. This strategy is called deep inspiration breath hold. In medicine, the word “inspiration” means “breathing in”. The patient takes in a deep breath (“deep inspiration”) and then they hold it during treatment (“breath hold”).
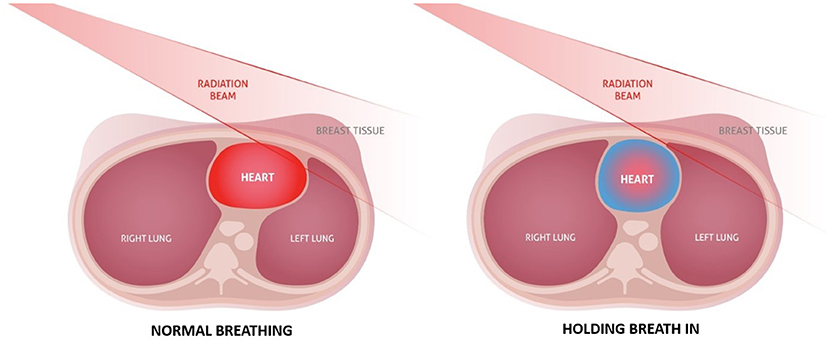
- Figure 2 - Cross-sectional pictures of a patient lying down to be treated for breast cancer.
- On the left, the patient is breathing normally, and the radiation beam aimed at the breast overlaps some of the patient’s heart. This could damage the heart. On the right, the patient is holding a breath in, which makes the lungs expand and pushes the breast away from the heart, so the patient’s breast cancer can be treated without damaging the heart (adapted with permission from Safer Radiation Therapy, Copyright by Vision RT Ltd., 2023).
When you look at Figure 2, it might not look like a very big difference between treating with normal breathing and treating with the patient holding their breath. But this little change can make treatment a lot safer for the patient, so it is important to do!
Most people cannot hold their breath for much longer than 20 s. Since it sometimes takes too long to deliver all the radiation while the patient holds one breath, the patient might be asked to hold their breast a few times. In that case, the radiation is paused, and the patient gets a break to breathe normally for a while. When the patient is ready, they take another deep breath in and hold it, and the radiation beam is turned back on to continue the treatment.
Breast cancer is not the only disease in which there is motion because of breathing. When a patient has a tumor in their lungs, liver, or pancreas, the radiation team can use similar strategies to make sure that they hit the target and miss the healthy tissue, just like with breast cancer.
Summary
Radiation is a tool that can help patients with cancer. When treating a target with radiation, it is very important to hit the right spot and avoid healthy tissue that is in the same region. Motion management strategies help accomplish this, even when the target is near body parts that move around. Patients can help with their own treatment, using techniques like deep inspiration breath hold, to make sure that the cancer cells are treated with high energy radiation while keeping healthy cells safe.
Glossary
Cancer: ↑ A disease in which cells start growing and sometimes spreading in an abnormal way that can cause problems in a person’s body. Tumors can be cancerous.
Radiation: ↑ Energy that can travel from place to place. When radiation has high enough energy, it can be harmful to living cells.
Linear Accelerator: ↑ A machine that generates, shapes, and directs radiation beams at cancer cells.
Radiation Therapy: ↑ A type of treatment used to damage cancer cells using high-energy radiation beams.
Motion Management: ↑ Strategies in radiation therapy to make sure that radiation reaches the target accurately, even when the target can move.
Deep Inspiration Breath Hold: ↑ A technique in radiation therapy in which a patient takes in a deep breath and holds it during treatment.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
Sincere thanks to the IF/THEN organization.
References
[1] ↑ Lim, M. L. F. 2006. Principles and Practice of Clinical Physics and Dosimetry. Madison, WI: Advanced Medical Publishing, Inc., 1.
[2] ↑ Karzmark, C. J., and Morton, R. J. 1998. A Primer on Theory and Operation of Linear Accelerators in Radiation Therapy, 2nd ed. Madison, WI: Medical Physics Publishing, 17.
[3] ↑ Siegel, R. L., Miller, K. D., Wagle, N. S., and Jemal, A. 2023. Cancer statistics, 2023. CA Cancer J. Clin. 73:17–48. doi: 10.3322/caac.21763
[4] ↑ Baskar, R., Lee, K. A., Yeo, R., and Yeah, K.-W. 2012. Cancer and radiation therapy: current advances and future directions. Int. J. Med. Sci. 9:193–9. doi: 10.7150/ijms.3635